Abstract
The aim of this study was to identify aggressive event incidence rates in the inpatient psychiatric setting, describe characteristics of events and differences based on aggression target and type (verbal vs. physical). A longitudinal study was carried out of aggressive events identified by workers in four inpatient psychiatric units using the Staff Observation of Aggression Scale-Revised (SOAS-R) over 6 weeks. A total of 113 aggressive events were recorded resulting in a rate of 13.27 events per bed per year. Verbal aggression was demonstrated in 86 % and physical aggression in 57 % of events. Most events (70.8 %, n = 81) targeted a worker. Compared to other targets, workers were 3.4 times more likely to feel threatened (95 % CI 1.2–9.6, χ2 = 5.08, p = 0.0242), and less likely to have a visible injury (OR 0.15, 95 % CI 0.04–0.6; χ2 = 7.1, p = 0.0078). Event severity ranged from 0 to 21 with a mean of 9.5(SD = 5.1), with 20 % considered severe. Verbal events had lower mean severity of 6.5(SD = 3.8) versus physical events with a severity of 11.8(SD = 4.8; t = 6.5, df = 111, p < 0.0001). In 57.5 % of events there was no consequence to the victim. For most events (76 %) resolution included workers talking to the patient, while 54 % involved use of medication. Restrictive measures (physical hold, seclusion or physical restraint) were involved in 24.8 % of events. Aggression incidence was similar to incidence found in other studies. Workers were the target of most aggressive events and many were identified as having no understandable provocation. Further understanding of event characteristics will promote more effective prevention and management of aggressive events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Aggression in inpatient psychiatry negatively affects patients and workers and prevention is difficult. Accurate patient aggressive event measurement is elusive despite better surveillance and understanding of risk factors [1–3]. In a recent review, an average of 9.3 events per patient per year were documented [4]. Psychiatric nurse aggression exposure is twice the rate of medical-surgical nurses, and a meta-analysis of nurse’s workplace violence reported an average exposure of 67.7 % and injury rates of 40.9 % in psychiatric settings [5, 6]. Aggression surveillance involves identification of sentinel events (injury, patient restraint) reported for safety and occupational health requirements [7, 8]. However, aggressive events span a spectrum from shouting to serious violence, far outnumbering reported sentinel events. In fact, only 40–57 % of aggressive events are reported with most only reported verbally [9]. Thus, improved measurement and surveillance methods are needed to better understand the spectrum of aggressive events.
Improved intervention in aggressive events reduces outcome severity for patients and workers and may eliminate use of coercive measures. Despite this, aggressive events and worker exposure will occur. For example, a patient may become angry and shout, the situation may escalate and a cup may be thrown and the patient may strike out or kick the worker. Successful de-escalation resolves many events at this stage. However an aggressive event occurred with a worker experiencing aggression exposure. Measures sensitive to the full continuum of aggressive events from verbal to physical are needed to track worker and patient exposure and changing incidence resulting from improvements in intervention. Study of aggressive event measures will aid in more accurate surveillance of actual aggressive event incidence. Characterizing events and factors involved in resolution are key to aggression prevention and reduction of worker exposure.
The Staff Observation of Aggression Scale-Revised (SOAS-R) is a measure describing aggressive event incidence and characteristics used in many locations, although few studies report rates from the United States [1, 4]. The SOAS-R ignores worker exposure, only recording patient aggressive events. Information from the SOAS-R can be compared across settings to understand differences in rates based on factors such as location, organization, type of clinical unit, and patient characteristics. The aim of this study was to identify the incidence of aggressive events in the inpatient psychiatric setting using the SOAS-R, to describe event characteristics, and to determine differences in events based on type of aggression (verbal, physical).
Methods
The Aggression Exposure study is a longitudinal study designed to obtain the incidence and characteristics of patient aggressive behavior in the inpatient psychiatric setting using a variety of measures, including the SOAS-R and piloting a new method of event measurement [10]. The setting was a convenience sample of four acute inpatient psychiatric units (two adult, one geriatric, one child and adolescent) of one psychiatric hospital in the northeastern United States (US). Clinical workers (nursing and professional staff) collected data over 10 weeks (based on pilot and administrative data on event frequency), with the initial 4 weeks monitoring only injury and restraint rates. The following 6 weeks (May–June 2011) the SOAS-R and other measures were used. Training on SOAS-R reporting was provided in worker meetings and individually. Workers were asked to record all aggressive events occurring during the 6 week period. Units were regularly visited to collect forms. This report discusses results reported using the SOAS-R.
SOAS-R
The Staff Observation Aggression Scale-Revised (SOAS-R) is completed by workers after witnessing aggressive behavior [11]. The scale defines aggression as “any verbal, nonverbal, or physical behavior that was threatening,” or “physical behavior that actually did harm”, and assesses five areas, including provocation, means, target, consequence(s) to victim(s), measure(s) to stop aggression, and number of days since admission. A total event severity score is obtained from the scale’s algorithm based on reports, ranging from 0 to 22, with scores of 0–7 indicating mild aggression severity, 8–15 moderate severity, and 16–22 severe severity [4, p16]. This scale is widely used to document aggressive events and has adequate validity and reliability. Concurrent validity of the SOAS-R with staff estimates on Visual Analog Scale correlations ranged from r = 0.49 to 0.62, while comparison to the Modified Overt Aggression Scale, the Violence Scale, and the Social Dysfunction and Aggression scale, ranged from 0.62 to 0.81 [4, p13]. Inter-rater reliability is not available, however for the original SOAS ranged from kappa = 0.61 to 0.74 [4].
The study was approved by the Human Subjects Committee. Data was not collected directly from patients or patient records. Clinical workers completed informed consents to participate in data collection.
Analysis
The unit of analysis in this study was the aggressive incident or event. Duplicate events were identified, with seven of 120 reports clearly reporting the same event by date, time and description. Event rates were calculated based on the number of events divided by 42 days in the study period and standardized to a per bed basis by dividing by the number of beds on each unit. The per bed per day rate was then adjusted to provide a per bed per year rate for comparison to other SOAS-R rates [4]. Severity scores were calculated as described by Nijman (1999) and Nijman (2002) [11, 12].
Differences in event characteristics were examined by aggression type (verbal vs. physical) and target (worker vs. other/no target). Differences were evaluated with Chi square or t tests, with p values <0.05 used to determine significance. Data entry and analyses were completed using SPSS and SAS [13].
Results
Aggression Incidence and Characteristics
A total of 113 events were identified, with a rate of 13.27 per bed per year. Events were more frequently reported on day (40 %) and evening shift (42 %) and less often on night shift (17 %). There was 6.7 times higher risk of physically aggressive events in the child-adolescent versus adult inpatient units (95 % Confidence Interval (CI) 1.8–24.5). In addition on the geriatric unit there was a nearly 12 times higher risk of staff members being targeted in the event (Odds Ratio (OR) 11.9, 95 % CI 1.5–94.3) compared to the adult unit.
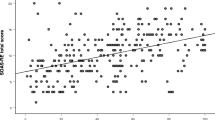
Events occurred from 0.5 to 55 days after admission, with a mean of 10 days. Almost half of aggressive events (46 %) occurred within the first 7 days of treatment (Fig. 1). This compares to an average length of stay of 9.7 days in this time period.
Provocation
There was no understandable provocation for half of the events (47 %, Table 1). Denying the patient something provoked 22 % of events (requests to leave, use the phone, eat certain foods). Helping patients with activities of daily living (ADL’s, hygiene, showering) or requiring a patient to take medication provoked 10 % and other patients provoked 9 % of events. ‘Other’ provocation was identified in 27 % of aggressive events, including patient care activities (moving/redirecting), wanting to leave, or cognitive state (mania, paranoia, delirium, substance-induced psychosis).
Means of Aggression
Verbal aggression occurred in 86 % of events, 57 % involved physical aggression (Table 2). Objects were used in 26 % of events (e.g. chairs, garbage cans). The body was used in 41 % of events (ex: hand, foot). Both objects and the body were used in 12 events, involving throwing objects, hitting or spitting. Only objects were used in 17 events and in 34 events (30 %) only the body was used, involving hitting, grabbing, punching, scratching, biting and spitting. Overall, the hands (punching, hitting) were used in 36 events (31.9 %), feet or kicking in 17(15 %), and teeth or biting in 11(9.7 %). In 21 events only the hand was used, in 6 the hand and some other body part were involved, while three or more body parts were used in nine events (Fig. 2).
Target of Aggression
Most events (71 %) involved a worker target (Table 2). Patients were the target of 11(10 %), and others in 10 events (9 %; visitor, EMT, security). Patients self-harmed in 11(10 %), there was no target in 12(11 %), and objects were targeted in 11(10 %).
Consequence of Aggression
In many events there was no consequence to the victim (58 %). In three events an object was damaged (3 %). The victim felt threatened in 35 events (31 %), and in 29 was the only consequence. Victims were 3.4 times more likely to feel threatened when workers were targeted (95 % CI 1.2–9.6, Wald chisq = 5.08, p = 0.0242); Injury occurred in 20 events(18 %), pain or visible injury in 16, and 14 required treatment(12 %). When workers were targeted, visible injury was 85 % less likely (95 %CI 0.04–0.6, Wald chisq = 7.1, p = 0.0078) and injury treatment 75 % less likely (95 %CI 0.08–0.80, Wald chisq = 5.5, p = 0.02). Workers were 11.8 times more likely to feel threatened when more than one body part was involved (95 % CI 2.96–46.75, Wald chisq = 14.3, p = 0.0008).
Measures to Stop Aggression
Only four events spontaneously resolved. In 76 % resolution involved talking to the patient, and in 20 % the patient was calmly removed from the situation. Medications were used in 61 events (54 %). Nearly half of all events (46 %) involved oral medication, and 11(10 %) involved parenteral medications. Restrictive measures were used in 25 %, 19 involved holding the patient physically (17 %), physical restraint was used in 14(12 %), and seclusion in 6(5 %).
Significant linear trends were found between severity of event and use of medication to intervene (Cochran-Armitage trend test z = −2.68, p = 0.0073), and severity and use of restrictive measures(hold, seclusion or restraint; Cochran-Armitage trend test z = −5.86, p < 0.0001). As expected, severe events were 60 times and moderate events 8.5 times more likely to use a restrictive measure versus mild events (χ 2 = 36.14, p < 0.0001).
For 45 events (39.8 %) workers checked the box, ‘Other’ measures and wrote in interventions including increased observation (n = 16, 35.6 %) with 10(22 %) using one to one observation. Medication use was identified as ‘other’ in nine events; with only one indicating use of medication on the SOAS-R. The use of multiple workers or security for assistance was identified in eight events. Ten events involved use of the patient’s room or other area rather than seclusion to decrease stimulation, of these, five involved one to one observation. Other measures identified included the patient self-calming, a decrease in privileges, allowing the patient to independently complete a task, leaving the room, redirecting the patient, and a verbal warning.
Severity
Event severity ranged from 0 to 21, with a mean of 9.5(SD = 5.1). Only 20 events (20.2 %) were considered severe, 36(36.4 %) were moderate, and 43(43.4 %) were of mild severity. Mean severity was not significantly different whether the patient had a single (mean = 10.1, SD = 5.2) versus repeated event (mean = 9.3, SD = 5.1; t = 0.81, p = 0.42).
Verbal only events had significantly lower severity (mean = 6.5, SD = 3.8) compared to physical events (mean = 11.8, SD = 4.8; t = −6.55, df = 110, p < 0.0001). Event severity significantly differed by shift, 6 % of events on the night shift were severe vs. 38 % severe on days and evenings. Event severity increased with increasing number of body parts and with increasing number of means used (Fig. 2).
Type of Event: Verbal versus Physical Aggression
Verbal aggression was reported in 97 events (86 %), with 51 % exclusively verbal, and 49 % involved physical aggression. Most physical events (75 %) involved both verbal and physical aggression. Event type varied significantly by unit, verbal aggression was more common on the geriatric unit and the adolescent unit more frequently reported physical aggression (83 % of events).
Denying requests was more likely to provoke a physical (84 %) versus verbal event (16 %, χ2 = 9.8, p = 0.0018). More than half (56 %) of physical events involved hitting or punching. Events involving the use of a body part were significantly more likely to result in a restrictive intervention measure (parenteral medication, being held with force, seclusion or restraint (45.7 vs. 10.5 %).
Events without a target were most often only verbal (83 %), and severity was significantly lower than events with a target (4.9 vs. 9.9, F = 11.54, p = 0.001). Two physical events without a target involved objects: a chair was ‘flipped over’; and a door slammed with objects thrown. When the target was identified as an object, nearly all were physical events (91 %).
Discussion
Aggression Incidence and Characteristics
Study results provide data on aggressive events from an acute inpatient psychiatric setting in the US. Event frequency (13.27 per bed per year) is within the range of event rates found elsewhere [11, 14–16]. For example in the Netherlands Nijman (1999) reported rates from 4.8 to 22.4 events per bed per year [11]. Omerov (2002) reported 1.58–4.82 events per bed per year in a psychosis unit in Sweden [16], and Nijman (2005) reported widely varying rates of event incidence (0.4–33.2 events per-patient or per-bed per year)) with a mean of 9.3 events per-patient per-year internationally, variation occurring based on population served, degree of acuity and length of stay [4]. In this study similar prevalence was found on day and evening shift (40, 42 % respectively) to that found elsewhere [17]. In other studies greater prevalence of events has been found in the day shift or evening shift vs. other shifts [15, 16].
Most events occurred soon after admission, and later events (up to 55 days into treatment) suggest different processes may be involved, possibly related to acuity of illness, or placement after discharge. Future study could characterize differences between events occurring early and late in admission.
Given significant differences in aggression rates by both type (verbal, physical), target, and unit (adult, geriatric, adolescent), analyses could characterize event trajectories based on type of unit when planning interventions, for example adolescents may respond differently to intervention than adults. In addition the care provided on geriatric units often involves close physical contact to assist individuals with ADL’s and heighten risk of aggressive events. Interventions could be designed specific to this population and their inherent needs.
The SOAS-R was useful to identify aggression incidence and characteristics (timing, severity) and provides meaningful information including provocation, means and target of aggression, effect on victim, and intervention measures. Some aspects of the scale, such as ‘felt threatened’ are unclear as to who is feeling the threat or target, and addition of fields such as person completing the scale, or others as possible target, victim or exposed would clarify event characteristics. As currently designed, a limitation of the SOAS-R is that it does not provide a means of identifying rates of worker or patient exposure to aggression, as worker exposure is not recorded with each event.
For half of the events reported, understandable provocation was unknown and needs to be better understood. Are these completely unexpected events or is the precipitant not on the scale? In-depth study of events reported may help to answer this question. It may be useful to supplement scale use with information gathering, including interviewing workers about events. Limitations may include that the scale doesn’t offer some precipitants as options or that with retrospective reporting, there is not adequate knowledge or recall of precipitants.
Given the large number of ‘other measures’ used to intervene (40 % of events) the SOAS-R form may be revised to reflect interventions such as: decreased stimulation; increased level of observation; offered medication with note of refused or taken; involvement of multiple staff; or that the event subsided without intervention(self-calming, left alone). Other changes might include simplifying or changing terms to those more commonly used in clinical practice, such as change to injectable or intramuscular(IM) medication from ‘parenteral’ or ‘per oral’.
Target of Events
Workers were most frequently targeted, which is similar to prior findings [11, 14, 17]. When ‘no provocation’ was identified, workers were most often targeted, which may relate to missing cues to precipitants or patient distress. Workers were more frequently a target when directly intervening with patients related to ADL’s, medications and refusing patient requests, suggesting these are times of greater risk. When workers were targeted, victims were more likely to feel threatened, however less likely to have visible injury or require treatment of an injury. While it may seem non-intuitive, one possibility is that injury or treatment was less likely because workers prevented escalation of incidents when they felt threatened. Adding fields to the SOAS-R that include aspects of worker exposure might provide a more complete recording of both patient events and worker exposure and better understanding of event prevention or resolution.
Severity
Mean event severity was 9.5(SD = 5.1), which is similar to mean severity of 9.2–11.0 in a review of SOAS results [3, p14]. Workers reported that the severity of verbal events was lower than physical events, providing evidence of construct validity. Severity scoring is determined by the highest scored item per column; however findings suggest there may be reason to further evaluate the scoring system. Though differences between verbal and physical events may seem to be an artifact of scoring, this would only account for 2 of the 5.3 point difference in severity score. Similarly the relation of severity to measure used may be an artifact, although only accounting for 2–4 points of the differences found; with severity ranging from 4 to 6.3 points on average for medication use and restrictive measures respectively. Future portrayal of ‘typical events’ by level of severity may provide better understanding of properties of severity.
Physical versus Verbal Events
Similar to other studies, verbal events were most common, and 43 % were ‘verbal only’ [17]. The high proportion of physically aggressive events (57 %) suggest that physical events are more likely to be recorded. Denying patient requests increase the likelihood of a physical event, and provides an area to consider in intervention design. For example, request denial is considered a ‘flashpoint’ for conflict and containment and is an intervention focus in the Safewards Trial which successfully reduced rates of aggressive events [18–20].
Strengths
The SOAS-R provides rich information about aggressive event characteristics, and is easy to complete. In the current study research personnel educated workers regarding procedures and provided regular follow-up. This study adds to the scarce information on event incidence and characteristics in US inpatient psychiatric settings. The use of the SOAS-R offers clarity in defining aggressive events and has a scale based formula to identify event severity which removes some of the subjective nature of aggressive event reporting. In addition the scale offers a more complete record of day to day aggressive events that are under-reported in most settings.
This information is important as there may be differences in settings across cultures and internationally. Results are representative of the experience of one urban inpatient psychiatric setting and rates of events may not be generalizable to other settings. However the 6-week period of data collection across four units provided some assurance that rates are not specific to individual patients, workers or unit. Further study is needed to understand expected rates and characteristics of aggression in US psychiatric settings.
Limitations
Underreporting is a common problem with retrospective measures, and has also been cited with the SOAS-R [4, p18]. It is possible that the incidence of aggression recorded in this study may not accurately reflect actual incidence rates over longer time periods or may be influenced by factors occurring during the study period. Little research on rates of aggressive events are available from the US using validated scales offering clear definitions of aggression as was used in this study. Additional research on US rates of aggressive incidents is important to better understanding how to prevent and intervene in aggressive events.
The high proportion of physical events reported may indicate under-reporting of verbal only events and needs to be evaluated in further research comparing SOAS-R reports to other measures. Although use of multiple measures concurrently may have resulted in worker fatigue with scale completion, it is also possible that use of multiple measures led to increased reporting due to worker motivation to appear consistent and comply with study demands. Lastly, severity of event scoring is algorithm based and perceptions of severity have not been validated internationally, further work in this area would be informative [3, 10].
Conclusion
The SOAS-R provides event and rate information about aggressive events in acute inpatient psychiatric settings. Results suggest that verbal and physical aggression are relatively common and rates similar internationally. Similar patterns of severity and worker targeting were also found. Improved methods of measuring aggressive events and worker exposure to aggression will aid in aggression prevention and efforts to reduce worker exposure. Further study of events across the continuum of aggression offers an opportunity to better understand ways to more effectively intervene with patient aggression.
References
Flannery RB, Wyshak G, Tecce JJ, Flannery GJ: Characteristics of American assaultive psychiatric patients: Review of published findings, 2000–2012. Psychiatric Quarterly 85:319–328, 2014.
Hamrin V, Iennaco J, Olsen D: A review of ecological factors affecting inpatient psychiatric unit violence: Implications for relational and unit cultural improvements. Issues in Mental Health Nursing 30(4):214–226, 2009.
Findorff MJ, McGovern PM, Wall M, Gerberich SG, Alexander B: Risk factors for work related violence in a health care organization. Injury Prevention 10:296–302, 2004.
NIjman HLI, Palmstierna T, Almvik R, Stolker JJ: Fifteen years of research with the Staff Observation Aggression Scale: A review. Acta Psych Scand 111:12–21, 2005.
Gerberich SG, Church TR, McGovern PM, Hasen H, Nachreiner N, Geissser M, Watt G: An epidemiological study of the magnitude and consequences of work related violence: The Minnesota nurses’study. Occupational Environmental Medicine 61:495–503, 2004.
Spector PE, Zhou ZE, Che XX.: Nurse exposure to physical and nonphysical violence, bullying, and sexual harassment: A quantitative review. International Journal of Nursing Studies 51:72–84, 2014.
Joint Commission. 2016. https://www.jointcommission.org/core_measure_sets.aspx Accessed 8 July 2016.
Occupational Safety and Health Administration. (2001). Recording and Reporting Occupational Injuries and Illness. Part 1904 C. Regulations (Standards-29 CFR) U.S. Department of Labor. http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_id=9638&p_table=STANDARDS Accessed 8 July 2016.
Findorff MJ, McGovern PM, Wall MM, Gerberich SG: Reporting violence to a health care employer: A cross-sectional study. AAOHN Journal 53(9):399–406, 2005.
Iennaco J, Dixon J, Whittemore R, Bowers L, (January 31, 2013). Measurement and Monitoring of Health Care Worker Aggression Exposure. OJIN: The Online Journal of Issues in Nursing. 2013; 18(1): Manuscript 3.
Nijman HLI, Muris P, Merckelbach HLGJ, Palmstierna T, Wistedt B, Vos AM, van Rixtel A, Allertz W: The staff observation aggression scale-revised (SOAS-R). Aggressive Behavior 25:197-209, 1999.
Nijman H, Evers C, Merckelbach H, Palmstierna T: Assessing aggression severity with the revised staff observation aggression scale. Journal Nervous and Mental Disease 190(3):198–200, 2002.
SAS Institute, Cary NC.
Kraus JE, Sheitman BB: Characteristics of violent behavior in a large state psychiatric hospital. Psychiatric Services 55(2):183–185, 2004.
Barlow K, Grenyer B, Ilkiw-Lavalle O: Prevalence and precipitants of aggression in psychiatric inpatients. Aust NZ J Psychiat 34:967–974, 2000.
Omerov M, Edman G, Wistedt B: Incidents of violence in psychiatric inpatient care Nordic Journal of Psychiatry 56:207–213, 2002.
Foster C, Bowers L, Nijman H: Aggressive behavior on acute psychiatric wards: Prevalence, severity and management. Journal of Advanced Nursing 58(2):140–149, 2007.
Bowers L, James K, Quirk A, Simpson A, Stewart D, Hodsoll J: Reducing conflict and containment rates on acute psychiatric wards: The Safewards cluster randomised controlled trial. International Journal of Nursing Studies 52:1412–1422, 2015.
Bowers L Safewards: A new model of conflict and containment on psychiatric wards. Journal of Psychiatric and Mental Health Nursing 21:499–508, 2014.
Bowers L, Alexander J, Bilgin H, Botha M, Dack C, James K, Jarrett M, Jeffery D, Nijman H, Owiti JA, Papadopoulos C, Ross J, Wright S, Stewart D: Safewards: The empirical basis of the model and a critical appraisal. Journal of Psychiatric and Mental Health Nursing 21:354–364, 2014.
Acknowledgments
We thank Lawrence Scahill PhD, Susan Busch PhD, and Len Bowers PhD for their guidance with the Aggression Exposure Study; Meghan Parmenter, Lauren Fiola, Rachel Mauro, Hannah de Long for their contributions as Research Assistants; Hospital and Nursing Administrators, Pamela Mathews, and the workers who assisted and participated in the Aggression Exposure Study. This publication was made possible by Clinical and Translational Science Award Grant Number UL1 RR024139 and KL2 RR024138 from the Yale Center for Clinical Investigation and the National Center for Research Resources and the National Center for Advancing Translational Science, components of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Joanne Iennaco, Robin Whittemore, Jane Dixon have declared that they have no conflicts to report.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Iennaco, J.D., Whittemore, R. & Dixon, J. Aggressive Event Incidence using the Staff Observation of Aggression Scale-Revised (SOAS-R): A Longitudinal Study. Psychiatr Q 88, 485–499 (2017). https://doi.org/10.1007/s11126-016-9462-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-016-9462-y