Abstract
Spatially concentrated, vaccine-hesitant populations represent an ongoing challenge to public health policies that emphasize mass vaccination as a means to eradicating certain infectious diseases. Previous research suggests that Amish populations, which are spatially clustered and rapidly growing, may be undervaccinated. However, existing evidence is limited to local case studies in pre-COVID-19 contexts. Using a series of negative binomial regression models, we evaluated the association between county-level vaccination rates and the percentage of Amish in 356 Amish-populated counties in the United States from February 1, 2021 through October 31, 2022 while controlling for a set of covariates known to impact vaccination rates. Our findings suggest that, after adjusting for county-level characteristics, Amish-populated counties had approximately 1.6% (95% CI: 1.1%-2.0%; p < 0.001) lower rates of getting COVID-19 vaccines. Our findings underscore the failure of public health outreach efforts to convince Amish to accept COVID-19 vaccines. Prevailing public representations of the Amish—as an unproblematic people removed from public affairs and largely unaware of the “outside world”—may have helped Amish avoid societal pressure to vaccinate. Furthermore, because Amish are not as much “hard to reach” as “hard to vaccinate,” we suggest service providers and policy-makers avoid top-down approaches that target the Amish—including cultural competency strategies that work to reduce perceived boundaries—and instead give Amish space to either initiate bottom-up partnerships with health services or accept responsibility for undervaccination in public life.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In developed countries such as the United States, mass vaccination campaigns have nearly eliminated rubella, measles, pertussis, and other infectious diseases. However, in an interview on National Public Radio (December 7, 2021), then-director of the National Institutes of Health, Francis Collins, expressed his surprise that 60 million Americans have not received COVID-19 vaccinations. Collins argued that a better understanding of individual health behavior and decision-making is needed for public health measures to have a full effect. To better understand an individual’s decision-making, researchers and service providers must account not only for individual decision-making calculus but also for the contexts in which individuals are embedded. Social contexts and population categories—such as ethnicity, religion, social class, neighborhood, race, or political affiliation—provide individuals with ideologies, repertoires of social actions, opportunities and constraints, and scripts for rationalization. Accordingly, attention to particular populations will help explain why clusters of people resist vaccination.
Vaccine hesitancy—an attitude—is the primary reason undervaccination exists in contexts where vaccines are readily available. When vaccine hesitancy arises from a population’s shared culture and that population is spatially concentrated, disease may spread rapidly through contagion. As such, vaccine-hesitant, spatially concentrated populations present an ongoing challenge both to the total elimination of vaccine-preventable contagious diseases and to medical training and infrastructure, which must remain responsive to increasingly unfamiliar yet age-old diseases. Public efforts to disseminate COVID-19 vaccinations provide an opportunity to identify the vaccine-hesitant populations and thus prepare medical infrastructure and outreach efforts for the possibility of place-specific outbreaks.
This present study introduces North America’s Amish as a spatially concentrated, rapidly growing population that may be undervaccinated due to vaccine hesitancy. To test our hypothesis, we conduct a regression analysis with county-level data about Amish populations and COVID-19 vaccination—among other social data—in the ten most Amish-populous states. Among existing assessments of Amish undervaccination, both our method and scale of population analysis are new. We find that the presence of Amish populations predicts low COVID-19 vaccination rates, net of other factors. Given the concentration of Amish in rural places and their rapid population growth, we conclude this article by discussing implications for public policy and service.
Prior Research
This study focuses on the Amish population in the ten most Amish-populated US states. The Amish are an ethnic religion concentrated primarily in rural areas in the US’s mid-Atlantic, Midwest, and upper South, and in southern Ontario, Canada. From the early 1700s to mid-1800s, Amish populations migrated to North America from the regions bordering contemporary Switzerland, Germany, and France. Families settled near each other in spatial clusters as they followed the frontier westward, from Pennsylvania through Ohio and Indiana and into the Great Plains. While some Amish settlements eventually disbanded or assimilated into the American mainstream, many exist today (Crowley, 1978; Hopple, 1981; Luthy, 1986; Reschly, 2000); see Anderson and Bacon (2023) for profiles of individual settlements, including those referenced throughout this article.
Though the Amish are a tiny fraction of North America’s population—approaching 400,000 people—they have long sustained a near-exponential growth rate (Cross, 1976; Donnermeyer et al., 2013; Landing, 1970; Rountzounis et al., 1968). This population growth is explained by high birth rates and low attrition rates, although rates vary across Amish churches, denominations, and settlements (Choy, 2020; Meyers, 1994; Wasao et al., 2021). The Amish maintain a strong sense of ethno-religious identity that supports maintenance of a minority language (“Pennsylvania German” or simply “Amish”), nearly universal endogamy, heritage-focused literature and religious worship forms, and other in-group practices (Byfield, 2019; Enninger, 1986; Enninger & Raith, 1982; Rumsey, 2016; Škender, 2020).
Given that the Amish are largely concentrated in rural areas, an outbreak of a contagious disease among them could strain an already limited health infrastructure (Gastañaduy et al., 2016). By late spring 2021, as COVID-19 vaccinations became widely available, news coverage began identifying areas with low vaccination rates, finding that some counties in rural areas had sizable Amish populations.Footnote 1 The news articles, taken together, suggested a broader pattern of Amish vaccination hesitancy. In academic literature, four bodies of research lead us to expect that the Amish population would, indeed, be hesitant to accept the COVID-19 vaccine.
Community-Level Studies of Undervaccination
Before COVID-19, community studies repeatedly documented undervaccination in Amish-dense regions, including Arthur, Illinois (Yoder & Dworkin, 2006), Holmes County, Ohio (Scott et al., 2021; Wenger et al., 2011), and Ashtabula County, Ohio (Kettunen et al., 2017). Further, Amish-focused case studies about outbreaks of rubella in Ethridge, Tennessee (Briss et al., 1992) and Holmes County, Ohio (Jackson et al., 1993); measles in Knox/Holmes Counties, Ohio (Gastañaduy et al., 2016); and pertussis in and around Arthur, Illinois (Medina-Marino et al., 2013) suggest undervaccination. Cumulatively, these cases point to undervaccination as a population-wide pattern (Anderson & Potts, 2022) and suggest that Amish populations will have low COVID-19 vaccination rates. However, we cannot conclude that, because the Amish are hesitant to accept other vaccines, Amish will be hesitant to accept COVID-19 vaccinations. The COVID-19 outbreak represents a new scenario at a new time, namely, during a pandemic, the like of which has not been known in North America for around a century. Further, public health efforts encouraging adoption of COVID-19 vaccinations have been extensive. Existing research suggests, in some cases, Amish may be responsive to such public vaccination efforts (Fullenkamp, 2021; Gastañaduy et al., 2016; Glover, 2015).
Insular Components of Amish Culture
Cultural and value orientations including social–political conservatism, low confidence in science, and low educational attainment often predict a lower likelihood of a population receiving COVID-19 vaccinations (Viswanath et al., 2021). The most common reasons for individuals’ rejection of COVID-19 vaccinations include the vaccine’s safety, side effects, actual effectiveness, and a personal suspicion about conspiracy and the politicking around the vaccine effort (Roy et al., 2022). These findings together suggest a profile of someone who hesitates to trust anonymous yet credentialed knowledge-validating authorities and who maintains some cultural/cognitive distance from institutionalized, mainstream, and esteemed Western processes. The Amish share many of these cultural orientations and rationales for rejecting modern medicine, including vaccinations. Their attitude toward the scientific health establishment is selective and somewhat critical (Anderson & Potts, 2022).
However, few empirical studies demonstrate why and how Amish cultural patterns might influence health behavior such as vaccine acceptance—perhaps because few collaborative bridges exist between physical health research and deep cultural research (Anderson & Potts, 2021; Jolly, 2017). For now, we can at least infer from cultural research that societal preconditions exist for Amish vaccine hesitancy. Researchers and service providers have made compelling arguments about how the Amish cultural schema is inwardly oriented, intensely sectarian, and insular (Anderson, 2017; Reschly, 2000). Amish cultural insularity is rooted in a concept of religious specialness, the significance of which is reaffirmed through quotidian social actions (Enninger, 1988b; Freudenburg et al., 2020; Petrovich, 2013, 2022a; Rumsey, 2010), a social structure that is kinship-oriented (Enninger, 1986; Škender, 2020), an in-group communication system—namely, language and dress—that creates “our” social spaces and triggers identity awareness (Byfield, 2019; Enninger, 1984; Enninger & Wandt, 1979), and an individual sense of ease navigating familiar in-group social contexts (Rumsey, 2016), among other social dynamics. Given the dense social networks of the Amish, much pressure exists to conform to cultural/religious ideals even if elements of one’s actual lifestyle deviate (Ems, 2022; Friesen & Friesen, 1996, Ch. 7; Kidder & Hostetler, 1990; Welk-Joerger, 2021).
The Amish sense of religious specialness means that individuals are likely to interpret life experiences—including health experiences—spiritually (Petrovich, 2022b; Sharpnack et al., 2010). Consequently, when seeking help for illness, Amish people usually turn to co-members, who are sensitive to religious and social needs (Hess, 2018; Sauder, 2020). They prefer health treatments confirmed as “our people’s”—from the herbs “we” use to clinics and doctors “we” like (Anderson & Potts, 2020). The health treatments most accessible to the Amish—who rarely go beyond eighth grade—are not scientific medicines but lay-accessible alternative and complementary health practices—which are often understood in spiritual terms (Welk-Joerger, 2019); these treatments hold a privileged place in health advice. Thus, one consideration for Amish individuals when deciding whether to accept vaccination will be their sense of how much this particular scientifically developed, institutionalized medical practice—that is, a practice disembodied from their familiar, integrated contexts—is something “we” accept.
Amish individuals also have a sense of assurance that the group can mediate or buffer outside problems and that, ultimately, some of “their” problems are not “our” problems (Hartman, 2001; Kidder & Hostetler, 1990; Longhofer, 1994). Amish people might recognize that COVID-19 is, scientifically, a real disease that can threaten life, but at the same time, they might be disinclined to view the threat as really impacting “our people.” It follows that, inasmuch as COVID-19 is viewed as “their” disease, vaccination, too, might not be for “our kind of people.” Indeed, some genetic and environmental evidence exists that plain people might not be as susceptible to some health problems (Anderson & Potts, 2022), such as asthma (Stein et al., 2016), certain cancers (Westman et al., 2010), and prolonged birthing (Jolly, 2014a). Some Amish might also have strong immune systems as a result of exposure to farm dust (Dhakal et al., 2019). Interpreted in the context of the social construction of illness paradigm (Conrad & Barker, 2010), these studies suggest that, in fact, Amish people can and do experience illnesses in ways distinctive to their culture.
Given the way Amish ethno-religious configurations intersect with Amish health practices and beliefs, we expect that Amish individuals would view with suspicion the COVID-19 vaccine, a scientifically complex and invasive medical treatment (that is, a personally unverifiable health product injected into one’s physical body) developed and promoted by unfamiliar institutions outside their cultural setting. Within this insular system, we further expect that opinions against the COVID-19 vaccine will be reinforced and solidified across time as talk circulates, so that rejecting the vaccine will be perceived as “our” decision, even though no peoplehood council, per se, such as church leaders, decided against it (Ems, 2022; Graybill, 2022).
Influence of Non-Amish Neighbors on the Amish
Amish insularity should not be conflated with being isolated or closed off; non-Amish and Amish network bridges are many, and influence flows both ways across these ties. The non-Amish people in areas Amish are present tend to be populations with characteristics also associated with overall vaccine hesitancy, including low-income, rural location, politically conservative/Republican, and low educational attainment (Anderson & Kenda, 2015; Hudson & Montelpare, 2021; Mann et al., 2022; Mollalo & Tatar, 2021; Viswanath et al., 2021).
Amish individuals typically manage diverse bridges to non-adherents, some of whom they might trust more than they trust other adherents (Jeong, 2013; Jolly, 2014b; Lutz, 2017; Martin, 2021). These “bridges” frequently begin as commercial or pragmatic relationships with local residents who work as taxi drivers, store clerks, laborers in trades economically related to common Amish occupations (Ems, 2022; Hawley & Hamilton, 1996; Jeong, 2013; Park, 2018), and service providers who have built trust (Hess, 2017; Miller-Fellows et al., 2018; Quinn, et al., 2021; Thalheimer, 2021). Such relationships, however, do not begin with assumptions of trust, as do co-adherent relationships (Farrar et al., 2018). Indeed, Amish people seem relatively quick to distrust the broader economic–industrial–governmental complex and its practitioners (Garrett-Wright et al., 2016; Long, 2022), which scientific medicine is part of. In particular, the institutionalization, bureaucratization, and governmental nature of public services can work against trust-building (Enninger, 1988a; Olshan, 1990; Reiling & Nusbaumer, 1997; Schlegel, 1997). Nevertheless, pervasive bridging does suggest Amish individuals might be variously impacted by non-adherent social systems and cultures, both those favoring and those cautioning COVID-19 vaccination. Given that ties of trust are more likely formed with local residents who are associated with population categories hesitant to accept the COVID-19 vaccine and that ties of trust with health service providers and others favoring vaccination are less common, we expect that the external ties of Amish people will reinforce aspects of Amish culture inclined toward vaccine hesitancy.
Amish Hesitancy to Adopt Measures Slowing the Spread of COVID-19
At the pandemic’s onset and prior to COVID-19 vaccination availability, a convenience sample of Amish adherents demonstrated hesitancy—though not total opposition—toward adopting public health measures, such as social distancing and masking, to slow the spread of COVID-19. This hesitancy likely extended to COVID-19 vaccinations. In two studies co-authored by the Centers for Disease Control and Prevention (CDC) and local health department partners, researchers interviewed approximately 10 Amish people, each from two of the three largest Amish settlements: Wayne County, Ohio, part of the greater Holmes County settlement (Ali et al., 2020), and Elkhart County, Indiana, part of the greater Elkhart-LaGrange Counties settlement (Duran et al., 2020). The goals were to assess Amish attitudes and practices regarding COVID-19 public health measures. Both studies documented rumors and misinformation among the Amish about COVID-19 and health measures (theme 2 from the Wayne County study/theme 3 from Elkhart), cultural and logistical barriers to practicing health measures and testing (respectively, themes 3, 5, 6/theme 1), social cohesion and the rapid spread of opinions about health across Amish social networks (themes 4, 7/theme 6), and emphasis on adherents selflessly helping each other with needs (themes 8, 10/topic “Community Facilitators”). The Elkhart study independently noted Amish people’s general distrust of the government, health care system, and media (theme 2); minimal concern about COVID-19’s impacts (4); and belief that prevention efforts were ineffective or overstated (5). If these small convenience samples are at all representative of the larger Amish population, we expect that Amish individuals have also disseminated misinformation about the COVID-19 vaccination, encountered cultural and logistical barriers to receiving vaccinations, spread health-based opinions about vaccinations in their networks, generally distrusted the institutions promoting vaccination efforts, and maintained skepticism about COVID-19’s impacts and the effectiveness of prevention efforts.
Research Questions and Hypothesis
Though existing studies document general Amish vaccine hesitancy in several local communities, no population-wide evidence of Amish vaccine hesitancy exists, let alone for the recent COVID-19 vaccines. Our study’s goal is to address a gap in current knowledge of population-wide vaccine hesitancy and hesitancy about the COVID-19 vaccine in particular. In this study, we ask “Do we find lower COVID-19 vaccine adoption rates in counties where a higher percentage of the population is Amish? That is, are the Amish vaccine hesitant, as evidenced by low county-level vaccination rates?” For the four reasons above—hesitancy toward vaccines in general, an insular ethnic context rooted in a sense of religious exceptionalism, social connections with vaccine-hesitant rural neighbors, and hesitancy to accept other COVID-19 public health measures—we hypothesize that the presence of Amish populations will be negatively associated with COVID-19 vaccination rates.
Data, Variables, and Methods
Because no individual data were collected at the time of vaccination that specifically identified Amish individuals, we use data from the 2020 US Religion Census, which provides the most recent county-level Amish population number that is peer reviewed and publicly available. This study focuses on the 10 states with the largest Amish populations: Ohio, Pennsylvania, Indiana, Wisconsin, New York, Michigan, Missouri, Kentucky, Iowa, and Illinois. Amish population numbers in other states are less than half that of the state with the tenth largest Amish population—hence, this cut-off was used.
The county-level vaccination rate was obtained from the CDC Data Tracker,Footnote 2 a website that records county-level vaccination rates from December 13, 2020, to the present. It also includes each county’s metropolitan status based on the National Center for Health Statistics (NCHS) urban–rural classification scheme and divides counties into metro/non-metro. Although the CDC Advisory Committee on Immunization Practices recommended the Pfizer or Moderna vaccinations in December 2020 (CDC, 2022), the CDC tracker shows that in the counties from the states selected for our study, people did not begin to receive vaccinations until late January 2021. Before that, residents were almost entirely unvaccinated. Accordingly, we selected February 1, 2021, as our start date and October 31, 2022, as our end date.Footnote 3
The CDC tracker presents vaccination rates as cumulative and, therefore, monotonically increasing with time. We determined the daily vaccination rate by subtracting the vaccinated population from that of the prior day, then divided by the county population. The vaccinated population was sourced from the CDC tracker’s series_complete_yes variable, which represents the number of people who have completed the primary vaccination series, i.e., the second dose of a two-dose vaccine or one dose of a single-dose vaccine. The county population was sourced from the 2020 census data.
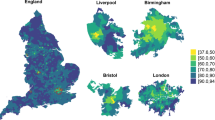
The daily vaccination rate has some outliers because the daily vaccinated population can vary substantially. For example, more people might be vaccinated on weekends than weekdays. To smooth out the outliers, we averaged the daily vaccination rate to a monthly vaccination rate weighted by the county population. In total, we obtained 7476 observations consisting of 21 months of data from 356 Amish counties. Figure 1 shows the distribution of the county-level monthly vaccination rate, demonstrating that the monthly vaccination rates are right-skewed with most observations below 0.1%.
Since the monthly vaccination rate is heavily right-tailed, we performed the Spearman rank correlation coefficient (rs), which provides higher variability than Pearson’s correlation coefficient for heavy-tailed data (De Winter et al., 2016). We then conducted a regression analysis of the vaccination rate of Amish-populated counties on the percentage of Amish in the overall population. Our regression analysis controlled for population characteristics that might also predict vaccine hesitancy in the larger, non-Amish population:
-
County-level median household income, with data from the 2019 American Community Survey (ACS), as a measure of household wealth (Khubchandani et al., 2021);
-
County metro/non-metro status, with data from the 2020 US Census, as a measure of rurality (Albrecht, 2021; Mueller et al., 2020);
-
Percentage voting Republican in the 2020 presidential election, using data from the MIT Election Lab,Footnote 4 as a measure of socio-political attitudes (Agarwal et al., 2021);
-
Percentage of evangelical Protestants, using data from the 2020 US Religion Census—as aggregated by the Association of Religion Data Archives (ARDA).Footnote 5 Evangelicalism is a religious family proximate to the Amish and experiences a degree of tension with “mainstream culture” (Smith & Emerson, 1998). While adherents of evangelicalism may be less likely to accept vaccination (Nagar & Ashaye, 2022), it is possible that specific beliefs within evangelicalism that cannot be isolated with our data might better explain undervaccination (Corcoran et al., 2021).
We initially included the percentage of college graduates in the model, assuming that educational attainment will influence vaccination rates (Paul et al., 2021). However, educational attainment is highly correlated with household income (r = 0.55, p < 0.05) and the percentage voting Republican (r = − 0.72, p < 0.05), causing multicollinearity. In response, we dropped the percentage of college graduates in the model.
As shown in Fig. 1, the dependent variable—county-level monthly vaccination rate—is non-negative and right-skewed. Consequently, we employed negative binomial regression because it is well suited for modeling non-negative, right-skewed data (Coxe et al., 2009; Liu et al., 2005). Data analyses were conducted using Stata 16.1. For modeling, we used xtnbreg, a Stata command that fits negative binomial regressions for panel data. Because this study is not an experimental design, statistical relationships are correlative, not causal.
Because our research employed publicly available, aggregated, secondary data and did not engage human subjects, this study was not subject to IRB review.
Results
Descriptive statistics are provided in Table 1. On average, the county-level monthly vaccination rate across all 2020 Amish-populated counties was about 0.1%. The average percentages of the Amish population and evangelical Protestants were, respectively, 2.1% and 19.7%.The percentage voting Republican in the 2020 presidential election was about 68.0%, and the average median household income was $53,090. A metropolitan designation applies to 26.0% of selected counties.
The Spearman correlations between the Amish population and vaccination rate are statistically significant and negative (rs = − 0.067, p < 0.05; N = 7476). The correlation is stronger for the top quartile of the Amish counties (rs = − 0.051, p < 0.05; N = 1869) compared to the bottom quartile (rs = 0.004; p > 0.05; N = 1869), although the correlation is not statistically significant for the bottom quartile of the Amish counties.
Note that the Spearman correlation is based on rank-transformed information from the data; the negative Spearman correlations between the Amish population and vaccination rate for the whole sample and the top quartile of the Amish counties suggests that the higher the counties rank in Amish population size, the lower they rank in the vaccination rate, and vice versa. Although the Spearman correlations are small, they do convey the message that the percentage of the Amish population would likely predict the vaccination rate at the county level. However, the Spearman correlations do not account for other covariates that could affect the vaccination rate. We performed negative binomial regression on the longitudinal data and included the aforementioned county-level socioeconomic and demographic characteristics. Table 2 shows the results for all Amish-populated counties and counties with an Amish population of more than 1%. We reported both the coefficients (\({\beta }_{i}\)) and the incidencerate ratios (\({e}^{{\beta }_{i}}\), or IRRs), an indicator representing the risk of exposure that enables easy comparison between two groups. The mean variance inflation factors (VIFs), an indicator of multicollinearity, are all below 1.5, suggesting no severe multicollinearity issues in the models. Using the overdisp (Fávero et al., 2020) command, we also tested for overdispersion, an assumption in negative binomial regression which refers to a situation where the variance of the response variable is greater than the mean (Cameron & Trivedi, 2013; Hinde & Demétrio, 1998). The results suggest that we could reject the hypothesis of no overdispersion in the data, making negative binomial regression an appropriate modeling approach.
The results suggest that higher percentages of Amish in a county significantly decrease the county-level vaccination rate while controlling for other covariates we would expect to also predict lower vaccination rates, such as political ideology, rural/non-rural status, household income, and evangelical Protestant affiliation. Specifically, on average, while holding all other variables constant in the model, we would expect a decrease of about 0.02% in COVID-19 vaccination rates as the percentage of Amish increase by 1 percent, a considerable drop when considering the average monthly vaccination rate was less than 0.1% in the selected counties. The regression results support our hypothesis that Amish affiliation independently predicts vaccine hesitancy.
To check for robustness, we ran a separate model, dropping counties with an Amish population below 1%. The direction and significance of the results were largely the same. We also conducted two sensitivity analyses to assess the robustness of previous models. First, we used the daily and weekly vaccination rates as the dependent variables and reran the negative binomial regression models, and the results were consistent across those models with daily, weekly, and monthly vaccination rates being the dependent variables (see Table 3 in Appendix A). Second, to overcome the possibility of overly complicating the study using panel data and various aggregation approaches, we took a simple and straightforward approach by selecting data from January 19, 2022, and performed a cross-sectional analysis. We selected this specific day as opposed to the most recent date because, for one, since October 20, 2022, the CDC started collecting weekly instead of daily vaccination data (Tin, 2022). For another, January 19, 2022, marks the day when there were the most COVID-19 cases since the outbreak of the pandemic. The results from the cross-sectional data analysis supported our main argument that the percentage of the Amish population tended to decrease the vaccination rate (see Table 4 in Appendix A).
Furthermore, in earlier analyses (available on request), we ran our models using 2010 Amish population data from the US Religion Census, effectively dropping the 10-and-under population from the 2020 analysis. Because Amish represent a high birth population, age distribution is skewed toward younger cohorts, who are less likely or unqualified to be vaccinated. The strength of 2010 and 2020 results were consistent, suggesting that the high percentage of Amish children is not misrepresenting the Amish as a whole.
Finally, a given county’s Amish population is almost always less than the county’s vaccinated population, and thus, it is possible most or all Amish are vaccinated. For example, if 50% of a county’s population is vaccinated and 10% of the county’s population is Amish, all Amish could be vaccinated. However, in two counties, the percentage of the county’s population that is Amish is higher than percentage of the population that is vaccinated. In 2020, Holmes County, Ohio’s population (44,004) was 44.76% Amish (19,696) but only 18.5% (8141) of its population were vaccinated as of October 26, 2022. In LaGrange County, Indiana, 43.43% of the population (40,119) was Amish (17,424) but only 23.2% (9308) were vaccinated. Even if the entire population of vaccinated in Holmes and LaGrange Counties was Amish, 58.67% (11,556) and 47.73% (8316) of the counties’ Amish populations, respectively, would still be unvaccinated, thus demonstrating that many Amish in these counties must be unvaccinated. This leads us to believe that Amish populations elsewhere are similarly undervaccinated.
Conclusions and Discussion
Using publicly available data and controlling for other variables, we have demonstrated that counties with sizable percentages of an Amish population tend to have disproportionately lower COVID-19 vaccination rates, suggesting that Amish people themselves have disproportionately lower COVID-19 vaccination rates. This finding supports our hypothesis that Amish are undervaccinated for COVID-19. As such, this study provides compelling evidence of Amish vaccine hesitancy toward COVID-19, adding evidence of Amish vaccine hesitancy more broadly. Among our control variables, voting Republican in the 2020 election and household income were significant in the expected directions: negatively and positively predicting vaccination rates, respectively. We were surprised that metro/non-metro status was not a significant predictor of vaccination rate. Evangelical affiliation was also not significant, though existing research is inconclusive about how and when evangelical affiliation predicts undervaccination.
This study’s findings support prior evidence that specific enclaves of Amish people are undervaccinated, in this case for COVID-19. Moving beyond localized studies in the literature, the findings here provide the first geographically broad and population-wide evidence that the Amish are undervaccinated for any particular vaccine. Though we believe it is a robust analysis, we realize our study has several limitations. First, our analysis of aggregated data is subject to the ecological fallacy, where conclusions and interpretations from a higher-level unit of analysis, such as the county level, do not apply to the individual level. Second, we have only empirically demonstrated that places with Amish populations have low COVID-19 vaccination rates; we have not demonstrated that the Amish people themselves are vaccine hesitant, though we have good reason to argue that position based on existing cultural research and ready availability of COVID-19 vaccines. Third, because there are relatively few large Amish settlements, our method reaches some limits, as we only find two cases where the Amish population is greater than the vaccination rate, meaning some Amish must be unvaccinated. Nevertheless, as the Amish population continues to grow and more places have sizeable Amish populations, we expect that the same relationship will be seen.
Public Perceptions of the Amish and Health Decision-Making
How have the Amish managed to collectively bypass COVID-19 vaccination? One strong possibility is in how they are perceived. Popular representations of the Amish have been largely positive (Boyer, 2008; Cong, 1994; Neuberger & Taman, 2014), even as critical representations do exist (Jolly, 2020; Völz, 2017). The preponderance of positive representations of the Amish—a people living in noble non-conformity—affords them some relief from pressure to conform to new norms, such as mass vaccination campaigns. In a particularly insightful study of health-related news coverage of an Ohio Amish measles outbreak, Fullenkamp (2021) demonstrated with two cases how “experts” not only socially construct “knowledge” but also “ignorance.” She showed how researchers, public health officials, and medical practitioners socially constructed the Amish as “unwillingly ignorant” about vaccination—“ignorant about their ignorance” because their “ignorance” was part and parcel of what media consumers interpreted as the separated lifestyle of the Amish; they were unaware of what they should know. As such, the Amish were not culpable for the measles outbreak, and health institutions felt responsible for providing education. Once health service providers educated the Amish, they were (purportedly) willing to comply; their “ignorance” about what they should know was overcome through public outreach. Fullenkamp compared this case to a simultaneous measles outbreak among “anti-vaxxer” parents visiting Disneyland. Media framed the parents as willfully “ignorant” and therefore irresponsible; the moral burden of the outbreak fell on parents, not health workers. In assigning culpability, health experts overlay moral dimensions on each population’s ignorance.
The Amish population has its share of heavy news consumers, and cohesive social networks serve to disseminate national and global news from these consumers. Based on this information, adherents rationalize their decision-making (Olshan, 1981), articulating diverse opinions (Kopecky & Hoiberg, 1994; Welk-Joerger, 2019) and internally managing both consensuses and prolonged disagreements (Anderson, 2019; Anderson & Potts, In press; Petrovich, 2017). With similar agency, they capably interact—whether as individuals or through group coordination—with non-Amish. Amish people’s involvement in North America’s participatory governments generally does not extend to office-holding, organized lobbying, campaigning, and other conspicuous forms of engaging the government—in fact, the absence of such direct involvement certainly bolsters the image of Amish as politically unproblematic (Rosenberg, 2020). However, they represent a powerful and relatively unified interest group capable of steering local and national policy (Olshan, 1990; Regehr, 1995), notably evidenced in a congressionally approved religious exemption from paying Social Security taxes (Glenn, 2001; McDevitt, 2010), a Supreme Court–sanctioned right to withhold their children from attending school beyond eighth grade (Bontrager, 2022; Peters, 2003), and the ability in some large Amish settlements to convince public school boards to create Amish-tailored but publicly funded programming (Howley et al., 2008; McConnell & Hurst, 2006; Thalheimer, 2021). At a local scale, Amish opinion leaders can effectively mobilize co-adherents’ sympathies for or against people—such as service providers and change agents—and severely enhance or curtail their ability to influence group thought and behavior (Bryan, 2016; Jolly, 2014b; Reiling & Nusbaumer, 1997). This evidence suggests that Amish people—though widely perceived as unproblematic and naïve, as intriguing and harmless—are engaging with national policy and politics through rationalized decisions to individually and collectively conform or resist and to strategically align with key stakeholders, even if in ways contrary to their own formal values (Kidder & Hostetler, 1990).
While service providers and policy-makers need not “balance out” the way Amish are positively represented with negative framing, they should reconfigure their perceptions of Amish people, as needed, from an innocently detached people to a people capable of rationalized decision-making who are engaging and steering public policy, even if indirectly. In this way, experts should approach the Amish population as they would any other ethnic, religious, or identity group: noting patterns and adjusting policy according to behavior. In the 2014 measles outbreak, the Amish likely accepted mass vaccination in part because press coverage—which did single out the Amish—suggested the Amish were not doing their part, and that they, in particular, were the focal point of this outbreak. The Amish experienced the public shame of being singled out as a people for causing a public health crisis.
Service and Policy Considerations
How, then, should public health providers and policy-makers promote healthcare innovations such as vaccinations to insular ethnic religious groups such as the Amish? Most of the published, peer-reviewed reports and research addressing effectiveness in professional healthcare work with the Amish offer micro-level advice through the multiculturalist-oriented cultural competency framework (Anderson & Potts, 2020). Cultural competency emphasizes personal knowledge of the population as the key to reducing barriers to service, which then unlocks effective service delivery. Indeed, personal knowledge of the population can help improve interactions—for example, clarifying communication, not offending, and better understanding considerations for decision-making. However, the seemingly endless lists of culturally competent interaction strategies and factoids can leave policy-makers and others with the impression that the group in question is a fragile and easily alienated population that struggles to interact outside of their own vacuum-sealed culture (Anderson & Potts, 2020). As such, cultural competency research seems to suggest—again, following Fullenkamp (2021)—that the Amish are ignorant about their ignorance, that Amish decision-making is unproblematic for society, and that, ultimately, culturally sensitive interactions initiated by service providers will improve cooperation. Regarding our present case, the cultural competency literature seems to suggest that Amish undervaccination is due to the population being “hard to reach” (Ozawa et al., 2019)—that is, cultural or tangible barriers can be reduced through cultural competency.
The effectiveness of cultural competency as a construct seems overstated. Amish people are as uncomfortable in unfamiliar social contexts—such as healthcare institutions—as anyone else. Additionally, many of the cultural competency-oriented recommendations for healthcare provider behavior sound a lot like what anyone would want: clarity in communications, trustworthiness, face-to-face time, and interactions in a warm and non-bureaucratic context (Anderson & Potts, 2020). Finally, cultural competency speaks only to micro-interactions and does not address macro-dynamics.
The cultural competency perspective might seem to promote community empowerment vis-à-vis the emphasis on sympathy and understanding, but it is a top-down strategy for diffusion and focuses on removing barriers to innovation adoption. Culturally sensitive efforts to increase vaccine availability and education might yield few results when Amish people do not feel like they “own” the innovation and decision. Because few Amish are credentialed health practitioners (a result of church proscriptions on secondary and post-secondary education), disparities can easily arise between the Amish population’s networks of knowledge (“our” knowledge) and healthcare establishments (“their” knowledge). Such disparities can be exacerbated when healthcare agents promote health resources to reduce perceived cultural barriers. Amish people might suspect ulterior, undisclosed motives—especially moves toward greater control and profit—hidden within programs from the government and large corporations (Anderson & Potts, 2020).
When a population is “hard to reach” (Ozawa et al., 2019), top-down approaches such as cultural competency might be preferred. However, given the ready availability of COVID-19 vaccines and the ways Amish people have rationalized non-adoption, we feel as if their undervaccination is likely due to Amish being “hard to vaccinate” (Ozawa et al., 2019)—that is, attitudinal and cultural reasons for undervaccination, as explained in point two in the background section of this paper. As such, service providers and policy-makers should consider bottom-up approaches to change, along with a view of the Amish population that places responsibility for their actions on them, not on health providers and policy-makers. With that approach, any barriers and boundaries effectively reduced are those that Amish people opt to reduce—they decide to approach policy-makers and service providers and ask for assistance solving a problem or else accept responsibility for undervaccination. That is to say, general policies and outreach efforts not specifically targeting the Amish but nevertheless changing their calculations might be more effective for society-wide vaccination efforts than targeting the Amish specifically, which might incite resistance. They must conclude on their own: “‘our’ ways, specifically, are causing ‘them’ injury.”
But can there be any real public harm to a failed top-down diffusion effort targeting the Amish? While public health policy-makers and service providers might consider any vaccination outreach effort as only resulting in vaccine uptake—even if just a sliver of a percentage increase—urgent, emergency efforts aimed at population-wide health practice adoption can have unintended backlash. In the panel discussion “The Plain People and COVID-19: Responses and Public Policy” at the July 2021 conference of the Amish & Plain Anabaptist Studies Association, pediatric geneticist Ethan Scott, who had just published a study of Holmes County, OH-area pre-COVID-19 Amish vaccination practices (Scott et al., 2021), suggested that the strong, politically polarized push for Americans to accept COVID-19 vaccines might be reducing Amish acceptance of other vaccines. We will reiterate his observation. Negative consequences of poorly received and population-targeted health messaging can reach further than just non-adoption of the new practice and extend to discontinuation of health practices already adopted. Policy makers and service providers should weigh out the risks of any top-down, targeted outreach strategies.
Variation in Vaccine Adoption
Even as our study suggests that Amish populations likely have lower COVID-19 vaccination rates, we caution service providers and policy-makers against assuming all Amish individuals are under- or unvaccinated. Though Amish people tend to develop dominant consensus on matters of interest, Amish culture is not homogeneous; varying health practices and outcomes are one sign of this diversity (Floersch et al., 1997). Even within very similar cultural settings, individuals might have intense opinions that differ one from another (e.g., Petrovich, 2017; Reiling, 2002; Thalheimer, 2021; Welk-Joerger, 2019). Additionally, the Amish do differ (increasingly) in class and material expenditures (Anderson & Autry, 2011; Choy, 2020; Moledina et al., 2014), and income/social class has been associated with COVID-19 vaccine acceptance in other populations (Hudson & Montelpare, 2021; Mollalo & Tatar, 2021). We thus emphasize that Amish identity should be considered an initial basis from which to probe vaccination attitudes and that Amish identity does not always mean vaccination hesitancy.
Future Directions
Populations with high undervaccination levels, such as the Amish, will continue to be of interest as practitioners respond to population-specific outbreaks. Ongoing inquiry is needed to understand how Amish peoplehood—including its religious, ethnic, and other components—provides a meaningful script for attitudes toward vaccination as well as why and how variation in Amish vaccination adoption occurs. This suggests a need for comprehensive, qualitative studies utilizing robust theories of health and health culture.
Data availability
Data and codes used for this study are available at https://github.com/shuai-zhou/AmishCovidVaccineAdoption.
Notes
Including LaGrange, Indiana (“Amish face barriers to COVID vaccines,” Elkhart Truth, April 3, 2021); Holmes, Ohio (“‘Not surprised’: Holmes County reporting lowest COVID-19 vaccination numbers in Ohio,” Fox 8, July 28, 2021); Osceola, Michigan (“Osceola County vaccination rate among the area's lowest,” Cadillac News, June 5, 2021); Clark, Wisconsin (“Vaccine hesitancy runs deep in rural Clark County, but efforts underway to reach out,” WPR, May 25, 2021); Todd, Minnesota (“Welcome to Todd County, where just 34% of people are vaccinated,” Minnesota Reformer, July 14, 2021); and the Kalona area of Iowa (“Shunning vaccines, Iowa Amish deal with COVID-19 as a community,” The Gazette, May 17, 2021).
Although we selected October 31, 2022, as the end date of this study, the actual date that reported COVID-19 vaccination before October 31, 2022, was October 26, 2022.
ARDA’s classification is guided by the RELTRAD scheme (that is, “Religious Traditions”) which aggregates religious denominations into broader religious families, including evangelical Protestant (Woodberry, Park, Kellstedt, Regnerus, & Steensland, 2012). Because RELTRAD places Amish into the evangelical Protestant tradition, for our calculations, we subtracted the Amish population from the total population of this category. Edmonson County, KY, was dropped from analysis as it impossibly reported 128.72% of the population as evangelical.
References
Agarwal, R., Dugas, M., Ramaprasad, J., Luo, J., Li, G., & Gao, G. (2021). Socioeconomic privilege and political ideology are associated with racial disparity in COVID-19 vaccination. Proceedings of the National Academy of Sciences, 118(33), e2107873118. https://doi.org/10.1073/pnas.2107873118
Albrecht, D. E. (2021). COVID-19 in Rural America: Impacts of politics and disadvantage. Rural Sociology, 87(1), 94–118.
Ali, H., Kondapally, K., Pordell, P., Taylor, B., Medina Martinez, G., Salehi, E., & Lloyd, S. (2020). COVID-19 outbreak in an amish community- Ohio, may 2020. Morbidity and Mortality Weekly Report, 69(45), 1671–1674.
Anderson, C. (2019). Of process, practice, and belief: What can we learn about old Amish church history and polity from this special issue’s source documents? Journal of Amish and Plain Anabaptist Studies, 7(2), 101–108.
Anderson, C., & Bacon, R. (2023). Profiles of Major Amish Settlements in North America: A Guide for Researchers and Service Providers. Journal of Amish and Plain Anabaptist Studies, 11(2).
Anderson, C. (2017). The undistinguished scholar of the Amish, Werner Enninger, -or- has the time yet come for rigorous theory in Amish studies? Journal of Amish and Plain Anabaptist Studies, 5(2), 196–238.
Anderson, C., & Kenda, L. (2015). What kinds of places attract and sustain Amish populations? Rural Sociology, 80(4), 483–511. https://doi.org/10.1111/ruso.12083
Anderson, C., & Potts, L. (2020). The amish health culture and culturally sensitive health services: an exhaustive narrative review. Social Science & Medicine, 265, 113466. https://doi.org/10.1016/j.socscimed.2020.113466
Anderson, C., & Potts, L. (2021). Research trends in Amish population health, a growing literature about a growing rural population. Journal of Rural Social Sciences, 36(1), 6.
Anderson, C., & Potts, L. (2022). Physical health conditions of the Amish and intervening social mechanisms: an exhaustive narrative review. Ethnicity & Health. https://doi.org/10.1080/13557858.2021.1968351
Anderson, C., & Potts, L. (In press). The Cultural and Religious Complexities of Amish-Focused Mental Health Conditions Research: Insights from an Exhaustive Narrative Review and Case Study of Counseling Controversies. Mental Health, Religion & Culture.
Anderson, S., & Autry, C. (2011). Leisure behaviour of the Amish. World Leisure Journal, 53(1), 57–66.
Bontrager, T. (2022). The Ramifications of Wisconsin v. Yoder: Six foundational problems with a 50-year old landmark case. Journal of Amish and Plain Anabaptist Studies, 10(1), 97–106.
Boyer, P. (2008). Understanding the Amish in twenty-first century America. Mennonite Quarterly Review, 82(3), 359–376.
Briss, P., Fehrs, L., Hutcheson, R., & Schaffner, W. (1992). Rubella among the Amish: resurgent disease in a highly susceptible community. Pediatric Infectious Disease Journal, 11(11), 955–959.
Bryan, E. (2016). The Amish beard cutting case: A defense lawyer’s perspective. Journal of Amish and Plain Anabaptist Studies, 4(1), 98–105.
Byfield, L. (2019). Labeling english learners: Teachers’ perceptions and implications. International Journal of Education & Literacy Studies, 7(4), 69–75.
Cameron, A. C., & Trivedi, P. K. (2013). Regression analysis of count data. Cambridge University Press.
CDC. (2022). CDC Museum COVID-19 Timeline. Retrieved from https://www.cdc.gov/museum/timeline/covid19.html
Choy, J. P. (2020). Religious rules as a means of strengthening family ties: Theory and evidence from the Amish. Journal of Comparative Economics, 48(3), 729–748. https://doi.org/10.1016/j.jce.2019.12.007
Cong, D. (1994). The roots of Amish popularity in contemporary USA. Journal of American Culture, 17(1), 59–66.
Conrad, P., & Barker, K. K. (2010). The social construction of illness: key insights and policy implications. Journal of Health and Social Behavior, 51(1), 67–79. https://doi.org/10.1177/0022146510383495
Corcoran, K. E., Scheitle, C. P., & DiGregorio, B. D. (2021). Christian Nationalism and COVID-19 Vaccine Hesitancy and Uptake. Vaccine, 39(45), 6614–6621. https://doi.org/10.1016/j.vaccine.2021.09.074
Coxe, S., West, S. G., & Aiken, L. S. (2009). The analysis of count data: A gentle introduction to Poisson regression and its alternatives. Journal of Personality Assessment, 91(2), 121–136.
Cross, H. (1976). Population studies and the Old Order Amish. Nature, 262(5563), 17–20.
Crowley, W. (1978). Old order amish settlement: Diffusion and growth. Annals of the Association of American Geographers, 68(2), 249–264.
De Winter, J. C., Gosling, S. D., & Potter, J. (2016). Comparing the Pearson and Spearman correlation coefficients across distributions and sample sizes: A tutorial using simulations and empirical data. Psychological Methods, 21(3), 273–290.
Dhakal, S., Wang, L., Antony, L., Rank, J., Bernardo, P., Ghimire, S., & Renukaradhya, G. (2019). Amish (Rural) vs. non-Amish (Urban) Infant fecal microbiotas are highly diverse and their transplantation lead to differences in mucosal immune maturation in a humanized germfree piglet model. Frontiers in Immunology. https://doi.org/10.3389/fimmu.2019.01509
Donnermeyer, J., Anderson, C., & Cooksey, E. (2013). The Amish population: county estimates and settlement patterns. Journal of Amish and Plain Anabaptist Studies, 1(1), 72–109.
Duran, D., Jack, S., Medina-Martinez, G., Pearson, M., Oliveira, S., & Campbell, E. (2020). Community Assessment of COVID-19, Elkhart County, IN. Retrieved from
Ems, L. (2022). Virtually Amish: Preserving community at the internet’s margins. MIT Press.
Enninger, W., & Raith, J. (1982). An Ethnography-of-Communication Approach to Ceremonial Situations. A Study on Communication in Institutionalized Social Contexts: The Old Order Amish Church Service. Wiesbaden, Germany: Franz Steiner Verlag.
Enninger, W. (1984). On the role of artifactual signification and communication in the organization of speaking. Papers in Linguistics, 17(1–4), 53–88.
Enninger, W. (1986). The theme of ethnicity in the literature of the Old Order Amish. In W. Enninger (Ed.), Studies on the languages and the verbal behavior of the Pennsylvania germans I (pp. 115–136). Franz Steiner Verlag Wiesbaden GMBH.
Enninger, W. (1988a). Coping with modernity: instrumentally and symbolically, with a glimpse at the Old order amish. Brethren Life and Thought, 33(3), 154–170.
Enninger, W. (1988b). The Social Construction of Past, Present, and Future in the Written and Oral Texts of the Old Order Amish: An Ethno-Semiotic Approach to Social Belief. In F. Poyatos (Ed.), Literary Anthropology (pp. 195–256). Amsterdam, Netherlands: Benjamins.
Enninger, W., & Wandt, K.-H. (1979). Social roles and language choice in an old order Amish community. Sociologia Internationalis, 17, 111–133.
Farrar, H., Kulig, J., & Sullivan-Wilson, J. (2018). Older adult caregiving in the amish: An integrative review. Journal of Cultural Diversity, 25(2), 54–65.
Fávero, L. P., Belfiore, P., Santos, M., & Souza, R. F. (2020). Overdisp: A stata (and mata) package for direct detection of overdispersion in poisson and negative binomial regression models. Statistics, Optimization and Information Computing, 8, 773–789.
Floersch, J., Longhofer, J., & Latta, K. (1997). Writing Amish culture into genes: Biological reductionism in a study of manic depression. Culture, Medicine, and Psychiatry, 21(2), 137–159.
Freudenburg, M., Lutz, M., & Radermacher, M. (2020). Gospels of prosperity and simplicity. Assessing variation in the protestant moral economy. Interdisciplinary Journal of Research on Religion., 16, 8.
Friesen, B., & Friesen, J. (1996). Perceptions of the Amish Way. Dubuque, IA: Kendall/Hunt.
Fullenkamp, N. K. (2021). Playing russian roulette with their kids: experts’ construction of ignorance in the California and Ohio measles outbreaks. Social Science & Medicine, 272, 113704. https://doi.org/10.1016/j.socscimed.2021.113704
Garrett-Wright, D., Main, M. E., & Jones, M. S. (2016). Anabaptist Members’ Perceptions and Preferences Related to Healthcare. Journal of Amish and Plain Anabaptist Studies, 4(2), 187–200.
Gastañaduy, P., Budd, J., Fisher, N., Redd, S., Fletcher, J., Miller, J., & DiOrio, M. (2016). A measles outbreak in an underimmunized Amish community in Ohio. New England Journal of Medicine, 375(14), 1343–1354. https://doi.org/10.1056/NEJMoa1602295
Glenn, B. (2001). Collective precommitment from temptation: The Amish and social security. Rationality and Society, 13(2), 185–204.
Glover, C. (2015). A Mathematical Model of the 2014 Ohio Measles Outbreak to Assess the Effectiveness of the Public Health Response. (M.S.), Ohio State University, Columbus, OH.
Graybill, B. (2022). Ethnography and Plain Anabaptist Women: Some Considerations on Positionality, Power, and Pandemic. Journal of Amish and Plain Anabaptist Studies, 10(1), 77–89.
Hartman, J. (2001). Power under the cover of tradition: A case of a ‘plain community.’ In B. Redekop & C. Redekop (Eds.), Power, Authority, and the Anabaptist Tradition (pp. 115–135). Johns Hopkins University Press.
Hawley, J., & Hamilton, J. (1996). Retail entrepreneurial values in a bicultural community: Cultural and economic contentions and negotiation. Journal of Socio-Economics, 25(6), 639–661.
Hess, R. (2017). Amish-initiated burn care project: case report and lessons learned in participatory research. Journal of Transcultural Nursing, 28(2), 212–219. https://doi.org/10.1177/1043659615613417
Hess, R. (2018). Amish and Mennonite lay caregivers’ experiences using the b&w burdock leaf treatment on burns and wounds: A qualitative study. Journal of Amish and Plain Anabaptist Studies, 6(2), 144–159.
Hinde, J., & Demétrio, C. G. B. (1998). Overdispersion: Models and estimation. Computational Statistics and Data Analysis, 27(2), 151–170.
Hopple, C. L. (1981). Germanic European origins and geographical history of the Southeastern Pennsylvania Amish. Pennsylvania Folklife, 31(2), 69–86.
Howley, A., Howley, C., Burgess, L., & Pusateri, D. (2008). Social class, Amish culture, and an Egalitarian Ethos: Case study from a rural school serving Amish children. Journal of Research in Rural Education, 23(3), 1–12.
Hudson, A., & Montelpare, W. J. (2021). Predictors of vaccine hesitancy: Implications for COVID-19 public health messaging. International Journal of Environmental Research and Public Health, 18(15), 8054.
Jackson, B., Payton, T., Horst, G., Halpin, T., & Mortensen, B. K. (1993). An epidemiologic investigation of a Rubella outbreak among the Amish of Northeast Ohio. Public Health Repository, 108(4), 436–439.
Jeong, S. (2013). The role of social capital for Amish entrepreneurs in pursuing informal economic opportunities. Journal of Amish and Plain Anabaptist Studies, 1(1), 127–168.
Jolly, N. (2014a). Amish femininity: New lessons from the Old Order. Journal of the Motherhood Initiative, 5(2), 75–89.
Jolly, N. (2014b). In this world but not of it: Midwives, Amish, and the politics of power. Sociological Research Online, 19(2), 1–10.
Jolly, N. (2017). Birthing new kinships: The cross-pollinating potential of Amish health research. Journal of Amish and Plain Anabaptist Studies, 5(2), 147–161.
Jolly, N. (2020). Hemmed In? considering the complexities of Amish womanhood. Journal of Amish and Plain Anabaptist Studies, 8(2), 159–168.
Kettunen, C., Nemecek, J., & Wenger, O. (2017). Evaluation of low immunization coverage among the Amish population in rural Ohio. American Journal of Infection Control, 45(6), 630–634. https://doi.org/10.1016/j.ajic.2017.01.032
Khubchandani, J., Sharma, S., Price, J. H., Wiblishauser, M. J., Sharma, M., & Webb, F. J. (2021). COVID-19 Vaccination hesitancy in the United States: A Rapid national assessment. Journal of Community Health, 46(2), 270–277. https://doi.org/10.1007/s10900-020-00958-x
Kidder, R., & Hostetler, J. (1990). Managing ideologies: Harmony as ideology in Amish and Japanese societies. Law and Society Review, 24(4), 895–922.
Kopecky, K., & Hoiberg, E. (1994). Conflict: A mainspring of Amish society. Pennsylvania Folklife, 43(3), 111–114.
Landing, J. (1970). Amish population changes, 1947–1964. Mennonite Historical Bulletin, 31(4), 4.
Liu, H., Davidson, R. A., Rosowsky, D. V., & Stedinger, J. R. (2005). Negative binomial regression of electric power outages in hurricanes. Journal of Infrastructure Systems, 11(4), 258–267.
Long, S. (2022). Attitudes toward transgenic corn usage among Amish & Conservative Mennonite farmers in Ohio. Journal of Amish and Plain Anabaptist Studies, 10(1), 61–76.
Longhofer, J. (1994). Nursing home utilization: A comparative study of the Hutterian Brethren, the Old Order Amish, and the mennonites. Journal of Aging Studies, 8(1), 95–120.
Luthy, D. (1986). The Amish in America: Settlements that failed, 1840–1960. Pathway Publications.
Lutz, M. (2017). Explaining anabaptist persistence in the market economy: Past paradigms and new institutional economics theory. Journal of Amish and Plain Anabaptist Studies, 5(2), 239–257.
Mann, S., Christini, K., Chai, Y., Chang, C.-P., Hashibe, M., & Kepka, D. (2022). Vaccine hesitancy and COVID-19 immunization among rural young adults. Preventive Medicine Reports, 28, 101845. https://doi.org/10.1016/j.pmedr.2022.101845
Martin, P. L. (2021). Penn state extension services and plain people: An inside perspective on a trust-based relationship. Journal of Amish and Plain Anabaptist Studies, 9(2), 221–231.
McConnell, D., & Hurst, C. (2006). No “Rip Van Winkles” Here: Amish Education since Wisconsin v. Yoder. Anthropology and Education Quarterly, 37(3), 236–254.
McDevitt, B. (2010). Amish Tax Case, New Wilmington, Pa. Western Pennsylvania Historical Magazine(Summer), 18–19.
Medina-Marino, A., Reynolds, D., Finley, C., Hays, S., Jones, J., & Soyemi, K. (2013). Communication and mass vaccination strategies after pertussis outbreak in rural Amish communities—Illinois, 2009–2010. Journal of Rural Health, 29(4), 413–419. https://doi.org/10.1111/jrh.12019
Meyers, T. (1994). The Old Order Amish: To remain in the faith or to leave? Mennonite Quarterly Review, 68(3), 378–395.
Miller-Fellows, S. C., Adams, J., Korbin, J. E., & Greksa, L. P. (2018). Creating culturally competent and responsive mental health services: A case study among the Amish population of Geauga County, Ohio. Journal of Behavioral Health Services & Research, 45(4), 627–639. https://doi.org/10.1007/s11414-018-9612-0
Moledina, A., McConnell, D., Sugars, S., & Connor, B. (2014). Amish economic transformations: New forms of income and wealth distribution in a traditionally “flat” community. Journal of Amish and Plain Anabaptist Studies, 2(1), 1–22.
Mollalo, A., & Tatar, M. (2021). Spatial modeling of COVID-19 vaccine hesitancy in the United States. International Journal of Environmental Research and Public Health, 18(18), 9488.
Mueller, J. T., McConnell, K., Burow, P. B., Pofahl, K., Merdjanoff, A. A., & Farrell, J. (2020). Impacts of the COVID-19 pandemic on Rural America. Proceedings of the National Academy of Sciences of the United States of America, 118(1), 2019378118.
Nagar, S., & Ashaye, T. (2022). A shot of faith—analyzing vaccine hesitancy in certain religious communities in the United States. American Journal of Health Promotion, 36(5), 765–767. https://doi.org/10.1177/08901171211069547
Neuberger, B., & Taman, K.-M. (2014). The image of the Amish in the New York Times versus the image of the Haredim in Haaretz (1980–2010). Conflict and Communication Online, 13(1), 1–17.
Olshan, M. (1981). Modernity, the folk society, and the Old Order Amish: An alternative interpretation. Rural Sociology, 46(2), 297–309.
Olshan, M. (1990). The Old Order Amish steering committee: A case study in organizational evolution. Social Forces, 69(2), 603–616.
Ozawa, S., Yemeke, T. T., Evans, D. R., Pallas, S. E., Wallace, A. S., & Lee, B. Y. (2019). Defining hard-to-reach populations for vaccination. Vaccine, 37(37), 5525–5534. https://doi.org/10.1016/j.vaccine.2019.06.081
Park, K. (2018). Interpreting Non-Amish perceptions of the Old Order Amish using cultural relativism and human rights frameworks. Journal of Amish and Plain Anabaptist Studies, 6(1), 117–143.
Paul, E., Steptoe, A., & Fancourt, D. (2021). Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. The Lancet Regional Health - Europe, 1, 100012. https://doi.org/10.1016/j.lanepe.2020.100012
Peters, S. F. (2003). The Yoder case: religious freedom, education, and parental rights. University Press of Kansas.
Petrovich, C. (2013). Spiritual theology in an Amish key: Theology, scripture, and praxis. Journal of Spiritual Formation & Soul Care, 6, 229–254.
Petrovich, C. (2017). More than forty Amish affiliations? Charting the fault lines. Journal of Amish and Plain Anabaptist Studies, 5(1), 120–142.
Petrovich, C. (2022a). Amish ecclesiology: Plural-Elder congregationalism, governing lines of fellowship, and envisioning the Church. Ecclesiology, 18(3), 297–318. https://doi.org/10.1163/17455316-18030004
Petrovich, C. (2022b). Reading, interpreting, and applying Christian scripture in Amish communities. Mennonite Quarterly Review, 96(4), 503–529.
Quinn, J., Kruse, J., Nwadike, L., Piñero, J. C., & Trinklein, D. (2021). The success of plain people’s produce auctions and partnership with Missouri extension. Journal of Amish and Plain Anabaptist Studies, 9(2), 177–190.
Regehr, T. D. (1995). Relations between the Old Order Amish and the state in Canada. Mennonite Quarterly Review, 69(2), 151–177.
Reiling, D. (2002). Managing the ‘Marginalized’ man: fieldwork, boundaries, and ethics of involvement. Journal of Multicultural Nursing & Health, 8(3), 15–20.
Reiling, D., & Nusbaumer, M. (1997). The Amish drug task force: A natural history approach to the construction of a social problem. Journal of Multicultural Nursing & Health, 3(2), 25–37.
Reschly, S. (2000). The Amish on the Iowa Prairie: 1840–1910. Johns Hopkins University Press.
Rosenberg, E. (2020). Amish and Hasidic litigation: A survival strategy. Journal of Church and State, 63(3), 485–505. https://doi.org/10.1093/jcs/csaa060
Rountzounis, J., Cohen, B., Joy, A., & Cook, R. (1968). Pockets of high fertility in the United States. Population Bulletin, 24(2), 25–55.
Roy, D. N., Biswas, M., Islam, E., & Azam, M. S. (2022). Potential factors influencing COVID-19 vaccine acceptance and hesitancy: A systematic review. PLoS ONE, 17(3), e0265496.
Rumsey, S. K. (2010). Faith in action: Heritage literacy as a synchronisation of belief, word, and deed. Literacy, 44(3), 137–143.
Rumsey, S. (2016). Coming of age: Amish heritage literacy practices of rumspringa, adult baptism, and shunning. In V. Lytra, D. Volk, & E. Gregory (Eds.), Navigating languages, literacies and identities: Religion in young lives (pp. 56–68). Routledge.
Sauder, M. (2020). Choosing whom to trust: Autonomy versus reliance on others in medical decision making among plain Anabaptists. Journal of Amish and Plain Anabaptist Studies, 8(1), 59–64.
Schlegel, C. (1997). AM fire and storm (Insurance): Simplicity in a strongly Amish institution. Mennonite Quarterly Review, 71(3), 365–376.
Scott, E. M., Stein, R., Brown, M. F., Hershberger, J., Scott, E. M., & Wenger, O. K. (2021). Vaccination patterns of the Northeast Ohio Amish revisited. Vaccine, 39(7), 1058–1063. https://doi.org/10.1016/j.vaccine.2021.01.022
Sharpnack, P., Quinn Griffin, M., Benders, A., & Fitzpatrick, J. (2010). Spiritual and alternative healthcare practices of the Amish. Holistic Nursing Practice, 24(2), 64–72.
Škender, V. (2020). Flesh, freundschaft, and fellowship: Towards a holistic model of the Amish kinship system. Journal of Amish and Plain Anabaptist Studies, 8(1), 1–22.
Smith, C., & Emerson, M. (1998). American evangelicalism: Embattled and thriving. University of Chicago Press.
Stein, M. M., Hrusch, C. L., Gozdz, J., Igartua, C., Pivniouk, V., Murray, S. E., & Sperling, A. I. (2016). Innate immunity and asthma risk in Amish and Hutterite farm children. New England Journal of Medicine, 375(5), 411–421. https://doi.org/10.1056/NEJMoa1508749
Thalheimer, S. (2021). A little more in the world: Why Amish parents choose to send their children to public schools. Journal of Amish and Plain Anabaptist Studies, 9(1), 27–54.
Tin, A. (2022). CDC ends daily reporting of COVID case and death data, in shift to weekly updates. CBS news. Retrieved from https://www.cbsnews.com/news/covid-19-cases-deaths-cdc-ends-daily-reporting-weekly-updates/
Viswanath, K., Bekalu, M., Dhawan, D., Pinnamaneni, R., Lang, J., & McLoud, R. (2021). Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health, 21(1), 818. https://doi.org/10.1186/s12889-021-10862-1
Völz, S. (2017). Towards “New Memoir”: Ira Wagler’s Ex-Amish life narrative growing up Amish. American Studies Journal. https://doi.org/10.18422/63-06
Wasao, S., Anderson, C., & Mpody, C. (2021). The persistently high fertility of a North American population: a 25-year restudy of parity among the Ohio Amish. Population Studies, 75(3), 477–486. https://doi.org/10.1080/00324728.2021.1883725
Welk-Joerger, N. (2019). Restoring eden in the Amish anthropocene. Environmental Humanities, 11(1), 72–100. https://doi.org/10.1215/22011919-7349418
Welk-Joerger, N. (2021). Performing Amish agrarianism: negotiating tradition in the maintenance of Pennsylvania dairy farms. Journal of Amish and Plain Anabaptist Studies, 9(2), 125–140.
Wenger, O., McManus, M., Bower, J., & Langkamp, D. (2011). Underimmunization in Ohio’s Amish: parental fears are a greater obstacle than access to care. Pediatrics, 128(1), 79–85. https://doi.org/10.1542/peds.2009-2599
Westman, J., Ferketich, A., & Kauffman, R. (2010). Low cancer incidence rates in Ohio Amish. Cancer Causes and Control, 21(1), 69–75.
Woodberry, R. D., Park, J. Z., Kellstedt, L. A., Regnerus, M. D., & Steensland, B. (2012). The measure of American religious traditions: Theoretical and measurement considerations. Social Forces, 91(1), 65–73.
Yoder, J., & Dworkin, M. (2006). Vaccination usage among an Old-Order Amish community in Illinois. Pediatric Infectious Disease Journal, 25(12), 1182–1183.
Funding
This research is supported in part by the Population Research Institute at Pennsylvania State University, which is supported by an infrastructure grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2CHD041025) and Social Environments and Population Health (T32HD007514) training grant, and USDA National Institute of Food and Agriculture and Multistate Research Project #PEN04623 (Accession #1013257). Further support was provided by a seed grant from the NIA-supported Interdisciplinary Network on Rural Population Health and Aging. Financial supporters had no role in the study design; collection, analysis, and interpretation of the data; writing the report; and the decision to submit for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Anderson, C., Zhou, S. & Chi, G. Population-Wide Vaccination Hesitancy among the Amish: A County-Level Study of COVID-19 Vaccine Adoption and Implications for Public Health Policy and Practice. Popul Res Policy Rev 42, 70 (2023). https://doi.org/10.1007/s11113-023-09816-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11113-023-09816-9