Abstract
Background and objectives
Marked changes in the hypothalamic-pituitary axis have been documented in patients with traumatic brain injury (TBI). These enduring endocrine challenges could significantly influence the physical and psychological outcomes thereby impacting overall recovery. This study aimed to determine the prevalence and types of endocrine dysfunction in men with chronic TBI and to determine the association of endocrine dysfunction with clinical outcomes.
Methodology
A cross-sectional study that included male participants of 25–45 years (N = 66) with moderate to severe TBI within 6–24 months of injury. Serum Cortisol, Free T4, TSH, Luteinizing hormone, Testosterone, ACTH, Prolactin and IGF-1 were assessed. Glasgow Outcome Scale Extended (GOS-E) and Modified Barthel Index (MBI) scores were also assessed in them.
Results
The study cohort comprised male patients with a mean ± age of 32.8 ± 5.7 years. Low IGF-1 levels were most commonly encountered, followed by hypogonadism. Hypopituitarism was present in 56.1%. The proportion of hypogonadism was significantly higher in the group with moderate-total dependence (13/26) as compared to the functionally independent (8/40) group (50% vs. 20%; P = 0.011). Univariate and multivariate logistic regression analysis was used to determine the factors associated with hypopituitarism, revealing that severity of injury (OR = 2.6;) and GOS-E (OR = 3.1) were significant (P < 0.10) on univariate analysis.
Conclusions
This study emphasizes the need to screen TBI patients for neuroendocrine dysfunction during the chronic phases and to establish screening criteria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic brain injury (TBI) is a leading cause of death and disability, particularly among young men. According to global statistics from the Centres for Disease Control and Prevention (CDC), road traffic accidents (RTA) alone resulted in the loss of 1.35 million lives [1]. Every day, nearly 3,700 lives are lost worldwide due to road traffic crashes. Within this alarming statistic, the age group most severely impacted is 5–29 years old, constituting a staggering 73% of total accidental deaths. It is noteworthy that over 90% of road traffic fatalities occur in low- and middle-income countries [1].
According to present data, a significant proportion of TBI patients, ranging from 20 to 50%, experience some level of pituitary dysfunction during the acute phase following the injury. Notably, in most cases, this dysfunction is transient [2]. Hypopituitarism contributes to substantial morbidity and mortality in affected patients, and it may be underdiagnosed, causing delayed recovery. Individuals with TBI may also have heightened skeletal fragility due to prolonged immobilization and metabolic changes [3]. Other features include lethargy, memory disturbances, depression, irritability, insomnia, and diminished libido [4]. These multifaceted effects significantly impact the quality of life (QoL), leading to substantial functional limitations and long-term neurological impairments. Gasco et al. identified a robust association between pituitary dysfunction and adverse cognitive outcomes, encompassing memory, attention, and language [5]. It has been documented that the implementation of hormone replacement therapy results in substantial improvements in QoL, cognitive deficits, and functional independence. This underscores the critical importance of early diagnosis and intervention in addressing endocrine dysfunction.
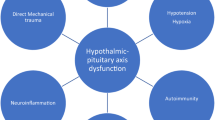
In a comprehensive systematic review, Schneider et al. documented a prevalence of 27.5% for hypopituitarism following TBI, wherein anterior pituitary dysfunction displayed a notable range spanning from 15–68% [6]. The pathophysiology of hypopituitarism subsequent to TBI is multifaceted, stemming from factors including damage to the pituitary stalk, ischemia/infarction of the pituitary gland as a primary cause, and secondary factors such as hypoxia, hypotension, and increased intracranial pressure [7]. Consequently, comprehensive screening for hypopituitarism in all patients with TBI is imperative. However, the impact of neuroendocrine deficiencies on clinical outcomes in TBI remains understudied, particularly using Modified Barthel Index (MBI) scores and Glasgow Outcome Scale Extended (GOS-E), which are pivotal for assessing rehabilitation progress and overall recovery. The prevalence of neuroendocrine dysfunction varies, influenced by factors such as the duration since injury, the nature of the injury, and variations in normal hormonal assays across studies [8].
Notably, the routine inclusion of endocrine function evaluation in the TBI rehabilitation protocol is lacking in the Indian scenario, leading to a significant proportion of TBI patients remaining undiagnosed and untreated for neuroendocrine dysfunction. Moreover, in India road traffic accidents (RTA) are more common in young males aged 25–45 years as compared to females in their most productive years. Since this age group represents the most productive individuals, with many of them being the sole breadwinners of their families, it’s important to identify any hormonal dysfunction related to traumatic brain injury that may hinder their ability to resume normal daily activities. Timely identification and intervention for endocrine abnormalities post-TBI hold the potential to enhance the rehabilitation process, aligning with the overarching goals of minimizing impairments, optimizing functional independence, and successfully reintegrating patients into the community. Furthermore, understanding the type and frequency of hormonal abnormalities will help in developing ethnicity-specific screening protocols that can aid in the early detection of these abnormalities Thus, in this study, we aimed to assess the prevalence and types of neuro-endocrine challenges in Indian men with chronic TBI assessed at 6 to 24 months post-injury and correlate these findings with clinical outcomes.
Methodology
This prospective cross-sectional study was conducted in the Physical Medicine and Rehabilitation Department of a tertiary care teaching hospital in southern India, following approval from the Institutional Ethical Committee (IRB No. 12670/dated 10.3.2020). The study period was from June 2020 to August 2021. This study conforms to all Strengthening the Reporting of Observational Studies in Epidemiology guidelines and reports the required information accordingly.
Selection of participants
A total of 66 participants with TBI were enrolled in this study based on specific inclusion criteria: male individuals aged 25–45 years, presenting with moderate or severe TBI, and attending outpatient clinics or undergoing rehabilitation in the inpatient wards of the Department of Physical Medicine and Rehabilitation, 6–24 months post-injury, after obtaining informed consent. We included males in the working age group in the sample to ensure a more uniform representation. RTA was particularly common among young males aged 25–45 in our study population, compared to females, especially during their most productive years. Exclusions comprised individuals with mild TBI, injury duration less than 6 months and more than 24 months, age less than 25 years and more than 45 years at the time of testing, chronic illnesses (CKD, CLD), active malignant tumors, patients on glucocorticoids, those with prior history of endocrine dysfunction, drugs affecting hypothalamic-pituitary function, those who had acquired SARS-CoV2 infection, patients in vegetative state and patients unwilling to participate in the study.
Assessment
A comprehensive history of pituitary hormonal hypofunction was meticulously collected, accompanied by relevant clinical examinations. The hormonal levels of all participants were thoroughly evaluated by conducting hormonal assays on their somatotropic, adrenal, thyroid, and gonadal axes.
Early morning fasting blood samples, obtained before 8:30 am, were analysed for anterior pituitary and their target hormones, including 8 am cortisol, free T4 (fT4), TSH, Luteinizing hormone (LH), Testosterone, ACTH (iced sample), Prolactin (in dilution), and Insulin-like growth factor-1 (IGF-1). The posterior pituitary axis was evaluated by daily monitoring of 24-hour urine input-output and serum electrolytes to check for diabetes insipidus.
Biochemistry
Serum levels of 8 am cortisol (N:16–25 mcg/dL), ACTH (N: 0–46 pg/mL), fT4 (N: 0.89–1.76 ng/dL), total T4 (N: 4.5–10.9 mcg/dL), TSH (N: 0.55–4.78 µIU/mL), Testosterone (N: 280–1000 ng/dL), LH (N: 0.8–7.6 µIU/mL), Prolactin (N: 2.1-17.7ng/mL) and age specified IGF-1 were analysed in the Department of Biochemistry using electrochemiluminescence method. Table 1 shows the hormone measurements and the analytical methods used to measure serum hormones.
Definitions
Serum 8 am cortisol levels were categorized into normal (16-25mcg/dl), borderline (4-15mcg/dl), and low cortisol levels (< 4mcg/dl) [9, 10]. Individuals with borderline cortisol levels underwent a validated ACTH stimulation test [11]. In this test, 25 units of Acton Prolongatum was intramuscularly injected over the deltoid region, followed by venous blood sampling for serum cortisol levels after 1 h. Cortisol levels less than 18 mcg/dL were considered indicative of hypocortisolemia, leading to initiation of long-term steroid supplementation. A cortisol level of ≥ 18 mcg/dL post ACTH stimulation confirmed the integrity of the pituitary-adrenal axis [12]. Central hypothyroidism was characterized by low T4/fT4 with normal or low TSH, while primary hypothyroidism exhibited low T4/fT4 with elevated TSH levels [10]. Subclinical hypothyroidism is characterized by a serum TSH above the upper reference limit combined with normal free thyroxine (T4) [13]. Subclinical hyperthyroidism is defined as a low or undetectable serum TSH with values within the normal reference range for both T3 and free T4 [14]. As growth hormone stimulation tests were not performed, individuals with IGF-1 levels below the age and gender-specified normative range were defined as having ‘low IGF-1 levels [15]. Hypogonadism is characterized by low morning serum total and/or free testosterone levels combined with symptoms and signs of testosterone deficiency [16]. Hyperprolactinemia is confirmed by a single measurement of serum prolactin levels above the upper limit of normal [17].
Functional status and outcomes
The functional status was evaluated utilizing the previously validated MBI, while global outcomes were assessed using the GOS-E. Administered by the principal investigator, these instruments are recognized for their reliability. The MBI, innovatively developed by Shah et al., demonstrates heightened sensitivity, offering nuanced insights into functional independence and limitations [18].
MBI is employed to assess performance in activities of daily living (ADL), providing a total score ranging from 0 to 100, with higher scores indicative of enhanced independence. It facilitates the evaluation of functional independence across 10 activities, encompassing feeding, bathing, grooming, dressing, bowel and bladder management, toilet use, transfers, mobility, and the use of stairs. MBI categorizes individuals into six levels of dependence based on their scores: total dependence (0–20), severe dependence (21–60), moderate dependence (61–90), slight dependence (91–99), and complete independence (100).
In contrast, the GOS-E demonstrates a more robust correlation with neuropsychological and psychosocial outcomes [19]. Utilized for the assessment of global outcome and independence, it categorizes patients into eight distinct groups: dead(D), vegetative state (VS), lower severe disability (SD-), upper severe disability (SD+), lower moderate disability (MD-), upper moderate disability (MD+), lower good recovery (GR-) and upper good recovery (GR+) [20].
For analysis in this study, the MBI was categorized into two groups: moderate to total dependence (0–90) and slight dependence to complete independence (91–100). Additionally, the GOS-E was divided into two categories: severe and moderate disability grouped together, and the other category represented good recovery.
Data analysis and statistics
Statistical analysis was done to calculate the prevalence and types of endocrine dysfunction in TBI patients and to study the association with functional status, severity of brain injury, and duration since the injury. Continuous variables were compared using the t-test. Categorical variables were presented as numbers and percentages. Chi-square test was used to test the association between the categorical variables. Bivariate correlations between two continuous variables were assessed using Pearson’s or Spearman’s correlation test as appropriate. Univariate and multivariate logistic regression analysis was used to study factors that were significantly associated with hypopituitarism in which a P-value of < 0.10 was considered significant for univariate analysis. For all other comparisons a two-tailed P-value of < 0.05 were considered significant. The statistical programs SPSS version 22 and Stata IC version 16 were used for data analysis.
Results
Study subjects and injury characteristics
A flow-diagram depicting patient recruitment and inclusion is shown in Fig. 1. The study cohort comprised 66 male patients aged 25–45 years, with a mean ± age of 32.8 ± 5.7 years. Comorbidities were present in 14% of patients and including diabetes mellitus, hypertension and psychiatric illness. RTA (86.4%) were the predominant cause of injury, followed by falls (10.6%). Focal injuries were identified in 69.6% of patients, with cranial fractures being the most prevalent, followed by subdural hematomas and contusions. Based on the initial Glasgow Coma Scale (GCS), 36 patients (54.5%) exhibited severe head injuries with GCS ranging from 3 to 8, while 30 patients (45.4%) had moderate injuries with GCS between 9 and 12. Patient and injury characteristics are detailed in Table 2.
Clinical outcomes
According to the GOS-E scores, 54 patients (81.8%) fell into the severe-moderate disability group, whereas 12 patients (18.2%) achieved a classification of good recovery. In terms of the MBI scores, 26 patients (39.4%) demonstrated dependency in ADL, while 40 patients (60.6%) exhibited independence in these activities.
Neuroendocrine dysfunction
The median duration since injury at which hormonal tests carried out (at a single time point) was 13 (6–24) months. 50% of patients (33) exhibited neuroendocrine-related symptoms, predominantly low mood, loss of appetite, and fatigue. Notably, 14 patients (58.3%) displayed symptoms despite normal laboratory findings pertaining to pituitary function, while 23 patients (54.8%) had abnormal hormonal results without apparent symptoms. The mean values (± SD) of various hormones analysed are presented in Table 1.
Hypothalamic-pituitary adrenal axis
Borderline cortisol levels (4–15 µg/dl) were identified in 34 patients (51.5%). Among these, 33 patients exhibited a favorable response following the ACTH stimulation test, whereas one patient displayed an inadequate cortisol response to Inj. Acton Prolongatum and was initiated on glucocorticoid replacement. Notably, ACTH levels were within the normal range for all 66 patients.
Hypothalamic-pituitary thyroid axis
Among the 66 patients, 3 (4.5%) exhibited central hypothyroidism, another 3 (4.5%) had primary hypothyroidism which were newly detected, and an additional 3 (4.5%) presented with mild subclinical hypothyroidism. One patient (0.2%) displayed biochemical evidence of subclinical hyperthyroidism, requiring ongoing follow-up. Those detected to have central or primary hypothyroidism were initiated on levothyroxine supplements.
Hypothalamic-somatotroph axis
Low concentrations of IGF-I were observed in 24 patients (36.36%) with TBI, possibly indicative of growth hormone deficiency, and notably, this constituted the most frequently encountered endocrine abnormality in the study cohort.
Hypothalamic-pituitary gonadal axis
The gonadotropin axis was assessed through the measurement of LH and testosterone levels. Low concentrations of testosterone were observed in 21 patients (31.8%), with inappropriately low or normal LH levels.
Prolactin
In the study cohort, 3.0% of patients showed mildly elevated prolactin levels, which was clinically insignificant.
None of the study subjects were noted to have diabetes insipidus.
The prevalence of various hormonal abnormalities is depicted in Fig. 2.
Patients with low testosterone were not commenced on replacement therapy, as they did not exhibit symptoms or signs of hypogonadism at the time of assessment, and they are planned for further assessment at follow-up. They have been counselled for testosterone therapy if low testosterone persists at follow-up and/or they develop clinical features of hypogonadism.
Growth hormone therapy was not initiated due to the prohibitive costs and unaffordability of patients for the same in the Indian setting. rhGH of 1 mL costs INR 15,000, and the per capita income of our patients is about INR 12,500 per month with most of them being daily-wage earners. Moreover, with the onslaught on the COVID-19 pandemic, most were without jobs during this time.
Association of endocrine dysfunction with injury characteristics and outcomes
Hormonal levels were compared between independent groups based on the severity of injury, the type of involvement (diffuse/focal), the duration of injury, level of functional independence (using MBI) and degree of disability (using GOS-E) depicted in Table 3. It was found that the serum testosterone (ng/dL) was significantly lower in the MBI category with moderate-total dependence as compared to the independent category (295.1 ± 112.5 vs. 361.8 ± 125.8; P = 0.02). Other comparisons were not significant. Serum testosterone also showed a significant positive correlation with the MBI scores (r = 0.4; P < 0.001). The proportion of hypogonadism was significantly higher in the group with moderate-total dependence (13/26) as compared to the functionally independent (8/40) group (50% vs. 20%; P = 0.011). The proportion of low IGF-1 levels was not different between various groups.
Hypopituitarism and associated factors
Post-traumatic hypopituitarism, as defined by the involvement of one or more axes, was present in 37/66 (56.1%) of the cohort. Isolated hormone deficiency was observed in 25 patients (37.9%), while 12 (18.2%) had multiple-axis hormone deficiency. The prevalence of hypopituitarism trended higher in individuals with severe injury as compared to moderate injury (66.7% vs. 43.3%; P = 0.05). A higher proportion of hypopituitarism was encountered in those with significant disability as compared to those without disability (61.1% vs. 33.3%), though this did not reach statistical significance. On performing a logistic regression analysis to determine the factors that were significantly associated with hypopituitarism, it was found that in the univariate analysis, the severity of injury (OR = 2.6; 95% CI: 0.9–7.1; P = 0.06) and GOS-E (OR = 3.1; 95% CI: 0.8–11.7; P = 0.08) were significant (P < 0.10); on the multivariate analysis however, these factors were not significant (Table 4).
Discussion
In this study that assessed neuroendocrine dysfunction in young men with chronic TBI, it was found that low IGF-1 levels were most frequently encountered, followed by hypogonadism. More than half of the cohort had hypopituitarism with involvement of one or more axes. Severity of initial injury and the presence of residual disability were significantly associated with post-traumatic hypopituitarism.
In the current study, only one patient was conclusively identified with low cortisol levels through an ACTH stimulation test. This patient was initiated on long-term steroid supplements and was advised on hydrocortisone stress protocol during period of stress. Levothyroxine supplements were initiated for patients diagnosed with hypothyroidism, following the guidance of Endocrinologists. Patients with low testosterone were not commenced on replacement therapy, as they did not exhibit symptoms or signs of hypogonadism at the time of assessment, and they are planned for further assessment at follow-up. They have been counselled for testosterone therapy if low testosterone persists at follow-up and/or they develop clinical features of hypogonadism. Growth hormone therapy was not initiated due to the prohibitive costs and unaffordability of patients for the same in the Indian setting.
This study exclusively included young male adults with a mean age of 32.8 years to maintain homogeneity, aligning with previous findings that neuroendocrine abnormalities are predominantly observed in males, with a mean age of 35.7 years [21]. The primary cause of TBI was road traffic accidents (86.4%), followed by falls (10.6%), and other causes included assault and gunshot injuries (3%), consistent with findings from other studies [22, 23]. According to the Ministry of Road Transport and Highways, an estimated 4.1 lakh road accidents were reported in the country in 2021, causing injuries to 3.4 lakh people. The most affected demographic was males in the age group of 18–45 years, contributing to 67% of total accidental deaths. This vulnerability is attributed to the predominant use of road transport by males, coupled with a lack of safety measures, resulting in a high burden of mortality and morbidity. Pituitary dysfunction post-TBI is usually transient in the acute phase, with many endocrine problems resolving over time. However, persistent issues after several months require further evaluation and treatment. Emelifeonwu’s study indicated that around one-third of TBI patients experience lasting anterior pituitary dysfunction for 12 months or more [24].
After TBI, pituitary dysfunction may not appear immediately. This dysfunction can manifest as a secondary autoimmune condition caused by the development of autoantibodies, which consist of anti-pituitary antibodies (APAs) and anti-hypothalamic (AHAs) autoantibodies [25]. The disruption of the blood-brain barrier during TBI can lead to the release of autoimmune antigens into circulation, which triggers the production of autoantibodies [26]. These autoantibodies can then attack the pituitary and hypothalamus, causing dysfunction. A definitive diagnosis of autoimmune hypopituitarism typically requires a biopsy of the gland, although alternative methods include measuring levels of specific hormones, detecting autoantibodies targeting pituitary cells, and MRI [27].
In 2008, Tanriverdi et al. proposed a link between APA and TBI-induced hypopituitarism. They studied 29 patients three years after they had sustained a TBI, along with a control group. The researchers found APA in 44.8% of patients but none in the control group. They found that patients who tested positive for APA had a significantly higher risk of hypopituitarism, which particularly affected gonadal and somatotroph function. Strong APA positivity was strongly correlated with pituitary dysfunction, especially GHD. Further research confirmed these findings, showing persistent GHD in patients, especially those with severe TBI, indicating a lack of recovery in pituitary function over time [28]. In a five-year prospective study by Tanriverdi et al., anterior pituitary function post-TBI was assessed in 25 patients (20 men, 5 women) at 12 months and five years, with 17 also evaluated at three years. GHD was the most common pituitary hormone deficit observed across all time points. The study also explored links between TBI-induced hypopituitarism and the presence of AHA and APA. Pituitary dysfunction showed a marked increase in the fifth year in patients with strong positivity for AHA and APA (titers ≥ 1/16) [29].
A study by Tanriverdi et al. showed that 43.3% of 30 TBI patients suffered from GHD. Out of the 13 patients with GHD, 7 (53.8%) recovered after 3 years of TBI. Also, 5 out of 6 patients with ACTH deficiency (83.3%) at the first-year evaluation had recovered after 3 years of TBI. One patient was diagnosed with new-onset GHD at the 3-year evaluation, while another patient had new-onset ACTH deficiency at the 3-year evaluation [30].
In a study focused on moderate to severe TBI patients with anterior pituitary dysfunction and its impact on functional outcome, Park et al. demonstrated that the anterior pituitary hormone-deficient group exhibited lower scores in cognition and functional outcome, as assessed by the Mini Mental Status Examination and Functional Independence Measure, respectively [31]. Another investigation conducted at Lille University Medical Centre Rehabilitation Institute revealed that patients with GHD displayed poor performance, low cognition, executive functioning, and ADL participation, with this hormone-deficient group, particularly those with GHD, experiencing a lower QoL [32]. Also, another study showed a significant correlation between hormone levels (FSH, testosterone, GH, FT3, and FT4) and global outcomes assessed by the GOS-E, indicating that lower hormonal levels are associated with poorer functional outcomes [33]. Reimunde et al., analysing the results of their interventional study on the effect of GH replacement and cognitive rehabilitation in TBI patients, recommended that GH replacement therapy can improve outcomes [34]. However, it’s noteworthy that all the mentioned studies were conducted in the acute phase of injury. There is a scarcity of literature assessing the impact of endocrine dysfunction on recovery in the chronic phase of TBI. Tan et al. proposed that screening for hormonal dysfunction in the acute phase may not be necessary as it is often transient [35]. Patients with a history of TBI showing persistent or new symptoms of potential hypopituitarism beyond 6 months should undergo hormonal deficiency screening, including fatigue, low mood, appetite loss, libido loss, polyuria, sexual dysfunction (in men), menstrual irregularities (in women), weight loss, and neuropsychiatric symptoms [36]. Due to symptom overlap between TBI and pituitary dysfunction, other potential causes must be considered and ruled out [8, 35]. Therefore, the screening of neuroendocrine problems is crucial in initiating treatment, thereby enhancing the QoL in TBI patients [4]. The following table (Table 5) depicts a summary of diverse studies investigating endocrine dysfunction among patients with TBI.
The strengths of this study are that it represents the first comprehensive analysis of pituitary dysfunction during the chronic phases post-TBI in Indian men with chronic TBI. The cohort was homogenous, comprising young males. However, this study is constrained by its small sample size due to the onset of the COVID-19 pandemic and the nature of the cross-sectional design. The exclusion of the female gender, the lack of data on the prevalence and nature of hypopituitarism at baseline, and the lack of assessment of free testosterone levels may pose additional limitations. The predominant endocrine dysfunction observed in this study was low IGF-1, utilized as a marker for growth hormone (GH) secretion. The diagnosis of GHD typically requires an insulin tolerance test (ITT); however, this was omitted to avoid insulin-induced hypoglycemia in patients with brain injuries, which could precipitate seizures. Although there exist other growth hormone stimulation tests that have been deemed safe with an acceptable and predictable side-effect profile [8], these were not performed as our study cohort involved men with chronic traumatic brain injury who primarily consulted or were admitted for the purpose of rehabilitation; there were societal constraints in performing these tests as the relatives were unwilling for the same and not prepared to give additional consent. This aspect further underscores the complexities involved in clinical research settings where patient consent and familial support are pivotal factors influencing the feasibility of specific diagnostic procedures. These limitations stand duly acknowledged. Moreover, factors influencing hormone levels, including stress induced by trauma, infections, elevated intracranial pressure (ICP), and seizures, were not subjected to analysis.
Conclusion
Posttraumatic hypopituitarism may be commonly encountered in the chronic phase of TBI and may be associated with both severity of initial injury and the presence of residual disability. Thus, this study emphasizes the importance of assessing endocrine dysfunction in patients during the chronic phases of TBI. The prompt recognition of hormonal deficiencies is vital for implementing necessary treatments, including hormonal replacement, which may contribute to improved participation in therapy and enhanced rehabilitation outcomes. Additionally, prospective randomized controlled studies could be conducted to evaluate the efficacy of hormone replacement therapy in addressing neuroendocrine dysfunction in TBI.
Data availability
The data sets generated and/or analyzed during the current study are not publicly available but are avaiable from the corresponding author on reasonable request.
Abbreviations
- ACTH:
-
Adrenocorticotropic hormone
- IGF:
-
Insulin-like growth factor-1
- TSH:
-
Thyroid stimulating hormone
- LH:
-
Luteinizing hormone
- DM:
-
Diabetes mellitus
- HTN:
-
Hypertension
- RTA:
-
Road traffic accident
- GCS:
-
Glasgow Coma Scale
- SDH:
-
Subdural haemorrhage
- SAH:
-
Subarachnoid haemorrhage
- EDH:
-
Extradural haemorrhage
References
Centers for Disease Control and Prevention (2011) WISQARS (Web-based injury statistics query and reporting system). Choice Rev 48(08):48–4227.
Gilis-Januszewska A, Kluczyński Ł, Hubalewska-Dydejczyk A (2020) Traumatic brain injuries induced pituitary dysfunction: a call for algorithms. Endocr Connect 9(5):R112–R123
Bajwa NM, Kesavan C, Mohan S (2018) Long-term consequences of Traumatic Brain Injury in Bone Metabolism. Front Neurol 9:115
Ghigo E, Masel B, Aimaretti G, Léon-Carrión J, Casanueva FF, Dominguez-Morales MR et al (2005) Consensus guidelines on screening for hypopituitarism following traumatic brain injury. Brain Inj 19(9):711–724
Prodam F, Gasco V, Caputo M, Zavattaro M, Pagano L, Marzullo P et al (2013) Metabolic alterations in patients who develop traumatic brain injury (TBI)-induced hypopituitarism. Growth Horm IGF Res 23(4):109–113
Schneider HJ, Kreitschmann-Andermahr I, Ghigo E, Stalla GK, Agha A (2007) Hypothalamopituitary Dysfunction following traumatic Brain Injury and Aneurysmal Subarachnoid Hemorrhage: a systematic review. JAMA 298(12):1429
Kim SY (2015) Diagnosis and treatment of Hypopituitarism. Endocrinol Metab 30(4):443
Mahajan C, Prabhakar H, Bilotta F (2023) Endocrine dysfunction after traumatic Brain Injury: an ignored clinical syndrome? Neurocrit Care 39(3):714–723
Yanase T, Tajima T, Katabami T, Iwasaki Y, Tanahashi Y, Sugawara A et al Diagnosis and treatment of adrenal insufficiency including adrenal crisis: a Japan Endocrine Society clinical practice guideline
Erturk E, Jaffe CA, Barkan AL (1998) Evaluation of the Integrity of the hypothalamic- pituitary-adrenal Axis by insulin. Hypoglycemia Test 83(7)
Nair A, Jayakumari C, George GS, Jabbar PK, Das DV, Jessy SJ et al (2019) Long acting porcine sequence ACTH in the diagnosis of adrenal insufficiency. Eur J Endocrinol 181(6):639–645
Gundgurthi A, Garg M, Dutta M, Pakhetra R (2013) Intramuscular ACTH Stimulation Test for Assessment of adrenal function. J Assoc Physicians India 61
Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I, Mechanick JI et al (2012) Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American thyroid Association. Endocr Pract 18(6):988–1028
Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL et al (2016) 2016 American Thyroid Association Guidelines for Diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 26(10):1343–1421
Yuen KCJ, Biller BMK, Radovick S, Carmichael JD, Jasim S, Pantalone KM et al (2019) American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of growth hormone Deficiency in adults and patients transitioning from Pediatric to Adult Care. Endocr Pract 25(11):1191–1232
Bhasin S, Brito JP, Cunningham GR, Hayes FJ, Hodis HN, Matsumoto AM et al (2018) Testosterone therapy in men with hypogonadism: an endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab 103(5):1715–1744
Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA et al (2011) Diagnosis and treatment of Hyperprolactinemia: an endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 96(2):273–288
Shah S, Vanclay F, Cooper B (1989) Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol 42(8):703–709
Levin HS, Boake C, Song J, McCauley S, Contant C, Diaz-Marchan P et al (2001) Validity and sensitivity to change of the Extended Glasgow Outcome Scale in mild to Moderate Traumatic Brain Injury. J Neurotrauma 18(6):575–584
Wilson L, Boase K, Nelson LD, Temkin NR, Giacino JT, Markowitz AJ et al (2021) A manual for the Glasgow Outcome Scale-Extended interview. J Neurotrauma 38(17):2435–2446
Olivecrona Z, Dahlqvist P, Koskinen LOD (2013) Acute neuro-endocrine profile and prediction of outcome after severe brain injury. Scand J Trauma Resusc Emerg Med 21(1):33
Alavi SA, Tan CL, Menon DK, Simpson HL, Hutchinson PJ (2016) Incidence of pituitary dysfunction following traumatic brain injury: a prospective study from a regional neurosurgical centre. Br J Neurosurg 30(3):302–306
Javed Z, Qamar U, Sathyapalan T (2015) Pituitary and/or hypothalamic dysfunction following moderate to severe traumatic brain injury: current perspectives. Indian J Endocrinol Metab 19(6):753
Emelifeonwu JA, Flower H, Loan JJ, McGivern K, Andrews PJD (2020) Prevalence of Anterior Pituitary Dysfunction twelve months or more following traumatic Brain Injury in adults: a systematic review and Meta-analysis. J Neurotrauma 37(2):217–226
Harsh V, Kumar A (2013) Role of autoantibodies in the pathophysiology of hypopituitarism following traumatic brain injury. Indian J Neurotrauma 10(1):63
Guaraldi F, Grottoli S, Arvat E, Ghigo E (2015) Hypothalamic-pituitary autoimmunity and traumatic brain Injury. J Clin Med 4(5):1025–1035
Harsh V, Jha S, Kumar H, Kumar A (2019) The autoimmune basis of hypopituitarism in traumatic brain injury: fiction or reality? Br J Neurosurg 33(1):58–61
Tanriverdi F, De Bellis A, Bizzarro A, Sinisi AA, Bellastella G, Pane E et al (2008) Antipituitary antibodies after traumatic brain injury: is head trauma-induced pituitary dysfunction associated with autoimmunity? Eur J Endocrinol 159(1):7–13
Tanriverdi F, De Bellis A, Ulutabanca H, Bizzarro A, Sinisi AA, Bellastella G et al (2013) A five year prospective investigation of anterior pituitary function after traumatic Brain Injury: is Hypopituitarism Long-Term after Head Trauma Associated with Autoimmunity? J Neurotrauma 30(16):1426–1433
Tanriverdi F, Ulutabanca H, Unluhizarci K, Selcuklu A, Casanueva FF, Kelestimur F (2008) Three years prospective investigation of anterior pituitary function after traumatic brain injury: a pilot study. Clin Endocrinol (Oxf) 68(4):573–579
Park KD, Kim DY, Lee JK, Nam HS, Park YG (2010) Anterior pituitary dysfunction in moderate-to-severe chronic traumatic brain injury patients and the influence on functional outcome. Brain Inj 24(11):1330–1335
Moreau OK, Yollin E, Merlen E, Daveluy W, Rousseaux M (2012) Lasting pituitary hormone Deficiency after Traumatic Brain Injury. J Neurotrauma 29(1):81–89
Zheng P, He B, Tong W (2014) Dynamic pituitary hormones change after traumatic brain injury. Neurol India 62(3):280
Reimunde P, Quintana A, Castañón B, Casteleiro N, Vilarnovo Z, Otero A et al (2011) Effects of growth hormone (GH) replacement and cognitive rehabilitation in patients with cognitive disorders after traumatic brain injury. Brain Inj 25(1):65–73
Tan CL, Alavi SA, Baldeweg SE, Belli A, Carson A, Feeney C et al (2017) The screening and management of pituitary dysfunction following traumatic brain injury in adults: British Neurotrauma Group guidance. J Neurol Neurosurg Psychiatry 88(11):971–981
Bondanelli M, Ambrosio MR, Zatelli MC, De Marinis L, Uberti EC (2005) degli. Hypopituitarism after traumatic brain injury. Eur J Endocrinol 152(5):679–91
Tanriverdi F, Senyurek H, Unluhizarci K, Selcuklu A, Casanueva FF, Kelestimur F (2006) High risk of Hypopituitarism after Traumatic Brain Injury: a prospective investigation of anterior pituitary function in the Acute Phase and 12 months after Trauma. J Clin Endocrinol Metab 91(6):2105–2111
Bavisetty S, Bavisetty S, McArthur DL, Dusick JR, Wang C, Cohan P, Boscardin WJ, Swerdloff R, Levin H, Chang DJ, Muizelaar JP, Kelly DF (2008) Chronic hypopituitarism after traumatic brain injury: risk assessment and relationship to outcome. Neurosurgery 62(5):1080–1093
Krewer C, Schneider M, Schneider HJ, Kreitschmann-Andermahr I, Buchfelder M, Faust M et al (2016) Neuroendocrine disturbances one to five or more years after traumatic Brain Injury and Aneurysmal Subarachnoid Hemorrhage: data from the German database on Hypopituitarism. J Neurotrauma 33(16):1544–1553
Yaseen NT, Al-Khaqani F, Mansour AA (2018) Patterns of pituitary dysfunction three months or more after traumatic brain injury. Avicenna J Med 8(04):125–132
Acknowledgements
None.
Funding
Fluid research Grant of Christian Medical College, Vellore.
Author information
Authors and Affiliations
Contributions
RT, TVP, conceived and designed the study. SSZ, JTJ, SR collected the results. SSZ, KEC, RT performed the data analysis, figure design and manuscript writing. NK, HSA, TVP, KEC, RT provided the needed support to investigate and supervise the findings of this work. All the authors revised the manuscript for important intellectual content and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zacharia, S.S., Thomas, R., Johnson, J.T. et al. Neuroendocrine challenges and clinical outcomes in men with chronic traumatic brain injury: a cross-sectional study. Pituitary (2024). https://doi.org/10.1007/s11102-024-01433-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s11102-024-01433-9