Abstract
Purpose
Hypofractionated stereotactic radiotherapy (HSRT) for refractory Cushing’s disease may offer a condensed treatment schedule for patients with large tumors abutting the optic chiasm unsuitable for stereotactic radiosurgery (SRS). To-date only four patients have been treated by HSRT in the published literature. We investigated the feasibility, toxicity, and efficacy of HSRT compared to SRS.
Methods
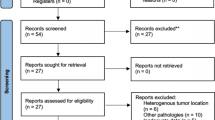
After approval, we retrospectively evaluated patients treated at our institution for refractory Cushing’s disease with SRS or HSRT. Study outcomes included biochemical control, time to biochemical control, local control, and late complications. Binary logistic regression and Cox proportional hazards regression evaluated predictors of outcomes.
Results
Patients treated with SRS (n = 9) and HSRT (n = 9) were enrolled with median follow-up of 3.4 years. Clinicopathologic details were balanced between the cohorts. Local control was 100% in both cohorts. Time to biochemical control was 6.6. and 9.5 months in the SRS and HSRT cohorts, respectively (p = 0.6258). Two patients in each cohort required salvage bilateral adrenalectomy. Late complications including secondary malignancy, radionecrosis, cranial nerve neuropathy, and optic pathway injury were minimal for either cohort.
Conclusions
HSRT is an appropriate treatment approach for refractory Cushing’s disease, particularly for patients with large tumors abutting the optic apparatus. Prospective studies are needed to validate these findings and identify factors suggesting optimal fractionation approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional pituitary adenoma hypersecreting adrenocorticotropic hormone (ACTH) was first described by Cushing in 1932 [1, 2]. The prevalence of Cushing’s disease is approximately 40 patients per million population with a female preponderance, and Cushing’s disease is diagnosed in approximately 8 patients per million US population annually [3, 4]. The pathogenesis of these tumors is poorly understood [5, 6]. Disruption of the hypothalamic–pituitary–adrenal axis due to ACTH hypersecretion leads to elevated serum and urinary cortisol levels [7]. Prolonged glucocorticoid exposure manifests as central obesity, fatigue with proximal myopathy, skin thinning with purple striae, and bruising [8]. Hypercortisolemia also promotes systemic arterial hypertension, osteoporosis, dyslipidemia, immunocompromise, diabetes mellitus, sexual dysfunction, menstrual irregularity, psychiatric disease including suicidality, and infertility [8]. These comorbidities significantly impair quality of life and, with particular regard to cardiovascular and infectious disease, contribute to excess morbidity and mortality [9-11].
The first-line treatment of Cushing’s disease is surgical resection typically by the transsphenoidal approach with selective adenomectomy or hemi/total hypophysectomy. Rates of immediate biochemical remission following primary surgery vary considerably and have been reported between 25 and 100%; one review reported an average immediate remission rate of 77.8% [7]. Late recurrence rates up to 10 years following primary surgery alone have also been heterogeneously reported between 0 and 51.2% and on average 32% [7]. Persistent hypercortisolism following surgical resection can be treated by repeat resection, medication, or radiation, with bilateral adrenalectomy as a final salvage alternative. Medical management can successfully control chronic biochemical disease, although medication alone does not offer definitive cure [12, 13]. While repeat surgery offers the potential for immediate disease remission, repeat resection is associated with a 42% likelihood of failure, in addition to the concomitant risks of an invasive procedure [7].
External beam radiation has been used in the treatment of Cushing’s disease since 1933 [1, 2, 14]. Radiation is typically delivered by conventional intensity-modulated radiation therapy (IMRT) over 5–6 weeks to 50.4–54 Gy or by stereotactic radiosurgery (SRS) in a single session to greater than 18 Gy [15]. SRS is associated with faster time to biochemical remission compared with IMRT, as well as greater convenience for the patient [16, 17]. However, IMRT is typically indicated for tumors greater than 3 cm or less than 5 mm from the chiasm due to an increased risk of optic pathway injury with single session SRS [15]. Patients with these challenging tumors may be suitable candidates for hypofractionated stereotactic radiotherapy (HSRT). HSRT, delivered in 2–5 fractions, may reduce the risk of optic toxicity and cranial nerve neuropathy compared to SRS due to the radiobiologic advantage of fractionation, which allows preservation of normal tissue and destruction of tumor due to biological differences in neoplastic and normal tissue [18]. HSRT may also offer patients a shorter time to biochemical remission compared to IMRT as well as convenience of a single week of treatment. However, this approach remains novel, and to-date the outcomes of HSRT for Cushing’s disease have been reported in only four patients over three separate studies [19-21]. Therefore, we sought to investigate the feasibility and efficacy of HSRT. The purpose of our study was to compare the local control, biochemical control, time to biochemical control, and toxicities of SRS and HSRT.
Methods
After institutional review board approval, we retrospectively evaluated adult patients with ACTH-secreting pituitary adenoma treated at our institution with linear accelerator-based SRS or HSRT between 1996 and 2018. Treatment decision-making in this study including surgery, medical management, and radiation was at the discretion of the treating physician and/or multidisciplinary tumor board. The electronic medical record was reviewed for demographics and clinical details. Toxicities were graded according to Common Terminology Criteria for Adverse Events version 5.0. Biologically effective dose (BED) and equivalent dose in 2 Gy fractions (EQD2) was calculated using an alpha/beta ratio of three for pituitary adenoma [18, 22-24]. Data were compiled using REDCap (Research Electronic Data Capture) [25]. Radiation-induced malignancy was defined as a new primary CNS malignancy within the 2 Gy isodose line based on the Cahan criteria [26]. Study outcomes included biochemical control, local control, endocrinopathy, and complications following multi-fraction SRS compared to single-fraction SRS. Local control was defined as the absence of tumor progression as determined by a neuroradiologist necessitating salvage intervention. Biochemical control was defined as hormone normalization with the assistance of suppressive medication as determined by the treating endocrinologist; complete biochemical control was defined as hormone normalization without the need for suppressive medications. Post-SRS endocrinopathy was defined as a new requirement to replace physiologic hormone as a result of pituitary insufficiency after SRS as determined by the treating endocrinologist.
Baseline characteristics and treatment details were summarized with descriptive statistics. The Shapiro–Wilk test was used to assess for normality of continuous variables. Covariates that lacked a normal distribution were described by median and range. Predictors of binary outcomes were evaluated by logistic regression. Time to event outcomes were analyzed by single predictor Cox proportional hazards regression models. Proportionality was assessed by Kolmogorov-type supremum test with 1000 simulations and by graphing martingale score residuals versus time. Strata were evaluated by fitting Kaplan–Meier curves and testing the two groups in a log-rank test. All confidence intervals were reported at 95% and all p values were reported as two-sided, with significance defined at a level of p < 0.05. All statistical analysis was performed using SAS version 9.4 (Cary, NC); plots were generated using GraphPad Prism version 7 (La Jolla, CA).
Results
A total of 18 patients were enrolled in the study. Clinicopathologic details are described in Table 1. Most patients were Caucasian females treated at a median age of 42 years. Patients typically came to medical attention with Cushingoid symptoms (n = 15, 83%). Patients were often diagnosed with pituitary macroadenoma (n = 11, 65%). 3 patients in the HSRT cohort had radiologic chiasm involvement at the time of diagnosis. All patients underwent surgical resection prior to radiation and were referred to radiation oncology due to persistent local or biochemical disease. Median follow-up after radiation treatment was 3 years.
Patients were treated with SRS (n = 9) or HSRT (n = 9). Patients treated with HSRT either received two fractions (n = 3), three fractions (n = 1), or five fractions (n = 5). Median total marginal dose to the PTV was 21 Gy with a median BEDtumor of 133 Gy and EQD2 of 80 Gy. The SRS and HSRT cohorts were not significantly different in terms of age, race, sex, tumor morphology, presenting symptoms, prior surgical resection, number of surgeries, or follow-up time (p > 0.05) (Table 2). Patients in the HSRT were treated to a higher total marginal dose (p = 0.0168), and patients in the SRS cohort were treated to a higher BEDtumor (p = 0.0048). Acute side effects of SRS included CTCAE grade 1 headache (n = 1); no other side effects were observed.
At the time of last follow-up, 2 patients in the SRS cohort had developed central hypothyroidism, 0 patients developed hypogonadotropic hypogonadism, and 2 patients in the HSRT cohort developed central adrenal insufficiency. Time to development of any endocrinopathy was not significantly different between the SRS and HSRT cohorts (p = 0.4077). Age, total dose, BEDtumor, number of surgeries, and number of fractions were also not predictive of post-SRS pituitary deficit.
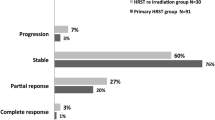
Overall local control at last follow-up was 100% with 0 local failures observed; time to local failure is plotted on Kaplan–Meier curves (Fig. 1). Single predictor and multivariable Cox proportional hazard regressions model analyses were not performed due to the absence of disease events. There were no pituitary-directed salvage therapies.
At last follow-up after SRS, 5 patients (39%) achieved biochemical control with or without medication assistance, and 4 patients (31%) achieved complete biochemical control without the need for medications. The mean time to biochemical control with medication was 9 months, and the mean time to complete biochemical control was 41 months (Fig. 2a, b). SRS versus HSRT was not associated with achievement of biochemical control, complete control, time to control, or time to complete control (Table 3). Age, sex, morphology, functional histology, number of surgeries, number of fractions, dose per fraction, total marginal dose, and BEDtumor were not associated with time to biochemical control or complete biochemical control (p > 0.05). Four patients underwent salvage bilateral adrenalectomy following radiation, two patients in each cohort. Median time to adrenalectomy was 2.1 years (IQR 1.0–3.9 years). Age, sex, single versus multisession SRS, BEDtumor, total marginal dose, number of surgeries, and number of fractions were not predictive of salvage bilateral adrenalectomy.
Over 110 years of patient follow-up after SRS, no patients were diagnosed with optic neuropathy, secondary malignancy, malignant transformation, cavernous sinus cranial neuropathy, or cerebrovascular complications. One patient was diagnosed with radionecrosis. This patient was treated with 1 fraction to a marginal dose of 21 Gy. Three years following SRS, she presented with altered mental status and was diagnosed with radionecrosis of the left temporal lobe with pathologic confirmation. Shortly thereafter she was diagnosed with subacute progressive encephalopathy secondary to adult-onset leukodystrophy with axonal spheroids and pigmented glia, and discharged to hospice care.
Discussion
In this study, we report the outcomes of patients with refractory Cushing’s disease treated with HSRT compared to SRS. To-date, this work represents the largest study of HSRT in the treatment of refractory Cushing’s disease. We demonstrate that HSRT is a feasible and appropriate treatment approach in the radiosurgical management of Cushing’s disease. Patients treated by HSRT appear to have comparable rates of biochemical control and time to biochemical control compared to SRS. HSRT may offer patients with large tumors or tumors with chiasmatic involvement a safe treatment comparable with IMRT with the convenience of a single week of treatment. Prospective studies of HRST are needed to validate the findings of this work and explore factors predictive of outcome with well-powered multivariable analyses.
Importantly, the BED and EQD2 of patients treated with SRS was significantly greater than the BED and EQD2 of patients treated with HSRT. Although HSRT achieves highly precise radiation deposition by stereotactic targeting, the dose and fractionation schemes reported here are not biologically equivalent to radiosurgery, and thus we interpret with caution our results showing that HSRT offers comparable time to biochemical control as SRS owing to sample size and follow-up limitations. Dose-escalation trials utilizing radiosurgical dosing delivered with stereotactic targeting in five fractions are warranted to assess feasibility and tolerance, as such regimens are hypothesized to have equivalent time to biochemical control outcomes as single-fraction SRS with improved toxicity profiles.
Rate of biochemical control following IMRT after surgical failure is approximately 80% with time to remission between 18 and 42 months [7, 15, 27-33]. In contrast, biochemical control rates following SRS appear to be between 85-100% with median time to normalization between 7.5 and 33 months [15, 34-38]. In our study, biochemical control and requirement for salvage adrenalectomy following SRS and HSRT appear comparable to historical rates after IMRT and SRS. Moreover, time to biochemical control in the HRST cohort appears similar to the SRS cohort and historical data. Local control also remains excellent after HSRT and is consistent with the IMRT and SRS literature reporting 95–100% local control [15]. Post-SRS hypopituitarism also appears similar between cohorts. Radiation-induced complications, such as blindness and secondary malignancy, were not observed in either cohort, precluding comparison.
Limitations to this study include its sample size and retrospective nature with associated biases such as selection bias. Follow-up time was also heterogeneous in our study, although balanced between cohorts, and rare late events such as secondary malignancy require long-term follow-up for full evaluation. A limited number of disease events also precluded our ability to evaluate predictive factors of outcome in multivariable analysis; well-powered prospective studies are needed to investigate such factors further.
HSRT is an appropriate treatment approach for patients with refractory Cushing’s disease. HSRT allows for radiobiologic protection of native structures with the convenience of 1-week treatment time. Dose-escalation studies are warranted to evaluate whether radiosurgical dosing for refractory Cushing’s disease in five fractions is feasible and well-tolerated, as dose-escalated multisession SRS over 5 fractions may offer patients equivalent time to biochemical control as SRS. Further studies evaluating HSRT are warranted to validate our findings here and further explore the utility of HSRT in the treatment of refractory Cushing’s disease.
References
Cushing H (1932) The basophil adenomas of the pituitary body and their clinical manifestations (pituitary basophilism). Bull Johns Hopkins Hosp 50:137–195
Cushing H (1932) Further notes on pituitary basophilism. JAMA 99:281–284
Buliman A, Tataranu L, Paun D et al (2016) Cushing’s disease: a multidisciplinary overview of the clinical features, diagnosis, and treatment. J Med Life 9:12–18
Broder MS, Neary MP, Chang E et al (2015) Incidence of Cushing’s syndrome and Cushing’s disease in commercially-insured patients %3c65 years old in the United States. Pituitary 18:283–289. https://doi.org/10.1007/s11102-014-0569-6
Dahia PLM, Grossman AB (1999) The molecular pathogenesis of corticotroph tumors. Endocr Rev 20:136–155. https://doi.org/10.1210/edrv.20.2.0358
Newell-Price J, Bertagna X, Grossman AB, Nieman LK (2006) Cushing’s syndrome. Lancet 367:1605–1617. https://doi.org/10.1016/S0140-6736(06)68699-6
Pivonello R, De Leo M, Cozzolino A, Colao A (2015) The treatment of cushing’s disease. Endocr Rev 36:385–486. https://doi.org/10.1210/er.2013-1048
Pivonello R, De Martino M, De Leo M et al (2008) Cushing’s syndrome. Endocrinol Metab Clin North Am 37:135–149. https://doi.org/10.1016/j.ecl.2007.10.010
Feelders RA, Pulgar SJ, Kempel A, Pereira AM (2012) The burden of Cushing’s disease: clinical and health-related quality of life aspects. Eur J Endocrinol 167:311–326. https://doi.org/10.1530/EJE-11-1095
Graversen D, Vestergaard P, Stochholm K et al (2012) Mortality in Cushing’s syndrome: a systematic review and meta-analysis. Eur J Intern Med 23:278–282. https://doi.org/10.1016/j.ejim.2011.10.013
Clayton RN (2010) Mortality in Cushing’s disease. Neuroendocrinology 92(Suppl 1):71–76. https://doi.org/10.4183/aeb.2010.83
Miller JW, Crapo L (1993) The medical treatment of cushing’s syndrome. Endocr Rev 14:443–458. https://doi.org/10.1210/edrv-14-4-443
Juszczak A, Ertorer ME, Grossman A (2013) The therapy of cushing’s disease in adults and children: an update. Horm Metab Res 45:109–117. https://doi.org/10.1055/s-0032-1330009
Mehta GU, Lonser RR, Oldfield EH (2012) The history of pituitary surgery for Cushing disease. J Neurosurg 116:261–268. https://doi.org/10.3171/2011.8.jns102005
Loeffler JS, Shih HA (2011) Radiation therapy in the management of pituitary adenomas [Review]. J Clin Endocrinol Metab 96:1992–2003. https://doi.org/https://dx.doi.org/10.1210/jc.2011-0251
Kong DS, Il Lee J, Do HL et al (2007) The efficacy of fractionated radiotherapy and stereotactic radiosurgery for pituitary adenomas: long-term results of 125 consecutive patients treated in a single institution. Cancer 110:854–860. https://doi.org/10.1002/cncr.22860
Mitsumori M, Shrieve DC, Alexander E et al (1998) Initial clinical results of linac-based stereotactic radiosurgery and stereotactic radiotherapy for pituitary adenomas. Int J Radiat Oncol Biol Phys 42:573–580. https://doi.org/10.1016/S0360-3016(98)00256-9
Fowler JF (2010) 21 Years of biologically effective dose. Br J Radiol 83:554–568. https://doi.org/10.1259/bjr/31372149
Pham CJ, Chang SD, Gibbs IC et al (2004) Preliminary visual field preservation after staged CyberKnife radiosurgery for perioptic lesions. Neurosurgery 54:799–810. https://doi.org/10.1227/01.NEU.0000114261.18723.6A
Adler JR, Gibbs IC, Puataweepong P, Chang SD (2006) Visual field preservation after multisession CyberKnife radiosurgery for perioptic lesions. Neurosurgery 59:2442–2454. https://doi.org/10.1227/01.NEU.0000223512.09115.3E
Liao HI, Wang CC, Wei KC et al (2014) Fractionated stereotactic radiosurgery using the Novalis system for the management of pituitary adenomas close to the optic apparatus. J Clin Neurosci 21:111–115. https://doi.org/10.1016/j.jocn.2013.03.024
Niranjan A, Flickinger JC (2008) Radiobiology, principle and technique of radiosurgery. Prog Neurol Surg 21:32–42. https://doi.org/10.1159/000156557
Kondziolka D, Shin SM, Brunswick A et al (2015) The biology of radiosurgery and its clinical applications for brain tumors. Neuro Oncol 17:29–44. https://doi.org/10.1093/neuonc/nou284
Hall EJ, Brenner DJ (1993) The radiobiology of radiosurgery: rationale for different treatment regimes for AVMs and malignancies. Int J Radiat Oncol Biol Phys 25:381–385. https://doi.org/10.1016/0360-3016(93)90367-5
Harris PA, Taylor R, Thielke R et al (2009) Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Cahan W, Woodard H (1948) Sarcoma arising in irradiated bone; report of 11 cases. Cancer 1:3–29
Sonino N, Zielezny M, Fava GA et al (1996) Risk factors and long-term outcome in pituitary-dependent Cushing’s disease. J Clin Endocrinol Metab 81:2647–2652. https://doi.org/10.1210/jc.81.7.2647
Howlett T, Plowman P, Wass J et al (1989) Megavoltage pituitary irradiation in the management of Cushing’s disease and Nelson’s syndrome: long-term follow-up. Clin Endocrinol 31:309–323
Vicente A, Estrada J, de la Cuerda C et al (2009) Results of external pituitary irradiation after unsuccessful transsphenoidal surgery in Cushing’s disease. Acta Endocrinol (Copenh) 125:470–474. https://doi.org/10.1530/acta.0.1250470
Tran LM, Blount L, Horton D et al (1991) Radiation therapy of pituitary tumors: results in 95 cases. Am J Clin Oncol 14:25–29. https://doi.org/10.1097/00000421-199102000-00005
Zierhut D, Flentje M, Adolph J et al (1995) External radiotherapy of pituitary adenomas. Int J Radiat Oncol Biol Phys 33:307–314. https://doi.org/10.1016/0360-3016(95)00071-6
Estrada J, Boronat M, Mielgo M et al (1997) The long-term outcome of pituitary irradiation after unsuccessful transsphenoidal surgery in cushing’s disease. N Engl J Med 336:172–177. https://doi.org/10.1056/nejm199701163360303
Minniti G, Osti M, Jaffrain-Rea ML et al (2007) Long-term follow-up results of postoperative radiation therapy for Cushing’s disease. J Neurooncol 84:79–84. https://doi.org/10.1007/s11060-007-9344-0
Voges J, Kocher M, Runge M et al (2006) Linear accelerator radiosurgery for pituitary macroadenomas: a 7-year follow-up study. Cancer 107:1355–1364. https://doi.org/10.1002/cncr.22128
Sheehan JP, Pouratian N, Steiner L et al (2011) Gamma knife surgery for pituitary adenomas: factors related to radiological and endocrine outcomes. J Neurosurg 114:303–309. https://doi.org/10.3171/2010.5.jns091635
Castinetti F, Nagai M, Morange I et al (2009) Long-term results of stereotactic radiosurgery in secretory pituitary adenomas. J Clin Endocrinol Metab 94:3400–3407. https://doi.org/10.1210/jc.2008-2772
Devin JK, Allen GS, Cmelak AJ et al (2004) The efficacy of linear accelerator radiosurgery in the management of patients with Cushing’s disease. Stereotact Funct Neurosurg 82:254–262. https://doi.org/10.1159/000083476
Jagannathan J, Sheehan J, Pouratian N et al (2007) Gamma knife surgery for Cushing’s disease. J Neurosurg 106:980–987. https://doi.org/10.3171/jns.2007.106.6.980
Acknowledgements
This work was supported by CTSA Award No. UL1TR000445 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Funding
There was no funding associated with this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Alexander Sherry declares that he has no conflicts of interest. Mohamed H. Khattab receives research funding support from Varian Medical Systems and Brainlab, Inc. Mark Xu declares that he has no conflicts of interest. Patrick Kelly declares that he has no conflicts of interest. Joshua Anderson declares that he has no conflicts of interest. Guozhen Luo declares that she has no conflicts of interest. Andrea Utz declares that she has no conflicts of interest. Lola Chambless declares that she has no conflicts of interest. Anthony Cmelak declares that he has no conflicts of interest. Albert Attia receives funding from Brainlab, AstraZeneca, and Novocure.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was waived by the IRB due to the determination of minimal risk of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sherry, A.D., Khattab, M.H., Xu, M.C. et al. Outcomes of stereotactic radiosurgery and hypofractionated stereotactic radiotherapy for refractory Cushing’s disease. Pituitary 22, 607–613 (2019). https://doi.org/10.1007/s11102-019-00992-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-019-00992-6