Abstract
Whether the preoperative use of somatostatin analogues (SA) improves surgical outcomes in acromegaly is still a matter of debate.
Objective
We conducted a systematic review of randomized, controlled trials that compared the short-term outcomes of preoperative use of SA (Pre-SA) with direct TSS (No-SA) for the treatment of newly diagnosed acromegaly.
Methods
Embase, Pubmed, Lilacs, and Central Cochrane were used as our data sources. The primary outcomes were no need for any adjuvant treatment 3 months after surgery, based on biochemical results (GH nadir after OGTT <1 μg/L and normal IGF-1 for age and gender), quality of life and mortality. The included trials were analyzed using the Grading of Recommendations Assessment, Development, and Evaluation approach.
Results
A total of 2.099 references were identified and two reviewers independently screened the titles and abstracts. From the 14 potentially eligible studies, four were included and ten were excluded due to lack of randomization or different outcomes. A pool of 261 patients was randomly assigned to Pre-SA or No-SA. Meta-analysis of IGF1 normalization showed a significant difference in favor of Pre-SA (RR 2.47; 95 % CI 1.66, 3.77). Adding a GH nadir on OGTT ≤1 μg/L, we found a RR of 2.15 (95 % CI 1.39, 3.33). Quality of evidence for no need of adjuvant postoperative treatment was moderate, but for improving quality of life was very low and for mortality was absent.
Conclusion
Pre-SA increases the chance of biochemical control of acromegaly 3 months after TSS in patients harboring GH-secreting pituitary macroadenomas.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acromegaly is a chronic disease observed in both men and women of any age characterized by excessive production of growth hormone (GH), which is related to a somatotroph pituitary adenoma in the vast majority of cases, and a consequent overproduction of insulin-like growth factor I (IGF-I) by the liver [1–3]. The diagnosis is frequently delayed 8–10 years after the first signs and symptoms due to the insidious development of the disease. Biochemical diagnosis is based on serum measurements of GH and IGF-1 and pituitary imaging reveals a pituitary macroadenoma in roughly 70 % of cases at diagnosis [3].
Transsphenoidal surgery (TSS) is the treatment of choice in most patients with acromegaly and promotes control of the disease in a significant proportion of cases. Surgical results are dependent on preoperative serum GH and IGF-I levels, tumor invasiveness and neurosurgeon’s skills [4]. In experienced hands, TSS alone results in cure of acromegaly in up to 90 % of patients with microadenomas and approximately 50 % of those with macroadenomas [5]. The success rates of TSS decline substantially in patients harboring large and invasive tumors, and other therapeutic modalities are needed when TSS fails [4].
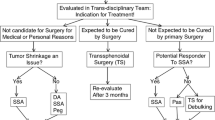
The somatostatin analogues (SA) lanreotide and octreotide have an important role in the adjuvant treatment of acromegaly. Moreover, they can be prescribed as first line therapy for patients with invasive tumors and low probability of surgical cure and for those with contra-indications for surgery. Their mechanism of action involves binding to somatostatin receptors (sstr), especially sub-type sstr2, with inhibition of GH secretion and/or cell proliferation. However, a question that remains opened is whether the preoperative use of SA improves or not the surgical outcomes and the success rates of the TSS. It has been claimed that tumor removal would be facilitated by SA pre-treatment due to softening of the tissue parenchyma induced by the drug [6, 7]. Other authors have also suggested that SA pretreatment would lead to shorter periods of hospitalization after TSS [8]. Nevertheless, the studies have reported on conflicting results, with some showing benefits [6, 8, 9], and others showing no difference [10, 11] on the impact of preoperative use of SA in the surgical outcomes.
For this reason, we have undertaken a systematic review of randomized, controlled trials that compared preoperative SA therapy with direct TSS in acromegaly to investigate the impact of preoperative medical treatment with SA in the surgical outcomes of newly diagnosed patients.
Methods
We have included randomized controlled trials involving newly diagnosed adults with acromegaly, who were randomized into intervention (Pre-SA) and comparison (No-SA) groups. In the Pre-SA group, patients received SA therapy before TSS and in the No-SA group; they were submitted to TSS without previous medical.
The primary postoperative outcomes analyzed in our study included no need for any adjuvant treatment of acromegaly 3 months after TSS (SA, radiotherapy or cabergoline), quality of life and mortality. Achievement of biochemical control of acromegaly (GH nadir after OGTT ≤1 μg/L or random GH <2.5 ng/mL and normal IGF-1 for age and gender) was used as criteria for no need of additional treatment. Secondary outcomes were improvement of acromegaly complications (cardiovascular disease, hypertension, diabetes mellitus), tumor shrinkage, costs, duration of hospitalization and surgery complications.
We have searched the following electronic data bases until December 2013 to identify randomized clinical trials involving preoperative SA (Pre-SA) versus direct TSS (No-SA) in the treatment of newly diagnosed acromegalic patients: Embase (1980–2013), PubMed (1966–2013), Lilacs (1982–2013) and the Cochrane Central Register of Controlled Trials (CENTRAL, the Cochrane Library, issue 2013). We also searched for ongoing clinical trials on ClinicalTrials.gov website. The Medical Subject Heading (MeSH) terms used included ‘‘Somatostatin Analogues’’, ‘‘Transsphenoidal Surgery’’, ‘‘Acromegaly’’ and ‘‘Randomized Controlled Trial’’. There was no language restriction.
Two reviewers (VSN and JMSC) independently screened the titles and abstracts identified by the literature search, and the studies potentially eligible for inclusion in the review were selected for complete reading.
Both reviewers assessed study quality and extracted data using an extraction template. In case of disagreements, there was a debate between the reviewers and a third party (EMKS) before the final decision. For each trial, we assigned quality scores for random sequence generation, allocation concealment, blinding of outcome assessment and incomplete outcome data, using the criteria described in the Cochrane Reviewers’ Handbook [12].
For the dichotomous outcomes, relative risk was calculated with a 95 % confidence interval and we expressed continuous variables as weighted mean difference along with their 95 % confidence intervals. Potential causes of heterogeneity among the studies were also analyzed. We used the I2 statistic to measure the proportion of statistical heterogeneity for each outcome. When the outcomes were homogeneous, we undertook a fixe defect meta-analysis (calculated in Review Manager 5.2 software). The sensitivity analysis was also performed by excluding clinical trials of low methodological quality. The quality of evidence per outcome measurement was graded according to the guidelines of the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) Working Group [13, 14].
Results
From the searches of databases, 2.099 references were identified (Fig. 1). Fourteen articles were potentially eligible for inclusion in the review, and from these, four publications were included in the final analysis [15–18]. Ten studies were excluded due to lack of randomization and different outcomes [6, 10, 11, 19–25].
The four studies included in the meta-analysis involved a total of 261 participants, and all were randomized clinical trials. Carlsen et al. [15] conducted a multicenter study, involving three centers in Norway; Shen et al. [16], Mao et al. [17], and Li et al. [18] performed their trials in three different single centers in China. In all studies a P value <0.05 was considered statistically significant in the differences between the groups. The main characteristics of the enrolled patients at each study and the included studies are presented in Tables 1 and 2, respectively.
Carlsen et al. [15] analyzed 62 newly diagnosed and untreated acromegalic patients indentified during an inclusion time of 5 years. There were 6 patients with micro and 26 with macroadenoma in the intervention group, and 5 patients with micro and 25 with macroadenoma in the control group. They were randomized directly to TSS surgery or to preoperative treatment with 20 mg of octreotide LAR intramuscular every 28 days for 6 months. All individuals were operated by one of the five dedicated neurosurgeons at each of the five University Hospitals in Norway. The time of follow up was 3 months postoperatively. Primary outcomes were tumor volume reduction and controlled disease according to IGF1 [(less than or equal to upper limit of normal (ULN))] or combined criteria (IGF1 normalization and GH nadir during an OGTT ≤1.0 μ/L). In patients with macroadenoma, controlled disease according to IGF1 normalization was significantly higher in Pre-SA than in No-SA (50 vs. 16 %; respectively; P = 0.017). The proportion of patients with microadenoma who achieved controlled disease according to IGF1 (either solely by IGF1 or by combined criteria) was the same in the two groups. Three months postoperatively tumor volume was 0.51 ± 0.73 ml in intervention group and 0.80 ± 1.45 ml in comparison group. Immediate and persistent surgical complications were reported on 4 and 3 cases, respectively, of the Pre-SA group and in 2 and 4 cases of the No-SA group.
Mao et al. [17] performed their trial in a University Hospital in China. Patients were recruited from January 2004 to December 2007. A total of 108 patients, all harboring macroadenoma, were randomized to 4-month preoperative treatment with lanreotide (Somatuline LA, Ipsen, Paris, France) or to direct TSS. Pretreatment started with 30 mg of lanreotide intramuscular every 2 weeks, with subsequent increase to 30 mg per week at week 8, if mean GH >2.5 μg/L on the GH day curve. In both groups, TSS was performed by two neurosurgeons dedicated to the treatment of pituitary tumors. Primary outcome was controlled disease evaluated 4-month postoperatively by IGF1 less than or equal to age-adjusted ULN. Controlled disease rate was significantly higher in Pre-SA group than No-SA group (49 % versus 18.4 %, respectively, P = 0.001). When a GH nadir during an OGTT ≤1.0 μg/L was added to the criteria, the rates were reduced to 38 and 18.4 % in Pre-SA and No-SA groups, respectively, a difference that was still statistically significant (P = 0.025).
Shen et al. [16] randomized 39 acromegaly patients, all with invasive macroadenoma, from January 2005 to June 2006 to preoperative treatment with 20 mg of octreotide LAR intramuscular every 28 days for 3 months or to TSS directly. Follow up was 26.6 ± 4.2 months after surgery, and all TSS were performed by a single experienced surgeon. Primary outcome was controlled disease defined by GH nadir during an OGTT ≤1.0 μg/L and normal IGF1 for age and gender. The secondary outcomes were tumor shrinkage, improvement in the levels of blood glucose and blood pressure, number of patients with impaired glucose tolerance (IGT), Diabetes Mellitus (DM) or high blood pressure, tumor texture, invasion and resection rate during surgery. All patients performed nadir GH and IGF1 evaluation, and pituitary MRI at 3 and 6 months, 1 year, and annual follow up. At 3 and 6 months of treatment, remission rate was significantly higher in Pre-SA than in No-SA (31.6 vs. 5 % and 42.1 vs. 10 %, P = 0.044 and 0.031; respectively). However, at long-term follow up the difference was not significant (31.6 % Pre-SA vs. 10 % No-SA). There were no differences in the level of blood glucose or blood pressure, and the number of patients with IGT or DM or high blood pressure.
Li et al. [18] enrolled 52 acromegaly patients from December 2006 to January 2010 to be randomized to preoperative treatment with lanreotide for 3 months or to direct TSS. Lanreotide was initiated at a dose of 30 mg every 2 weeks, with subsequent increase to 30 mg per week at week 8, if mean GH >2.5 μg/L on the GH day curve. All patients had macroadenoma promoting bony destruction or invasion into sphenoid sinus. The same two neurosurgeons operated all patients. Postoperative evaluation was performed 3 months after surgery with GH nadir during an OGTT ≤1.0 μg/L and normal IGF1 as primary outcomes. The secondary outcome was tumor consistency during surgery. They found significantly higher remission rate in the Pre-SA group in comparison with the No-SA (45.8 vs. 5 %, respectively; P < 0.05).
The risk of bias (random sequence generation, allocation concealment, blinding of outcome assessment and incomplete outcome data) of four included studies are presented in Table 2.
The meta-analysis of IGF1 normalization showed a significant difference in favor of Pre-SA [RR 2.47; (95 % CI 1.66, 3.77)] (Fig. 2). When adding a GH nadir during an OGTT ≤1 μg/L, the meta-analysis evidenced a RR of 2.15 (95 % CI 1.39, 3.33) and a risk difference of 22 %, also favoring the Pre-SA group (Fig. 3). The effect was inconclusive for patients with microadenoma, due to small number. In two studies [15, 17], controlled disease was estimated for age-adjusted cutoff levels of IGF1 ranging from 80 to 120 % of the ULN, and again the meta-analysis showed significantly higher remission rates in Pre-SA than No-SA. We also performed the meta-analysis of IGF1 normalization based on somatostatin analogue (lanreotide and octreotide); the statistic results maintained favoring significantly the Pre-SA patients, without difference between these subgroups; (RR 2.5 (1.51–4.15, P = 0.0004) and 2.42 (1.25–4.71 P = 0.009), respectively).
Only two studies assessed the duration of postoperative hospital stay and the results were similar between both groups [15, 17]. Meta-analysis of surgical complications did not differ between the groups (Fig. 4).
The quality of evidence of no need for complementary treatment of acromegaly 3 months after surgery were graded according to the guidelines of the GRADE Working Group [13, 14] (Table 3).
Discussion
In many cases, acromegaly is caused by large and invasive macroadenomas, which are prone to partial tumor resection and low postoperative remission rates, with the need for complementary therapies to control the disease activity. Theoretically, preoperative use of SA could potentially reduce GH levels and alter tumor characteristics, influencing positively the surgical outcomes. However, there is no clear evidence that this concept is true and available results from published studies are still controversial. Thus, we decided to perform a carefully systematic review of only randomized and controlled trials with the hypothesis that preoperative SA therapy improves the remission rates of TSS in acromegaly.
Four studies were included and a pool of 261 patients was randomly assigned to Pre-SA (lanreotide in two studies and octreotide and two studies) or No-SA. SA was prescribed 3 months before surgery in two studies [16, 18], 4 months in one study [17] and 6 months in another study [15]. In all studies, biochemical controlled disease was the primary outcome, as defined by normal IGF-1 for age and gender and/or GH nadir after OGTT ≤1 μg/L. The biochemical criteria are adopted as the main outcome as therapeutic decision for the need of complementary therapy in acromegaly are usually based on GH and IGF1 measurements performed 3–6 months post-operatively [1, 3, 26].
Our results showed a relative risk of 2.15 (95 % CI 1.39, 3.33) in favor of Pre-SA, meaning that the patients receiving SA at least 3 months before TSS have 22 % less risk to receive a complementary treatment 3 months post-operatively than patients referred to direct surgery.
Concerning timing of outcome measurement, only Shen et al. [16] followed up their patients at 6 and 12 months after TSS. At 6 months, the results were also in favor of Pre-SA, while no difference in the remission rates was observed after 12 months. However, except for patients who received gamma-knife radiotherapy (4/8 in the intervention and 7/18 in the control group), the authors did not give information in relation to other complementary treatments were given for uncontrolled patients in both groups, which might potentially influence the results. Nevertheless, as only this study measured the outcomes 6 months after surgery, remission rates at short term in these patients (even in macroadenoma) deserve some attention, for the reason that IGF1 evaluation at 3 months postoperatively may not completely rule out ongoing effects of the pre-surgery somatostatin analogues.
Our results were similar to a recent systematic review published by Pita-Gutierrez et al. [27]. However, in their review other studies than randomized trials were included (five retrospective and three prospective nonrandomized studies). Although they analyzed separately three selected randomized trials, the study published in 2012 was not included [18]. Moreover, there was no mention about how study quality was assessed. Our review was performed according to the Cochrane Collaboration, including only randomized trials as they are more likely to provide unbiased information than other study designs. In addition, to the best of our knowledge, this is the first systematic review in this field using the GRADE approach.
Applying GRADE approach for no need of complementary treatment 3 months post TSS [28–31], rating down for the risk of bias was not required. Loss of follow-up did not have an important impact in our meta-analysis, since in two trials all participants completed treatment [15, 16]), in one [17] the number of patients who lost follow-up was the same in the study groups and in the other one [18] the lost was less than 6 % and similar in the groups. Despite that the included studies were not blinding for outcomes, they were not subjective and the assessments were not susceptible to bias (only laboratory interpretations). The P value for the test of heterogeneity was <0.0001 and the I2 = 0 %, showing that the quality of evidence for inconsistency was not decreased.
For systematic reviews, precision refers to reviewers’ confidence on the estimates of the intervention effects. If the 95 % CI excludes a relative risk (RR) of 1.0, and the total number of events or patients exceeds the OIS (Optimal Information Size) criteria, precision is adequate. In this review, for the two most important outcomes, the CI excluded a RR of 1.0. However, to meet OIS criteria the required sample size and number of events (assuming α of 0.05 and β of 0.2) for a relative risk reduction of 25 % was approximately 2,000 patients and 325 events, respectively [30]. Therefore, rating down for imprecision was warranted in our systematic review.
Concerning publications bias, the quality of evidence was not reduced because none of included studies were funded by pharmaceutical company; only one study mentioned that the study drug was supplied by Novartis SA [15]. Taking account that a large number of acromegaly patients receive SA therapy for prolonged time, we do not believe that the results of our study have any commercial implication.
None of the included studies evaluated quality of life. So we inferred this outcome for laboratory results. We judged that the absence of GH and IGF1 normalization 3 months after TSS could negatively influence quality life of patients. As this was an indirect association, we rated down two points for indirectness. For the other four factors in deciding on quality of evidence (risk of bias, imprecision, inconsistency and publication bias), the graduation was the same as for no need of complementary treatment 3 months after TSS.
Mortality related to TSS was not evaluated in the included studies. Two studies analyzed duration of postoperative hospital stay and the results were similar between both groups. Similarly, surgical complications in all included studies were not different between the groups. In summary, the quality of evidence of the GRADE system for the no need of complementary therapy 3 months postoperatively in acromegaly in relation to preoperative therapy with SA was moderate.
References
Melmed S, Colao A, Barkan A et al (2009) Guidelines for acromegaly management: an update. J Clin Endocrinol Metab 94:1509–1517. doi:10.1210/jc.2008-2421
Melmed S (2006) Acromegaly. N Engl J Med 355:2558–2573. doi:10.1111/j.1365-2036.2011.04905.x
Vieira Neto L, Abucham J, de Araujo LA et al (2011) Recommendations of Neuroendocrinology Department from Brazilian Society of Endocrinology and Metabolism for diagnosis and treatment of acromegaly in Brazil. Arq Bras Endocrinol Metabol 55:91–105. doi:10.1590/S0004-27302011000200001
Nomikos P, Buchfelder M, Fahlbusch R (2005) The outcome of surgery in 668 patients with acromegaly using current criteria of biochemical “cure”. Eur J Endocrinol 152:379–387. doi:10.1530/eje.1.01863
Wass JA, Turner HE, Adams CB, HE, Adams CB (1999) The importance of locating a good pituitary surgeon. Pituitary 2:51–54
Stevenaert A, Harris AG, Kovacs K, Beckers A (1992) Presurgical octreotide treatment in acromegaly. Metabolism 51–58
Abe T, Lüdecke DK (2001) Effects of preoperative octreotide treatment on different subtypes of 90 GH-secreting pituitary adenomas and outcome in one surgical centre. Eur J Endocrinol 145:137–145. doi:10.1530/eje.0.1450137
Colao A, Ferone D, Cappabianca P et al (1997) Effect of octreotide pretreatment on surgical outcome in acromegaly. J Clin Endocrinol Metab 82:3308–3314. doi:10.1097/00019616-199803000-00020
Barkan AL, Lloyd RV, Chandler WF et al (1988) Preoperative treatment of acromegaly with long-acting somatostatin analog SMS 201-995: shrinkage of invasive pituitary macroadenomas and improved surgical remission rate. J Clin Endocrinol Metab 67:1040–1048
Biermasz NR, van Dulken H, Roelfsema F (1999) Direct postoperative and follow-up results of transsphenoidal surgery in 19 acromegalic patients pretreated with octreotide compared to those in untreated matched controls. J Clin Endocrinol Metab 84:3551–3555
Kristof RA, Stoffel-Wagner B, Klingmüller D, Schramm J (1999) Does octreotide treatment improve the surgical results of macro-adenomas in acromegaly? A randomized study. Acta Neurochir (Wien) 141:399–405. doi:10.1007/s007010050316
The Cochrane Collaboration (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. Version 510 [updated March 2011] Cochrane Collab. www.cochrane-handbook.org
Guyatt GH, Oxman AD, Kunz R et al (2008) What is “quality of evidence” and why is it important to clinicians? BMJ Br Med J 336:995–998. doi:10.1136/bmj.39490.551019.BE
Guyatt G, Oxman AD, Akl EA et al (2011) GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64:383–394. doi:10.1016/j.jclinepi.2010.04.026
Carlsen SM, Lund-Johansen M, Schreiner T et al (2008) Preoperative octreotide treatment in newly diagnosed acromegalic patients with macroadenomas increases cure short-term postoperative rates: a prospective, randomized trial. J Clin Endocrinol Metab 93:2984–2990. doi:10.1210/jc.2008-0315
Shen M, Shou X, Wang Y et al (2010) Effect of presurgical long-acting octreotide treatment in acromegaly patients with invasive pituitary macroadenomas: a prospective randomized study. Endocr J 57:1035–1044. doi:10.1507/endocrj.K10E-203
Mao Z, Zhu Y, Tang H et al (2010) Preoperative lanreotide treatment in acromegalic patients with macroadenomas increases short-term postoperative cure rates: a prospective, randomised trial. Eur J Endocrinol 162:661–666. doi:10.1530/EJE-09-0908
Li Z-Q, Quan Z, Tian H-L, Cheng M (2012) Preoperative lanreotide treatment improves outcome in patients with acromegaly resulting from invasive pituitary macroadenoma. J Int Med Res 40:517–524. doi:10.1177/147323001204000213
Carlsen SM, Svartberg J, Schreiner T et al (2011) Six-month preoperative octreotide treatment in unselected, de novo patients with acromegaly: effect on biochemistry, tumour volume, and postoperative cure. Clin Endocrinol (Oxf) 74:736–743. doi:10.1111/j.1365-2265.2011.03982.x
Losa M, Mortini P, Urbaz L et al (2006) Presurgical treatment with somatostatin analogs in patients with acromegaly: effects on the remission and complication rates. J Neurosurg 104:899–906. doi:10.3171/jns.2006.104.6.899
Plöckinger U, Quabbe H-J (2005) Presurgical octreotide treatment in acromegaly: no improvement of final growth hormone (GH) concentration and pituitary function. A long-term case-control study. Acta Neurochir (Wien) 147:485–493; discussion 493. doi:10.1007/s00701-005-0511-9
Waśko R, Ruchała M, Sawicka J et al (2000) Short-term pre-surgical treatment with somatostatin analogues, octreotide and lanreotide, in acromegaly. J Endocrinol Invest 23:12–18
Ezzat S, Kontogeorgos G, Redelmeier DA et al (1995) In vivo responsiveness of morphological variants of growth hormone-producing pituitary adenomas to octreotide. Eur J Endocrinol 133:686–690. doi:10.1530/eje.0.1330686
Thapar K, Kovacs KT, Stefaneanu L et al (1997) Antiproliferative effect of the somatostatin analogue octreotide on growth hormone-producing pituitary tumors: results of a multicenter randomized trial. Mayo Clin Proc 72:893–900. doi:10.4065/72.10.893
Cannavò S, Squadrito S, Curtò L et al (2001) Effectiveness of slow-release lanreotide in previously operated and untreated patients with GH-secreting pituitary macroadenoma. Horm Metab Res 33:618–624. doi:10.1055/s-2001-17910
Giustina A, Chanson P, Kleinberg D et al (2014) Expert consensus document: a consensus on the medical treatment of acromegaly. Nat Rev Endocrinol 10:243–248. doi:10.1038/nrendo.2014.21
Pita-Gutierrez F, Pertega-Diaz S, Pita-Fernandez S et al (2013) Place of preoperative treatment of acromegaly with somatostatin analog on surgical outcome: a systematic review and meta-analysis. PLoS One. doi:10.1371/journal.pone.0061523
Guyatt GH, Oxman AD, Kunz R et al (2011) GRADE guidelines: 7. Rating the quality of evidence—inconsistency. J Clin Epidemiol 64:1294–1302. doi:10.1016/j.jclinepi.2011.03.017
Guyatt GH, Oxman AD, Kunz R et al (2011) GRADE guidelines: 8. Rating the quality of evidence—indirectness. J Clin Epidemiol 64:1303–1310. doi:10.1016/j.jclinepi.2011.04.014
Guyatt GH, Oxman AD, Kunz R et al (2011) GRADE guidelines 6. Rating the quality of evidence—imprecision. J Clin Epidemiol 64:1283–1293. doi:10.1016/j.jclinepi.2011.01.012
Guyatt GH, Oxman AD, Montori V et al (2011) GRADE guidelines: 5. Rating the quality of evidence—publication bias. J Clin Epidemiol 64:1277–1282. doi:10.1016/j.jclinepi.2011.01.011
Acknowledgments
We thank Dr. Gordon H. Guyatt to help us to apply the GRADE system in this Systematic Review and Dr. Sergio Alberto Rupp de Paiva to motivate us to use the GRADE approach. This work was supported by Sao Paulo State Research Foundation (FAPESP); Grant # 2011/20517-2.
Conflict of interest
V. S. Nunes and C. L. Boguszewski receive consulting fees from Novartis and travel expenses from Ipsen. J. M. S. Correa, M. E. S. Puga and E. M. K. Silva have no relationships to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nunes, V.S., Correa, J.M.S., Puga, M.E.S. et al. Preoperative somatostatin analogues versus direct transsphenoidal surgery for newly-diagnosed acromegaly patients: a systematic review and meta-analysis using the GRADE system. Pituitary 18, 500–508 (2015). https://doi.org/10.1007/s11102-014-0602-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-014-0602-9