Abstract
Background
Coronavirus disease 2019 (COVID-19) is a global pandemic. Hydroxychloroquine (HCQ)-associated cardiovascular adverse events (CVAEs) have been increasingly reported.
Aim
This study aimed to present an observational, retrospective, and comprehensive pharmacovigilance analysis of CVAE associated with HCQ in patients with and without COVID-19 using the US Food and Drug Administration Adverse Events Reporting System (FAERS) data from January 2020 to December 2020.
Method
We identified 3302 adverse event reports from the FAERS database in the year 2020 and divided them into COVID-19 and non-COVID-19 groups, respectively. Then we analyzed whether there were differences in CVAEs between the two groups.
Results
We found that CVAE was higher in cases with COVID-19 compared to those without COVID-19, odds ratio (OR) of 1.26 and a 95% confidence interval (95% CI) of 1.02–1.54. Cases with COVID-19 treated with HCQ exhibited relatively higher proportions of torsade de points (TdP) and QT prolongation (OR 3.10, 95% CI 2.24–4.30), shock-associated TdP (OR 2.93, 95% CI 2.13–4.04), cardiac arrhythmias (OR 2.07, 95% CI 1.60–2.69), cardiac arrhythmia terms (including bradyarrhythmias and tachyarrhythmias) (OR 2.15, 95% CI 1.65–2.80), bradyarrhythmias (including conduction defects and disorders of sinus node function) (OR 2.56, 95% CI 1.86–3.54), and conduction defects (OR 2.56, 95% CI 1.86–3.54).
Conclusion
Our retrospective observational analysis suggested that the proportion of CVAE associated with HCQ, especially TdP and QT prolongation, was higher in patients with COVID-19. Understanding the effects of COVID-19 on the cardiovascular system is essential to providing comprehensive medical care to patients receiving HCQ treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impact statements
-
The data mining approach can be used to analyze drug-associated adverse events based on real-world FAERS data.
-
HCQ remains an old and safe drug. The results suggest that future studies on the mechanism of drug–disease interaction between HCQ and virus infection or the cardiovascular effects of viruses such as COVID-19 are needed.
-
The results suggest we should be more cautious when designing protocols for unknown infectious viral diseases when considering HCQ regimens.
Introduction
Hydroxychloroquine (HCQ) and chloroquine (CQ) are 4-aminoquinoline antimalarial drugs. Since its approval, granted by the US Food and Drug Administration (FDA) in 1955, HCQ has become a commonly prescribed drug for treating malaria, rheumatoid arthritis, and systemic lupus erythematosus, with a better safety profile than CQ [1]. Recently, several studies have examined HCQ and CQ as antiviral drugs in severe acute respiratory syndrome (SARS) and human immunodeficiency virus (HIV) infections [2, 3].
There were 524 million confirmed cases of coronavirus disease 2019 (COVID-19) caused by SARS coronavirus 2 (SARS-CoV-2) on May 19, 2022, and 6 million died [4]. No specific treatments for COVID-19 were available at the beginning of the global pandemic. HCQ and CQ demonstrated antiviral properties in an early in vitro study [5, 6] and received the FDA emergency use authorization for COVID-19 in March 2020 [7, 8]. However, in light of ongoing serious cardiac adverse events (CVAE) and other serious adverse effects, the known and potential benefits of HCQ no longer outweigh the known and potential risks for authorized use. Thus, the FDA revoked the emergency authorization on June 20, 2020 [9,10,11]. HCQ was known to affect the cardiovascular system upon its approval [1]. Meanwhile, some drug safety surveillance reports mentioned that HCQ use was associated with a higher CVAE reporting rate [12, 13]. HCQ was shown to significantly increase CVAEs by a modest adjusted odds ratio (OR) of 1.22 (95% confidence interval CI 1.18–1.25) [12]. However, few studies have assessed HCQ safety in COVID-19 patients over the past year [13,14,15].
As a classic antimalarial and antirheumatic drug, HCQ has been used relatively safely for nearly 67 years [1]. CVAEs caused by HCQ are important considerations in clinical practice, especially when HCQ is combined with other cardiotoxic drugs, such as remdesivir, lopinavir/ritonavir, arbidol, or azithromycin. Routine ECG monitoring is recommended in such cases [7, 8]. It is critical to elucidate whether HCQ is less safe for COVID-19 patients, whether CVAEs are attributed only to HCQ, or if the incidences and severity degrees of CVAEs are potentially affected by the presence of SARS-CoV-2. The answers to these questions can be obtained by examining possible CVAEs associated with HCQ in patients with and without COVID-19 and the relative proportions of CVAEs in the two groups.
To date, a sufficient number of outcomes in COVID-19 patients have been accumulated in real-world practice. The FDA Adverse Event Reporting System (FAERS) database is one of the largest open spontaneous reporting systems with many adverse events (AE) reports. It is an excellent source for post-marketing pharmacovigilance analysis [16]. FAERS reports can be quantitatively analyzed using data mining techniques to identify possible associations between drugs and AEs [16].
Aim
The study aimed to evaluate and characterize CVAEs associated with HCQ in patients with or without COVID-19 through an observational, retrospective pharmacovigilance analysis.
Ethics approval
The FAERS database contains anonymized patient information. The Ethics Committee of the West China Hospital has confirmed that no ethical approval was required.
Method
Data source
A total of 68 quarterly datasets of the AE reports (January 2004 to December 2020) were downloaded from FAERS [17]. Each quarterly data file consisted of the following seven tables: demographic and administrative information (DEMO), adverse events (REAC), drug and biological information (DRUG), patient outcomes (OUTC), indications of drug administration (INDI), therapy start and end dates for reported drugs (THER), and report sources (RPSR). Both the AEs in the REAC table and the indications in the INDI table were coded by the Medical Dictionary for Regulatory Activities (MedDRA). All data were managed using Microsoft SQL Server 2017 software.
Duplicate DEMO records were removed. For reports with the same CASE number (CASEID), the most recent report date (FDA_DT) in the “DEMO” table was selected. For reports with the same CASE and FDA_DT values, the one with the highest ISR number (a unique number for identifying an AE report) was selected.
Study design and inclusion/exclusion criteria
Identifying HCQ-related cases: different HCQ drug names were transformed into generic names using MedEx software (MedEx UIMA 1.3.7, Vanderbilt University, USA) [18]. We then restricted the drug role to the primary suspected drug in the DRUG table and linked it to the DEMO table by CASEID to obtain HCQ-related cases. To make the evaluation more accurate, we excluded patients with pre-existing cardiovascular diseases using the Standardized MedDRA Queries (SMQ, version 23.1) narrow search, including 23 SMQ terms and 334 Preferred Terms (Supplemental Table S1). Taking into account the risk of bias caused by different reporting trends and safety culture during the long period of 2004–2020 and the SARS-CoV-2 outbreak at the end of 2019, we excluded cases before 2020 (identified by the reporting time). The remaining cases were analyzed in the present study. After identifying the HCQ case, we further divided HCQ cases into the COVID-19 and non-COVID-19 groups and investigated whether there were differences in the characteristic parameters of CVAEs. We identified COVID-19 cases using an SMQ narrow search (SMQ coded 20000237) (Supplemental Table S1), including 18 Preferred Terms.
The outcome indicator was whether CVAE was reported among HCQ-related cases. CVAE cases in both groups were also identified by an SMQ narrow search (Supplemental Table S1). Additionally, the time to event was further calculated using the event date of the DEMO table and the start date of drug therapy. We excluded cases with a start date later than the event date. The prognosis analysis of included cases related to HCQ, such as death, life-threatening condition, hospitalization, disability, and other serious events, was analyzed. Common concomitant drugs and the potential impact of combination therapy were analyzed.
Statistical analysis
We used OR and 95% CI values to compare the proportion of CVAEs in the COVID-19 and non-COVID-19 groups. Continuous variables were reported as mean ± standard deviation or median and compared using Student’s t-test or the Mann–Whitney U test. Categorical variables were compared using the χ2 test or Fisher’s exact test. We then performed a propensity score matching (PSM) analysis to balance variables between groups. The 1:1 PSM analysis was performed using the PSM model of SPSS software. It included variables available from FAERS such as patient sex, age group, country of occurrence, and type of reporter. These were sampled without replacement. Both exact and fuzzy matches were used for the optimal matching with a matching tolerance of 0.001 [19, 20]. The missing data were treated as an independent classification. The effects were considered statistically significant when P < 0.05. All statistical analyses were performed using SPSS software (version 25.0; IBM Corporation, Armonk, New York, USA).
Results
Case identification in FAERS
After filtering, 12,875,561 AE cases were retained. A total of 9885 HCQ-associated AE cases were obtained, and 299 with pre-existing cardiovascular disease complications and 6284 before 2020 were excluded. Finally, we identified 3302 AE cases associated with HCQ, including 1824 cases with COVID-19 diagnosis (COVID-19 group) and 1478 cases without COVID-19 diagnosis (non-COVID-19 group), with 262 and 174 CVAE cases in each group, respectively (Fig. 1).
Analysis of HCQ AE case characteristics
The characteristics of the included HCQ AE cases are listed in Table 1. After PSM was performed by patient sex, age group, country of occurrence, and reporter type with 0.001 tolerance, 1620 cases were collected.
CVAE analysis associated with HCQ
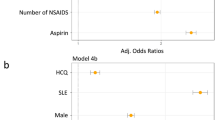
The HCQ-associated CVAEs were higher in the COVID-19 group than in the non-COVID-19 group (OR 1.26, 95% CI 1.02–1.54, P = 0.030). After PSM, the difference was not significant (OR 1.21, 95% CI 0.92–1.58, P = 0.193) (Table 2). Then we performed further comparisons of HCQ-associated CVAEs based on each SMQ term (Supplemental Table S1). The ORs of six CVAEs, “Torsade de Pointes (TdP)/QT prolongation” (OR 3.10, 95% CI 2.24–4.30, P < 0.001), “TdP, shock-associated conditions” (OR 2.93, 95% CI 2.13–4.04, P < 0.001), “Cardiac arrhythmias” (OR 2.07, 95% CI 1.60–2.69, P < 0.001), and the next level of “Cardiac arrhythmias,” “Cardiac arrhythmia terms (including bradyarrhythmias and tachyarrhythmias)” (OR 2.15, 95% CI 1.65–2.80, P < 0.001), “Bradyarrhythmias (including conduction defects and disorders of sinus node function)” (OR 2.56, 95% CI 1.86–3.54, P < 0.001), and “Conduction defects” (OR 2.56, 95% CI 1.86–3.54, P < 0.001) were significantly higher within COVID-19 groups compared to non-COVID-19 groups. However, the ORs of two CVAEs, “Cardiac failure” (OR 0.27, 95% CI 0.14–0.55, P < 0.001), and “Cardiomyopathy” (OR 0.12, 95% CI 0.06–0.26, P < 0.001), were significantly lower within COVID-19 groups compared to non-COVID-19 groups. After PSM, the differences were still significant (Fig. 2). The detailed data are provided in Supplemental Table S2.
Comparison of HCQ-associated CVAEs in detail in patients with or without COVID-19 based on SMQ narrow search. CVAE cardiovascular adverse event, OR odds ratio, CI confidence interval, PSM propensity score matching, TdP/QTp Torsade de Pointes/QT prolongation, TdPs shock-associated Torsade de Pointes, CA cardiac arrhythmia, CA_B/T Cardiac arrhythmia terms (including bradyarrhythmias and tachyarrhythmias), CA_B/T_B bradyarrhythmias (including conduction defects and disorders of sinus node function), CA_B/T_B_C conduction defects, CA_B/T_T tachyarrhythmias (including supraventricular and ventricular tachyarrhythmias), CA_B/T_T_S supraventricular tachyarrhythmias, CA_B/T_T_V ventricular tachyarrhythmias, CA_B/T_T_N nonspecific tachyarrhythmia terms, CA_B/T_N nonspecific cardiac arrhythmia terms, CA_CN congenital and neonatal arrhythmias, CSs shock-associated circulatory or cardiac conditions (excluding torsade de pointes), IHD ischaemic heart disease, IHD_MI myocardial infarction, IHD_O other ischaemic heart disease, HBP Hypertension, CF cardiac failure, CMP cardiomyopathy
Time to onset of CVAE associated with HCQ
There were 638 HCQ-associated AE cases with sufficient time data for further analysis, including 505 in the non-COVID-19 group (20 CVAE cases) and 133 in the COVID-19 group (9 CVAE cases). The mean time to the occurrence of CVAE in the non-COVID-19 group was 1.49 ± 2.37 years. For the nine CVAE cases in the COVID-19 group, the time interval analysis showed that all CVAEs occurred on the day of HCQ administration, including shock-associated TdP in seven cases, one heart failure, and one conduction dysfunction.
AE prognosis analysis
The prognoses of HCQ-associated AEs in patients with and without COVID-19 were analyzed in 2974 cases (Table 3). Compared to the non-COVID-19 group, the COVID-19 group had a significantly lower proportion of CVAE death cases (OR 0.41, 95% CI 0.22–0.78, P = 0.008). However, the proportion of other severe outcomes of AE was not significantly different between the groups (OR 1.16, 95% CI 0.89–1.41, P = 0.379).
Concomitant drugs
The number of co-administered drugs was significantly different between the two groups: 3.94 ± 3.46 in the COVID-19 group and 6.67 ± 8.39 in the non-COVID-19 group (P < 0.05). The top five concomitant drugs in the non-COVID-19 group were glucocorticoids (764, 51.69%), methotrexate (568, 38.43%), leflunomide (326, 22.06%), adalimumab (249, 16.85%), and etanercept (240, 16.24%). In contrast, the top five concomitant drugs were azithromycin (782, 42.87%), glucocorticoids (491, 26.92%), lopinavir and ritonavir (488, 26.75%), tocilizumab (366, 20.07%), and ceftriaxone (319, 17.49%) in the COVID-19 group (Supplemental Table S3).
In addition, we analyzed and compared the effect of combination therapy on CVAE in both groups (Supplemental Table S4). For cases in which HCQ was co-administered with azithromycin (the most common co-prescribed drug in patients with COVID-19), the proportion of CVAE was significantly lower in the COVID-19 group compared to that in the non-COVID-19 group (OR 0.34, 95% CI 0.18–0.63, P = 0.001).
Discussion
Our study provides new evidence for the differences in the distribution of HCQ-associated CVAEs between COVID and non-COVID patients by investigating the characteristics of spontaneous AE reports in the FAERS database. We discovered significant differences in sex, age group, country of occurrence, and reporter occupation, between patients with and without COVID-19, which were consistent with the epidemiological characteristics of the diseases. The use of HCQ as an anti-rheumatic drug has been associated with AEs more frequently in females than in males, which aligns with the characteristics of rheumatic diseases. However, in our analysis, more male patients (51.75%) were infected with COVID-19. The gender distribution of reports was consistent with the epidemiological characteristics of COVID-19 [21]. Therefore, more men might be prone to receiving HCQ treatment for COVID-19 and report HCQ-related AEs. As an open, spontaneous reporting system, non-healthcare professionals accounted for a large proportion of reporters in FAERS [22]. We found that more healthcare providers reported HCQ-related AEs after the COVID-19 pandemic, which increased the credibility of these reports.
We found that CVAE associated with HCQ was slightly higher in COVID-19 patients (OR 1.26, P = 0.030). According to the subgroup analysis, the COVID-19 group had significantly higher risks of TdP and QT prolongation associated with HCQ treatment than the non-COVID-19 group (OR 3.10, P < 0.001). The current real-world data mining results were consistent with our hypothesis that COVID-19 might play a critical role in CVAEs associated with HCQ. In other words, some pathological processes triggered by COVID-19 could exacerbate the reaction to HCQ or HCQ-containing regimens in patients with COVID-19 [23]. For example, other drugs extending the QT interval are often prescribed with HCQ [24].
On the contrary, the proportions of “Cardiac failure” and “Cardiomyopathy” associated with HCQ treatment were significantly lower in the COVID-19 group than in the non-COVID-19 group. This observation is different from other studies [23, 25, 26]. Our findings indicate that when HCQ is used in patients with COVID-19, the adverse events of heart failure or cardiomyopathy may be less concern. Of course, our results might be limited by the number of cases analyzed.
Although the time data were limited in the present study, among the nine CVAE cases with time data in the COVID-19 group, seven suffered shock-associated TdP. In these seven TdP cases, four patients received HCQ and azithromycin combination therapies. Regarding the onset, all instances of CVAEs in the non-COVID-19 group occurred years after HCQ administration. On the contrary, CVAEs happened on the day of HCQ treatment in the COVID-19 group. The difference could be attributed to the fact that medical professionals paid particular attention to the safety of HCQ and carefully observed patients during the treatment of COVID-19.
The prognosis analysis showed that the proportion of CVAE death cases in the COVID-19 group was significantly lower than in the non-COVID-19 group, OR 0.41. However, this does not necessarily imply a better prognosis of CVAE associated with HCQ in the COVID-19 group. Many factors could influence the outcome, including timely management by healthcare professionals. The higher prevalence of healthcare professionals among those who reported CVAEs in the COVID-19 group corroborates this notion. Of course, we cannot rule out that the prognosis for CVAE in COVID-19 patients might be better, and further evaluation may be necessary.
The risk of AE was approximately 1.20–4.08 fold higher in HCQ-treated patients than in the control group (without HCQ regimen) [27,28,29]. One systematic review and meta-analysis found that the mortality difference was not significant, neither in the HCQ treatment group (relative risk RR 0.86, 95% CI 0.71–1.03) nor in the HCQ plus azithromycin treatment group (RR 1.28, 95% CI 0.76–2.14) in comparison to controls [27]. In our study, we found that the distribution of concomitant drugs was consistent with the indications for which HCQ was approved and the recommendations of treatment guidelines for the respective diseases from the FDA, the World Health Organization, and the China National Health Commission [7, 8]. We found a significant increase in azithromycin use among COVID-19 patients who reported AEs. The drug combinations could lead to potential drug-drug interactions and the outbreak of reports about the unsafe use of HCQ [14, 24, 30, 31]. Interestingly, we found that the proportion of CVAEs developed after combining azithromycin and HCQ in the COVID group was lower than in the non-COVID group (OR 0.34, P = 0.001). The results could mean that when HCQ and azithromycin were co-administered in COVID-19 patients, we should probably be more concerned about non-CVAEs rather than CVAEs.
Our pharmacovigilance study has several limitations. First, our data source was from the spontaneous reporting system, a voluntary reporting platform open to the public. The incompleteness of the data, underreporting, overreporting, and missing information are inevitable [32]. Our results could be biased by unmeasured confounding factors. Although PSM was performed, identifying and adjusting all risk factors could not be fully achieved. Furthermore, the temporality of events, i.e., exposure to HCQ and infection to SARS-Cov-2, was unclear in the cases analyzed. Therefore, our study does not provide sufficient evidence on the causality and merely suggests the necessity for well-organized clinical studies concerning the associations observed. More research is needed to understand the epidemiological and pathophysiological basis of the interactions between CVAE and COVID-19, which might affect the link between CVAEs and HCQ use.
Conclusion
Understanding the impact of COVID-19 on the cardiovascular system is essential to providing comprehensive medical care to patients receiving HCQ treatment. We found that the proportion of CVAE (especially TdP and QT prolongation) associated with HCQ in COVID-19 patients was higher than in non-COVID patients. The proportions and characteristics of CVAE in COVID patients could not be explained solely by adverse drug effects but were likely influenced by the COVID-19 pathology. Although HCQ is no longer used to treat COVID-19, many HCQ-related studies are ongoing. Our study suggests that we should be more cautious when designing protocols for unknown infectious viral diseases when considering HCQ regimens. Future studies on the mechanism of drug–disease interaction between HCQ and virus infection or the cardiovascular effects of viruses such as COVID-19 are needed.
References
Concordia Pharmaceuticals Inc. Product monograph: Plaquenil® (Hydroxychloroquine sulfate Tablets). 2019. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/009768Orig1s051lbl.pdf. Accessed 5 May 2022.
Savarino A, Boelaert JR, Cassone A, et al. Effects of chloroquine on viral infections: an old drug against today’s diseases? Lancet Infect Dis. 2003;3(11):722–7.
Rolain JM, Colson P, Raoult D. Recycling of chloroquine and its hydroxyl analogue to face bacterial, fungal and viral infections in the 21st century. Int J Antimicrob Agents. 2007;30(4):297–308.
World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2022. Available at https://covid19.who.int/table. Accessed 20 May 2022.
Wang M, Cao R, Zhang L, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–71.
Devaux CA, Rolain JM, Colson P, et al. New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19? Int J Antimicrob Agents. 2020;55(5):105938.
US Food And Drug Administration. Authorization letter: Chloroquine phosphate and hydroxychloroquine sulfate for treatment of COVID-19. 2020. https://www.fda.gov/media/136534/download. Accessed 20 Mar 2022.
National Health Commission of the People's Republic of China. COVID-19 Diagnosis and Treatment Protocol (Trial Version 8, Revised Version). 2021. http://www.nhc.gov.cn/yzygj/s7653p/202104/7de0b3837c8b4606a0594aeb0105232b.shtml. Accessed 12 Mar 2022.
US Food And Drug Administration. Revocation letter: Chloroquine phosphate and hydroxychloroquine sulfate for treatment of COVID-19. 2020. https://www.fda.gov/media/138945/download. Accessed 20 Mar 2022.
Gautret P, Lagier JC, Honoré S, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open label non-randomized clinical trial revisited. Int J Antimicrob Agents. 2021;57(1):106243.
Gautret P, Lagier JC, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;56(1):105949.
Cohen IV, Makunts T, Moumedjian T, et al. Cardiac adverse events associated with chloroquine and hydroxychloroquine exposure in 20 years of drug safety surveillance reports. Sci Rep. 2020;10(1):19199.
Goldman A, Bomze D, Dankner R, et al. Cardiovascular adverse events associated with hydroxychloroquine and chloroquine: a comprehensive pharmacovigilance analysis of pre-COVID-19 reports. Br J Clin Pharmacol. 2021;87(3):1432–42.
Diaby V, Almutairi RD, Chen Z, et al. A pharmacovigilance study to quantify the strength of association between the combination of antimalarial drugs and azithromycin and cardiac arrhythmias: implications for the treatment of COVID-19. Expert Rev Pharmacoecon Outcomes Res. 2021;21(1):159–68.
Dauner DG, Dauner KN. Summary of adverse drug events for hydroxychloroquine, azithromycin, and chloroquine during the COVID-19 pandemic. J Am Pharm Assoc (2003). 2021;61(3):293–8.
US Food And Drug Administration. Data Mining at FDA: White Paper (2018). 2018. https://www.fda.gov/science-research/data-mining/data-mining-fda-white-paper. Accessed 20 Mar 2022.
US Food And Drug Administration. FDA Adverse Event Reporting System (FAERS) Quarterly Data Extract Files. 2021. https://fis.fda.gov/extensions/FPD-QDE-FAERS/FPD-QDE-FAERS.html. Accessed 21 Apr 2021.
Wu B, Hu Q, Tian F, et al. A pharmacovigilance study of association between proton pump inhibitor and dementia event based on FDA Adverse Event Reporting System data. Sci Rep. 2021;11(1):10709.
Yao XI, Wang X, Speicher PJ, et al. Reporting and guidelines in propensity score analysis: a systematic review of cancer and cancer surgical studies. J Natl Cancer Inst. 2017;109(8):djw323.
Johnson SR, Tomlinson GA, Hawker GA, et al. Propensity score methods for bias reduction in observational studies of treatment effect. Rheum Dis Clin North Am. 2018;44(2):203–13.
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506.
Chen C, Wu B, Zhang C, et al. Immune-related adverse events associated with immune checkpoint inhibitors: an updated comprehensive disproportionality analysis of the FDA adverse event reporting system. Int Immunopharmacol. 2021;95:107498.
Talasaz AH, Kakavand H, Van Tassell B, et al. Cardiovascular complications of COVID-19: pharmacotherapy perspective. Cardiovasc Drugs Ther. 2021;35(2):249–59.
Anupama BK, Adhikari S, Chaudhuri D. Prolonged QT interval in a patient with coronavirus disease-2019: beyond hydroxychloroquine and azithromycin. J Investig Med High Impact Case Rep. 2020;8:2324709620948407.
Bader F, Manla Y, Atallah B, et al. Heart failure and COVID-19. Heart Fail Rev. 2021;26(1):1–10.
Weckbach LT, Curta A, Bieber S, et al. Myocardial inflammation and dysfunction in COVID-19-associated myocardial injury. Circ Cardiovasc Imaging. 2021;14(1): e012220.
Shamshirian A, Hessami A, Heydari K, et al. The role of hydroxychloroquine in COVID-19: a systematic review and meta-analysis. Ann Acad Med Singap. 2020;49(10):789–800.
Hussain N, Chung E, Heyl JJ, et al. A meta-analysis on the effects of hydroxychloroquine on COVID-19. Cureus. 2020;12(8):e10005.
Wright C, Ross C, Mc GN. Are hydroxychloroquine and chloroquine effective in the treatment of SARS-COV-2 (COVID-19)? Evid Based Dent. 2020;21(2):64–5.
Sisti G, Schiattarella A, Sisti A. Treatment of COVID-19 in pregnancy with hydroxychloroquine and azithromycin: a case report. Acta Biomed. 2020;91(4):e2020123.
Mitra RL, Greenstein SA, Epstein LM. An algorithm for managing QT prolongation in coronavirus disease 2019 (COVID-19) patients treated with either chloroquine or hydroxychloroquine in conjunction with azithromycin: possible benefits of intravenous lidocaine. HeartRhythm Case Rep. 2020;6(5):244–8.
Sakaeda T, Tamon A, Kadoyama K, et al. Data mining of the public version of the FDA adverse event reporting system. Int J Med Sci. 2013;10(7):796–803.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
This research was funded by the National Key Research and Development Program of China (Grant No. 2020YFC2008302). The sponsor had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Luo, M., Wu, B., Li, Y. et al. An observational, retrospective, comprehensive pharmacovigilance analysis of hydroxychloroquine-associated cardiovascular adverse events in patients with and without COVID-19. Int J Clin Pharm 44, 1179–1187 (2022). https://doi.org/10.1007/s11096-022-01457-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-022-01457-w