Abstract
Background Information on the extent of high-risk prescribing for nonsteroidal anti-inflammatory drugs (NSAIDs) across developing countries is scarce. Objectives This study examines the prescribing pattern for NSAIDs in primary care, assesses the extent of high-risk NSAIDs prescribing and identifies associated factors. Setting 129 public and 416 private primary care clinics in Malaysia. Methods Data were derived from the National Medical Care Survey 2014, a cross-sectional survey on primary care morbidity patterns and clinical activities in Malaysia. Types of NSAIDs, indications for NSAIDs use and proportion of high-risk NSAIDs prescribing were assessed. Factors associated with high-risk NSAIDs prescribing were identified with a multivariable logistic regression. Weighted results, adjusted for sampling design and non-response were presented. Main outcome measures Prescribing pattern of NSAIDs, proportion of high-risk NSAIDs prescribing and its associated factors. Results Among the 55,489 patients who received NSAIDs, diclofenac was the most frequently prescribed NSAID (40.5%, 95% CI 40.1–40.9%), followed by mefenamic acid (29.2%, 95% CI 28.8–29.6%). The commonest indications for NSAIDs use were musculoskeletal condition and respiratory tract infection, both at 17.8% (95% CI 17.4–18.1%). A total of 22.9% (95% CI 22.6–23.3%) patients received high-risk NSAID prescriptions. Of these, 47.8% (95% CI 46.9–48.7%) did not receive adequate gastroprotection despite being at risk, 24.8% (95% CI 24.0–25.5%) were prescribed NSAIDs despite having cardiovascular comorbidities and 22.4% (95% CI 21.7–23.2%) were prescribed high-dose NSAIDs. The odds of receiving high-risk NSAID prescriptions increased with the number of drugs prescribed (OR 1.23, 95% CI 1.06–1.43) and the number of diagnoses in one visit (OR 2.21, 95% CI 1.71–2.86). The odds of being prescribed high-risk NSAID prescriptions were lower in patients with secondary (OR 0.52, 95% CI 0.35–0.77) and tertiary education (OR 0.39, 95% CI 0.22–0.68) compared to patients without formal education. Patients’ citizenship, indication for NSAID prescriptions and whether a medical certificate was issued were also significantly associated with the likelihood of receiving high-risk NSAID prescriptions. Conclusions A quarter of NSAIDs prescribed in Malaysian primary care setting is categorised as high-risk prescribing. Targeted strategies are necessary to improve patient safety.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
Patients should be informed of the benefits and harms of NSAIDs through public health awareness campaigns, and be empowered to enquire about the treatment they receive as well as be actively involved in treatment decision making.
-
A constant review on safety of NSAIDs use or a safer alternative to NSAIDs is important, especially in patients who are on NSAIDs regularly and are at high risk of adverse effects from NSAIDs.
-
Establishing practice management software applications such as computerised design support systems with drug interaction alerts, drug monitoring reminders and patient information sharing among prescribers and pharmacists to guide prescribers in decisions to prescribe NSAIDs may potentially reduce initiations of high-risk NSAID prescriptions.
-
Routine use of NSAIDs for acute respiratory tract infections is questionable. Reasons of its use and outcomes from this treatment should be explored.
Introduction
Patient safety in relation to drug use in primary care is an area of increasing concern. About 50% of hospital admissions from preventable drug-related morbidity were caused by four drug classes; NSAIDs being one of them [1]. Despite their usefulness, NSAIDs are long known for their adverse effects, with the main risk being upper gastrointestinal bleeding. In the United States, over 100,000 hospitalisations and 16,500 deaths from NSAID-related gastrointestinal complications are reported annually [2]. Besides caution in the use among people with asthma and chronic kidney disease [3], NSAIDs usage is associated with an increased risk of cardiovascular events, in particular with diclofenac [4].
Adverse drug effects from NSAIDs are largely preventable and is often related to the extent of its prescription and use of other drugs. High-risk prescribing is defined as drug prescribing by healthcare professionals where significant risk of harm to patients is evident and the prescription should either be avoided or monitored regularly for its appropriateness [5]. Among developed countries, about 24.4–30% of primary care patients were prescribed NSAIDs, with rates of high-risk NSAIDs prescribing ranging from 7 to 16% [6,7,8,9]. In low and middle-income regions however, limited information is available on the utilisation pattern of NSAIDs and the extent of its high-risk prescribing. In Malaysia, a study from a public primary care clinic showed that more than one-third of patients who visited the clinic received at least one NSAID and of these, 6.6% had potential prescription-related problems [10]. Primary care in Malaysia is provided by both public and private sectors. Having representative data from both sectors would gain more accurate estimates on the extent of NSAIDs use in Malaysia.
Aim of the study
This study aims to determine the prescribing pattern of NSAIDs in the Malaysian primary care setting, to assess the extent of high-risk NSAIDs prescribing and to identify factors associated with it by deploying data from a nationally representative survey.
Ethics approval
Ethics approval for the National Medical Care Survey (NMCS), the larger survey where data of this study were retrieved from was obtained from the Medical Research and Ethics Committee, Ministry of Health Malaysia (ID: NMRR-09-842-4718).
Methods
Data source
This analysis utilised data from a larger study, the NMCS. In brief, NMCS was a national survey designed to quantify morbidity patterns and clinical activities in the primary care setting [11]. A total of 139 out of 911 public and 1002 out of 5646 private clinics were randomly sampled from all 13 states and 3 federal territories in Malaysia using cluster random sampling, stratified by states and sectors. In total, a response rate of 92.8% (n = 129) was achieved for public clinics and 41.5% (n = 416) from private clinics.
Each clinic was assigned a random date for data collection between January and May 2014. On the allocated date, prescribers were asked to document data on every patient’s sociodemographic characteristics, reasons for seeking medical care, diagnoses made, prescriptions provided, types of investigations, procedures and counselling performed, and whether follow-ups were provided. Diagnoses and reasons for visits were coded using International Classification of Primary Care, Second Edition (ICPC-2) [12] while drugs were coded using the Anatomical Therapeutic Chemical (ATC) Classification [13].
Participant selection
In this study, we included patients who were prescribed at least one systemic NSAID, comprising of non-selective NSAIDs and selective Cox-2 inhibitors (or coxibs). Nonsteroidal anti-inflammatory drugs (NSAIDs) were defined as ATC codes of M01A except M01AX (glucosamine and chondroitin sulfate).
Criteria for high-risk prescribing
As most guidelines address the use of NSAIDs specifically within certain conditions, we compiled the operational criteria of high-risk NSAIDs prescribing for this study from several international guidelines [3, 14,15,16,17]. The criteria are listed in Table 1.
Determinant measures
Parameters for analysis were identified from different levels. Patient-level factors included (1) demographic characteristics: sex, ethnicity, citizenship and educational level, (2) type of clinics visited: public or private, (3) number of concurrent diagnoses and prescribed drugs, (4) indications for NSAID prescriptions, and (5) whether a medical certificate was issued or not. Issuance of a medical certificate was used as a proxy for the severity of a condition. Patient’s age was incorporated as part of the outcome measure for high-risk prescribing. Prescribers and clinic-level factors included (1) prescribers’ characteristics: age, sex, years of experience in primary care, qualification, average weekly working hours, place of graduation and (2) clinic-related factors: group or solo practice, location, availability of electronic medical records (EMR) and number of daily attendances.
Statistical analysis
First, numbers and proportions were derived for types of NSAIDs prescribed, indications for prescriptions and extent of high-risk prescribing for each criterion. Weighted results were presented, adjusting for sampling design and non-response.
Second, a multivariable logistic regression adjusted for complex survey design was performed to determine relevant factors that influenced the likelihood of receiving high-risk NSAID prescriptions with the operational criteria stated. Odds ratios with the corresponding 95% confidence intervals were reported. Significance level was set at p < 0.05.
Third, the extent of missing data was assessed. Proportion of missing data ranged from 0.4% for age to 25% for whether a medical certificate was issued. Missing data was imputed using multiple imputation by chained equations (MICE) with m = 10 to minimise loss of statistical power and bias [18].
Statistical analysis was performed with Stata SE Version 15 (StataCorp LP, College Station, TX).
Results
From the NMCS survey, 17.0% (n = 55,489) of patients received at least one NSAID at their primary care visit. Table 2 shows the largest proportion of NSAIDs prescribing was for the age groups between 20 and 64 years (81.5%). The majority of those who received NSAIDs were Malaysian (89.9%), of Malay ethnicity (61.1%) and had secondary education and above (75.4%). Eighty-six percent of the patients were treated at private clinics. A total of 64.6% were prescribed with 3 drugs or more and 80.7% of the patients had a single diagnosis during the visit.
Among the 6348 prescribers, median age was 46.0 years with a median duration of practice in primary care of 13.5 years (Table 2). The median weekly working hours for the prescribers was 45.9 h. The majority of the prescribers were medical doctors (92.5%). Most of the NSAIDs were prescribed from solo practices (68.1%), urban clinics (86.3%), clinics that did not use electronic medical records (72.9%), and clinics that had median daily attendances of 40 patients.
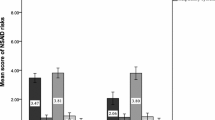
Figure 1 shows that the top 3 NSAIDs prescribed were diclofenac (40.5%, 95% CI 40.1–40.9%), mefenamic acid (29.2%, 95% CI 28.8–29.6%) and ibuprofen (9.3%, 95% CI 9.1–9.6%). Use of coxibs was low: 2.6% (95% CI 2.5–2.7%) for etoricoxib and 2.4% (95% CI 2.3–2.6%) for celecoxib. Musculoskeletal symptom/condition and respiratory tract infection (RTI) were the two main indications for NSAID prescriptions (17.8%, 95% CI 17.4–18.1%) and followed by injury (13.2%, 95% CI 12.9–13.4%) (Fig. 2).
Types of NSAIDs prescribed among primary care attendees in Malaysia (n = 60853b). Error bar denotes 95% CI of the proportion of NSAIDs. aOther NSAIDs include acemetacin, ketorolac and tenoxicam. bTotal number of NSAIDs prescribed. Abbreviations NSAIDs nonsteroidal anti-inflammatory drugs, CI confidence intervals
Indications for prescription of NSAIDs among primary care attendees in Malaysia (n = 55489d). Error bar denote 95% CI of the proportion of NSAID indications. Abbreviations NSAIDs nonsteroidal anti-inflammatory drugs, CI confidence intervals. aInjury includes, but is not limited to fractures, sprains, strains, burns and lacerations. bSkin symptom/condition includes, but is not limited to abscesses, cellulitis, skin infections and ulcers. cOral symptom/condition includes, but is not limited to mouth ulcers, tooth and gum-related conditions. dThe main indication was chosen for patients with more than one indications
Out of 55,489 patients who received NSAIDs, 12,728 patients (22.9%, 95% CI 22.6–23.3%) were categorised as receiving high-risk NSAID prescriptions. Table 3 shows the proportion of high-risk NSAIDs prescribing by criterion. Inadequate gastroprotection was the most common criterion (47.8%, 95% CI 46.9–48.7%), followed by concurrent use of NSAIDs with risk factors for coronary heart disease (24.8%, 95% CI 24.0–25.5%), prescription of high dose NSAIDs (22.4%, 95% CI 21.7–23.2%) and concurrent prescription of two or more NSAIDs (18.4%, 95% CI 17.8–19.1%). A small percentage (2.1%, 95% CI 1.8–2.3) of patients received a combination of NSAIDs, ACE-inhibitors or ARBs and diuretics.
Among the 6286 patients who were at risk of gastrointestinal bleed, 81.6% had no gastroprotection, 15.2% received inadequate gastroprotection which include antacids (7.8%), standard dose H2-receptor antagonist (7.2%), or other drugs (0.2%) and only 3.2% received proton-pump inhibitors or double-dose H2-receptor antagonists (percentages not shown in the tables).
Table 4 shows that Malaysians had two times higher odds (OR 2.00, 95% CI 1.02–3.92) of being prescribed high-risk NSAIDs compared to non-Malaysians. The odds of receiving high-risk NSAID prescriptions increased with the number of drugs prescribed (OR 1.23, 95% CI 1.06–1.43) and number of diagnoses a patient had in the visit (OR 2.21, 95% CI 1.71–2.86). High-risk NSAID prescriptions were more prevalent among patients who had musculoskeletal symptom/condition (OR 2.07, 95% CI 1.53–2.79). Patients with secondary (OR 0.52, 95% CI 0.35–0.77) and tertiary education (OR 0.39, 95% CI 0.22–0.68) had lower odds of being given high-risk NSAID prescriptions compared to patients without formal education. The odds of receiving high-risk NSAID prescriptions were lower among those given medical certificate (OR 0.73, 95% CI 0.56–0.95) compared to those who were not. None of the prescriber or practice characteristics was significantly associated with high-risk NSAIDs prescribing.
Discussion
Diclofenac was the most commonly prescribed NSAID, followed by mefenamic acid which together accounted for more than two-third of NSAID prescriptions in primary care in Malaysia. The two most common indications for NSAID prescriptions included musculoskeletal condition and RTI. Nearly a quarter of NSAIDs prescribing was categorised as high-risk. Of these, almost half were patients with risk of gastrointestinal bleed who were not prescribed with adequate gastroprotection while 18–25% were patients who had risk factors for coronary heart disease, received concurrent NSAIDs or high dose NSAIDs. Patients’ citizenship and level of education, indication for NSAID prescriptions, issuance of a medical certificate, number of drugs received and number of diagnoses for the visit significantly influenced the likelihood of high-risk NSAIDs prescribing.
We found diclofenac was the top most prescribed NSAID. This was expected as similar evidences have been reported locally [10, 19] and worldwide [20]. However, our findings showed a high usage of mefenamic acid in our primary care, instead of ibuprofen which was popular elsewhere [6, 9]. This is consistent with previous local studies where diclofenac and mefenamic acid were reported as the most commonly prescribed NSAIDs [10, 21]. The use of mefenamic acid has been known to be more popular among Asian countries compared to western countries [20]. As both drugs were widely used, it is crucial that we understand possible adverse effects with their use for patient safety. A constant review or consideration for safer alternative to NSAIDs is important, in particular among patients who are taking these drugs regularly and are at high risk of adverse effects from NSAIDs.
Apart from the established NSAIDs use for musculoskeletal conditions, other routinely reported indications for NSAIDs in previous studies include soft tissue injuries, headache and menstrual pain [6, 8, 9]. One notable finding from our study was the uncommonly high usage of NSAIDs for RTI, where the frequency of use equates that for musculoskeletal conditions. This was similar to a study from Oman that reported 21% of the NSAID prescriptions were for acute RTI and ear, nose, and throat complaints in primary care [6]. Routine use of NSAIDs for acute RTI remains questionable, especially when they are linked to more adverse effects than paracetamol. To date, NSAIDs have not been shown to improve respiratory symptoms or reduce the duration of infection in RTI [22].
A total of 22.9% of NSAID prescriptions were categorised as high-risk in our study. This was higher than the rate of high-risk NSAIDs prescribing found in England [7] and the Netherlands, at 7.4% and 13% respectively [9]. It was also higher than that a study from Oman in which 16% of NSAID users had a risk factor for NSAID-related adverse effects [6] and that found in a local study from a single primary care centre where 6.6% of NSAID users had potential prescription-related problems [10]. These variations could be due to differences in criteria used to define patients with high-risk NSAIDs prescribing as well as different settings.
The risk of developing an adverse gastrointestinal complication is 3 times more likely in NSAID users compared to non-NSAID users and this risk increases to 5 times among those aged ≥ 60 years [23]. Despite the risk, inadequate gastroprotection with the use of NSAIDs in patients with gastrointestinal bleeding risk is a long-known issue. Previous studies had shown that the proportions of adequate gastroprotection for NSAID users ranged from 37 to 48% in different countries [24,25,26]. A local single-centred study reported 29.7% of patients at risk of gastrointestinal bleed were provided adequate utilisation of gastroprotective strategies [27].We highlighted a lower proportion of adequate gastroprotection at 3.2%. Another noteworthy point is the prescription of antacids as a form of gastroprotection. Antacids are widely used to relieve heartburn and indigestion but these drugs have been found to be ineffective for NSAIDs-related gastroprotection. Antacids delay and reduce the absorption of systemic NSAIDs [28], thereby its prescription would have a risk of nullifying the intended benefits from using NSAIDs.
Between 18 and 22% of high-risk prescription of NSAIDs were attributed to concomitant prescribing of two or more NSAIDs and high dose NSAIDs. This prescribing pattern had been reported to bring little additional benefits in terms of pain relief and quality of life [29]. Besides that, a quarter of the patients had at least one concurrent cardiovascular comorbidity, which is common among primary care attendees. With increasing evidence on the risks of cardiovascular events associated with the use of coxibs, diclofenac and high-dose ibuprofen [30], the net benefit of prescribing NSAIDs has to be weighed against its risks in these patients.
We found that increase in the number of comorbidities and the number of drug prescriptions increased the odds of a patient receiving high-risk NSAID prescriptions. As reported in previous studies [7, 31], the number of drug prescriptions often increased with increasing number of comorbidities. The risk of high-risk prescribing has been shown to increase with the number of drugs administered to elderly patients in hospitals [32]. Our study showed a similar picture with higher odds of high-risk NSAIDs prescribing in primary care with increased number of drugs prescribed.
We also found that patients with higher education levels were less likely to receive high-risk NSAID prescriptions. Patients with higher education levels are usually more aware of adverse effects from drugs, understand the types of drugs they are taking concurrently and would want to be involved in health care decisions [33]. There is increasing evidence that involvement of patients in health decision making would reduce their willingness to accept risky treatments [34].
Pain and discomfort are common reasons for NSAID prescriptions among patients who had musculoskeletal conditions. The higher odds of receiving high risk NSAID prescriptions among these patients could be due to the use of higher doses or multiple concurrent NSAIDs to alleviate symptoms and relieve pain. Nevertheless, it is also likely that the significance of this factor, patient’s citizenship and whether a patient was given a medical certificate were attributed to the confounding influence of age. Previous studies have shown that increase in age rises the odds of being prescribed high-risk NSAIDs [5, 7, 31]. Age however, is part of the composite measure that defines the outcome and thus, is not included as a predictor in the model.
Strengths of this study included that data on NSAID prescriptions were derived from a nationally representative primary care survey in Malaysia. We had anticipated the poorer response rates from the private clinics and had accounted a 70.0% drop-out rate from the private clinics in the sample size calculation for NMCS [11]. With 41.5% response rate from the private clinics in this study, the required sample size was achieved. Besides, we had accounted for over and under-representativeness in each state and sector in the country and had adjusted the results for non-response. Multiple imputation was carried out to reduce potential bias from missing data. We also looked at different levels of predictors in the regression analysis as decisions for prescribing are often multifactorial. There is possible underestimation of the true rates of high-risk NSAIDs prescribing due to a lack of information with regards to patient’s past medical history and concurrent use of over-the-counter NSAIDs. Although reasons for not prescribing adequate gastroprotective agents were not assessed, possible absolute contraindications or side effects with these agents were low.
Implications for practice
There are a few aspects of which findings from this study can be translated into practice.
Firstly, change has to be advocated to prescribers and health regulators. As NSAIDs have long been accepted as effective drugs for pain and inflammation, proposing a change in prescribing behaviour can be difficult. In routine clinical practice, weighing the cardiovascular and gastrointestinal risks against benefits of pain relief is not easy. This is particularly difficult among patients with multiple comorbidities and hence, multiple drugs use as shown in this study. Therefore, the use of practice management software applications such as computerised design support systems to guide prescribers in decisions for NSAID prescriptions should be considered. These systems could contain drug interaction alerts, drug monitoring reminders and patient information sharing among prescribers and pharmacists to reduce initiation of high-risk prescriptions and improve monitoring of treatment [35]. A similar pharmacist-led information technology intervention comprising of feedback, educational outreach and dedicated support had been shown to be effective in reducing inappropriate prescribing [36]. In addition, continuous medical education on new evidence of NSAIDs safety profile should be provided.
Secondly, empowering patient. This is parallel to our findings where patients with higher educational level had lower odds of receiving high-risk NSAID prescriptions. Prescribing decision largely falls in the hands of the prescribers. Nevertheless, patients should be empowered to enquire about their treatment and its potential adverse effects. The approach of shared decision making could bring about positive impacts in prescribing decisions [37]. Besides that, patients could be the ones requesting NSAIDs and thus, they should be informed of the benefits and harms of NSAIDs through public health awareness campaigns and patient education.
Thirdly, there is little evidence on the extent of cardiovascular or gastrointestinal risks with the use of mefenamic acid, despite being similar to diclofenac in terms of its COX-2 selectivity [38]. As mefenamic acid is commonly used, it is important to understand about the possible adverse effects that it may cause. In addition, the reasons for NSAIDs use in acute RTI and outcomes from this treatment should be explored in future studies.
Conclusion
In summary, high-risk NSAIDs prescribing is common in primary care in Malaysia. A concerted effort is warranted from policy makers, prescribers and patients to improve patient safety.
References
Howard RL, Avery AJ, Slavenburg S, Royal S, Pipe G, Lucassen P, et al. Which drugs cause preventable admissions to hospital? A systematic review. Br J Clin Pharmacol. 2007;63:136–47.
Singh G. Recent considerations in nonsteroidal anti-inflammatory drug gastropathy. Am J Med. 1998;105:31s–8s.
Risser A, Donovan D, Heintzman J, Page T. NSAID prescribing precautions. Am Fam Physician. 2009;80:1371–8.
Schjerning Olsen AM, Fosbol EL, Gislason GH. The impact of NSAID treatment on cardiovascular risk—insight from Danish observational data. Basic Clin Pharmacol Toxicol. 2014;115:179–84.
Dreischulte T, Guthrie B. High-risk prescribing and monitoring in primary care: how common is it, and how can it be improved? Ther Adv Drug Saf. 2012;3:175–84.
Al-Shidhani A, Al-Rawahi N, Al-Rawahi A. Non-steroidal anti-inflammatory drugs (NSAIDs) use in primary health care centers in A’Seeb, Muscat: a clinical audit. Oman Med J. 2015;30:366–71.
Guthrie B, Donnan PT, Murphy DJ, Makubate B, Dreischulte T. Bad apples or spoiled barrels? Multilevel modelling analysis of variation in high-risk prescribing in Scotland between general practitioners and between the practices they work in. BMJ Open. 2015;5:e008270.
Hawkey CJ, Cullen DJ, Seager JM, Holmes S, Doherty M, Wilson JV, et al. Pharmacoepidemiology of non-steroidal anti-inflammatory drug use in Nottingham general practices. Aliment Pharmacol Ther. 2000;14:177–85.
Koffeman AR, Valkhoff VE, Celik S, W’t Jong G, Sturkenboom MC, Bindels PJ, et al. High-risk use of over-the-counter non-steroidal anti-inflammatory drugs: a population-based cross-sectional study. Br J Gen Pract. 2014;64:e191–8.
Dhabali AA, Awang R, Hamdan Z, Zyoud SH. Associations between prescribing nonsteroidal anti-inflammatory drugs and the potential prescription-related problems in a primary care setting. Int J Clin Pharmacol Ther. 2012;50:851–61.
Sivasampu S, Wahab Y, Ong S, Ismail S, Goh P, Jeyaindran S. National Medical Care Statistics Primary Care 2014: National Clinical Research Centre Ministry of Health Malaysia 2014.
International Classification of Primary Care, Second Edition (ICPC-2). Geneva: World Health Organization; 2004. http://www.who.int/classifications/icd/adaptations/icpc2/en/. Accessed 20th April 2019.
ATC/DDD Index 2017. WHO Collaborating Centre for Drug Statistics Methodology. 2017. https://www.whocc.no/atc_ddd_index/. Accessed 20th April 2019.
Lanza FL, Chan FK, Quigley EM. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104:728–38.
McGinn D. Polypharmacy medicine optimisation review (PMOR): protocol for prescribing NSAIDs initiation, review & discontinuation. August 2014.
Medicines and Healthcare Products Regulatory Agency. Diclofenac: new contraindications and warnings. United Kingdom. 2013. https://www.gov.uk/drug-safety-update/diclofenac-new-contraindications-and-warnings. Accessed 20th April 2019.
Scottish Government Model of Care Polypharmacy Working Group. Polypharmacy guidance. 2nd ed. Edinburgh: Scottish Government; 2015.
Graham JW. Missing data analysis: making it work in the real world. Annu Rev Psychol. 2009;60:549–76.
Chua SS, Paraidathathu T. Utilisation of non-steroidal anti-inflammatory drugs (NSAIDs) through community pharmacies in Malaysia. Asia Pac J Public Health. 2005;17:117–23.
McGettigan P, Henry D. Use of non-steroidal anti-inflammatory drugs that elevate cardiovascular risk: an examination of sales and essential medicines lists in low-, middle-, and high-income countries. PLoS Med. 2013;10:e1001388.
Khairudin KA, Jatau AI, Manan MM, Chua ST, Chitneni M, Abdullah AH, et al. Utilization pattern of non-steroidal anti-inflammatory drugs at a primary health care in Malaysia. Indian J Pharm Educ Res. 2017;51:156–61.
Kim SY, Chang YJ, Cho HM, Hwang YW, Moon YS. Non-steroidal anti-inflammatory drugs for the common cold. Cochrane Database Syst Rev. 2015;9:CD006362.
Gabriel SE, Jaakkimainen L, Bombardier C. Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. A meta-analysis. Ann Intern Med. 1991;115:787–96.
Thiefin G, Schwalm MS. Underutilization of gastroprotective drugs in patients receiving non-steroidal anti-inflammatory drugs. Dig Liver Dis. 2011;43:209–14.
Valkhoff VE, van Soest EM, Sturkenboom MC, Kuipers EJ. Time-trends in gastroprotection with nonsteroidal anti-inflammatory drugs (NSAIDs). Aliment Pharmacol Ther. 2010;31:1218–28.
Vanderstraeten G, Lejeune TM, Piessevaux H, De Bacquer D, Walker C, De Beleyr B. Gastrointestinal risk assessment in patients requiring non-steroidal anti-inflammatory drugs for osteoarthritis: the GIRANO study. J Rehabil Med. 2016;48:705–10.
Lee HL, Chua SS, Mahadeva S. Utilization of gastroprotective strategies for nonsteroidal anti-inflammatory drug-induced gastrointestinal events in a major teaching hospital. Ther Clin Risk Manag. 2016;12:1649–57.
Verbeeck RK, Blackburn JL, Loewen GR. Clinical pharmacokinetics of non-steroidal anti-inflammatory drugs. Clin Pharmacokinet. 1983;8:297–331.
Kovac SH, Saag KG, Curtis JR, Allison J. Association of health-related quality of life with dual use of prescription and over-the-counter nonsteroidal antiinflammatory drugs. Arthritis Rheum. 2008;59:227–33.
McGettigan P, Henry D. Cardiovascular risk with non-steroidal anti-inflammatory drugs: systematic review of population-based controlled observational studies. PLoS Med. 2011;8:e1001098.
Ble A, Masoli JA, Barry HE, Winder RE, Tavakoly B, Henley WE, et al. Any versus long-term prescribing of high risk medications in older people using 2012 Beers Criteria: results from three cross-sectional samples of primary care records for 2003/4, 2007/8 and 2011/12. BMC Geriatr. 2015;15:146.
Onder G, Landi F, Cesari M, Gambassi G, Carbonin P, Bernabei R. Inappropriate medication use among hospitalized older adults in Italy: results from the Italian Group of Pharmacoepidemiology in the Elderly. Eur J Clin Pharmacol. 2003;59:157–62.
Xu RH, Wong EL. Involvement in shared decision-making for patients in public specialist outpatient clinics in Hong Kong. Patient Prefer Adherence. 2017;11:505–12.
Fraenkel L, Peters E. Patient responsibility for medical decision making and risky treatment options. Arthritis Rheum. 2009;61:1674–6.
Pearson SA, Moxey A, Robertson J, Hains I, Williamson M, Reeve J, et al. Do computerised clinical decision support systems for prescribing change practice? A systematic review of the literature (1990-2007). BMC Health Serv Res. 2009;9:154.
Avery AJ, Rodgers S, Cantrill JA, Armstrong S, Cresswell K, Eden M, et al. A pharmacist-led information technology intervention for medication errors (PINCER): a multicentre, cluster randomised, controlled trial and cost-effectiveness analysis. Lancet. 2012;379:1310–9.
Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27:S110–27.
Cryer B, Feldman M. Cyclooxygenase-1 and cyclooxygenase-2 selectivity of widely used nonsteroidal anti-inflammatory drugs. Am J Med. 1998;104:413–21.
Acknowledgements
We thank the Director-General of Health, Ministry of Health, Malaysia for his permission to publish this manuscript. Our sincere thanks go to the NMCS team, providers and patients from all participating clinics. We would like to acknowledge the contribution of Norazida Ab Rahman in editing the manuscript. We are also grateful to the Malaysian Research Grant, Ministry of Health, Malaysia for funding the NMCS.
Funding
NMCS is funded by the Malaysian Research Grant, Ministry of Health, Malaysia (Grant No. NMRR-09-842-4718). WYH is supported by the Honours Track of the MSc Epidemiology, University Medical Center Utrecht, the Netherlands, which has been made possible by a grant from the Netherlands Organization for Scientific Research grant (Grant No. 022.005.021). The funders had no role in the study design, analysis and preparation of the manuscript.
Conflicts of interest
All authors declare that they have no conflicts of interest.
Data availability
The datasets containing individual level data that were generated and analysed for the current study are not publicly available due to ethical and patient confidentiality restrictions. All requests for access to the data should be addressed to Dr Sheamini Sivasampu at contact@crc.gov.my.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hwong, W.Y., Lim, Y.M.F., Khoo, E.M. et al. High-risk nonsteroidal anti-inflammatory drugs prescribing in primary care: results from National Medical Care Survey Malaysia. Int J Clin Pharm 42, 489–499 (2020). https://doi.org/10.1007/s11096-020-00966-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-00966-w