Abstract
Background Hypoglycemia is an acute and frequent complication of diabetes. Objectives To assess the number of hospital admissions due to iatrogenic hypoglycemia in Alsace (France) over a year, to estimate the associated economic burden and to identify causes. Method A retrospective analysis was performed using data extracted from hospital databases. Costs were calculated from French official tariffs. Setting 31 public and private hospitals. A review of the medical records of patients with iatrogenic hypoglycemia-related hospital admissions was performed at the University Hospital of Strasbourg. Main outcome measures Hypoglycemia–related hospital admissions: number, costs and causes. Results Out of 42,381 hospitalizations, 147 iatrogenic hypoglycemia–related hospital admissions (0.4%) were identified; 41 patients with type 1 diabetes mellitus and 106 with type 2. The total cost associated to the 147 events was € 407,441. The median cost per patient was € 1,224.6 [563.0–2,505.7 (interquartile range)] for type 1 diabetes mellitus and € 3,670.9 [2,505.7–3,670.9] for type 2. Forty-six patients over the 147 were coming from the University Hospital of Strasbourg. In this hospital, the most common origin of the hypoglycemia was missed meals (n = 7), the second was a mismatch between antidiabetic medicines and carbohydrate intake (n = 6), the third was an incorrect use of antidiabetic medicines (n = 5). Conclusions 147 hospitalizations due to iatrogenic hypoglycemia were identified with an estimated global cost of € 407,441. Optimizing therapy with low-risk hypoglycemic medicines, improving access to continuous glucose monitoring systems and offering adequate education, could help address the causes of hypoglycemia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Impacts on practice
-
Promoting therapeutic education sessions would help diabetic patients to better manage their medicines.
-
Physicians should be more aware of the innovative medicines available, as well as new technological monitoring tools.
-
Pharmacists’ interventions should focus primarily on patients at risk of hypoglycemia, i.e. patients with type 1 diabetes mellitus and frail older patients with type 2 diabetes mellitus.
-
The French hospital medical-administrative database is an effective tool to explore iatrogenic events. It gives the opportunity to focus on specific topics such as iatrogenic hypoglycemia-related hospital admissions and to study the associated costs.
Introduction
Hypoglycemia is the most common acute metabolic complication of diabetes. Its diagnosis is based on the Whipple triad: (1) sweating, headache, confusion, fatigue, pallor, palpitations, convulsions…, (2) abnormal low blood glucose and (3) rapid resolution of symptoms after blood sugar normalization [1]. Apart from situations such as insulinoma and bariatric surgery, hypoglycemia is an iatrogenic event induced by antidiabetic medicine [1]. It has been estimated, in a real-life setting (DIALOG study) [2], that 85.3% of patients with type 1 diabetes mellitus (T1DM) and 43.6% with type 2 (T2DM) reported experiencing at least one confirmed hypoglycemic event over a period of 30 days [2]. These hypoglycemic episodes may require treatment up to hospitalization and represent a substantial cost to healthcare systems [3].
Aim of the study
By using data extracted from the hospital medical-administrative PMSI (Programme de Médicalisation des Systèmes d’Information) database, the aims of the study were: to assess the number of hospital admissions due to iatrogenic hypoglycemia (IH) among diabetic patients in Alsace (France) in 2014, to estimate the cost impact associated with their management and to identify causes and contributing factors of these iatrogenic events.
Ethics approval
Information strictly required for the purpose of the study was collected in an anonymized manner. Informed consent was not required, since this was an observational, non-interventional retrospective study.
Methods
Exploitation of data extracted from regional PMSI database: setting
The study was conducted in Alsace, France, a region of 1 873 million inhabitants. A retrospective analysis was performed using data extracted from the regional and anonymous PMSI database over a one-year period (2014). This PMSI database gathers all stays of medicine, surgery and obstetrics performed by public and private hospitals of Alsace (31 hospitals). The data management department of the regional health agency (ARS) performed the data extraction. The department holds the agreements to conduct such studies in accordance with the policy of the French data protection agency (CNIL).
The regional PMSI database gathers anonymous demographic patient information (gender, year of birth…), details of the hospital stays (name of the hospital, types of hospitalization, duration, passage through emergencies) and mode of discharge (return home…).
Concerning the clinical data, each French hospital stay is associated with the release of a standard discharge summary (Résumé de Sortie Standardisé—RSS). This RSS, which is a combination of several medical unit summaries (Résumé d’Unité Médicale—RUM), contains the primary diagnosis that led to the admission and related, or significant associated diagnoses.
Diagnoses, either primary, related, or associated are encoded using the International Classification of Diseases, 10th revision (ICD-10).
Each RSS is then integrated to a Diagnosis Related Group (DRG) used for classification of hospital stays and ultimately for payment (DRG tariffs). All RSS become anonymous e.g. RSA (Résumé Standard Anonymisé) when they are transmitted to the ARS.
Inclusion and exclusion criteria
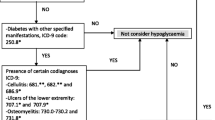
Only hospital stays of diabetic patients aged 18 and over were considered. They were identified using the following ICD-10 codes “E10 patients with T1DM” or “E11 patients with T2DM”. Data collected in the regional PMSI database did not contain the description of the medical acts performed during emergency visits.
IH-related hospital admissions were identified when the main diagnosis of the first RUM of the hospital stays was: “E16.0 IH, no coma” or “E16.1 other hypoglycemia” or “E16.2 unspecified hypoglycemia” or “T38.3 intoxication with insulin and oral hypoglycemic agents”. Hospital admissions with code reflecting a voluntary intoxication were excluded (ICD-10 codes: X64).
Economic evaluation
Costs were considered from the healthcare payer’s perspective. They were estimated using the 2014 tariffs for public and private hospitals. It should be mentioned that public hospitals tariffs cover all medical and technical acts whereas private hospitals tariffs do not include physician fees.
Exploitation of data extracted from medical records
While the regional PMSI database contains information on healthcare expenditures, it does not record medicines and contains few medical data. Because of these limitations, especially the lack of information about the causes of IH, an additional study was set up in parallel at the University Hospital of Strasbourg (UHS). UHS is a public hospital and the largest hospital in Alsace (n = 2,600 beds). A retrospective review of the medical records of patients with IH-related hospital admissions was thus conducted at this hospital. The IH-related hospital admissions were identified with the same criteria (ICD-10 codes) as those used with the regional PMSI database. For each stay, data collected were age of the patient, body mass index, cardiovascular risk factors (hypertension, dyslipidemia, tobacco, alcohol), glycated hemoglobin (HbA1c), antidiabetic medicines, use of an insulin pump, mention of participation in therapeutic education sessions, causes of the hypoglycemia.
Statistical analysis
For quantitative variables, the normality of the distribution was calculated with the Shapiro–Wilk test. The analysis revealed p values greater than 0.05 (quantitative variables not normally distributed). The data were therefore expressed as medians and interquartile range (IQR). Statistical analyses were performed using R Studio R version 3.4.0 (2017-04-21, https://cran.r-project.org/).
Results
Exploitation of data extracted from the regional PMSI database
The regional and anonymous PMSI database provided the distribution of diabetic patients, over the age of 18, hospitalized in Alsace in 2014 (Fig. 1). The sample included 42,381 hospital stays for diabetes; 4,310 (10.2%) of those stays matched with T1DM and 38,071 (89.8%) matched with T2DM.
Among the 42,381 stays, 147 IH-related hospital admissions (0.4%) were identified. Among the 147 hospitalizations for IH, there were 41 T1DM patients (1.0% of all T1DM hospitalizations) and 106 T2DM patients (0.3% of all T2DM hospitalizations). The primary diagnoses of the first RUM associated to the stays were «E16.0, E16.1 or E16.2» for 142 stays (40 T1DM and 102 T2DM) and «T38.3» for 5 stays (1 T1DM et 4 T2DM).
Characteristic of the diabetic patients with IH-related hospital admissions
The median age of the 41 T1DM hospitalized patients with IH was 50 years (IQR [42-76]). The median length of stays was 4.0 days (IQR [1.0–7.0]). Among the 41 T1DM patients, 31 (75.6%) went through emergency departments.
The 106 T2DM patients hospitalized with IH had an average age of 67 years (IQR [76–82]). The median duration of the stays was 7.5 days (IQR [4.0–12.8]). Among the 106 T2DM patients, 74 (69.8%) went through emergency departments. One death was recorded.
Hospital costs related to diabetes and iatrogenic hypoglycemia
The total costs related to the 147 hospitalizations for IH were € 407,441. The median cost of the patient stays was € 1,224.6 (IQR [563.0–2,505.7]) for T1DM and € 3,670.9 (IQR [2,505.7–3,670.9]) for T2DM. Hospitalization costs were highly variable and included the costs of 9 hospitalizations without overnight stay (6 for T1DM and 3 for T2DM). These latter hospitalizations were less expensive.
Exploitation of data extracted from medical records: characteristic of the diabetic patients with IH-related hospital admissions
Forty-six patients extracted from the PMSI regional database were coming from UHS. This diabetic population included 16 T1DM and 30 T2DM patients. Median ages were 49 years (IQR [45–66]) and 77 (IQR [71–81]) for T1DM and T2DM patients respectively. The median body mass index of the T1DM patients was 25 kg/m2 (IQR [24–28]) whereas the one of T2DM patients was 27 kg/m2 (IQR [25–32]). The high blood pressure was the main cardiovascular comorbidity found (9 T1DM and 24 T2DM patients), followed by dyslipidemia (7 T1DM and 15 T2DM patients) and active smoking (3 T1DM and 5 T2DM patients). Finally, the last HbA1c rate measured was 7.6% (IQR [6.9–8.6]) for T1DM and 7.1% (IQR [6.4–8.1]) for the T2DM patients.
Characteristics of hospital stays
Concerning the mode of entry of the 46 patients, 31 patients (67.4%) came through the emergency department. The median duration was 4.5 days (IQR [2.5–7.0]) of T1DM patients’ stays was and the one of T2DM patients was 12.0 days (IQR [8.0–18.0]).
Antidiabetic medication
Outpatient antidiabetic medicines were collected from the medical records. All T1DM patients (n = 16) were treated with at least one insulin. Five had an insulin pump. Nine patients were treated with short and long acting insulins. One patient had mixed, short and long acting insulins combination and 1 patient was on NPH insulin. The most prescribed insulins in T1DM patients were insulin glargine U100/mL (8 patients) and insulin aspart (5 patients). Concerning T2DM patients (n = 30), 16 patients were treated with insulins alone. Eight patients were treated with one insulin (4 patients with a mixed insulin, 4 patients with a long acting insulin) and 8 patients were treated with two insulins (6 patients with short and long acting insulins and 2 patients with short acting and mixed insulins). The most prescribed insulins were insulin glargine U100/mL (7 patients) and insulin aspart (6 patients). Seven patients were treated with oral antidiabetic medicines (OAM) without insulin: 3 patients had a monotherapy (2 patients with a sulfonylurea and 1 with a glinide), 2 patients had a combined therapy associating metformin and a sulfonylurea and 2 patients had a triple-therapy: metformin, a sulfonylurea and a gliptine or acarbose. Seven patients had an association of insulin and OAM: 1 patient had an insulin pump associated to a combined-therapy of metformin and a gliptine, 4 patients with insulin and metformin, 1 patient with insulin and a sulfonylurea, and 1 patient with insulin and a gliptine.
Participation in therapeutic education sessions was noted in medical records for 7 T1DM and 11 T2DM patients.
Hypoglycemic events: causes
The causes of hypoglycemia were specified in medical records for 21 patients. The most common patient behavioral factor which induced episode of hypoglycemia was missed meals (n = 7). The second cause was a mismatch between insulin or OAM doses compared to carbohydrate intake (n = 6). The third was an incorrect use of antidiabetic medicines (n = 5) by the patients; the reported errors were the following: confusion between fast- and slow acting insulins (n = 3) and overuse (n = 2). Episodes of hypoglycemia also occurred in older patients with long-acting sulfonylureas (n = 2) and in one patient with a combined therapy of a sulfonylurea potentiated by voriconazole (n = 1).
Discussion
Main points
Using PMSI database, we identified, within a one-year period, 147 IH-related hospital admissions in Alsace. These hospital admissions represented a total cost of € 407,441. The data obtained through the review of the medical records allowed us to identify causes of IH such as errors in treatment administration and inappropriate medicine prescriptions.
Strengths and limitations
The French PMSI database contains more than 98% of all public and private hospital stays of medicine, surgery and obstetrics [4]. This medical-administrative database has been used for epidemiology and medical-economic purposes [4]. However, it is clear that the PMSI database still remains an untapped source of information on the health-care system and is underexploited. To our knowledge, this study is the first to have used a French regional PMSI database to identify hospital admissions due to hypoglycemia in diabetic patients. However, it can be specified that anticoagulant adverse reactions leading to hospitalizations have already been identified using a similar pattern [4].
The reports contained in the PMSI database are coded by medical staff under the supervision of the PMSI department of each hospital. Coding quality in the PMSI database is expected to be high and is guaranteed by quality checks regularly performed within each hospital. External audits are also conducted by health insurance as hospital financial resources are directly related to the coded information.
Patients going through emergency departments and then immediately leaving the hospital (e.g. emergency visit alone) were not considered in our approach. Thus, the use of the PMSI led to an underestimation of the total number of iatrogenic hypoglycemic events leading to hospital.
Hospital costs
The use of the regional PMSI database allowed us to evaluate the economic burden associated with IH-related hospital admissions. In Alsace, the 147 hospital admissions cost € 407,441 for 1 year. Reported on a national scale, it would reach € 13,581 367 for 1 year in France. This estimated cost represents the total direct cost for the French national health insurance. Considering that, we did not gather all cases (exclusion of emergency visits alone) and that neither physician fees of private hospitals nor private insurance charges were included, this result represents the lower range of the cost associated with the management of IH-related hospital admissions. Furthermore, hospital admissions are only one aspect of IH-related morbidity. A larger proportion of hypoglycemic events may occur in ambulatory care and are also costly.
The median cost of hospitalization for IH in T1DM patients was € 1,224.6 while the one for T2DM patients was for € 3,670.9. The costs associated with hypoglycemia in patients with T1DM and T2DM were assessed by other authors [3, 5,6,7]. For severe hypoglycemic events requiring hospitalization, the estimated costs per event and for any kind of diabetic patients ranged from € 1,300 to € 3,298 (United Kingdom, Spain and Germany) [3]. The mean cost of a severe hypoglycemic event requiring hospitalization in T2DM patients in Portugal was estimated to be € 3,132; a little lower than the one found in a Swedish study which reported total costs of € 3,918 per severe hypoglycemic event treated in hospital [5].
Even if costs observed in European countries do not differ meaningfully from ours, they cannot be readily compared with our data (and between them). They were obtained by using different methodological approaches and sources: direct analysis, micro-costing, claims database, reports…. Despite these limitations, our data as well as the published studies clearly illustrate that hypoglycemia must be recognized as an important factor in the management of diabetic patients and support the development of improvement strategies.
IH-related hospital admissions: causes and improvement strategies
While there are extensive evidences on the risk of hypoglycemia in T1DM, until recently there has been little published data on hypoglycemia in T2DM. This is suggesting that hypoglycemia in T2DM is not a serious or frequent adverse event. In our study, although the occurrence of IH-related hospital admissions was greater in T1DM, the total number of IH-related hospital admissions in Alsace was higher in T2DM (101 vs. 41). This shows that the physicians should not consider hypoglycemia as a minor medical event in T2DM.
The missed meals or meals low in carbohydrate content were the most frequent causes of IH-related hospital admissions in UHS. This is remarkably consistent across different data sets suggesting that this factor should be reviewed with all diabetic patients as well as with their caregivers [8].
The errors of medicine administration observed in our study also highlighted the reality of patients-induced hypoglycemic episode. They invite health professionals to change their approach and find more appropriate interpersonal interactions to discuss face-to-face issues of pharmacotherapy with their patients [9].
We did not design our study to identify the most prevalent medicine classes or individual agents associated with IH-related hospital admissions. Insulins and insulin releasing agents (secratagogue) such as sulfonylureas and glinides were found unsurprisingly. The use of long-acting sulfonylureas in older TDM2 patients and combined therapy (sulfonylurea + voriconazole) found in our study should have been avoided. This constitutes inappropriate medicine prescriptions [10].
The economic and clinical burden of hypoglycemia is now better recognized under our real-life setting conditions. It requires the implementation of quality improvement strategies in daily practices.
Recurrent severe hypoglycemia can lead to a fear of hypoglycemia, which in turn can reduce adherence to therapeutic decisions and increase the risk of morbidity and mortality [11,12,13]. As advocated, French, European and American recommendations no longer, systematically favor intensified regimens [14]. Stopping glinides and sulfonamides in fragile patients should be considered. In these patients, antidiabetic agents of the incretinomimetic class may be an alternative that leads to a lower risk of hypoglycemia [10]. Newer, long-acting insulins (insulin glargine 300 U/mL or insulin degludec) with regard to their more flat and prolonged kinetic profile (up to 36 h) also offer the advantage of lower risk of hypoglycemia compared with older basal insulins (insulin glargine U100/mL, insulin detemir) [15,16,17]. In the recent study of Karamat et al., switching to insulin degludec from basal insulins (insulin glargine U100/mL or insulin detemir) was estimated to achieve substantial cost savings in their cohort of patients due to the reduction of severe hypoglycemic events [17]. As the cost of IH events is considerable, used in appropriate targeted patients, newer long-acting insulins could therefore lead to significant cost savings despite their higher acquisition cost.
The development of continuous glucose monitoring (CGM) systems displaying values in real time has been intensively promoted during recent years, leading to CGM systems with approximately the same precision as currently available blood glucose meters [18, 19]. Implementation of routine use of CGM systems could then have a substantial benefit, especially in patients with impaired hypoglycemia awareness. However, the profile of “responsive” patients who get the best outcome from CGM has yet to be determined [18, 19].
It also appears essential to offer the patient a tailored therapeutic education focused on the prevention of hypoglycemia, its identification and management [8, 20]. In our clinical study, 64% of T1DM and only 36% of T2DM patients had participated in therapeutic education sessions. In addition, clinical pharmacist interventions, carried out at hospital discharge, could enable patients to better understand their treatment and thus reduce IH. These pharmacist interventions should primarily target at-risk diabetic population of hypoglycemia e.g. T1DM patients and frail older patients with T2DM [13, 21]. A recent systematic review and meta-analysis confirmed that pharmacist interventions improve glycemic control in T2DM patients compared with usual care [9].
Conclusion
The study provides a picture of the economic impact of IH-related hospital admissions in Alsace (France) and highlights the main causes of hospitalizations: missed meals, mismatches between insulin or OAM doses compared to carbohydrate intake and incorrect use of antidiabetic medicines. Optimizing therapy with low-risk hypoglycemic medicines, improving access to continuous glucose monitoring systems and offering adequate training, could help addressing the causes of hypoglycemia, reducing the costs of hospitalization and improving the quality of life of diabetic patients.
References
Frier BM. Hypoglycaemia in diabetes mellitus: epidemiology and clinical implications. Nat Rev Endocrinol. 2014;10:711–22.
Cariou B, Fontaine P, Eschwege E, Lièvre M, Gouet D, Huet D, et al. Frequency and predictors of confirmed hypoglycaemia in type 1 and insulin-treated type 2 diabetes mellitus patients in a real-life setting: results from the DIALOG study. Diabetes Metab. 2015;41:116–25.
Hammer M, Lammert M, Mejías SM, Kern W, Frier BM. Costs of managing severe hypoglycaemia in three European countries. J Med Econ. 2009;12:281–90.
Heng C, Rybarczyk-Vigouret MC, Michel B. Anticoagulant-related hospital admissions: serious adverse reactions identified through hospital databases. Pharmacoepidemiol Drug Saf. 2015;24:144–51.
Holbrook T, Tang Y, Das R, Shankar RR, Tunceli K, Williams J, et al. Direct medical costs of severe hypoglycaemic events in patients with type 2 diabetes in England: a retrospective database study. Int J Clin Pract. 2017;71.
Ward A, Alvarez P, Vo L, Martin S. Direct medical costs of complications of diabetes in the United States: estimates for event-year and annual state costs (USD 2012). J Med Econ. 2014;17:176–83.
Aronson R, Galstyan G, Goldfracht M, Al Sifri S, Elliott L, Khunti K. Direct and indirect health economic impact of hypoglycaemia in a global population of patients with insulin-treated diabetes. Diabetes Res Clin Pract. 2018;138:35–43.
Iqbal A, Heller SR. The role of structured education in the management of hypoglycaemia. Diabetologia. 2018;61(4):751–60.
Aguiar PM, de Brito GC, de Lima TM, Santos APAL, Lyra DP, Storpirtis S. Investigating sources of heterogeneity in randomized controlled trials of the effects of pharmacist interventions on glycemic control in type 2 diabetic patients: a systematic review and meta-analysis. PLoS ONE. 2016;11:e0150999.
Wong CW. Avoiding hypoglycaemia: a new target of care for elderly diabetic patients. Hong Kong Med J Xianggang Yi Xue Za Zhi Hong Kong Acad Med. 2015;21:444–54.
Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, Byington RP, Goff DC, Bigger JT, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59.
ADVANCE Collaborative Group, Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–72.
Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–39.
Halimi S. Severe hypoglycaemia the “tip of the iceberg”: an underestimated risk in both type 1 and type 2 diabetic patients. Diabetes Metab. 2015;41:105–6.
Lau IT, Lee KF, So WY, Tan K, Yeung VTF. Insulin glargine 300 U/mL for basal insulin therapy in type 1 and type 2 diabetes mellitus. Diabetes Metab Syndr Obes. 2017;10:273–84.
Ritzel R, Roussel R, Bolli GB, Vinet L, Brulle-Wohlhueter C, Glezer S, et al. Patient-level meta-analysis of the EDITION 1, 2 and 3 studies: glycaemic control and hypoglycaemia with new insulin glargine 300 U/mL versus glargine 100 U/mL in people with type 2 diabetes. Diabetes Obes Metab. 2015;17:859–67.
Karamat MA, Dar S, Bellary S, Tahrani AA. Clinical and cost implications of insulin degludec in patients with type 1 diabetes and problematic hypoglycemia: a quality improvement project. Diabetes Ther Res Treat Educ Diabetes Relat Disord. 2018;9:839–49.
Aberer F, Hajnsek M, Rumpler M, Zenz S, Baumann PM, Elsayed H, et al. Evaluation of subcutaneous glucose monitoring systems under routine environmental conditions in patients with type 1 diabetes. Diabetes Obes Metab. 2017;19:1051–5.
Wild SH, Hanley J, Lewis SC, McKnight JA, McCloughan LB, Padfield PL, et al. Supported telemonitoring and glycemic control in people with type 2 diabetes: the telescot diabetes pragmatic multicenter randomized controlled trial. PLoS Med [Internet]. 2016 [cited 2016 Aug 22];13. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4961438/.
Hermanns N, Kulzer B, Krichbaum M, Kubiak T, Haak T. Long-term effect of an education program (HyPOS) on the incidence of severe hypoglycemia in patients with type 1 diabetes. Diabetes Care. 2010;33:e36.
Mathur S, Zammitt NN, Frier BM. Optimal glycaemic control in elderly people with type 2 diabetes: What does the evidence say? Drug Saf. 2015;38:17–32.
Acknowledgements
The authors wish to acknowledge Dr. Sylvie Fontanel and Daouda Camara from the ARS Grand Est (extraction of the data from regional PMSI database), Dr. Gabriel Nisand from the PMSI Department of the University Hospital of Strasbourg (access of the patients’ medical records) and Dr. Valérie Leray for proofreading and linguistic review of the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflict of interest relevant to the subject of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Richard, T., Issa, R., Andres, E. et al. Iatrogenic hypoglycemia–related hospital admissions identified through databases: economic burden and causes. Int J Clin Pharm 41, 1159–1165 (2019). https://doi.org/10.1007/s11096-019-00877-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-019-00877-5