Abstract
Background Valproate is a widely prescribed antiepileptic drug for generalized epilepsies, due to the extensive knowledge on its efficacy since it is on the market for many decades. However, a large number of new antiepileptic medicines was introduced into clinical practice and may be better options for treatment, considering that these medicines differ in terms of efficacy spectrum. Despite extensive research, questions regarding which medicine would constitute the first option for the monotherapy treatment of generalized epilepsy remain. Aim of the Review To compare the relative efficacy of all available antiepileptic drugs in the monotherapy treatment of generalized epileptic seizures; and also to compare all antiepoileptig drugs with valproate, which is the current first-line treatment for generalized epilepsy. Methods A systematic review for randomized controlled clinical trials was performed. Network meta-analyses used Bayesian random effects model. Sensitivity analyses determined the results´ robustness. The relative probability of two efficacy outcomes (“Seizure free” and “Therapeutic inefficacy”) to happen for each medcicine was calculated using the Surface Under the Cumulative Ranking Curve. Results Seven papers (1809 patients) studied the efficacy of valproate, lamotrigine, phenytoin, carbamazepine, topiramate, levetiracetam, and phenobarbital in the treatment of generalized tonicclonic, tonic, and clonic seizures. Phenytoin demonstrated to be inferior to valproate in leaving the patient free of these seizures types [OR: 0.50 (95% CrI 0.27, 0.87)]. Lamotrigine (61%) showed the highest probability of presenting the outcome “Seizure free”, followed by levetiracetam (47%), topiramate (44%), and valproate (38%) in the treatment of generalized tonic–clonic, tonic, and clonic seizures. Meanwhile, valproate exhibited greater chance of presenting the outcome “Therapeutic inefficacy” (62%). Regarding absence seizures itself, there was no difference in the efficacy of lamotrigine and ethosuximide when compared to valproate. However, the ranking indicates that ethosuximide (52%) and valproate (47%) are both more likely than lamotrigine to keep the patient free of seizures. Conclusions Lamotrigine, levetiracetam, and topiramate are as effective as valproate for treating generalized tonic–clonic, tonic, and clonic seizures. Meanwhile, valproate and ethosuximide are the best options for the treatment of absence seizures promoting better control of seizures, which is the primary goal of pharmacotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on Practice
-
Lamotrigine, levetiracetam and topiramato are as effective as valproate for treating generalized tonic–clonic, tonic, and clonic seizures.
-
Valproate and ethosuximide promote better control of absence seizures.
-
Lamotrigine stands out as the most tolerable option for monotherapy treatment.
Introduction
Epilepsy is the most common serious neurological disorder in adults, affecting about 70 million people worldwide [1]. Although generalized epilepsies represent only 30% of the total, they are often more debilitating [2] and so may lead to cognitive, psychological and social difficulties, mood disorders, and decreased quality of life [3, 4].
The proper choice of an antiepileptic drug (AED) is the key to therapeutic success, given that about 50% of patients with epilepsy become seizure free with the initial monotherapy, but only 11% of the patients whose monotherapy fails due to inefficacy undergo remission with the second treatment option [5, 6]. This indicates that the probability of seizure remission decreases with each treatment failure.
As general rule, the treatment of epilepsy should start as monotherapy, since polytherapy presents modest advantages in terms of seizure control and also increases the risk of adverse reactions (AR), what hinders adherence to treatment [7]. In this sense, valproate (VPA) is a widely prescribed AED in the treatment of generalized epilepsies due to the extensive knowledge on its efficacy, since it has been on the market for many years [8]. However, in recent decades, several new AEDs were introduced into clinical practice and some of them differ in terms of pharmacological properties and efficacy spectrum, which may constitute greater options for treatment [9, 10].
The amount of scientific information on the efficacy of AEDs in the treatment of epilepsy is vast, however updated information available in the literature appears to be fragmented, hindering proper conclusions and alignment of clinical approaches to evidence-based practice, which is fundamental to prevent patient exposure to unnecessary risks [11]. Thus, questions remain such as which AED has the highest efficacy in the monotherapy of generalized epileptic seizures? Is VPA still the best option for the monotherapy treatment of generalized epileptic seizures, despite the emergence of new AEDs?
Aim of the review
To compare the relative efficacy of all available AEDs in monotherapy treatment of generalized epileptic seizures. In addition, to compare each AED with VPA, considered the current first-line treatment for generalized epilepsy.
Methods
A systematic review was conducted in compliance with both Cochrane’s guideline [12] and PRISMA statement [13]. Searches using appropriate terms (Online Resource 1) combined by Boolean operators (AND, OR, NOT) were carried out in the following databases from inception until May 03, 2015: Medline/Pubmed, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials. We supplemented this electronic database search by examining all the included articles´ references.
Selection and data collection´s steps were performed independently by two different authors. Any conflicts were resolved by consensus. After duplicate studies removal, titles and abstracts were screened in order to identify potentially relevant articles. Then, the full text of each selected abstract was read in order to confirm the attendance to the following inclusion criteria: randomized controlled clinical trial; in English, Portuguese, or Spanish language; patients with generalized epileptic seizures (all ages); study intervention being monotherapy treatment with oral use of AED at therapeutic concentrations; comparison of this with another monotherapy consisting of oral use of AED or placebo; patients being followed up for ≥ 15 days (which corresponds to five phenobarbital-PB—elimination half-lives, enough time to ensure the plasma concentration reached the steady state considering that PB’s half-life is the longest among all AED); presence of at least one the following efficacy outcomes: number of patients becoming seizure free in the end of the maintenance treatment period, and number of patients withdrawn from the study due to therapeutic inefficacy (i.e. the lack of effect and/or worsening crises) [14]. Studies comparing different pharmaceutical formulations/doses were excluded so as to avoid data heterogeneity.
For each included study we extracted the following characteristics: year and country of publication, patients’ age range, sample size, duration of the treatment maintenance period, blinding (patients and physicians), number of study groups, AED used in each group, and number of patients that presented previously cited outcomes. We considered results expressed exclusively in numerical form or percentage in order to promote an optimal data extraction, therefore preventing any bias. We assessed the quality of included studies through risk of bias assessment using The Cochrane Collaboration’s tool for assessing risk of bias [12], which categorizes the study as ‘Low risk’ of bias, ‘High risk’ of bias, or ‘Unclear risk’ of bias. The presence of publication bias was explored by the Harbord test [15].
Statistical analysis
Agreement among the authors during the steps of selection and quality assessment was classified into poor, fair, moderate, good and very good reflecting Kappa coefficient < 0.20, 0.21–0.40, 0.41–0.60, 0.61–0.80, 0.81–1.0, respectively [16].
We used Bayesian random effects model [17] with non-informative prior distribution [normal prior with mean of 0 and large variance (10,000)] to perform network meta-analyses combining direct and indirect evidence [18]. Odds ratios were estimated with corresponding 95% credibility intervals (95% CrI) using Markov Chain Monte Carlo simulation with 4 parallel chains of 30,000 tuning and 20,000 simulation iterations. Inconsistencies between direct and indirect comparisons were assessed through node split model [19]. In network meta-analyses, because of the more complex data structure, the evidences´ inconsistency model should assess heterogeneity measure of the performed comparisons.
In addition, the relative probability of two efficacy outcomes to happen for each AED was calculated using the Surface Under the Cumulative Ranking Curve (SUCRA) [20]. Probability would be one when AED shows the highest chance of presenting the outcome. In order to check the results’ robustness, we conducted sensitivity analysis [17, 21], stratifying the results into subgroups according to seizure type, bias risk classification, age range and maintenance treatment period ≤ 24 and ≤ 48 weeks. Analyses were performed in WinBugs software (Medical Research Council, Biostatistics Unit, Cambridge, UK) version 3.2.3.
Results
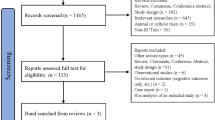
The literature search retrieved 18,874 studies (Fig. 1). However, only 16 [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37] met the inclusion criteria, totaling 4702 patients with generalized epileptic seizures (Table 1). The first study was published in 1983 and the most recent, in 2013. The follow-up median time was 48 weeks (4–288 weeks) with 93.7% of the studies following the patients for at least 24 weeks. In the quality analysis, 43.8% of the studies showed unclear risk of bias, while 37.5% presented high risk of bias and 18.8%, low risk of bias. The overall agreement among authors regarding the studies selection and quality assessment stages were good (k = 0.78) and very good (k = 0.87), respectively. The Harbord test found no evidence of the presence of publication bias in this systematic review (p = 0.304). Most studies reported that AED dose was within the therapeutic dose range. Also, all of them reported the drug was slowly titrated from a low dose up to a well-defined range of serum concentration for each AED.
VPA was tested in 13 studies, lamotrigine (LTG) and phenytoin (PHT) in seven, carbamazepine (CBZ) in five, ethosuximide (ESM) in two, topiramate (TPM), levetiracetam (LEV), placebo and PB in one. Network meta-analyses were performed for the outcomes “Seizure free” and “Withdrawal due to therapeutic inefficacy” (Online Resource 2). Sensitivity analyses group showed no evidence of difference in efficacy by both age range (Online Resource 3) and maintenance treatment period < 24 weeks or < 48 weeks (Online Resource 4). However, sensitivity analyses by seizures type found difference in the efficacy of AED studied in the treatment of absence seizures, for this reason, these type of seizures were analyzed separately. In addition, sensitivity analysis identified a change in the results withdrawing studies with high risk of bias. Therefore, six studies with high risk of bias were excluded from the final results of network meta-analyses [24, 26, 29, 30, 33, 35].
Generalized tonic–clonic, tonic, and clonic seizures
Network meta-analysis regarding AED efficacy in the treatment of generalized tonic–clonic, tonic, and clonic seizures included seven studies [22, 28, 31, 32, 34, 36, 37], comprising 1809 patients (Table 2) and there was no inconsistency among the studies (Online Resource 5). With respect to the “Seizure free” outcome, PHT demonstrated to be inferior to VPA [OR: 0.50 (95% CrI: 0.27, 0.87)] (Fig. 2).
Regarding the relative probability of two efficacy outcomes to occur for each studied AED, LTG (61%) and VPA (62%) had the highest probability of presenting the outcomes “Seizure free” and “Withdrawal due to therapeutic inefficacy”, respectively (Fig. 3).
Absence seizures
Four studies [23, 25,26,27] reported patients with absence seizures. However, one of them presented high risk of bias [26], this way network meta-analyses of absence seizures included only three studies [23, 25, 27] (Table 3). There was no inconsistency among them (Online Resource 6), and evidences suggest there is no difference in the efficacy of LTG or ESM when compared to VPA (Fig. 4). However, the ranking indicated ESM (52%) and VPA (47%) are more likely than LTG to keep the patient free of seizures (Fig. 5).
Discussion
This study provides an overview on the efficacy of the most common AED used in monotherapy treatment regimens in patients with generalized epileptic seizures (Tables 2 and 3) and compares them with VPA, which is actually considered the initial standard treatment for generalized epilepsy. In relation to the seven AEDs tested in the treatment of generalized tonic–clonic, tonic, and clonic seizures, no difference was observed in the risk of the patient to become seizure free or stopping the treatment due to therapeutic inefficacy (lack of effect and/or worsening crises) among VPA, CBZ, LTG, LEV, PB e TPM (Table 2). These drugs are effective and widely used in clinical practice, however, when ranked, VPA, LTG, LEV and TPM stood out as the best options (Fig. 3).
LTG showed the highest probability of keeping the patient free of seizures (61%), followed by LEV (47%), TPM (44%) and VPA (38%). This outcome is very important for improving the patients’ quality of life, given that seizures reduce their sociability and increase stigmatization [38]. Nevertheless, during the efficacy evaluation, it is also important to consider the chance of therapeutic failure, which leads to the change in the therapy. In this regard, our result is reassured, since LTG presented the lowest probability of patient stopping the treatment due to therapeutic inefficacy. Thus, despite VPA, TPM, LEV, and LTG being the top four AEDs on the efficacy rank, LTG may be highlighted as the best one (Fig. 3).
Notably, VPA continues to be a suitable option for the treatment of generalized tonic–clonic, tonic and clonic seizures, especially considering its low cost. Also, due to the large amount of experiences accumulated in decades of usage, health professionals feel safe managing VPA therapy. Though, monotherapy with LTG, LEV or TPM (more expensive) can be fully justified in these cases, since their efficacy profile is similar to VPA, added to that the evidence that patients are more likely to be free of generalized tonic–clonic, tonic and clonic seizures using any of these three AEDs (Fig. 3). Moreover, LTG, LEV and TPM have low enzyme induction potential [8, 10], reducing therefore the number of possible interactions, which can favor their indication for patients in use of several drugs. Consequently, they would be more tolerable considering the reduced probability of adverse reactions [39].
Although CBZ and PB are effective for the treatment of generalized seizures (Table 2), the probability rank showed these AEDs (along with the PHT) have the least probability in keeping the patient seizure free. This is due to the fact that the probability rank is the sum of several consecutive simulations of probability that ranks the treatments from the best to the worst option and may increase the statistical power of the study and capture modest differences between treatments. This fact is observed in practice where CBZ is widely used for the treatment of focal seizures [8]. Thus, the calculation and graphic representation of SUCRA (Fig. 3) constitute a simple and useful way to visualize the comparison of all studied AEDs, since SUCRA has the advantage of simplifying the information on each treatment’s effect through a single value [40].
Regarding the treatment of absence seizures, this study provided evidence that ESM is the drug that has the highest probability of keeping patients free of seizures (52%). Although it occupied a position close to VPA (47%), it was slightly higher than LTG (37%) (Fig. 5), which explains the network meta-analysis’ results evidenced that patients with absence seizures taking ESM are more likely to be seizures free than patients using LTG [OR: 0.31 (95% CrI: 0.11, 0.91)] (Table 3). ESM is a useful AED in the treatment of absence seizures and its efficacy profile is very similar to VPA (Fig. 5). On one hand, however, the use of ESM is considered inappropriate in patients presenting more than one seizure type, such as absence and tonic–clonic seizures, due to limited efficacy in the treatment of absence seizures [41], reinforcing the benefit of VPA use in these cases. On the other hand, ESM has a place in the treatment of patients with a risk of valproate -induced hepatotoxicity [8].
Although databases search returned 11 systematic reviews, these represent exclusively direct comparisons between only two AEDs, or even between one AED and placebo as monotherapy (CBZ, clobazam, LTG, oxcarbazepine, PB, PHT, pregabalin, sulthiame, VPA and vigabatrin) (Online Resource 7), which does not allow a general comparison regarding all AEDs. In this context, network meta-analyses constitutes a relevant tool, once it made possible to compare the efficacy and tolerability of several AEDs used to treat epilepsy and, above all, meta-analytic measures of the relative effect on the efficacy can actually guide health professionals, facilitating the process of selection of a certain AED for monotherapy of generalized epilepsy.
This study has some limitations. First, we did not include unpublished studies, because of the difficulty in accessing their data, though the Harbord test found no evidence of the presence of publication bias in the obtained results. Second, this study did not evaluate the impact of AEDs in the quality of life of patients with epilepsy, because these studies are incipient and employ different methodologies.
Another restriction of this study refers to the absence of the outcome “Time to first seizure” that is considered in some clinical trials. We could not include this due to the deficient standardization of the studies’ periods (number of weeks), since they vary widely (12, 24, 36, and 48 weeks) and are represented by graphs. Thus, these data collection would be inadequate and imprecise. Such inaccuracy and lack of standardization are elucidated in the previous published systematic reviews (Online Resource 7), which did base their results on these corresponding outcomes, but were unable to summarize them.
Half of all included studies in this systematic review (52%) presented unclear risk of bias, indicating they do not provide enough information for a proper analysis of most evaluated domains, which highlights the lack of well-designed epilepsy randomized clinical trials. Nevertheless, the results are robust and reliable once they are based on consistent data and relative methodological quality, as we excluded studies with high risk of methodological bias. In addition, 60% of included studies were composed of maintenance periods equal to or greater than 48 weeks, which is according to specialists, enough time to evaluate the efficacy of AED [42], Furthermore, the sensitivity analysis showed the studies with shorter periods of maintenance did not change the results.
Conclusion
In the last decades, the technological development has advanced at an accelerated pace and health professionals need to be updated. The adequate choice of an antiepileptic drug is fundamental to the success of treatment of generalized epileptic seizures and this systematic review’s data allow the alignment of clinical practice to good scientific evidence. Network meta-analyses enabled the achievement of numerical summary measures synthesizing the available information on the efficacy of AEDs in the treatment of generalized epileptic seizures. Thereby, lamotrigine, levetiracetam, and topiramate are as effective as valproate for treating generalized tonic–clonic, tonic, and clonic seizures, and lamotrigine stands out as the most tolerable option for monotherapy treatment in these cases. Meanwhile, valproate and ethosuximide are more effective options for the treatment of absence seizures promoting better control of seizures, which is the primary goal of pharmacotherapy [8].
References
Ngugi AK, Bottomley C, Kleinschmidt I, Sander JW, Newton CR. Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia. 2010;51(5):883–90.
Shorvon SD. Epidemiology, classification, natural history, and genetics of epilepsy. Lancet. 1990;336:93–6.
Lhatoo SD, Johnson AL, Goodridge DM, MacDonald BK, Sander JW, Shorvon SD. Mortality in epilepsy in the first 11–14 years after diagnosis: multivariate analysis of a long-term, prospective, population-based cohort. Ann Neurol. 2001;49(3):336–44.
Rugg-Gunn FJ, Sander JW. Management of chronic epilepsy. BMJ. 2012;345:1–7.
Perucca E, Beghi E, Dulac O, Shorvon S, Tomson T. Assessing risk to benefit ratio in antiepileptic drug therapy. Epilepsy Res. 2000;41(2):107–39.
Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000;342(5):314–9.
Sirven JI, Noe K, Hoerth M, Drazkowski J. Antiepileptic drugs 2012: recent advances and trends. Mayo Clin Proc. 2012;87(9):879–89.
Shorvon SD, Perucca E, Enge J. Handbook of epilepsy treatment. 3a Edição. United Kingdom: Wiley-Blackwell; 2010. ISBN 978-1-4051-9818-9.
Mattson RH. Medical management of epilepsy in adults. Neurology. 1998;51(5):15–20.
Emilio P, Torbjörn T. The pharmacological treatment of epilepsy in adults. Lancet Neurol. 2011;10:446–56.
Savi MGM, Silva EL. Information flow in the clinical practice of resident physicians: an analysis from an evidence-based medicine perspective. Ciência Inf. 2009;38(3):177–91.
Higgins JPT, Thompson SG. Cochrane handbook for systematic reviews of interventions, Version 5.1.0. The Cochrane Collaboration, 2011. www.cochrane-handbook.org. Accessed 1 May 2015.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(6):e1000097.
Glauser T, Ben-Menachem E, Bourgeois B, Cnaan A, Chadwick D, Guerreiro C, et al. ILAE treatment guidelines: evidence-based analysis of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 2006;47(7):1094–120.
Harbord RM, Egger M, Sterne JC. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med. 2005;25(20):3443–57.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Cipriani A, Higgins JP, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Ann Intern Med. 2013;159(2):130–7.
Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23:3105–24.
Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29(7–8):932–44.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71.
Lau J, Ioannidis JPA, Schmid CH. Quantitative syntesis in systematic reviews. Ann Intern Med. 1997;127(9):820–6.
Brodie MJ, Richens A, Yuen AW. Double-blind comparison of lamotrigine and carbamazepine in newly diagnosed epilepsy. Lancet. 1995;345(8948):476–9.
Callaghan N, O’Hare J, O’Driscoll D, O’Neill B, Daly M. Comparative study of ethosuximide and sodium valproate in the treatment of typical absence seizures (petit mal). Dev Med Child Neurol. 1982;24(6):830–6.
Callaghan N, Kenny RA, O’Neill B, Crowley M, Goggin T. A prospective study between carbamazepine, phenytoin and sodium valproate as monotherapy in previously untreated and recently diagnosed patients with epilepsy. J Neurol Neurosurg Psychiatry. 1985;48(7):639–44.
Coppola G, Auricchio G, Federico R, Carotenuto M, Pascotto A. Lamotrigine versus valproic acid as first-line monotherapy in newly diagnosed typical absence seizures: an open-label, randomized, parallel-group study. Epilepsia. 2004;45(9):1049–53.
Frank LM, Enlow T, Holmes GL, Manasco P, Concannon S, Chen C, et al. Lamictal (lamotrigine) monotherapy for typical absence seizures in children. Epilepsia. 1999;40(7):973–9.
Glauser TA, Cnaan A, Shinnar S, Hirtz DG, Dlugos D, Masur D, et al. Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy: initial monotherapy outcomes at 12 months. Epilepsia. 2013;54(1):141–55.
Marson AG, Al-Kharusi AM, Alwaidh M, Appleton R, Baker GA, Chadwick DW, et al. The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalised and unclassifiable epilepsy: an unblinded randomised controlled trial. Lancet. 2007;369(9566):1016–26.
Ramsay RE, Wilder BJ, Murphy JV, Holmes GL, Uthman B, Slateret J, et al. Efficacy and safety of valproic acid versus phenytoin as sole therapy for newly diagnosed primary generalized tonic-clonic seizures. J Epilepsy. 1992;5(1):55–60.
Rastogi P, Mehrotra TN, Agarwala RK, Singh VS. Comparison of sodium valproate and phenytoin as single drug treatment in generalised and partial epilepsy. J Assoc Physicians India. 1991;39(8):606–8.
Richens A, Davidson DL, Cartlidge NE, Easter DJ. A multicentre comparative trial of sodium valproate and carbamazepine in adult onset epilepsy. Adult EPITEG Collaborative Group. J Neurol Neurosurg Psychiatry. 1994;57(6):682–7.
Steiner TJ, Dellaportas CI, Findley LJ, Gross M, Gibberd FB, Perkin GD, et al. Lamotrigine monotherapy in newly diagnosed untreated epilepsy: a double-blind comparison with phenytoin. Epilepsia. 1999;40(5):601–7.
Steinhoff BJ, Ueberall MA, Siemes H, Kurlemann G, Schmitz B, Bergmann L. The LAM-SAFE Study: lamotrigine versus carbamazepine or valproic acid in newly diagnosed focal and generalised epilepsies in adolescents and adults. Seizure. 2005;14(8):597–605.
Thilothammal N, Banu K, Ratnam RS. Comparison of phenobarbitone, phenytoin with sodium valproate: randomized, double-blind study. Indian Pediatr. 1996;33(7):549–55.
Trinka E, Marson AG, Van Paesschen W, Kälviäinen R, Marovac J, Duncan B, et al. KOMET: an unblinded, randomised, two parallel-group, stratified trial comparing the effectiveness of levetiracetam with controlled-release carbamazepine and extended-release sodium valproate as monotherapy in patients with newly diagnosed epilepsy. J Neurol Neurosurg Psychiatry. 2013;84(10):1138–47.
Turnbull DM, Howel D, Rawlins MD, Chadwick DW. Which drug for the adult epileptic patient: phenytoin or valproate? Br Med J (Clin Res Ed). 1985;290(6471):815–9.
Wilder BJ, Ramsay RE, Murphy JV, Karas BJ, Marquardt K, Hammond EJ. Comparison of valproic acid and phenytoin in newly diagnosed tonic-clonic seizures. Neurology. 1983;33(11):1474–6.
Bandstra NF, Camfield CS, Camfield PR. Stigma of epilepsy. Can J Neurol Sci. 2008;35(4):436–40.
Campos MSA, Ayres LR, Morelo MR, Marques FA, Pereira LR. Efficacy and tolerability of antiepileptic drugs in patients with focal epilepsy: systematic review and network meta-analyses. Pharmacotherapy. 2016;36(12):1255–71.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71.
Sato S, White BG, Penry JK, Dreifuss FE, Sackellares JC, Kupferberg HJ. Valproate versus ethosuximide in the treatment of absence seizures. Neurology. 1982;32:157–63.
Glauser T, Ben-Menachem E, Bourgeois B, Cnaan A, Guerreiro C, Kälviäinen R, et al. Updated ILAE evidence review of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 2013;54(3):551–63.
Funding
No funding was received in support of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Campos, M.S.d.A., Ayres, L.R., Morelo, M.R.S. et al. Comparative efficacy of antiepileptic drugs for patients with generalized epileptic seizures: systematic review and network meta-analyses. Int J Clin Pharm 40, 589–598 (2018). https://doi.org/10.1007/s11096-018-0641-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-018-0641-9