Abstract
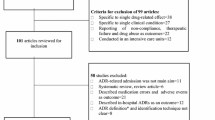
Background Drug hypersensitivity reactions (DHRs) constitute a large portion of adverse drug reactions (ADRs), but studies for DHR incidence based on national data are scarce. Objective This study aimed to estimate the incidence and patterns of DHRs in a Korean population and the associated utilization of medical resources using the national claims data. Setting The retrospective cohort study performed using the national insurance claim database of the Health Insurance Review and Assessment (HIRA) in Korea. Methods The International Classification of Disease 10th revision code was used to identify DHRs with 20 drug induced DHR codes. The claim data with a diagnosis of DHR in the 2009-2014 periods were analyzed. Main outcome and measure The annual incidence and the 6-year incidence rates were calculated. Incidence rate coefficients were analyzed by sex, age, and year. DHRs following with visits of emergency department (ED) or intensive care unit (ICU) were assessed for utilization of medical resources and risk of ER or ICU visits by sex and age Results A total of 535,049 patients with 1,083,507 claims were assessed in the HIRA database for 6 years. DHR incidence was high in the elderly. The risk of ED and ICU visit with DHR was also higher in the elderly than in the young [highest relative risk, RR of ED 2.59 (1.65–4.07), ICU 5.04 (2.50–10.18)]. DHRs related to blood were high in the young age. Conclusion Incidence of DHRs in the real-world clinical practice was higher in the elderly and female. Clinical consequence was more severe in the elderly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
Drug-induced dermatitis, allergic purpura, and toxic liver disease are the DHRs with the most frequent incidence in Korea, and the most severe DHRs are the shock due to anesthesia and toxic epidermal necrolysis (TEN).
-
Medical staff should be suspicious of the possibility of DHRs, especially in elderly.
Introduction
Drug therapy is often accompanied by unexpected, unwanted reactions to patient with adverse drug reactions (ADRs). ADRs accounted for 3–6% of all hospitalizations, and as many as 10–15% inpatients experienced ADRs [1,2,3]. There are two subtypes of ADRs: Type A reactions are dose dependent and predictable, while type B reactions are dose independent and unpredictable [4]. Drug hypersensitivity reactions (DHRs) are an example of type B reactions. The term ‘drug allergy’ is often used in a general sense; however, it should only be used for an ADR with established immunological mechanisms. DHR is, therefore, considered the preferred term and includes both allergic and non-allergic reactions [5, 6].
Many studies have demonstrated the importance and severity of DHRs, which constitute one-third of all ADRs. Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) have been related to a high risk of morbidity and mortality [7]. In a retrospective study of 63 hospitals in the USA, 33.5% of ADRs with emergency department (ED) visits were associated with DHRs [8]. The epidemiologic data related to DHRs have increased steadily. The general clinical symptoms, culprit drugs, and incidence of DHRs have been reported [9, 10]. However, nationwide general population cohort studies with various DHRs are few.
Korea has begun to collect the self-reporting ADRs by patient through the designated institutions in 1988. The regional pharmacovigilance (PV) centers were reorganized in 2006, and Korea Institute of Drug Safety and Risk Management (KIDS) was established for the purpose of centralized systematic ADR data management in 2012. Currently, patients or health care provider reports ADRs voluntarily via 27 regional PV centers and KIDS.
The Korean national health insurance (NHI) system for all citizens has implemented with the electronic claim process through the Health Insurance Review and Assessment (HIRA). The system includes an administrative claims database that can be effectively utilized for epidemiological research [11,12,13]. HIRA database would be useful to carry out the epidemiology study of DHR since the DHR cohort studies are very few for the rare and unexpected events.
Aim of the study
Studies for DHR incidence based on national data are scarce. This study aimed to estimate the incidence and patterns of DHRs in a Korean population and the associated utilization of medical resources related to DHRs using the national claims data.
Ethics approval
This study was approved by Institutional Review board (IRB) at Ajou University (No. 201507-HR-BM-001-01). The study also obtained an official approval from the HIRA research inquiry commission. Each patient’s personal privacy was protected by de-identification of the national insurance claim data for analysis.
Methods
Definition of DHRs
In this retrospective cohort study, we used the International Classification of Disease 10th revision (ICD-10) codes to define DHRs. Stausberg and Hasford [14, 15] classified DHRs into seven diagnostic code categories in accordance with their validity as indicators for ADRs. The most relevant category was level A with subgroups of A1 and A2. A1 was defined as ‘caused by a drug,’ and A2 was defined as ‘caused by a drug or other substance’. Benkhaial et al. [16] specified the codes of allergic drug reaction that were potentially drug-induced. Ten DHR diagnostic codes from the study by Stausberg et al. and those specified by Benkhaial et al. were selected to identify DHRs with level A category. Total 20 DHR codes were included for the final analysis (Table 1).
Data source and statistical analysis
The Korean national insurance claim data from HIRA were reviewed for the period of 2009–2014. The NHI is a universal health care system that covers the entire Korean population of approximately 50 million as a social insurance benefits scheme. The HIRA data consist of demographic information, diagnosis by the Korean Standard Classification of Disease-6 (KCD-6) with extension of ICD-10, prescription records, medical procedures and services, health care providers, and medical resources utilization. To analyze the incidence of DHRs among all Korean, the data for total population enrolled in the NHI were referred to through the open access data available from the Korean Statistical Information Service (KOSIS) (www.kosis.kr).
Incidence trends were analyzed for each DHR code. The annual incidence proportion (IP) for years from 2009 to 2014 was calculated as the number of patients with each DHR code divided by the total number of insured persons. For example, the number of patients with ‘D59.0’ (drug-induced autoimmune hemolytic anemia, DIHA) was 119 and the total number of insured persons in 2009 was 48,613,534; the annual IP of ‘D59.0’ in 2009 is 0.0000024 (24/10 million persons). The incidence rates (IRs) during the 6-year period were calculated based on person-years. The number of patients with each DHR code was divided by disease-free years of total insured persons. While the number of patients with D59.0 in year 2009–2014 was total 441 (119, 177, 55, 29, 27, and 34 for each year), the disease-free year of 119 patients in 2009 was approximately 1 year and that of 177 patients in 2010 was approximately 2 years. The total number of insured persons in 6 years calculated by dynamic population method was 49,464,599 [17]. In such a case, the IR of D59.0 is calculated as: (119 + 177 + 55 + 29 + 27 + 34)/[(119 * 1) + (177 * 2) + (55 * 3) + (29 * 4) + (27 * 5) + (34 * 6) + ((49,464,599 − 441) * 6)] = 0.0000015 (15/10 million person-years).
The IRs were expressed as both crude rates and age-standardized rates (ASRs). The world standard population distribution from the WHO was used to calculate the ASRs. IP and IR for each DHR were presented as 10 million persons (10MP) and 10 million person-years (10MPY), respectively. Poisson regression analysis was performed to analyze the IR coefficient by sex, age, and year. The number and cost of DHR-related ED and intensive care unit (ICU) visits were also assessed. Odds ratio (OR) among DHR codes about ED and ICU visits and the relative risk (RR) of each codes about ED and ICU visits by sex and age were calculated. Chi-square test and Fisher’s exact test were used in comparing categorical data.
Statistical analysis was performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). IR coefficients, OR and RR were presented with 95% confidence intervals (CIs) and p values less than 0.05 were considered significant.
Results
Total number of claim data with DHR codes was 1,083,507 in 535,049 patients during the period of 2009–2014. Female were 57.5% of patients. The highest proportion of DHRs was observed in the 45–64 years group. DHRs decreased in the young ≤ 19 years and increased continuously in the elderly ≥ 65 years on reflection of the age distribution in Korean population (Table 2). Patients with diagnosis of DIHA (D59.0) and drug-induced fever (DIF) (R50.2) were concentrated in the less than 5 years group (43.31 and 58.84%, respectively). The ICD-10 codes for diseases associated with blood occurred in the young age group (0–19 years, 33.64%) at a higher incidence. The codes for diseases of the skin and subcutaneous tissue were higher in the adults (87.32%) compared to the younger (12.68%) (Fig. 1).
The DHRs with a crude incidence rate (IR) of more than 2000 patients per 10MPY were allergic contact dermatitis (ACD) (L23.3, 4701/10MPY), generalized skin eruption (L27.0, 4743/10MPY), allergic purpura (D69.0, 3389/10MPY), and toxic liver disease with hepatitis (K71.6, 2046/10MPY). The age-standardized rates (ASR) for above DHRs were 4320 (L23.3), 4295 (L27.0), 3882 (D69.0), and 1709 (K71.6) per 10MPY, respectively. Drug-induced non-autoimmune hemolytic anemia (D59.2, 2/10MPY and ASR 1/10MPY), acute drug-induced interstitial lung disorders (J70.2, 3/10MPY and ASR 3/10MPY), drug-induced pemphigus (L10.5, 4/10MPY and ASR 3/10MPY), and shock due to anesthesia (T88.2, 2/10MPY and ASR 2/10MPY) were the DHRs associated with the lower IRs (Table 3).
The graph plotted for crude IRs of the DHRs by 5-year age groups showed a slightly cosine curve. Most of DHRs occurred at a lower frequency in the early adolescents and reached a peak incidence for the patients in age 70s. However, allergic purpura (D69.0, 10,248/10MPY) had a peak incidence in the 5–9-year group (Fig. 2, Supplement 1).
A Poisson regression analysis of the IR coefficient revealed that 14 DHRs codes were higher in women, and drug-induced acute pancreatitis (K85.3) was higher incidence in men significantly (Table 4). Drug-induced SLE (M32.0) had a particularly high coefficient (8.30; 95% CI, 6.56–10.49) in women. There was no remarkable change by year; however, DIHA (D59.0) and drug-induced aplastic anemia (D61.1) decreased steadily compared to other DHRs. In analysis by the four age groups, the incidence rates increased with age overall but, those for D59.0, D69.0, and R50.2 decreased with age. The IR coefficients by age were 0.51 (95% CI 0.45–0.57) for DIHA (D59.0), 0.88 (0.87–0.89) for allergic purpura (D69.0), and 0.41 (0.38–0.44) for DIF (R50.2), respectively (Table 4). The IR ratios for the three codes were especially higher in the young age ≤ 19 years (Supplement 2).
The highly diagnosed DHR in ED and ICU was for shock due to anesthesia (T88.2) with 75.71% and 11.43%, respectively. However, the DHR resulting in most frequent ED visits during the study period was generalized skin eruption (L27.0), with a total of 139,330 claims. Most ICU visits, on the other hand, were for anaphylactic shock due to adverse effect of correct drug or medicament properly administered (T88.6) with 184 claims. Severe DHRs of SJS (L51.1) and TEN (L51.2) also had more than 100 claims for ICU visits in 2009–2014 (126 and 110 claims, respectively). The most expensive cost per claim was observed for TEN with 942 ± 39.59 USD (Table 5).
Proportions of DHR with ED or ICU visit out of total claims of each DHR were expressed as odds ratio (OR) with reference to toxic liver disease with hepatitis (K71.6). The DHRs with high ED or ICU visit were drug-induced acute pancreatitis [K85.3, OR ED 3.19 (95% CI 2.79–3.65); ICU 23.35 (15.38–35.46)], shock due to anesthesia [T88.2, ED 8.58 (4.97–14.83); ICU 97.36 (45.94–206.36)], and anaphylactic shock due to adverse effect [T88.6 ED 5.57 (5.27–5.89); ICU 24.06 (19.53–29.65)]. TEN (L51.2) was more diagnosed in ICU than in ED [ED 1.48 (1.35–1.62); ICU 42.13 (33.05–53.71)]. In contrast, claims of generalized or localized skin eruption (L27.0, L27.1) were more dominant in ED visits [L27.0 ED 3.03 (2.99–3.07); ICU 0.07 (0.04–0.10), L27.1 ED 3.38 (3.32–3.44); ICU 0.009 (0.001–0.06), Table 6].
ED or ICU visits by sex for each DHR did not show a specific tendency and was not statistically significant (Table 7). Among the four age groups (≤ 19, 20–44, 45–64, ≥ 65 years), age-related risk of ED or ICU visits in the older age groups (45 years or older) was higher than in the younger age groups (44 years or younger). The 65-year or older group was especially high in ICU visits (Table 8).
Discussion
There are several target organs for DHRs, and multiple symptoms of DHR have been reported in previous ADR studies [18,19,20]. Cutaneous symptoms are the most reported DHRs in terms of frequency and risk. In this study, DHR codes for cutaneous symptoms like contact dermatitis, skin eruption, SJS, and TEN were included for the drug-induced DHR. Severe cutaneous adverse reactions (SCARs) such as SJS, TEN, drug eruption with eosinophilia and systemic symptom (DRESS), and acute generalized exanthematous pustulosis (AGEP) have been studied by several investigators in Asia [21,22,23]. Allergic contact dermatitis (ACD) was also among the frequently reported DHRs in Korea, as identified in this study. Antimicrobial agents and topical medications are the known allergens associated with DHRs; however, the incidence or prevalence of ACD due to drugs in the general population is not yet known [24].
Our data showed the higher incidence rate of DHR with increasing age except DHRs related to blood, such as a drug-induced hemolytic anemia, which were higher incidence in children. The pediatric population might have more sensitization to drug with immature metabolism system than adults [1, 25]. Old age was a risk factor for DHRs [26, 27]. Polypharmacy was also an important risk of DHRs, and DHR-related drug therapy was more reported in the elderly [20, 28,29,30].
DIHA, allergic purpura, and drug-induced fever (DIF) were more frequently diagnosed in the young age groups. There is a few reported data for DIHA as a rare incidence in the general population. A study on children reported that over 65% of autoimmune hemolysis occurred in children < 5 years with ceftriaxone as the most frequent culprit drug [31, 32]. In our study, DIF was also frequent in the < 5-year group (58.84%), with the higher IRs in young age group, while drug fever may have been underestimated in the adult age group as a general manifestation appearing along with other symptoms. Vaccination may also contribute to this observation as children are vaccinated against numerous pathogens until approximately 5 years after birth, and they occasionally experience fever as a typical ADR to vaccines [33,34,35]. Allergic purpura was also high in the 5–9-year age group. Previous surveillance studies on immunoglobulin A vasculitis (Henoch–Schönlein purpura), a representative manifestation of allergic purpura, reported high incidence in the 5–10 years [36].
Women experienced DHRs higher than men for most of DHRs as reported in other previous studies. Drug-induced SLE had the highest IR coefficient, 8.30 (95% CI 6.56–10.49) in the female in this study. A epidemiologic study in a predominantly white population in the USA reported an SLE incidence rate of 5.1 per 100,000 (95% CI 3.5–6.6) in the female and 0.8 per 100,000 (0–1.6) in the male [37].
Shock to anesthesia was the highest cause for both ED and ICU visits. According to the published epidemiologic data, mortality associated with anaphylaxis during surgeries was in the range of 0–9% [38,39,40,41]. The physical condition due to surgery and anesthesia-induced cardiopulmonary dysfunction are known risk factors for anaphylaxis during surgery [42]. This study showed a different trend in visits to ED or ICU by DHRs. A comparative study about characteristics of the elderly visiting a medical ED in Korea showed that 55.5% of patients visited ED directly for urgent and immediate medical care without transfer through other medical institutions and 46.6% visits by walking [43]. Skin eruption was a symptom easily perceived by the patient and was ranked as 4th and 6th of ED visit with rare ICU visit in this study. ICU care is needed for critically ill patients who need hourly and/or invasive monitoring [44]. TEN is one of the severe DHRs, which was more prominent ICU than ED in this study. The mortality rate at 6 weeks of TEN was reported 46% in RegiSCAR (International Registry of Severe Cutaneous Adverse Reaction) group study [45]. The rate of ICU or ED visits was also high in the elderly. A prospective cohort study in Taiwan reported that the proportion of ADRs leading to ED visits in the older age group was 14.3 per 1000 and the younger group was 4.1 per 1000 [46]. Because geriatric populations have multiple diseases and weaken physical condition, immediate treatment is required when symptoms occur.
This study has strength as an epidemiologic research for DHRs of the general population in Korea. DHRs are relatively uncommon, and studies are usually limited in sample size. This study on incidence of DHRs on nearly entire Korean population for 6 years increases the strength of the study. In addition, analysis of incidence according to age, sex, and year of DHR occurrence further increases our understanding of the DHR characteristics in the Korean population. Analyzing ICU or ED visit for each DHR also added information regarding to medical resource utilization from this study.
We also have carried out a separate study not published yet to analyze data of the Korean pharmacovigilance centers to where the spontaneous reports of DHR were reported. Out of total 662,160 ADR reports during 1989–2014, 17.7% (116,209) were the DHRs with WHO-adverse reaction terminology codes. The data of spontaneous reports could not be compared directly to the results of this study with HIRA claim data assessing incidence of DHRs in the Koreans (around 0.18%, 90,000 patients out of 50,000,000 population).
There are some limitations in this study based on the insurance claim data. We were unable to verify information such as clinical laboratory data, family and social history, and other supporting clinical data. Although the ICD-10 codes have been used for a long time since 1990, classification of some allergic diseases is often difficult to use the ICD-10 codes because of uncertain terminologies. For this reason, DHRs without ICD-10 codes were not included in this study, although DHR associated symptoms were present. Furthermore, there is a possibility of under-coding or over-coding for a certain diagnosis. The lack of analysis of the causative drug is also the limit of this study. The claim data with DHRs included the medications, such as steroids or antihistamines, to treat the DHR when the prescriptions were analyzed. The further analysis is in progress performed for the suspected drug using the claim data which included the prescriptions for 6 months prior to the index date of DHR event in each patient during the study period. If research is conducted on the causative drug, it will be more helpful to understand the current state of DHR in Korea. According to a WHO report, ICD-11 will be released in 2018. The allergist communities are reviewing the adequacy of the new codes and have proposed their professional opinion [47,48,49]. The category of drug hypersensitivity was added, the new diagnostic codes were formed, and the existing diagnostic codes were subdivided [50]. These efforts in the newly constructed diagnostic codes may improve the quality of epidemiologic research. This study warrants the health professionals should have more efforts to identify or prevent DHRs with review of any known drug allergy using information technology in the computerized prescription order entry of the electronic medical record system. In the future, a genetic testing prior to use of the high-risk drug like abacavir can prevent the severe life-threatening DHRs.
Conclusion
The major diagnostic codes of drug hypersensitivity reactions were allergic contact dermatitis, generalized skin eruption, allergic purpura, and toxic liver disease with hepatitis in Korea. Female showed a higher DHR than male, and the incidence generally increased with age. However, drug-induced autoimmune hemolytic anemia, allergic purpura, and drug-induced fever occurred at a higher frequency in the younger age group. Severe cutaneous adverse reactions, anaphylaxis, or shock was diagnosed highly in ED and ICU. DHRs leading to ICU and ED visits were also high in the elderly. Future efforts to prevent DHRs including severe events should be implemented in the health care system through application of information technology and the advanced knowledge of pharmacogenomics associated DHRs.
References
Thong BY, Tan T. Epidemiology and risk factors for drug allergy. Br J Clin Pharmacol. 2011;71:684–700.
Kongkaew C, Noyce PR, Ashcroft DM. Hospital admissions associated with adverse drug reactions: a systematic review of prospective observational studies. Ann Pharmacother. 2008;42:1017–25.
Demoly P, Hillaire-Buys D. Classification and epidemiology of hypersensitivity drug reactions. Immunol Allergy Clin North Am. 2004;24:345–56.
Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet. 2000;356:1255–9.
Demoly P, Adkinson NF, Brockow K, Castells M, Chiriac AM, Greenberger PA, et al. International consensus on drug allergy. Allergy. 2014;69:420–37.
Doña I, Barrionuevo E, Blanca-Lopez N, Torres M, Fernandez T, Mayorga C, et al. Trends in hypersensitivity drug reactions: more drugs, more response patterns, more heterogeneity. J Investig Allergol Clin Immunol. 2014;24:143–53.
Gomes ER, Demoly P. Epidemiology of hypersensitivity drug reactions. Curr Opin Allergy Clin Immunol. 2005;5:309–16.
Budnitz DS, Pollock DA, Weidenbach KN, Mendelsohn AB, Schroeder TJ, Annest JL. National surveillance of emergency department visits for outpatient adverse drug events. JAMA. 2006;296:1858–66.
Turner PJ, Gowland MH, Sharma V, Ierodiakonou D, Harper N, Garcez T, et al. Increase in anaphylaxis-related hospitalizations but no increase in fatalities: an analysis of United Kingdom national anaphylaxis data, 1992–2012. J Allergy Clin Immunol. 2015;135(956–63):e1.
Heinzerling L, Tomsitz D, Anliker M. Is drug allergy less prevalent than previously assumed? A 5-year analysis. Br J Dermatol. 2012;166:107–14.
Kim B, Kim J, Kang M, Yang M, Park H, Min K, et al. Allergies are still on the rise? A 6-year nationwide population-based study in Korea. Allergol Int. 2016;65:186–91.
Lee CH, Kim J, Jang EJ, Kim YJ, Choi S, Lee JH, et al. Healthcare utilisation by pregnant patients with asthma in South Korea: a cohort study using nationwide claims data. BMJ Open. 2015;5:e008416.
Kim JY, Lee J, Ko Y, Shin J, Jung S, Choi N, et al. Multi-indication carbamazepine and the risk of severe cutaneous adverse drug reactions in Korean elderly patients: a Korean health insurance data-based study. PLoS ONE. 2013;8:e83849.
Stausberg J, Hasford J. Drug-related admissions and hospital-acquired adverse drug events in Germany: a longitudinal analysis from 2003 to 2007 of ICD-10-coded routine data. BMC Health Serv Res. 2011;11:134.
Stausberg J, Hasford J. Identification of adverse drug events. Dtsch Arztebl Int. 2010;107:23–9.
Benkhaial A, Kaltschmidt J, Weisshaar E, Diepgen TL, Haefeli WE. Prescribing errors in patients with documented drug allergies: comparison of ICD-10 coding and written patient notes. Pharm World Sci. 2009;31:464–72.
Vandenbroucke JP, Pearce N. Incidence rates in dynamic populations. Int J Epidemiol. 2012;41:1472–9.
Roujeau J, Haddad C, Paulmann M, Mockenhaupt M. Management of nonimmediate hypersensitivity reactions to drugs. Immunol Allergy Clin North Am. 2014;34:473–87.
Çelik G, Karakaya G, Öztürk A, Gelincik A, Abadoğlu Ö, Sin A, et al. Drug allergy in tertiary care in Turkey: results of a national survey. The ADAPT study: adult drug allergy perception in Turkey. Allergol Immunopathol. 2014;42:573–9.
Dodiuk-Gad RP, Laws PM, Shear NH. Epidemiology of severe drug hypersensitivity. Semin Cutan Med Surg. 2014;33:2–9.
Chung WH, Wang CW, Dao RL. Severe cutaneous adverse drug reactions. J Dermatol. 2016;43:758–66. https://doi.org/10.1111/1346-8138.13430.
Kano Y, Tohyama M, Aihara M, Matsukura S, Watanabe H, Sueki H, et al. Sequelae in 145 patients with drug-induced hypersensitivity syndrome/drug reaction with eosinophilia and systemic symptoms: Survey conducted by the Asian Research Committee on Severe Cutaneous Adverse Reactions (ASCAR). J Dermatol. 2015;42:276–82.
Yang MS, Kang MG, Jung JW, Song WJ, Kang HR, Cho SH, et al. Clinical features and prognostic factors in severe cutaneous drug reactions. Int Arch Allergy Immunol. 2013;162:346–54.
Victor FC, Cohen DE, Soter NA. A 20-year analysis of previous and emerging allergens that elicit photoallergic contact dermatitis. J Am Acad Dermatol. 2010;62:605–10.
Gomes ER, Kuyucu S. Epidemiology and risk factors in drug hypersensitivity reactions. Curr Treat Options Allergy. 2017;4:239–57.
Hierro Santurino B, Mateos Conde J, Cabero Moran MT, Miron Canelo JA, Armentia Medina A. A predictive model for the diagnosis of allergic drug reactions according to the medical history. J Allergy Clin Immunol Pract. 2016;4(292–300):e3.
Rubio M, Bousquet P, Gomes E, Romano A, Demoly P. Results of drug hypersensitivity evaluations in a large group of children and adults. Clin Exp Allergy. 2012;42:123–30.
Batzing-Feigenbaum J, Schulz M, Schulz M, Hering R, Kern WV. Outpatient antibiotic prescription. Dtsch Arztebl Int. 2016;113:454–9.
Yoon YK, Park GC, An H, Chun BC, Sohn JW, Kim MJ. Trends of antibiotic consumption in Korea according to national reimbursement data (2008–2012): a population-based epidemiologic study. Medicine (Baltimore). 2015;94:e2100.
Schmidt M, Hallas J, Friis S. Potential of prescription registries to capture individual-level use of aspirin and other nonsteroidal anti-inflammatory drugs in Denmark: trends in utilization 1999–2012. Clin Epidemiol. 2014;6:155–68.
Garratty G. Immune hemolytic anemia associated with drug therapy. Blood Rev. 2010;24:143–50.
Sokol RJ, Hewitt S, Stamps BK, Hitchen PA. Autoimmune haemolysis in childhood and adolescence. Acta Haematol. 1984;72:245–57.
Black C, Tagiyeva-Milne N, Helms P, Moir D. Pharmacovigilance in children: detecting adverse drug reactions in routine electronic healthcare records. A systematic review. Br J Clin Pharmacol. 2015;80:844–54.
Sullivan JE, Farrar HC. Section on clinical pharmacology and therapeutics, committee on drugs. Fever and antipyretic use in children. Pediatrics. 2011;127:580–7.
Stockwell MS, Broder K, LaRussa P, Lewis P, Fernandez N, Sharma D, et al. Risk of fever after pediatric trivalent inactivated influenza vaccine and 13-valent pneumococcal conjugate vaccine. JAMA Pediatr. 2014;168:211–9.
Piram M, Mahr A. Epidemiology of immunoglobulin A vasculitis (Henoch–Schonlein): current state of knowledge. Curr Opin Rheumatol. 2013;25:171–8.
Jarukitsopa S, Hoganson DD, Crowson CS, Sokumbi O, Davis MD, Michet CJ, et al. Epidemiology of systemic lupus erythematosus and cutaneous lupus erythematosus in a predominantly white population in the United States. Arthritis Care Res. 2015;67:817–28.
Mitsuhata H, Matsumoto S, Hasegawa J. The epidemiology and clinical features of anaphylactic and anaphylactoid reactions in the perioperative period in Japan. Masui. 1992;41:1664–9.
Gibbs N, Sadleir P, Clarke R, Platt P. Survival from perioperative anaphylaxis in Western Australia 2000–2009. Br J Anaesth. 2013;111:589–93.
Light KP, Lovell AT, Butt H, Fauvel NJ, Holdcroft A. Adverse effects of neuromuscular blocking agents based on yellow card reporting in the U.K.: are there differences between males and females? Pharmacoepidemiol Drug Saf. 2006;15:151–60.
Hepner DL, Castells MC. Anaphylaxis during the perioperative period. Anesth Analg. 2003;97:1381–95.
Volcheck GW, Mertes PM. Local and general anesthetics immediate hypersensitivity reactions. Immunol Allergy Clin North Am. 2014;34:525–46.
Yu S-J, Gang I-S. A comparative study on the process of hospital visits according to the characteristics of the elderly visiting to emergency medical centers. Korean J Health Serv Manag. 2014;8:27–39.
Nates JL, Nunnally M, Kleinpell R, Blosser S, Goldner J, Birriel B, et al. ICU admission, discharge, and triage guidelines: 000 framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016;44:1553–602.
Sekula P, Dunant A, Mockenhaupt M, Naldi L, Bavinck JNB, Halevy S, et al. Comprehensive survival analysis of a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Investig Dermatol. 2013;133:1197–204.
Chen YC, Huang HH, Fan JS, Chen MH, Hsu TF, Yen DH, et al. Comparing characteristics of adverse drug events between older and younger adults presenting to a Taiwan emergency department. Medicine (Baltimore). 2015;94:e547.
Tanno LK, Calderon MA, Goldberg BJ, Akdis CA, Papadopoulos NG, Demoly P. Categorization of allergic disorders in the new World Health Organization International Classification of Diseases. Clin Transl Allergy. 2014;4:42.
Tanno LK, Calderon MA, Goldberg BJ, Gayraud J, Bircher AJ, Casale T, et al. Constructing a classification of hypersensitivity/allergic diseases for ICD-11 by crowdsourcing the allergist community. Allergy. 2015;70:609–15.
Tanno LK, Calderon M, Papadopoulos NG, Demoly P, EAACI/WAO Task force of a Global Classification of Hypersensitivity/Allergic diseases. Mapping hypersensitivity/allergic diseases in the International Classification of Diseases (ICD)-11: cross-linking terms and unmet needs. Clin Transl Allergy. 2015;5:20.
Tanno LK, Calderon MA, Demoly P. Joint Allergy Academies. New allergic and hypersensitivity conditions section in the International Classification of Diseases-11. Allergy Asthma. Immunol Res. 2016;8:383–8.
Funding
This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation funded by the Ministry of Science, ICT & Future Planning, Republic of Korea (No. 2013M3A9B5075838).
Conflicts of interest
The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Han, J., Ye, YM. & Lee, S. Epidemiology of drug hypersensitivity reactions using 6-year national health insurance claim data from Korea. Int J Clin Pharm 40, 1359–1371 (2018). https://doi.org/10.1007/s11096-018-0625-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-018-0625-9