Abstract
Background Venous thromboembolism (VTE) is an important and potentially preventable cause of morbidity and mortality in hospitalised patients. It is a significant, international patient safety issue affecting medical, surgical and mental health in-patients. There is a paucity of published evidence on the incidence of VTE, and the role of VTE risk-assessment and prophylaxis, in mental healthcare settings. Epidemiological evidence indicates that antipsychotic medications are an independent risk factor for VTE. Objective To explore healthcare practitioners’ experiences and perspectives regarding VTE prophylaxis for in-patients in mental health services in Ireland. Setting This study was conducted in two national teaching hospitals in Dublin, Ireland. Method This experiential, qualitative study was conducted using face-to-face, semi-structured interviews. Purposive sampling was used to allow strategic selection of participants from the pharmacy, medical and nursing disciplines. Data was analysed using inductive thematic analysis. Consolidated criteria for reporting qualitative studies guidelines were used as a reporting framework. Main outcome measure Participants’ views on VTE prophylaxis for mental health in-patients. Results Five key themes were derived: risk factors in mental health, attitudes to risk-assessment, challenges with VTE prophylaxis, lack of awareness, and lack of evidence in mental health. Conclusion The results indicate considerable diversities in perceived risk of VTE, and in experiences with VTE risk-assessment and prophylaxis. VTE risk was considered in practice specifically for immobile, older adults and eating disorder patients on bed rest. Specific research is required to address this area of clinical uncertainty in mental health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
There is a lack of awareness of VTE risk for mental health patients.
-
There is a need for a cultural awareness of VTE risk in mental health across the medical, pharmacy and nursing disciplines.
-
In-patients in mental health settings may have inherent or acquired risk factors for VTE, and some patients may be classified in the high risk category.
-
Pharmacists and medical prescribers working in mental health in-patient settings should be familiar with risk factors for VTE, and provide a clinical service capable of identifying high-risk patients.
Introduction
Venous thrombosis is a condition “in which a blood clot (thrombus) forms in a vein, most commonly in the deep veins of the legs, called deep vein thrombosis (DVT)” [1]. The thrombus may dislodge from its site of origin and travel in the blood to the lung as a potentially fatal pulmonary embolism (PE) [1]. Venous Thromboembolism (VTE) includes both DVT and PE [1]. VTE constitutes a major global burden of disease with approximately 10 million cases occurring each year, and accounts for the third leading vascular disease after acute myocardial infarction and stroke [2].
VTE is a multi-causal condition which may result from the co-occurrence of several risk factors [3]. Risk factors include immobilisation, age, active cancer, previous VTE, obesity, smoking, dehydration, hormonal therapy, significant medical co-morbidities, and pregnancy [1, 3,4,5].The association between antipsychotic medications and VTE has been investigated in multiple observational studies [4, 6,7,8,9,10]. A meta-analysis of 11 cohort and case–control studies indicated that antipsychotics are associated with a statistically significant increase in the risk of developing VTE; Odds Ratio 1.54 (95% CI 1.28–1.86) [6].
There is a wealth of published research on VTE risk-assessment and prophylaxis in hospitalised medical and surgical patients. General risk reduction measures in hospitalised patients include encouraging mobilisation, and preventing dehydration [1, 3,4,5]. Prophylaxis may include mechanical methods e.g. use of anti-embolism stockings, and/or pharmacological prophylaxis including low molecular weight heparins (LMWH) [1, 3,4,5]. There is a paucity of evidence on the absolute risk reduction, and the risks associated with VTE prophylaxis in mental healthcare settings. A prospective study examining the incidence of VTE in psychiatric hospitalised patients identified an incidence of VTE of 2.2% at day 10 of admission (95% CI 1.1–4.1%; n = 449) and 3.5% at day 90 (95% CI 2–5.6%; n = 458) [11]. The incidence of VTE in patients aged 75 years with a diagnosis of dementia increased to 8.2% at day 10 and 12.5% at day 90 [11].
Aim of the study
To explore healthcare practitioners’ experiences and perspectives regarding VTE prophylaxis for in-patients in mental health services in Ireland.
Ethics approval
Aston University Research Ethics Committee approval was granted on 16/12/2015 (Reference number: 144-2015-AP #882).
Method
Consolidated criteria for reporting qualitative studies (COREQ) guidelines were used as a reporting framework for this study [12]. This exploratory study involved face-to-face, semi-structured interviews of healthcare practitioners in two mental health in-patient hospitals in Dublin, Ireland. Participants included those working in an independent psychiatric Hospital, Saint John of God Hospital, Dublin; and a public, medical Hospital, St Vincent’s University Hospital, Dublin.
Saint John of God Hospital is an independent not-for-profit 183 bed acute psychiatric, teaching hospital, providing general and specialist in-patient care to adolescents, adults and older adults. St Vincent’s University Hospital is a major, national, academic Hospital providing front line emergency services and national medical care at inpatient and outpatient level. The hospital has 479 in-patient beds, with a designated 36 bed mental health in-patient unit.
Purposive sampling was used, to allow strategic selection of participants [13]. This involved selection of participants on the basis that they would be able to provide ‘information rich’ data to analyse [13]. Maximum heterogeneity sampling [13] was used to include variation in age, discipline, patient population, and experience with adults and older adults. Participants were selected from the medical, pharmacy and nursing disciplines to sample for diversity of perspectives from these disciplines.
A distribution list of eligible participants was generated by the research team, and the co-facilitator sent a generic email to seek expressions of interest. Interested participants were contacted by the principal investigator, and asked to complete a short participant demographics form. Participants were provided with a detailed participant information sheet on the research project, which contained relevant details on the investigator.
A list of open-ended interview questions was prepared by the principal investigator (Appendix 1). Semi-structured interview questions were not provided to participants prior to the interview. Interviews were scheduled and conducted by the principal investigator, at either of the two sites. An electronic recording device was used to record the interviews. Only the principal investigator and the participant were present during the interview. At the start of each interview, each participant was given a brief summary of the terminology to be used in the interview, informed of the audio-recording procedure for the interview, and asked to sign a written consent form. Participants were also informed that the principal investigator would make field notes during the interview process. Interview transcripts were offered to be made available to return to participants, when transcription completed, for comment or correction. No participants elected to review their transcript, and no participant feedback was provided on the findings [12]. Interviews were between 20 and 35 min in duration.
Inclusion criteria:
-
Healthcare practitioners in current roles of Consultant Psychiatrists, Registrars, Pharmacists, Clinical Nurse Managers, Clinical Nurse Specialists and Staff Nurses.
-
Practitioners working in adult or older-adult mental health in-patient units in the two study sites.
-
Participants must provide informed written consent.
Exclusion criteria:
-
Practitioners not providing in-patient clinical care.
-
Practitioners working in adolescent or intellectual disability mental health services.
Each interview recording was transcribed by the principal investigator and thematically analysed. Data was initially coded using complete coding throughout the entire dataset [13]. Coding involved identification of words or brief phrases that captured the essence of the relevance of that piece of data to the research question [13]. Semantic coding was used, as codes were data-derived and reflected the semantic content of the data [13]. Microsoft Word software was used for code filing and mapping. Codes were combined to form themes, which captured a common, recurring pattern in a dataset, clustered around a central organising concept [13]. The themes were identified using an inductive approach and were therefore data-driven, as they were strongly linked to the data [13]. Inductive analysis involved coding the data without attempting to channel it into a pre-existing coding frame or the researcher’s analytical preconceptions [13].
Fifteen potential practitioners were invited to participate. One did not respond to the expression of interest email, and all others invited agreed to participate. 14 participants were interviewed: 6 Consultant Psychiatrists, 3 Senior Pharmacists, 2 Registrars, 2 Staff Nurses and 1 Clinical Nurse Manager. The sample size was governed by the degree of data saturation; the point at which additional data failed to generate new information [13]. Participants selected worked with diverse patient populations including general adults with schizophrenia, affective disorders, personality disorders, older adults with affective disorders and dementing illnesses, and in a specialist adult eating disorder unit.
Results
Five key themes emerged from data analysis:
-
1.
VTE Risk factors in mental health.
-
2.
Attitudes to risk assessment.
-
3.
Challenges with VTE prophylaxis.
-
4.
Lack of awareness in mental health.
-
5.
Lack of evidence in mental health.
VTE risk factors in mental health
All participants reported on experiences with patients with general risk factors for VTE, and specific risk factors relevant to mental health. General risk factors described included age profile, previous history of VTE, dehydration, obesity, concomitant medicines and co-morbidities.
Well obviously one of the risk factors is everybody over 60 or 65 so, but also people who have poor mobility, people who are admitted who are bed–bound, are wheelchair bound, people who become very dehydrated, maybe other comorbid illnesses (Medical [M];2).
Risk factors reported as specific to mental health in-patients included reduced mobility due to acute mental health illnesses including catatonia (a state of increased muscle tone that affects extension and flexion) [14], and severe depression.
It can happen in people that it’s not apparent that they’re at higher risk, so for example I had a gentleman with severe depression, who developed a PE, really because of immobility (M;14).
Several participants acknowledged antipsychotics as an independent risk factor for VTE in mental health in-patients.
I have come across people, one in particular, that did have VTE as a result of antipsychotic treatment, and you know, consequently that medicine was stopped (M; 11).
Attitudes to VTE risk assessment
Considerable diversities in attitudes to VTE risk assessment were identified. Some participants considered VTE risk routinely for all patients on admission. Risk-assessment in older adults, and in those with eating disorders on bed–rest was cited as highly relevant to their clinical assessment on admission.
It’s really important, we’ve got one of the particular fields (eating disorders) that it’s really important in because the patients we have coming into us..they’re on bed rest (M; 6).
These participants emphasised the importance of considering VTE risk, and systematic enquiry of risk factors, as part of a comprehensive admission assessment.
So when a person is admitted, we look at, clearly the referral letter, the background history, medical history, any previous history of VTE, any risk factors for it…I mean we do usually take a very comprehensive history in psychiatry, maybe in our medical history it (VTE risk) should be something that we should routinely be asking, rather than waiting for it to come up in the assessment (M; 6).
Participants working with general adult cohorts cited VTE risk assessment as less relevant or not relevant, as their patient populations were predominantly mobile, and many did not consider VTE risk factors routinely on admission.
Possibly if a patient were to have a history of DVTs or PE, we would, but it’s not something that we would do regularly (Nursing [N]; 7).
Regarding the use of VTE risk-assessment pro-formas, most participants indicated they did not routinely use a formal risk-assessment tool on admission.
We don’t have a formal practice or procedure in place..we don’t have a VTE risk assessment in place, but it would be something that would be at the back of your mind. I can think of 3 or 4 patients at the moment for whom we have discussed it recently (Pharmacy [P]; 3).
Some Consultants indicated that they would have a low threshold of referral for symptomatic patients rather than provide routine risk-assessment and prophylaxis.
I would have a very high index of suspicion, so anyone I see, with any suggestion, of calf tenderness, any swelling, anything at all, I would immediately have D Dimers sent, and they get checked, and it happens fast…. because the consequences of missing it are very serious (M;13).
Several participants when considering this risk, acknowledged the potentially serious consequences of VTE.
Yea, like it’s fairly important, it’s something that could kill you, and swiftly (M; 10).
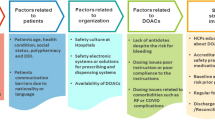
Challenges with VTE prophylaxis
Participants reported adverse patient experiences with the administration of prophylactic LMWH.
The patients don’t like it. It’s painful. They get bruised. They don’t like the injections (M; 13).
There were also reports of adverse patient experiences with the use of anti-embolism stockings.
We’ve even run into problems because their skin is so friable that actually the stockings were causing quite a lot of trauma to the very vulnerable skin (M; 6).
Concerns were expressed regarding administration of daily subcutaneous injections for patients that are acutely unwell, and may be extremely anxious.
If somebody is very agitated they’re not going to want to be injected everyday. That could be quite difficult (P; 4).
Concerns were also expressed regarding consent, capacity issues, and that patients may refuse to have daily sub-cutaneous injections.
And then the patient needs to be informed as well so they would have to have consent, there might be some consent issues…they may themselves refuse to have a daily subcut injection (P;3).
Participants from all disciplines expressed concerns regarding adverse effects of pharmacological prophylaxis and risk of bleeding.
I’d have lots of clinical concerns about bleeding risk, enormous clinical concerns, and it’s a major issue (M; 13).
Participants also expressed concerns regarding pharmacological prophylaxis and interaction with other medicines that may increase the risk of bleeding including antiplatelet agents and antidepressants.
I mean if someone was on 2 antiplatelets you might be a bit more wary of it (pharmacological prophylaxis); and if they’re on an antidepressant (P; 4).
Concerns were expressed by nursing staff regarding administration of LMWH, lack of familiarity with these medicines, and adverse effects.
I do understand it is subcut medication, and we would be able to administer that, but I suppose we don’t know that much about it, or what to kind of look out for in relation to side effects, things like that, or how to explain it to a patient (N;12).
Lack of awareness in mental health
A lack of knowledge and awareness of VTE risk factors, and VTE risk assessment in mental health was identified.
Knowledge of the risk assessment tool and knowledge of the risks in psychiatry, so lack of knowledge among the full multidisciplinary team I would say (P; 3).
Several participants acknowledged that there is more awareness of VTE risk in general hospitals, and a lack of awareness in mental health services.
I suppose it’s not a risk that we generally consider in mental health settings, which is very different to my experience working in general hospital setting (M;5).
From a patient safety perspective, the need for provision of good physical health care in addition to mental health care in mental health units was identified.
One would be to ensure that we’re providing a safe service to our patients so excellence in clinical care would be a target, to address not only the psychiatric needs of the patient, but providing good medical care to our patients (M;2).
Lack of evidence in mental health
All participants acknowledged the evidence base on VTE risk-assessment and prophylaxis for in-patients in general acute hospitals, but highlighted the paucity of research specific to mental health in-patients.
I’d also imagine that, and I might be wrong, but you know that it probably is a lack of research in general, to guide practice in it (M; 5).
Several participants described occurrence of cases of VTE in their experience, and indicated this may be a rare occurrence in practice.
Yea I’ve seen the papers. I can honestly say I don’t think I’ve seen the patients (M; 10).
Am, and I can only speak for my own area, but I would say that what I’ve seen and thankfully, I have never seen a patient in my care, die acutely from pulmonary embolus, in a psychiatric setting. I have, on the other hand, seen several patients develop deep vein thrombosis, whilst an in-patient (M; 14).
Some participants indicated that cases of VTE may be missed in practice. Also, VTE may be under-reported as a cause of death in mental health in-patient units as other co-morbidities and pathologies may have been attributed.
I suspect we probably miss a lot of cases to be honest (M; 11).
I suspect we have no idea, how many deaths here, I mean there aren’t very many but I suspect we’ve no idea how many of them actually started out as DVTs and became PEs. They would probably get recorded as heart attacks or something. I would think so, unless they have a post mortem, but a lot of these people have chronic other illnesses going on (M; 10).
There was uncertainty expressed about the evidence for appropriate prophylaxis; whether it should be pharmacological or mechanical, and what the recommended duration of prophylaxis should be.
I don’t even know if there is much evidence for TED stockings (P; 4).
And people didn’t know what to do, do they stay on the low molecular weight heparins or not, do they stop them or not, because their risk factors haven’t appreciably altered (M; 13).
The need for evidence-based guidelines and a risk-assessment tool specific for mental health in-patients was identified across the disciplines.
Maybe education, or information, and then in addition to that if there was a simple, a fairly straightforward tool that was easy for anyone to complete, and if that would assist in, you know establishing if someone was at risk of VTE, that would be really good (P;1).
Discussion
The results of this study indicate that patients in mental healthcare settings may have general risk factors for VTE, and specific risk factors related to their psychiatric medications or conditions. The findings provide valuable insight into relevance, awareness, and practices of VTE risk-assessment. The clinical practice of early detection of cases of VTE and intervention, rather than routine VTE prophylaxis, was also discussed. Overall, the findings identify the lack of research and evidence-based guidelines for mental health clinicians.
The data generated in this study indicate variances in perceived risk of VTE, and practices of VTE risk-assessment. VTE risk may be considered routinely for all patients on admission or for particular patients. In this study, age profile, and immobility or reduced mobility, emerged as the core inclusion criteria that prompted further clinical assessment for VTE risk.
For clinicians working with general adults, this risk was not highlighted as a priority, and participants indicated this was not considered systematically on admission. Clinicians working with older adults with reduced mobility or immobility, and eating disorder patients on bed rest indicated that VTE risk-assessment was considered routinely in the admissions process.
National and International risk-assessment tools are available for assessing risk factors for VTE in hospitalised patients. Patients may have inherent risks on admission e.g. previous history of VTE, and acquired risks during hospitalisation e.g. immobilisation. The Padua Prediction Score for calculation of VTE risk in hospitalised medical patients ranks active cancer, previous VTE, decreased mobility, and thrombophilia as the highest scoring risk factors [15]. Specific risk factors related to mental health described by participants in this study included immobility due to catatonia and severe depression, and risk associated with antipsychotic medications.
The exact biological mechanisms underlying the association of antipsychotics and VTE are unclear. Potential etiopathogenic factors associated with antipsychotics have been proposed, including drug-induced sedation, obesity, enhanced platelet aggregation, elevation of antiphospholipid antibodies, hyperhomocysteinemia and hyperprolactinaemia [7]. Obesity is associated with a two to three fold increase in VTE risk (BMI > 30 kg/m2), and Metabolic Syndrome is associated with a twofold increased risk [3].
Several participants described individual cases of DVT and PE that they had encountered in practice. Participants acknowledged that although case numbers of VTE were low in their experience, the consequences of any case, and particularly PE, can be fatal. Data from the Swedish Adverse Reactions Advisory Committee identified 12 cases of thromboembolism during Clozapine treatment, during April 1989 and March 2000, and in 5 cases the outcome was fatal [11]. Results from a mortality review in a study completed in a mental health trust in the UK indicated that 2 of 16 deaths (12.5%) referred to the Coroner during a 1 year period were due to PE [16].
Participants indicated that cases of VTE may be missed, or under-reported as a cause of death in mental health in-patients. This is consistent with a theme of the UK Royal College of Psychiatrists report which stated that a number of deaths on mental health in-patient units remain unexplained [17]. In the general population, it is universally recognised that fatal PE is under-diagnosed because signs and symptoms may be non-specific, and attributable to other pathologies [3].
Comprehensive clinical knowledge of prescribing, monitoring and medication interactions is required when prescribing pharmacological prophylaxis for VTE. Specific contra-indications and potential adverse effects of both mechanical and pharmacological prophylaxis need to be considered. The challenges encountered with providing prophylaxis in the mental health settings were described by participants. The results indicate that adverse patient experiences with administration of subcutaneous injections, and capacity issues, need to be considered.
Concerns were expressed by Consultants and Registrars regarding risk of bleeding with LMWH, and lack of knowledge of interactions. This is consistent with key themes identified in a qualitative study in the UK that explored current practice of VTE in acute trusts [18]. The authors identified concerns around VTE prophylaxis treatment, administration and contraindications; and highlight the importance of continuous training for clinical staff [18].
Appropriate knowledge regarding measurement, application and daily inspection requirements is required for safe application of anti-embolism stockings. Nursing staff identified a training requirement due to lack of familiarity with medicines used in prophylaxis, administration of LMWH, and a lack of knowledge on monitoring for adverse events.
A lack of awareness of this risk in mental health was derived as a major theme. A lack of knowledge and awareness was identified across the disciplines, and a need for staff education. Participants acknowledged a need for increased awareness, increased knowledge of risk factors, and a need for systematic enquiry of risk factors on admission.
VTE risk-assessment and prevention has been identified in this study as a patient safety issue. The use of the NHS Safety Thermometer and the integration of VTE risk-assessment as part of physical health assessment have been demonstrated in a UK Mental Health Trust [19]. Routine completion of VTE risk assessment on admission was implemented in an adult and older adult psychiatric unit within Oxford Health NHS Foundation [19]. A recent quality improvement project involved the implementation of a VTE prophylaxis protocol in an older adult ward in a UK NHS hospital [20]. The impetus for this project was two presentations of VTE (one fatal PE, and one symptomatic DVT) on an older adult psychiatric ward over a 6 month period [20]. The authors acknowledge the lack of a validated risk assessment tool in mental health, and used an adaptation of the NICE tool, with additional risk factors for mental health [20].
A specific area of uncertainty that was highlighted in this study was the appropriate duration of prophylaxis in the mental health care setting. The mean length of stay in an in-patient mental healthcare setting is substantially greater than an acute medical setting. UK hospital episode statistics indicate the mean length of stay in mental healthcare settings for an adult and older adult are 52.1 and 93.2 days respectively, versus 5.5 days in an acute medical unit [21]. Data derived from the Swedish Adverse Reactions Advisory Committee indicated that in 8 of 12 patients (67%) that experienced VTE during clozapine treatment, symptoms occurred in the first 3 months of treatment [10].
To the knowledge of this researcher, this is the first qualitative study to explore practitioners’ experiences and perspectives regarding VTE prophylaxis in mental health in-patient services across the medical, pharmacy and nursing disciplines. The involvement of participants from three different disciplines, allowed for data source triangulation, and a broad and diverse spectrum of perspectives to be conceptualised.
It is recognised that qualitative research values subjectivity and reflexivity, and it is acknowledged that the principal investigator brings her subjectivity, views and perspectives into this research study [13]. Reflexivity is also an essential requirement in qualitative research and involves critical reflection on the role of the researcher in the project and their relation to knowledge [13]. The principal investigator in this research project was a female Chief Pharmacist, with over 10 years’ experience working as a specialist, mental health, hospital Pharmacist.
It is acknowledged that the experiences reported in this study reflect those of practitioners currently working in two national hospitals in Dublin, Ireland. The two sites included were selected to include participants working in an independent psychiatric hospital, and a mental health in-patient unit in a large, national, medical hospital. This selection process cannot claim national or international representativity, but aimed to include a clinically recognisable selection of participants, that is transferable. It is acknowledged that not all areas of mental health may be represented.
Conclusion
Thrombovigilance is imperative for hospitalised patients. The patient’s risk profile should be assessed on admission and during hospitalisation if the clinical profile changes. This study has highlighted that in-patients in mental health settings may have inherent or acquired risk factors for VTE, and some may be classified in the high risk category. The most appropriate risk reduction measures, and VTE prophylaxis, remain an area of considerable uncertainty in mental health. There is a need for a cultural awareness of VTE risk in mental health across the medical, pharmacy and nursing disciplines. Further research is required specifically for mental health in-patients, and evidence-based guidelines to inform practice.
References
National Institute for Health and Care Excellence. Venous thromboembolism: reducing the risk for hospitalised patients. Clin Guidel. 2010;92 (updated June 2015). https://www.nice.org.uk/guidance/cg92/resources/venous-thromboembolism-reducing-the-risk-for-patients-in-hospital-pdf-975745995973. Accessed 11 Sept 2017.
Raskob GE, Angchaisuksiri P, Blanco AN, Buller H, Gallus A, Hunt BJ, et al. Thrombosis: a major contributor to global disease burden. Arterioscler Thromb Vasc Biol. 2014;34:2363–71.
Scottish Intercollegiate Guidelines Network. Prevention and management of venous thromboembolism. Natl Clin Guidel. 2010;122 (Updated October 2014). http://www.sign.ac.uk/assets/sign122.pdf. Accessed 11 Sept 2017.
Hippsley-Cox J, Coupland C. Development and validation of risk prediction algorithm (QThrombosis) to estimate future risk of venous thromboembolism: prospective cohort study. BMJ. 2011;343:d4656.
Department of Health UK. Risk assessment for VTE. 2010. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digitalasset/dh_113355.pdf. Accessed 11 Sept 2017.
Barbui C, Conti V, Cipriani A. Antipsychotic drug exposure and risk of venous thromboembolism: a systematic review and meta-analysis of observational studies. Drug Saf. 2014;37:79–90.
Masopust J, Maly R, Valis M. risk of venous thromboembolism during treatment with antipsychotic agents. Psychiatry Clin Neurosci. 2012;66:541–52.
Zhang R, Dong L, Shao F, Tan X, Ying K. Antipsychotics and venous thromboembolism risk: a meta-analysis. Pharmacopsychiatry. 2011;44:183–8.
Parker C, Coupland C, Hippisley-Cox J. Antipsychotic drugs and risk of venous thromboembolism: nested case-control study. BMJ. 2010;341:c4245.
Hagg S, Bate A, Stahl M, Spigset O. Associations between venous thromboembolism and antipsychotics. A study of the WHO database of adverse drug reactions. Drug Saf. 2008;31(8):685–94.
Delluc A, Montavon S, Canceil O, Carpentier M, Nowak E, Mercier B, et al. Incidence of venous thromboembolism in psychiatric units. Thromb Res. 2012;130(6):e283–8. https://doi.org/10.1016/j.thromres.2012.10.002 (Epub 2012 Oct 23).
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32 item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57.
Braun V, Clarke V. Successful qualitative research, a practical guide for beginners. London: SAGE Publications Ltd; 2013.
Cowen P, Harrison P, Burns T. Shorter oxford textbook of psychiatry. 6th ed. Oxford: Oxford University Press; 2012.
Barbar S, Noventa F, Rossetto V, Ferrari A, Brandolin B, Perlati M, et al. A risk assessment model for the identification of hospitalised medical patients at risk for venous thromboembolism: the Padua prediction score. J Thromb Haemost. 2010;8(11):2450–7. https://doi.org/10.1111/j.1538-7836.2010.04044.x.
Jenkinson J. A critical analysis of VTE prophylaxis in psychiatric patients. Poster presentation. Royal College of Psychiatrists’ International Congress; 2012.
Royal College of Psychiatrists. Whole-person care: from rhetoric to reality. Achieving parity between mental health and physical health. Occasional paper OP88. 2013. http://www.rcpsych.ac.uk/files/pdfversion/OP88xx.pdf. Accessed 11 Sept 2017.
McFarland L, Murray E, Harrison S, Heneghan C, Ward A, Fitzmaurice D, et al. Current practice of venous thromboembolism prevention in acute trusts: a qualitative study. BMJ Open. 2014;4(6):e005074.
Al-Taiar H, Nathoo A, Shaheed S. Physical health and VTE risk assessment audit-mental health division (re-audit). 2013. https://www.nice.org.uk/sharedlearning/physical-health-vte-risk-assessment-audit-mental-health-division-re-audit. Accessed 11 Sept 2017.
Croxford A, Clare A, Mc Curdy K. Introduction of venous thromboembolism prophylaxis protocol for older adult psychiatric patients. BMJ Qual Improv Rep. 2015. https://doi.org/10.1136/bmjquality.u205852.w3226.
Patel R. Venous thromboembolism prophylaxis in mental healthcare: do the benefits outweigh the risks? BJ Psych Bull. 2015;39:61–4.
Acknowledgements
We acknowledge the contribution of Dr Consilia Walsh, St Vincent’s University Hospital, Dublin to the participant selection and recruitment process. We acknowledge the contribution of participants from both Saint John of God Hospital, and St Vincent’s University Hospital, Dublin.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest
No conflict of interest declared for each author and contributor.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Purcell, A., Clarke, M. & Maidment, I. Venous thromboembolism prophylaxis in mental health in-patient services: a qualitative study. Int J Clin Pharm 40, 543–549 (2018). https://doi.org/10.1007/s11096-018-0599-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-018-0599-7