Abstract
Background The prescription is one of the factors that influences rational use of medicines. The evaluation of prescribing indicators should contribute to organization of primary health care services. Objective The aim of this study was to evaluate prescribing indicators and associated factors in primary health care in the northeast health district, Belo Horizonte, Brazil. Setting Twenty primary health care units in the Northeast Health District, Belo Horizonte, Brazil. Method The study was cross sectional. Indicators proposed by World Health Organization were used to evaluate rational use of medicines. Main outcome measure Indicators evaluated were average number of medicines per prescription, proportion of medicines with antibiotic, injectable, medicines prescribed by generic name and medicines present in the essential medicines list. Results Three hundred and ninety-nine patients were interviewed. The average number of medicines per prescription was 3.5 (SD 2.2). The proportion of medicines with antibiotic, injectable, medicines prescribed by generic name and medicines present in the essential medicines list was 17.8, 9.8, 94.9, 91.4%, respectively. Patient age ≥60 years was positively associated with number of medicines per prescription (P = 0.00). Conclusion In the northeast health district of Belo Horizonte, the proportion of prescriptions of antibiotics and injections, the adoption of prescribing by generic name and the prescribing of essential medicines were satisfactory in this study considering reference values for these indicators and international scientific literature. However, the mean number of prescribed medicines requires a more in-depth evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
Improving knowledge about prescribing indicators related to rational use of medicines and their associated factors is important in primary health care.
-
In the North-East of Brazil it seems important to subsidize educational activities for prescribers, pharmacists and health professionals and implementation of pharmaceutical clinical services.
-
The average number of medicines per prescription in the region around Belo Horizonte should be reduced.
Introduction
Primary health care provides comprehensive, integrated, and appropriate care over time, with emphasis on prevention and promotion. Communities are its basis for planning and action [1].
Medicines are essential elements of the health care system, and the evaluation of the rational use of medicines is important for the improvement of primary health care.
According to the World Health Organization (WHO), rational use of medicines requires ‘that the patients receive medicines appropriate to their clinical needs, in doses that meet their own individual requirements, for an adequate period of time, and at the lowest cost to them and their community’ [2]. Aspects that influence the rational use of medicines should be related to the health care system, prescriber, dispensing facility, patient, and community [3]. The World Health Organization (WHO) estimated that half of all drugs in the world are prescribed, dispensed or used improperly [4]. Irrational use of medicines may result in consequences such as increased morbidity and mortality, increased costs, the emergence of antimicrobial drug resistance [5], adverse drug reactions and hospitalizations. According to a systematic review, the median percentage of preventable drug-related admissions to hospital was 3.7% (range 1.4–15.4) [6]. A study estimates the impact of adverse drug reactions in the United States of America may cost up to 30.1 billion dollars annually [7].
The WHO proposes indicators to evaluate rational use of medicines in health services and in surveys, including aspects of prescription, dispensing, and health facilities [8, 9]. Prescribing indicators include average number of medicines per prescription, proportion of medicines prescribed by generic name, proportion of medicines on essential medicines list, proportion of patients prescribed injections, and proportion of patients prescribed antibiotics [8, 9]. The WHO did not empirically determined an international standard of the prescribing indicators [10], but recommended reference values for these indicators [11, 12].
A WHO document published in 2007, ‘WHO Operational package for assessing, monitoring and evaluating country pharmaceutical situations: guide for coordinators and data collectors’, presents survey methods to evaluate prescribing indicators in health facilities [9]. A systematic review of studies of medicine use pattern through indicators identified 900 studies in 104 countries [13]. From these studies, 46% were conducted in primary health care (PHC) settings, 21% in a mix of hospitals and PHC settings, 13% in hospitals only, 15% in pharmacies, 2% in non-licensed shops and 3% in households [13]. Assessment of medicine use patterns with the WHO indicators has been used to subsidize actions to promote rational use of medicines, especially in developing countries [14]. In a few studies conducted in PHC facilities in the last 20 years in Brazil, China and Pakistan, the mean number of prescribed medicines changed from 2.3 to 2.7 [15,16,17], the proportion of patients prescribed antibiotics ranged from 40.1 to 53.9% [15,16,17], the proportion of medicines prescribed by generic name ranged from 64.1 to 84.2% [15, 16], and the proportion of medicines on the essential medicines list changed from 67.7 to 78.3% [15, 16]. Research on prescription indicators in primary health care is scarce, particularly research that evaluates associated factors.
Aim of the study
The aim of this study was to evaluate prescribing indicators and associated factors in primary health care in the northeast health district of Belo Horizonte, Minas Gerais, Brazil.
Ethics approval
Prior to conducting research, formal approval was received from the Ethics Committee of Federal University of Minas Gerais and from the Municipal Secretariat of Health of Belo Horizonte (CAAE 31867714.6.0000.5149). Participating patients and prescribers signed an informed consent form.
Methods
Study design and setting
This was a cross-sectional study carried out in northeast health district of Belo Horizonte, Brazil. The municipality of Belo Horizonte is administratively divided into 9 health districts. The northeast health district, the setting of this study, has a warehouse that supplies medicines to 21 primary health care facilities that provide health services for 290,353 residents [18].
Indicators
The forms of the study were designed to calculate prescribing indicators proposed by the WHO [9]: average number of medicines per prescription, proportion of prescriptions of antibiotics, proportion of prescriptions of injections, proportion of medicines prescribed by generic name and proportion of medicines on essential medicines list. The list of indicators and methods for calculation are described in Table 1.
A WHO document recommends evaluating prescribing indicators through survey with patients and prescribers in health facilities. Considering this, two different data collection forms were designed: one to interview patients and observe their prescription and another to interview prescribers.
In the patient form, questions included demographics characteristics such as sex and age. In the patient form there were fields in which researchers filled data on prescriptions presented by the patients, after verifying the prescriptions. The purpose to interview patients and to verify their prescriptions was for measuring prescribing indicators: average number of medicines per prescription, proportion of prescriptions of antibiotics, proportion of prescriptions of injections, proportion of medicines prescribed by generic name and proportion of medicines on essential medicines list.
The prescriber form included two questions: one about the presence of the essential medicine list (EML) in their offices and the other about training in rational use of medicines in the past 12 years. The purpose to interview prescribers was collect data to analyse association of prescribing indicators with presence of the EML and training in rational use of medicines.
Study sample
The sample of this study was selected in three stages: selection of primary health care facilities, selection of patients, and selection of prescribers for the survey. The selection in stages was performed based on a WHO document that proposed survey with patients and prescribers in health facilities. All of the 21 PHC facilities were approached for the study; however, 20 agreed to participate and were included.
The parameters used to calculate the minimum sample size of patients to be interviewed in the survey were a proportion of 50% for indicators due to an unknown frequency of the event of interest, design effect of 1, significance level of 5%, and confidence interval (CI) of 95%. The calculation was performed using OpenEpi open source software, and the result was a minimum sample size of 384 patients.
The prescribers present in the primary health care facility at the time of the survey were interviewed. The calculation of the minimum sample size of prescribers was not performed because those data were not used for the calculation of prescribing indicators, it was used to analyse factors associated.
Data collection
Prior to data collection, a guideline was developed to standardize procedures. A 1-week training was held for data collectors. The training included a lecture about the guideline of the survey and meetings to solve doubts of the researchers about procedures to be performed in the research.
A pilot study was conducted to verify the feasibility of the data collection. Pharmacists and students of Pharmacy with experience in pharmaceutical services composed the team of researchers. Data collection through interview was conducted in November and December 2014. Patients were interviewed by researchers after being attended in the pharmacy of PHC unit with a prescription. During interview, researchers analysed the prescription of the patient and recorded data on generic and brand name of medicines prescribed, whether the medicine was actually dispensed, whether the medicine was antibiotic, injectable and included in the Essential Medicines List. The evaluation of proportion of medicines prescribed by generic name was performed by researchers through analyses of brand name of medicines written in the prescription. Researchers interviewed 399 patients. All prescribers that worked in PHC unit in the day of survey of patients were invited to participate in the survey.
Data entry was performed in PSPP statistical software datasheets. A guideline was developed to standardize data entry procedures. The guideline included instruction for researchers to type data on datasheets. Two-pass verification was performed on data generated for 10% of the sample to check reliability between researchers. Three datasheets were developed: prescribers, patients, and medicines prescribed. All datasheets had variables that identified facilities to enable analysis connecting data from all of three.
Data analysis
The prescribing indicators were described through frequencies, means, and standard deviations. Analysis units were the patient and the medicine.
Multivariate regression models were used to analyse factors associated to prescribing indicators. The indicators related to rational use of medicines selected for the analysis of association were: number of medicines prescribed, proportion of antibiotic prescriptions, and proportion of patients with all medicines prescribed by generic name. They were considered dependent variables. The factors associated with dependent variables were considered independent variables and included patient age ≥60 years, female sex, patient from facilities with prescriber with essential medicines list in the office, patient from facilities with prescriber trained in rational use of medicines.
A logistic regression with odds ratio calculation was used to investigate association between independent variables with proportion of antibiotic prescriptions and proportion of patients with all medicines prescribed by generic name.
A linear regression model with beta coefficient calculation was used to investigate association between number of medicines prescribed with independent variables.
A significance level of 5 and 95% CI were considered in the statistical analyses. Statistical analyses were performed using PSPP statistical software.
Results
In the 20 primary health care facilities included in the study, 399 patients and 127 prescribers were interviewed. All of the prescribers (127) agreed and were included in the study.
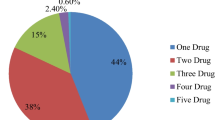
The 399 patient prescriptions included 1383 medicines, with an average of 3.5 medicines (SD 2.2) per patient and a median of 3. Two hundred and seventy-two (68.2%) patients were female. Patients aged ≥60 years comprised 31.6% of the sample. Seventy-nine (19.8%) prescriptions were from primary health care facilities that had medicine out of stock at the time of the survey.
Twelve (9.4%) prescribers possessed one copy of the essential medicine list in their offices, which they presented to the researchers. Nine (7.1%) prescribers reported training in rational use of medicines in the past 12 years.
Table 2 shows the values for average number of medicines per prescription, proportion of prescriptions of antibiotics, proportion of prescriptions of injections, proportion of medicines prescribed by generic name and proportion of medicines on essential medicines list.
Among the independent variables associated to proportion of prescription of antibiotics, only patient age ≥60 years presented a significant association (P < 0.001). None of the independent variables presented significant association with proportion of patient with all medicines prescribed by generic name (Table 3).
According to Table 3, the only independent variable that presented significant association with number of medicines prescribed were patient age ≥60 years (P < 0.001).
Discussion
The prescription is one of the factors that influences the rational use of medicines, and then analysis of prescribing indicators in the northeast health district of Belo Horizonte is relevant.
The average number of medicines per prescription (average 3.5 with standard deviation of 2.2) found in this study was higher than those observed in studies carried out in different countries [13, 15, 16] and higher than reference value (lower than 2) for the indicator [11, 12]. An appropriate prescription must contain the possible minimum of medicines to the reduce probability of adverse reactions and drug–drug interactions [19]. In some situations, a high number of medicines could be appropriate for the patient; however, in this study the evaluation of the clinical needs of patients was not possible because of research methods. Patient age ≥60 years was positively associated with the number of medicines per prescription, which could be explained by the higher frequency of chronic diseases and medicine use in older populations. To avoid high and unnecessary number of drugs, it is recommended frequent review of the need for the use of drugs by the pharmacist in partnership with the health team. Behavioral changes such as the practice of physical exercises, food reeducation and educational activities may contribute to reduce number of medicines for the control of chronic diseases, which are prevalent in the elderly population.
The proportion of prescriptions of antibiotics in the northeast health district of Belo Horizonte was lower than that of Brazilian research conducted in 2004 [15] and studies carried out in China [16] and Ethiopia [14] and lower than reference value for the indicator (lower than 30%) [11, 12], suggesting that overprescribing of antibiotics is not a problem in the district studied. Overprescribing of antibiotics can result in bacterial resistance to antibiotics. A lower frequency of antibiotics was observed in patients aged ≥60 years, which could be explained by the higher prevalence of chronic diseases in older populations [20]. Actions to avoid overprescribing of antibiotics are relevant to prevent bacterial resistance to antibiotics. Educational activities on rational use of antibiotics to health professionals and patients and incentives for prescribers to adopt clinical protocols for treatment of infections in younger populations are recommended.
Our study reported a proportion of prescriptions of injections lower than reference value for this indicator (lower than 20%) [11, 12], suggesting that high use of injections is not a problem in the northeast health district of Belo Horizonte. The present study showed a higher proportion of prescribed injectable medicines than a Brazilian study (6.9%) [15]; however, the methods of the 2 studies were different. In the study published in 2009 [15], contraceptive injections were excluded from the analysis. The use of injections must be restricted to specific clinical situations due to the risk of this route of administration. In primary health care facilities in Brazil, injections are used for the treatment of acute cases and in situations for which there is no other pharmaceutical form available, such as prescribed insulin.
The prescription by generic name may prevent prescription and dispensing errors, since the use of the brand name may lead to risk of switching medications. This study found that the proportion of medicines prescribed by generic name that were also on essential medicines list was greater than values observed in other studies [13, 15, 16] and near the reference value (100%) [11, 12]. The informatized system used to prescribe medicines in primary health care facilities in the northeast health district of Belo Horizonte may have contributed to this result. The system provides the prescriber with information about medicines on the essential medicines list by generic name. Only 9.4% of prescribers reported training in rational use of medicines. A cross-sectional study conducted in an outpatient clinic in Africa found that 11.1% of prescribers were actively receiving update information on the topic rational use of medicines and 100% reported that they needed more information to improve quality of prescribing [21].
Limitations were observed in this study. Information regarding demographic characteristics of prescribers and educational activities on the rational use of medicines in primary health care facilities was not collected. Thus, the influence of these factors on prescribing indicators was not evaluated. The goal of this study was not to evaluate whether prescribed medicines were appropriate for the clinical needs of the patients. However, the research provided an analysis of the influence of facility variables on prescribing indicators, and there is little in the scientific literature on this topic.
Conclusion
In the northeast health district of Belo Horizonte, the proportion of prescriptions of antibiotics and injections, the adoption of prescribing by generic name and the prescribing of essential medicines were satisfactory in this study considering reference values for these indicators and international scientific literature. However, the mean number of prescribed medicines requires a more in-depth evaluation. The evaluation should focus on the need of pharmaceutical products and the implementation of pharmaceutical clinical services. Information on prescribing indicators should inform the development of strategies to improve the rational use of medicines in primary health care level, such as clinical and educational activities and improvement of management of health services.
References
Pan American Health Organization. Renewing primary health care in the Americas: a position paper of the Pan American Health Organization. Washington: PAHO; 2007. http://apps.who.int/medicinedocs/documents/s19055en/s19055en.pdf. Accessed 10 June 2017.
World Health Organization. The rational use of drugs: report of the Conference of Experts Nairobi, 25–29 November 1985. Geneva: WHO; 1987. http://apps.who.int/medicinedocs/documents/s17054e/s17054e.pdf. Accessed 10 June 2017.
Management Sciences for Health. Managing access to medicines and health technologies. Arlington: Management Sciences for Health; 2012. http://apps.who.int/medicinedocs/documents/s19577en/s19577en.pdf. Accessed 10 June 2017.
World Health Organization. The world medicines situation 2011. Geneva: WHO; 2011. http://www.who.int/medicines/areas/policy/world_medicines_situation/WMS_ch6_wPricing_v6.pdf. Accessed 10 June 2017.
Chaturvedi VP, Mathur AG, Anand AC. Rational drug use—As common as common sense? Med J Armed Forces India. 2012;68(3):206–8.
Howard RL, Avery AJ, Slavenburg S, Royal S, Pipe G, Lucassen P, et al. Which drugs cause preventable admissions to hospital? A systematic review. Br J Clin Pharmacol. 2007;63(2):136–47.
Sultana J, Cutroneo P, Trifirò G. Clinical and economic burden of adverse drug reactions. J Pharmacol Pharmacother. 2013;4(Suppl1):S73–7.
World Health Organization. How to investigate drug use in health facilities: selected drug use indicators. Action Programme on Essential Drugs. Geneva: World Health Organization; 1993. http://apps.who.int/medicinedocs/en/d/Js2289e/. Accessed 10 June 2017.
World Health Organization. WHO operational package for assessing, monitoring and evaluating country pharmaceutical situations: guide for coordinators and data collectors. Geneva: WHO; 2007. http://www.who.int/medicines/publications/WHO_TCM_2007.2.pdf. Accessed 10 June 2017.
Ofori-Asenso R, Brhlikova P, Pollock AM. Prescribing indicators at primary health care centers within the WHO African region: a systematic analysis (1995–2015). BMC Public Health. 2016;16:724.
Dumoulin J, Kaddar M, Velásquez G. Guide to drug financing mechanisms. Geneva: World Health Organization; 1998. http://apps.who.int/medicinedocs/en/d/Jh2928e/. Accessed 10 June 2017.
Harvard Medical School and Harvard Pilgrim Health, World Health Organization. Using indicators to measure country pharmaceutical situations Fact Book on WHO Level I and Level II monitoring indicators. Geneva: World Health Organization; 2006. http://www.who.int/medicines/publications/WHOTCM2006.2A.pdf. Accessed 10 June 2017.
Holloway KA, Ivanovska V, Wagner AK, Vialle-Valentin C, Ross-Degman D. Have we improved use of medicines in developing and transitional countries and do we know how to? Two decades of evidence. Trop Med Int Health. 2013;18(6):656–64.
Desalegn AA. Assessment of drug use pattern using WHO prescribing indicators at Hawassa University teaching and referral hospital, south Ethiopia: a cross-sectional study. BMC Health Serv Res. 2013;13:170.
Emmerick IC, Luiza VL, Pepe VL. Pharmaceutical services evaluation in Brazil: broadening the results of a WHO methodology. Cien Saude Colet. 2009;14(4):1297–306.
Dong L, Yan H, Wang D. Drug prescribing indicators in village health clinics across 10 provinces of Western China. Fam Pract. 2011;28(1):63–7.
Siddiqi S, Hamid S, Rafique G, Chaudhry S, Ali N, Shahab S, et al. Prescription practices of public and private health care providers in Attock District of Pakistan. Int J Health Plann Manage. 2002;17(1):23–40.
Secretaria Municipal de Saúde de Belo Horizonte. Plano Municipal de Saúde 2014-2017 [Municipal Health Plan 2014-2017]. Belo Horizonte: Secretaria Municipal de Saúde de Belo Horizonte; 2014.
Farias AD, Cardoso MAA, Medeiros ACD, Belém LF, Simões MOS. Indicadores de prescrição médica nas unidades básicas de Saúde da Família no município de Campina Grande, PB [Prescription indicators in Family Health basic units of the municipal district of Campina Grande, PB]. Rev Bras Epidemiol. 2007;10(2):149–56.
Lima-Costa MF, Matos DL, Camargos VP, Macinko J. Tendências em dez anos das condições de saúde de idosos brasileiros: evidências da Pesquisa Nacional por Amostra de Domicílios (1998, 2003, 2008) [10-year trends in the health of Brazilian elderly: evidence from the National Household Sample Survey (PNAD 1998, 2003, 2008)]. Cien Saude Colet. 2011;16(9):3689–96.
Ojo MA, Igwilo CI, Emedoh T. Prescribing patterns and perceptions of health care professionals about rational drug use in a specialist hospital clinic. J Public Health Afr. 2014;5(2):242.
Funding
None.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lima, M.G., Dutra, K.R. & Martins, U.C.M. Prescribing indicators in primary health care in Belo Horizonte, Brazil: associated factors. Int J Clin Pharm 39, 913–918 (2017). https://doi.org/10.1007/s11096-017-0501-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-017-0501-z