Abstract
Background There is a relative paucity of information to characterise potential changes in medication regimen complexity and prevalence of prescribing of potentially inappropriate medications after hospitalisation, both in Australia and elsewhere. Objective To evaluate medication regimen complexity and the prevalence of potentially inappropriate medications before and after admission to hospital. Setting General medical units of a tertiary care hospital in Australia. Methods Retrospective cohort study of patients aged 65 years and above. Medication complexity was measured by using the Medication Regimen Complexity Index (MRCI). Main outcome measure The primary outcome was the change in the Medication Regimen Complexity Index for all prescribed medications after hospitalization. Results A convenience sample of 100 patients was included in the study. There was a significant change in the mean medication complexity score (as measured using the MRCI), increasing from 29 at the time of admission to 32 at the time of discharge (p < 0.05). Factors such as baseline medication regimen complexity (pre-admission MRCI) and length of stay in the hospitals appear to influence the change in medication complexity. However, the proportion of patients prescribed at least one potentially inappropriate medicine (PIM) decreased significantly, from 52% pre-hospitalization to 42% at discharge (p = 0.04). Conclusions Relative to the time of admission, overall medication complexity increased and the proportion of patients who were prescribed PIMs decreased after hospitalisation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impact on practice
-
Pre-admission screening with the medication regimen complexity index (MRCI), documentation of changes in MRCI, and the presence of potentially inappropriate medicines can help identify patients requiring higher pharmaceutical care input.
-
Pharmacists should take a more proactive roles in monitoring the use of medications with high risk of causing adverse drug reactions in general.
Introduction
Hospital admissions often involve significant changes to a patient’s medication regimen. Previous research suggests that the number of prescribed medications and regimen complexity may increase with hospitalisation [1,2,3,4], possibly leading to greater challenges for older people in self-managing medication usage after discharge [5]. Possible adverse impacts associated with an increased number of medications include less reliable adherence [6,7,8,9], higher risk of adverse health events [6, 7], higher health-care costs [7, 10], increased risk of hospitalisation [11, 12], and premature mortality [7, 13]. Prescribing of potentially inappropriate medications (PIMs) after hospitalisation [14], is also associated with confusion, increased falls, and early mortality [15]. However, it is important to acknowledge that a hospitalisation period also provides an opportunity for re-evaluation of the possible risks and potential benefits of a patient’s medication regimen.
Besides the number of medications, the complexity of a medication regimen is also contributed to by such factors as dosage frequency, administration instructions, and the selection of specific dosage forms. The medication regimen complexity index (MRCI), was developed to more comprehensively describe the complexity of a medication regimen, beyond a measure based simply upon the number of medications prescribed. This validated tool includes 65 items grouped into three subgroups: dose forms, dosing frequencies, and additional instructions relevant to drug administration. The MRCI generates a score that has no upper limit, but a higher score signifies a more complex medication regimen [5]. There is evidence that higher MRCI scores are associated with poorer adherence, increased risk of emergency department presentation, and hospitalisation [16]. The most frequently employed approach to review PIM prescribing involves use of the “Beers Criteria,” an approach based upon interdisciplinary consensus which specifies an explicit list of PIMs that should generally be avoided in older adults. Although sometimes criticised, the Beers criteria have been recently updated and are still a valuable tool to investigate the prescribing of medicines that may be inappropriate for use for elderly people [15]. With the exception of one study from a major Australian public teaching hospital, there remains minimal information regarding medication complexity assessed by the MRCI before and after hospitalisation.
Aim
The primary aim of the present study was to assess the changes in medication regimen complexity by reviewing the MRCI before and after hospitalisation. The secondary aim was to examine the prevalence of prescribing of PIMs at the time of hospital discharge, using the 2015 Beers Criteria.
Ethics approval
Unconditional approval was granted by the Southern Adelaide Clinical Human Research Ethics Committee prior to the commencement of the study.
Method
This was a retrospective cohort study involving a convenience sample of patients aged 65 years and older who were admitted to the general medical units of a tertiary care hospital in South Australia. A list of patients who were admitted to the general medical units of the hospital between 1st Nov 2015 and 24th Nov 2015 was generated using the hospital’s electronic records system. Patients were excluded if they were admitted for palliative care, or into surgical or psychiatric units. Short stay patients hospitalised for diagnostic and/or elective procedures under rheumatology, sleep, urology, and gastroenterology units were also excluded. Patients were further omitted from analysis if they had not been prescribed any medications for chronic illnesses before admission, died during the admission, or were transferred to another acute care hospital for the management of new-onset acute illness or for management of exacerbation of pre-existing conditions. All data collection was performed by the primary investigator.
Information regarding pre-admission and discharge medications for the calculation of the pre- and post-hospitalisation MRCI and for the identification of PIMs prescribed before and after hospitalisation was collected from the hospital’s electronic medical record system. The medication history and admission documentation (recorded by the clinical pharmacist and admitting physician, respectively) were used to gather the relevant pre-hospitalisation information. For post-hospitalisation data, the discharge medication lists and separation summaries were used as information sources. Other information collected included the patients’ age, gender, point of entry, total length of stay, whether a drug administration aid (DAA) was used for medication management, the number of PIMs, and availability of an action plan in the separation summary if PIM was present at the time of discharge.
MRCI assessment
The primary outcome measure was assessed by comparing any change in the MRCI for all prescribed medications before and after hospitalisation.
PIM assessment
The Beers Criteria 2015 were used to identify prescribing of PIMs. The number of PIMs before and after hospitalisation was recorded. In addition, if PIMs were present upon discharge, the separation summary provided to the patients’ general practitioner (primary care physician) or care provider was reviewed to examine if additional recommendations had been made regarding the ongoing use of these PIMs. The separation summary routinely contains information describing past medical history, history of presenting complaint, diagnosis, inpatient treatments, discharge medication list, and follow up plans. It was provided to every patient on discharge as a form of communication tool to facilitate seamless care transition from the tertiary sector to the primary care setting.
Data analysis
Based on a previous study, a power calculation confirmed that with a change of 2 points in the MRCI scale, a sample size of 99 subjects was required. A change of 2 points in MRCI was chosen as the threshold for expected effect size because a change (addition or ceasing) of one medication would normally result in a change of 2 points in MRCI [16].
Statistical analyses were performed using IBM SPSS Statistics V21.0 Proportional comparisons were analysed with the McNemar’s test, changes in mean MRCI scores using a paired t test and potential associations between the change in MRCI after hospitalisation and pre-admission MRCI, were further analysed with a multiple regression model incorporating the following factors: use of DAA on discharge, gender, age and length of hospital stay.
Results
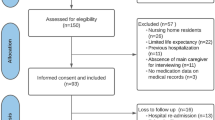
Of 370 patients admitted to the hospital during the data capture window, 270 were excluded from analysis. These included patients admitted to units other than general medicine (n = 225), those who died during the admission (n = 3), those transferred to other hospitals during admission (n = 5), age <65 years (n = 31), and those not taking any chronic medications (n = 5), and one patient admitted for a biopsy. A total of 100 patients were included in the study.
The mean age of all patients was 82 ± 9.15 years and female patients comprised 60% of the sample. The average age for women was 83 ± 8.9 and 81 ± 9.5 years for men. Mean duration of inpatient stay was 18 ± 15.9 days. There was no difference in the proportion of patients who used some form of Drug Administration Aid (DAA) to manage their medications before and after hospitalisation (53 vs. 56%, p = 0.25).
The key findings of the study are summarised in Table 1. The mean overall MRCI score increased after hospitalisation from 28.70 to 32.46 (p = 0.007). There were 64 patients who experienced an average increase in the MRCI of 9.5 ± 8.2 after hospitalisation. Conversely, 31 patients saw an average decrease in MRCI of 7.3 ± 6.5, and 5 patients’ MRCI were unchanged.
There was a significant association between change in MRCI score and higher preadmission MRCI score (R = 0.679, p ≤ 0.0001) see Fig. 1. Regression analysis did not reveal an association between age (p = 0.472), gender (p = 0.659), or use of a DAA on discharge (p = 0.646) and changes in MRCI score. Length of hospital stay however did significantly affect the change in MRCI score (p < 0.0001).
After hospitalisation, 58% of patients (n = 30) who were prescribed PIMs had either an increase in the number of PIMs, or no change, compared to 42% (n = 22) who experienced either a decrease in the number of PIMs (n = 7) or complete ceasing (n = 15) of all PIMs. In addition, five patients who were originally not prescribed any PIM at the time of admission were prescribed a PIM at the end of the hospital stay. Spironolactone was prescribed for three patients with a creatinine clearance <30 ml/min and moxonidine for the two patients whose use of first-line antihypertensives was not optimised. Of the three patients prescribed spironolactone, only one had a separation summary that specifically instructed the local doctor to closely monitor the patient’s serum potassium and kidney function. The breakdown of the PIM by the categories used in the Beers criteria is provided in Table 2. Of 42 patients for whom at least one PIM was present at discharge, only three were found to have a full plan of action that addressed the PIMs included in their separation summary. A further two patients did have a documented plan addressing prescribed PIMs. For the remainder of patients prescribed PIMs at discharge, the separation summary did not address issues related to the PIMs.
Discussion
In this study, hospitalisation was associated with significantly increases in medication regimen complexity and the overall number of medications prescribed. Compared to the findings of Elliott et al., where there was an increase of up to 55% in the MRCI score at the time of hospital discharge, the magnitude of increase in MRCI observed in this study (13%) was much lower, possibly reflecting the higher initial clinical complexity of patients (MRCI 28 vs. 18) [17]. This may also mean that doctors were more reluctant to add more medications to patients who already had been taking high number of medications.
Not unexpectedly, and reassuringly, patients who were admitted with more complex medication regimens were more likely to have their medication regimen simplified. However, even if a highly complex medication regimen gets simplified, careful attention to follow-up is required. As is the case when initiating a new medication, the medication simplification process must be approached with due vigilance. This points to an opportunity for the integral involvement of pharmacists as medication therapy specialists who play important roles in assessing the possible effects of various changes in the medications. To ensure continuity of care the medical staff assuming responsibility for community-based care of these patients must receive concise and comprehensive information detailing the medication changes. There is evidence to show that the medical staff are more likely to accept the medication changes and maintain these going forward if clear information is communicated to them [18]. The pharmacists involved could play an integral part in making this happen.
This study shows that hospitalisation resulted in a statistically significant reduction in the prevalence of the use of PIMs identified using the updated Beers Criteria produced in 2015 by the American Geriatrics Society. The overall mean number of PIMs prescribed also significantly decreased during hospitalisation, and this result might be expected, given that the medical teams consist of physicians, pharmacists, nurses, and other allied health professionals who were experienced in caring for the older patients. The medications that were included in the Beers list were identified after an interdisciplinary consensus process highlighted them as having a high potential for causing harm if prescribed for older adults, suggesting that experienced multidisciplinary care teams who are accustomed to dealing with older people are likely to have little difficulty in identifying them as potentially problematic. However, it is of some concern that more than half of the patients who were admitted with PIMs either experienced an increase in PIM prescribing, or no change by the end of the hospital stay, and moreover that there was a small number of patients who were not treated with a PIM at admission but who were at discharge, signifying that there is still room for improvement in addressing the issue of PIMs.
As regards the specific individual agents identified as PIMs, it is not surprising that Proton Pump Inhibitors (PPIs) featured prominently among the PIMs prescribed (Table 2), and could well have been the most commonly encountered PIMs in prevalence for both the pre- and post-admission phase if not for the conservative approach to identifying these drugs as PIMs. A PPI was deemed appropriate if the patient was shown to have a diagnosis such as gastroesophageal reflux disease (with or without current active symptoms), or if the drug was used to protect against the effects of ulcer-inducing medications, where use of a PPI is indicated to prevent possible drug-related harm. It was noted that potentially inappropriate use of the PPI agents was increased with hospitalisation. However, the increase was at least partly due to the failure to remove the drugs whenever the indication was no longer present (e.g. ceasing of antiplatelet agents where a PPI used was for gastroprotection). Even though there is mounting evidence that the PPIs are not a benign class of drugs, it seems that years of conditioning have still managed to sustain high level of tolerance for the extended use of these agents [19]. There is an urgent need to educate health professionals about potential dangers of the ongoing inappropriate use of PPIs.
Benzodiazepines were the most common PIMs used by the patients before admission. Almost all of the benzodiazepines prescribed were short or intermediate acting agents. This possibly reflects the view among the health professionals that long-acting agents are more harmful than their shorter acting counterparts, an assertion that has been disputed [16]. The benzodiazepines were the PIM class that was most likely to be ceased, especially if prescribed for insomnia. In fact, the withdrawal of the agents contributed most to the reduction in the prevalence of PIMs in the post-admission phase. However, benzodiazepines were often left unaltered if these drugs were used for treating agitation in patients suffering from behavioural and psychological symptoms of dementia (BPSD). This was consistent with the prescribing practice of some physicians who favoured benzodiazepines over antipsychotics for the treatment of BPSD, contrary to what the Beers criteria suggest.
The findings from a population-based study from Canada, where increased use of spironolactone in HF patients was accompanied by increases in the rates of hospital admissions for hyperkalemia and in-hospital death from hyperkalemia, underline the importance of using spironolactone appropriately [20]. The lack of proper monitoring plan in the separation summaries of patients with creatinine clearance <30 ml/min initiated on spironolactone is concerning. Moxonidine is not mentioned specifically in the 2015 Beers list but it is a centrally acting alpha 2 adrenoreceptor agonist, which the Beers criteria rate with a strong recommendation to avoid in elderly people. Moxonidine should be used only if first line antihypertensives are not effective or not tolerated, which was not the case with the patients who were treated with this drug in our study. These findings suggest a knowledge gap with regards to the medications in question that need to be addressed [15, 21, 22].
In the present study the prevalence of action plans addressing the approach to prescribing and monitoring of PIMs after discharge was low. Unfortunately, the present study was not designed to explore the reasons for this and further research will be required to address this issue. The need to avoid prescribing PIMs is by no means absolute, but their use should be accompanied by closer monitoring for adverse effects. One way to promote this vigilance is through the formulation of action plans for the various carers of the patients after hospitalisation, especially the local doctors.
The study provides some additional insight into the nature of change in medication complexity and in the prevalence of PIM after hospitalisation in the Australian context. However, its generalizability may be limited by its small size and single centre design. This is also the limitation regarding findings derived from data other than the primary endpoint. Another limitation of the study is the sole reliance upon the explicit parameters of the 2015 Beers Criteria to determine the appropriateness of a medication. Using a combination of explicit criteria and a thorough examination of corresponding clinical information may have yielded a more accurate picture for the use of some inappropriate medications in the study sample. Moreover, ideally future research should preferably address the prevalence of drug-related problems as well as PIM use and medication complexity. Due to the retrospective design and limited time resources, changes of medications during the hospital stays were not taken into account in this research. Identification of Beers PIMs was entirely dependent on information available in documents used as information sources, and had other sources been utilised, the prevalence of PIM may have been found to be different. Even though the present study only considered the total number of medications without differentiating to as-needed, chronic, and short-course medications, previous research by Elliot et al. suggested that the conclusions might have been similar had this been the case [17].
Conclusion
In conclusion, this study suggests that hospitalisation appears to be associated with increased medication complexity in general, but the direction and magnitude of the change in the medication complexity seems to be determined largely by a patient’s baseline MRCI and the length of hospital stay. Studying the prevalence of PIM could help to identify knowledge gaps among the health professionals regarding the use of these drugs, and with a concerted response to information gained, the quality of patient care could be improved.
References
Betteridge TM, Frampton CM, Jardine DL. Polypharmacy—we make it worse! A cross-sectional study from an acute admissions unit. Intern Med J. 2012;42:208–11.
Saad M, Harisingani R, Katinas L. Impact of geriatric consultation on the number of medications in hospitalized older patients. Consult Pharm. 2012;27:42–8.
Corsonello A, Pedone C, Corica F, Incalzi RA. Polypharmacy in elderly patients at discharge from the acute care hospital. Ther Clin Risk Manag. 2007;3:197–203.
Elliott RA, O’Callaghan CJ, Paul E, George J. Impact of an intervention to reduce medication regimen complexity for older hospital inpatients. Int J Clin Pharm. 2013;35:217–24.
George J, Phun YT, Bailey MJ, Kong DC, Stewart K. Development and validation of the medication regimen complexity index. Ann Pharmacother. 2004;38:1369–76.
Nikolaus T, Kruse W, Bach M, Specht-Leible N, Oster P, Schlierf G. Elderly patients’ problems with medication. An in-hospital and follow-up study. Eur J Clin Pharmacol. 1996;49:255–9.
Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5:345–51.
Coons SJ, Sheahan SL, Martin SS, Hendricks J, Robbins CA, Johnson JA. Predictors of medication noncompliance in a sample of older adults. Clin Ther. 1994;16:110–7.
Balkrishnan R. Predictors of medication adherence in the elderly. Clin Ther. 1998;20:764–71.
Fulton MM, Allen ER. Polypharmacy in the elderly: a literature review. J Am Acad Nurse Pract. 2005;17:123–32.
Flaherty JH, Perry HM 3rd, Lynchard GS, Morley JE. Polypharmacy and hospitalization among older home care patients. J Gerontol A Biol Sci Med Sci. 2000;55:M554–9.
Frazier SC. Health outcomes and polypharmacy in elderly individuals: an integrated literature review. J Gerontol Nurs. 2005;31:4–11.
Espino DV, Bazaldua OV, Palmer RF, Mouton CP, Parchman ML, Miles TP, et al. Suboptimal medication use and mortality in an older adult community-based cohort: results from the Hispanic EPESE study. J Gerontol A Biol Sci Med Sci. 2006;61:170–5.
Page RL II, Linnebur SA, Bryant LL, Ruscin JM. Inappropriate prescribing in the hospitalized elderly patient: defining the problem, evaluation tools, and possible solutions. Clin Interv Aging. 2010;5:75–87.
American Geriatrics Society. Beers criteria update expert panel. American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older. J Am Geriatr Soc. 2015;2015(63):2227–46.
Herings RM, Stricker BH, de Boer A, Bakker A, Sturmans F. Benzodiazepines and the risk of falling leading to femur fractures. Dosage more important than elimination half-life. Arch Intern Med. 1995;155:1801.
Elliott RA, O’Callaghan CJ. Impact of hospitalisation on the complexity of older patients’ medication regimens and potential for regimen simplification. J Pharm Pract Res. 2011;41:21–5.
Stange D, Kriston L, Wolff von A, Baehr M, Dartsch DC. Simplification of medication regimens—a novel aspect of pharmaceutical care in hospital. Eur J Hosp Pharm. 2012;19:222.
Wolfe MM. Overview and comparison of the proton pump inhibitors for the treatment of acid-related disorders. In: Post TW (Ed), UpToDate, Waltham, MA. Accessed 02 Jul 2016. https://www.uptodate.com/contents/overview-and-comparison-of-the-proton-pump-inhibitors-for-the-treatment-of-acid-related-disorders?source=search_result&search=over%20view%20proton%20pump%20inhibitors&selectedTitle=1~150.
Juurlink DN, Mamdani MM, Lee DS, Kopp A, Austin PC, Laupacis A, et al. Rates of hyperkalemia after publication of the randomized aldactone evaluation study. N Engl J Med. 2004;351:543–51.
Australian Medicines Handbook 2016 (online). Adelaide: Australian medicines handbook Pty Ltd; 2016 January. http://amhonline.amh.net.au/.
Therapeutic Goods Administration. Database of adverse event notifications (DAEN). Canberra, Australia. http://apps.tga.gov.au/PROD/DAEN/daen-entry.aspx.
Acknowledgements
The authors would like to acknowledge the help of Winifred Greenshields, Associate Director of Pharmacy, Southern Adelaide Local Health Network, who assisted by facilitating data collection. We also thank Professor Adrian Esterman, Professor of Biostatistics from the University of South Australia, for his valuable advice. We also acknowledge and appreciate support from the Ministry of Health of Singapore and Ng Teng Fong General Hospital for the first author’s participation in the study.
Funding
The authors confirm that no funding from third party has been received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There is no conflict of interest involved in the publication of the study findings.
Rights and permissions
About this article
Cite this article
Chang, W.T., Kowalski, S.R., Sorich, W. et al. Medication regimen complexity and prevalence of potentially inappropriate medicines in older patients after hospitalisation. Int J Clin Pharm 39, 867–873 (2017). https://doi.org/10.1007/s11096-017-0490-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-017-0490-y