Abstract
Background Resistance to antibiotics is a major threat to global health and general public play a significant role in the fight against antimicrobial resistance. Objective The present study aimed to identify the knowledge, attitudes, and practice of the general public towards antibiotic use in China. Setting Randomly selected parks in three cities of western, central and eastern China: Xi’an, Changsha, and Nanjing. Method A cross-sectional survey was conducted on a sample of 1400 residents, from January to June 2015. Main outcome measures Knowledge, attitudes and practices scores toward self-medication with antibiotics and compliance with antibiotic regimens. Results The response rate was 86.0% (n = 1204). Only 192 (19.5%) respondents gained a score of 3 or above, and the maximum score of 4, reflecting poor knowledge towards antibiotics. Just over half (54.8%) of respondents incorrectly believed antibiotics were effective against viral infections and only one-third (34.3%) knew that antibiotics were not anti-inflammatories. Nearly half of the respondents (49.0%) had changed the dosage when taking antibiotics, 35.6% switched to another class, 33.4% had not finished the full treatment course and over 60.0% kept leftover antibiotics for future use. Almost half of the respondents (45.7%) stated they had used antimicrobials during the last 6 months and 64.4% of them had self-medicated. Conclusion This study identified serious misconceptions regarding antibiotics use in the Chinese general public. Effective interventions should be developed to provide practical and appropriate advice to effect behaviour change within this population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Impact on practice
-
The knowledge of the Chinese population about proper use of antibiotics is low, and needs to be improved.
-
Effective measures should be taken to limit over-the-counter purchase of antibiotics.
Introduction
The emergence and spread of resistance to antibiotics is a major global public health problem for the twenty-first century [1, 2]. In 2010, a study published in “The Lancet” reported superbugs, which were highly resistant to almost all antibiotics [3]. A global report from the World Health Organization (WHO) collected data from national and international surveillance networks for the first time, highlighting the presence of antimicrobial resistance (AMR) in many parts of the world [4]. The problem is particularly acute in China, which has a higher prevalence of AMR compared with other countries [5]. For example, the overall prevalence of erythromycin-resistant Streptococcus pneumonia and ciprofloxacin-resistant Escherichia coli was 94.7% and 65.7% in community settings, respectively [6, 7].
The increase in prevalence of AMR may result in longer lasting illnesses, increased hospital stays, higher treatment costs and increased mortality rates [2]. It is estimated that by 2050, the world’s population will be reduced by between 11 million and 444 million and the global economy will be reduced by 0.1–3.1% without effective antibiotics [8]. The inappropriate and excessive use of antibiotics are the main drivers for the increase in AMR [9], and misuse of antibiotics exists not only in hospital and primary care settings, but also in the community.
Self-medication refers to the use of medicine to treat self-diagnosed disorders or symptoms, without medical supervision, which can easily lead to the inappropriate use of antibiotics [10]. Antibiotics are the most commonly self-medicated drugs in many parts of the world, with a wide variation between countries and regions. It is estimated that nearly two-thirds of all oral antibiotics used worldwide are obtained without a prescription [11]. A systematic review analysed non-prescription antimicrobial use from 1970 to 2009, based on 35 community surveys from five continents, and showed that self-medication with antibiotics varied from 3% to 100% [12]. Self-medication of antibiotics is a concerning behaviour and can lead to the indiscriminate use of drugs, incorrect dosages and incomplete courses, all of which are associated with an increased risk of resistance [2, 13, 14].
In China, antibiotics are always perceived as a panacea by the general public and some medical workers [5]. Self-medication with antibiotics is a common phenomenon in community [15, 16]. To combat AMR, the State Food and Drug Administration has restricted antibiotics to prescription-only medicines since 2004 [17]. The dispensing of antibiotics in China is only legal when they are prescribed by practitioners. However, antibiotics can be easily purchased without prescription and are accessible from most community pharmacies [14].
Non-adherence to antibiotic regimens and inappropriate antibiotic use are strongly associated with public awareness and knowledge of antibiotics [18]. Several studies [19,20,21,22] have discussed the correlation between the patients’ perceptions of antibiotic and the behavior of using antibiotic. Many of these have found that a higher level of knowledge was a predictor for a positive attitude, which will ultimately influence patients’ self-medicating behaviour. The general public therefore, play a significant role in reducing indiscriminate use of antibiotics and it is essential to understand their awareness of antimicrobials. There have been some single-center studies in China investigating the use, knowledge, attitudes and behaviours of the general public [23], doctors [24], students [19, 25,26,27], and parents [26, 28] towards antimicrobials. To the best of our knowledge, there are few studies situated in China focusing on public awareness and attitudes towards AMR.
Aim of the study
The objective of this study was to explore knowledge, attitudes, and practice (KAP) towards antibiotic use in the general public in eastern, central and western China.
Ethics approval
Xi’an Jiaotong University Health Science Center, Shaanxi Provincial Department of Health and Shaanxi Food and Drug Administration approved the study prior to data collection. The participants were informed of the aims of our study prior to participation. All participants gave a verbal consent to participate in this survey. Ethical approval was obtained from the Xi’an Jiaotong University’s Research Ethics Committee.
Method
Study design and population
A cross-sectional survey was designed and conducted in a sample of the Chinese general public, between January and June 2015. Based on the per capita gross domestic product, and geographic location, the research was conducted in three cities of western, central and eastern China: Xi’an, Changsha, and Nanjing. We used a multi-stage sampling design. Within each city, four districts were chosen and in each chosen district the largest park was selected. Questionnaires were given to randomly selected adults in each park. This study was carried out on working days as well as weekends, and at different times of the day. Sample size was determined using the Raosoft sample size calculator [29], with a 5% margin of error, a confidence interval of 95%, and an expected response rate of 50%. The minimum sample size estimated for the study was 384 participants from each city. Assuming an attrition rate of 20%, a sample of 1400 people was enrolled on to this study. The inclusion criteria were: (1) adults aged 18 years and over; (2) people who understood the term antibiotic and had used antibiotics at any point during their lifetime; and (3) Chinese speakers who lived in the study area and agreed to take part in the study.
Data instrument and collection
A five-part questionnaire, containing 29 closed questions, was adapted and modified from previous studies [25, 27, 30,31,32]. Part one included questions on the respondents’ demographic characteristics. Part two investigated the respondents’ knowledge about antibiotic indications, antibiotic administration, and use of antibiotics. This section was assessed using a three-point scale; ‘Yes’, ‘No’ or ‘Uncertain’ and also included a multiple-choice question about the source of their antibiotic knowledge. Parts three and four were based on a 5-point Likert scale to evaluate attitudes and practices towards self-medication with antibiotics and compliance with antibiotic regimens, with answers ranging from “strongly agree” to “strongly disagree”, or from “always” to “never”. Part five was designed to investigate recent use of antibiotics (within the past 6 months). Participants were required to complete further information, including the frequency, source and reason for taking antibiotics, if they had taken antibiotics without prescription during this period.
The questionnaire was available in Chinese and was validated by a clinical pharmacist and a professor of Pharmacy Administration. To optimize the clarity of the language used and questionnaire structure, a pilot study was conducted among 30 participants at a park in Xi’an. We also tested the validity and reliability of the questionnaire, to validate its internal consistency and the coefficient. Cronbach’s Alpha of knowledge, attitude and practice part was 0.75, 0.81 and 0.79 respectively, giving a reasonable level of validity [33].
Data collection was completed by graduate students specializing in Pharmacy Administration at Xi’an Jiaotong University. Questionnaires were randomly given to the general public and collected face-to-face by investigators to increase the response rate. In the covering letter, participants were informed of the purpose of the study and the generic names of the commonly used antibiotics. All study participants gave a verbal consent to participate in the study.
Data management and analysis
All data were entered and verified using EpiData version 3.1 (Odense, Denmark), and analysed using SPSS version 18.0 (SPSS Inc., Chicago, IL). A scoring system was used to assess respondents’ KAP. In the knowledge section, 1 point was given for each correct answer and 0 for each mistake or unsure response. In the attitude and behaviour section, responses were given a corresponding score of 5, 4, 3, 2 and 1 for positive response to negative response. Descriptive statistical analysis was reported as frequency and median (interquartile range, hereinafter referred to as IQR). Wilcoxon signed-rank and Kruskal–Wallis tests were used to examine differences between median scores. Chi square tests were used to determine the influence of demographic characteristics on self-medication. The questionnaire which has more than three of the unfinished items in the first part was excluded from further analysis. In all statistical analyses, the level of statistical significance was set at P < 0.05.
Results
In total, 1400 questionnaires were distributed and 1255 returned (89.6% response rate). Fifty-one questionnaires were excluded because of incomplete data, resulting in a final response rate of 86.0%. Detailed demographic characteristics of the respondents are presented in Table 1. In total, there were 405 (33.6%) from Xi’an, 405 (33.6%) from Changsha, and 385 (32.8%) from Nanjing. The gender of respondents were distributed almost equally (51.7% were male while 48.3% were female). No more than 15.0% of participants stated they were uninsured, and more than half of respondents (62.5%) characterized their health status as good. The majority of respondents had completed high school (80.5%) and were employed or self-employed (64.3%).
Knowledge
The overall median knowledge score was 1 (IQR 0–2), out of a maximum of 4. Only 192 (15.9%) respondents gained a score of 3 or above, demonstrating poor knowledge of antibiotics. There were significant differences in knowledge scores between participants in different cities (P < 0.001), age groups (P < 0.001), education level (P < 0.001) and employment status (P < 0.001) (Table 1). Respondents with a higher education level, 18–30 year olds, students and Nanjing residents were found to contribute significantly to the overall knowledge score.
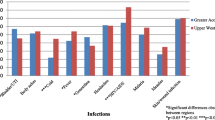
This study identified some confusion surrounding the role of antibiotics. Just over half (n = 659; 54.8%) of participants incorrectly agreed that “antibiotics are effective against viral infections” and only one-third (n = 413; 34.3%) of participants knew that antibiotics and anti-inflammatories are not the same drugs. Additionally, fewer than half of respondents knew that antibiotics should only be purchased with a prescription (n = 585; 48.6%). Differences were identified between Xi’an, Changsha and Nanjing for the above three statements (Table 2). Furthermore, the study participants demonstrated poor knowledge about the use of antibiotics. Just over half of participants (n = 687; 57.1%) agreed with the statement “It is okay to stop taking an antibiotic when symptoms are improving”.
Attitude
In the section assessing attitude, the overall median score was 17 (IQR 15–18) out of a maximum score of 25, reflecting a moderate attitude towards antibiotics. Attitude score was associated with age (P < 0.001), education level (P < 0.001), employment status (P = 0.002), health insurance (P = 0.013), self-rated health status (P = 0.019) and study area (P < 0.001) (Table 1). It was noted that lower educational qualifications, 41–60 year olds, having no health insurance and being resident in Xi’an were strongly associated with a negative attitude about the use of antibiotics.
Table 3 showed the frequency and percentage of responses for the statements about attitude. A small proportion (n = 174; 14.4%) incorrectly believed that antibiotics can be used immediately to treat the common cold. About 11.0% (n = 141) of respondents agreed that expensive antibiotics are more effective and have fewer side effects. Nearly one-third (n = 373; 31.0%) of participants would use leftover antibiotics if they had a respiratory tract infection. A considerable proportion of respondents (n = 523; 43.4%) incorrectly agreed that they could change the dosage by themselves during the course of antibiotic treatment. However, only 452 (37.5%) of respondents were aware that treatment effectiveness would be reduced if the full course of antibiotic was not completed.
Practice
The median practice score was 18 (IQR 16–20) out of a maximum score of 25. Respondents from Nanjing and Changsha had higher scores for their antibiotic practices compared with respondents from Xi’an, with median scores of 18 and 18 compared with 17 (P < 0.001) (Table 1).
When assessing behaviour, the majority of participants (77.0%) had kept leftover antibiotics at home in case of future need. Incorrect use of antibiotics existed in respondents in this survey; 16.4% of respondents stated they would change the dosage and 6.3% of respondents stated they would switch antibiotics during the course of antibiotic treatment by themselves. Furthermore, less than one-third (28.8%) of respondents stated they had finished the full course of antibiotic treatment. Detailed frequencies of responses about practices are shown in Table 4.
Recent use of antibiotics
When investigating recent use of antibiotics, 550 (45.7%) respondents stated they had used antimicrobials in the last 6 months, while 352 (64.0%) respondents had self-medicated. Self-medication was significantly influenced by age (P = 0.009) and self-rated health status (P = 0.007). 18–40 year olds, or self-rated good health status of the respondents were more likely to use antibiotics for self-treatment. The main source of self-medicated antibiotics was retail pharmacies (80.2%). Other sources included leftover medication from a previous prescription (17.8%) and friends (2.0%). A cough, sore throat, and bronchitis were the most frequent reasons reported for antibiotic use, followed by a runny nose, nasal congestion, fever and toothache.
Discussion
This is the first questionnaire survey to be conducted in eastern, central and western China to provide baseline data regarding the KAP towards the use of antibiotics among Chinese general public.
Knowledge
The present study revealed insufficient general knowledge about antibiotics, particularly the role of antibiotics. In a survey of the general public in Malaysia, 67.2% incorrectly thought that antibiotics were also used to treat viral infections [32]. In China, 21.0% of parents believed that antibiotics could be effective for viral infections and 34.0% thought antibiotics were the same as anti-inflammatories [28]. In Kuwait, there was a lower standard of knowledge regarding antimicrobials, as 46.2% of respondents incorrectly believed antibiotics are effective against viruses [34]. Furthermore, the present study also found that less than half of respondents knew that antibiotics should be purchased with a doctor’s prescription, which may be an important reason for self-medication.
Attitude
Our findings indicated that the prevalence of inappropriate attitudes towards antimicrobials was high. Specifically, 14.1% of participants agreed that they would take antibiotics when they got a common cold, 31.0% would use leftover antibiotics for respiratory tract infections and 43.4% would change the dosage by themselves during the course of antibiotic treatment. These results were slightly different compared with previous studies. A survey conducted in western China showed that 35.1% of college students had a positive attitude towards antibiotic use for the common cold [25]. In Malaysia, a survey conducted in 2012 reported 14.7% of respondents believed that “I will use leftover antibiotics for a respiratory illness (runny nose/sore throat/flu)” and only 3.5% of patients would take antibiotics according to the instructions on the label [30]. Most respiratory infections are self-limiting and caused by viruses, and cannot be treated with antibiotics [13].
Self-medicating behaviour
Regarding self-medication with antibiotics, just under a third (29.2%) of respondents classified themselves as having self-medicated in the previous 6 months. This is similar to data reported from previous studies in Kuwait, Italy, Jordan and Bangladesh [34,35,36,37]. However, it is lower than in other areas of China, the United Kingdom, Malaysia and Mongolia [18,19,20, 25], and higher than in the Algarve and Albania [38, 39]. The difference in prevalence of self-medication with antibiotics in these studies could be attributed to the use of different methods in the studies, as well as different study areas, populations, sample sizes, the period of investigation and awareness of antibiotics.
The present study also revealed that people were less likely to adhere to the full course of antibiotics when self-medicating. Inappropriate use and over-use of medicines does not only waste resources, but also results in difficulties for further treatment [40]. Furthermore, inappropriate use and over-use of antibiotics is leading to increased AMR.
Limitations
There are several limitations in this study. First, it was conducted in parks, therefore only included the specific group of people, and has excluded anyone who may be unwilling or unable to go outdoors, which will inevitably have introduced some selection bias to the sample. To improve the sample’s representativeness, the present study was conducted on both work and non-work days, and at different times of the day; and if there were a crowd of people, we only surveyed one person from them to avoid the cluster effect. Second, similar to other self-administered surveys, the results obtained are reliant on the honesty, understanding and recall ability of the respondents. Finally, this is a cross-sectional study representing one point in time, and may not reflect any dynamic changes in respondents’ awareness with regard to the use of antibiotics.
Conclusion
The Chinese general public has serious misconceptions and moderate attitude towards use of antibiotics. A considerable proportion of respondents self-medicated with antibiotics in the past 6 months, and the indiscriminate use of antibiotics was prevalent. Legislation should be developed and implemented to enforce regulations limiting over-the-counter purchase of antibiotics. Health education and interventions for the general public should be established to promote prudent use of antibiotics in the general population.
References
World Health Organization. The world health report 2007. A safer future: global public health security in the 21st century. http://www.who.int/whr/2007/en/. Accessed 28 Oct 2015.
World Health Organization. WHO global strategy for containment of antimicrobial resistance. http://www.who.int/csr/resources/publications/drugresist/WHO_CDS_CSR_DRS_2001_2_EN/en/. Accessed 28 Oct 2015.
Kumarasamy KK, Toleman MA, Walsh TR, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis. 2010;10:597–602.
World Health Organization. Antimicrobial resistance: global report on surveillance 2014. http://www.who.int/drugresistance/documents/surveillancereport/en/. Accessed 28 Oct 2015.
Xiao Y, Zhang J, Zheng B, et al. Changes in Chinese policies to promote the rational use of antibiotics. PLoS Med. 2013;10:e1001556.
Xiao YH, Giske CG, Wei ZQ, et al. Epidemiology and characteristics of antimicrobial resistance in China. Drug Resist Update. 2011;14:236–50.
Xiao YH, Shen P, Wei ZQ, et al. Mohnarin report of 2011: monitoring of bacterial resistance in China. Chin J Nosocomiol. 2012;22:4946–52.
Taylor J, Hafner M, Yerushalmi E, et al. Estimating the economic costs of antimicrobial resistance: model and results. http://www.rand.org/content/dam/rand/pubs/research_reports/RR900/RR911/RAND_RR911.pdf. Accessed Oct 11 2016.
You JHS, Yau B, Choi KC, et al. Public knowledge, attitudes and behavior on antibiotic use: a telephone survey in Hong Kong. Infection. 2008;36:153–7.
World Health Organization. Guidelines for the regulatory assessment of medicinal products for use in self-medication. http://apps.who.int/medicinedocs/en/d/Js2218e/. Accessed 28 Oct 2015.
Council USNI. National intelligence estimate: the global infectious disease threat and its implications for the United States. ECSP Rep. 2000;6:33–65.
Morgan DJ, Okeke IN, Laxminarayan R, et al. Non-prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis. 2011;11:692–701.
Grigoryan L, Haaijer-Ruskamp FM, Burgerhof JGM, et al. Self-medication with antimicrobial drugs in Europe. Emerg Infect Dis. 2006;12:452–9.
Li Y. China’s misuse of antibiotics should be curbed. BMJ. 2014;348(feb125):g1083.
Kan Q, Wen J, Liu X, et al. Inappropriate use of antibiotics in children in China. Lancet. 2016;387:1273–4.
Wun YT, Lam TP, Lam KF, et al. The public’s perspectives on antibiotic resistance and abuse among Chinese in Hong Kong. Pharmacoepidemiol Drug Saf. 2013;22:241–9.
State Food and Drug Administration. The five prescription sales only antibacterial released by SFDA. http://eng.sfda.gov.cn/WS03/CL0757/61674.html. Accessed 11 Oct 2016.
McNulty CAM, Boyle P, Nichols T, et al. Don’t wear me out—the public’s knowledge of and attitudes to antibiotic use. J Antimicrob Chemother. 2007;59:727–38.
Pan H, Cui B, Zhang D, et al. Prior knowledge, older age, and higher allowance are risk factors for self-medication with antibiotics among university students in southern China. PLoS ONE. 2012;7:e41314.
Togoobaatar G, Ikeda N, Ali M, et al. Survey of non-prescribed use of antibiotics for children in an urban community in Mongolia. Bull World Health Organ. 2010;88:930–6.
Grigoryan L, Burgerhof JG, Degener JE, et al. Attitudes, beliefs and knowledge concerning antibiotic use and self-medication: a comparative European study. Pharmacoepidemiol Drug Saf. 2007;16:1234.
Li YF, Rao KQ, Ren XW. Use of and factors associated with self-treatment in China. BMC Public Health. 2012;12:1–9.
Gu J, Zhao J, Huang Y, et al. Use of antibiotics by urban and rural residents in Heilongjiang Province, China: cross-sectional study. Trop Med Int Health. 2015;20:1815–22.
Sun Q, Dyar OJ, Zhao L, et al. Overuse of antibiotics for the common cold–attitudes and behaviors among doctors in rural areas of Shandong Province, China. BMC Pharmacol Toxicol. 2015;16:6.
Lv B, Zhou ZL, Xu GP, et al. Knowledge, attitudes, and practices concerning self-medication with antibiotics among university students in western China. Trop Med Int Health. 2014;19:769–79.
Huang Y, Gu J, Zhang M, et al. Knowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese students. BMC Med Educ. 2013;13:163.
Zhu X, Pan H, Yang Z, et al. Self-medication practices with antibiotics among Chinese university students. Public Health. 2016;130:78–83.
Yu M, Zhao G, Lundborg CS, et al. Knowledge, attitudes, and practices of parents in rural China on the use of antibiotics in children: a cross-sectional study. BMC Infect Dis. 2014;14:1–8.
Sample size calculator. http://www.raosoft.com/samplesize.html. Accessed 28 Oct 2015.
Lim KK, Teh CC. A cross sectional study of public knowledge and attitude towards antibiotics in Putrajaya, Malaysia. South Med Rev. 2012;5:26–33.
Jose J, Jimmy B, AlSabahi AGMS, Al Sabei GA. A study assessing public knowledge, belief and behavior of antibiotic use in an Omani population. Oman Med J. 2013;28:324–30.
Ling OA, Hassali MA, Al-Haddad MS, et al. Public knowledge and attitudes towards antibiotic usage: a cross-sectional study among the general public in the state of Penang, Malaysia. J Infect Dev Ctries. 2011;5:338–47.
Iacobucci D, Duhachek A. Advancing alpha: measuring reliability with confidence. J Consum Psychol. 2003;13:478–87.
Awad AI, Aboud EA. Knowledge, attitude and practice towards antibiotic use among the public in Kuwait. PLoS ONE. 2015;10:e0117910.
Napolitano F, Izzo MT, Di GG, Angelillo IF. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS ONE. 2013;8:e84177.
Shehadeh M, Suaifan G, Darwish RM, et al. Knowledge, attitudes and behavior regarding antibiotics use and misuse among adults in the community of Jordan. A pilot study. Saudi Pharm J. 2012;20:125–33.
Biswas M, Roy MN, Manik MI, et al. Self medicated antibiotics in Bangladesh: a cross-sectional health survey conducted in the Rajshahi City. BMC Public Health. 2014;14:847.
Ramalhinho I, Cordeiro C, Cavaco A, et al. Assessing determinants of self-medication with antibiotics among Portuguese people in the Algarve Region. Int J Clin Pharm. 2014;36:1039–47.
Jorgji K, Bebeci E, Apostoli P, Apostoli A. Evaluation of use of antibiotics without prescription among young adults in Albania case study: Tirana and Fier District. Hippokratia. 2014;18:217–20.
World Health Organization. Promoting rational use of medicines: core components. http://apps.who.int/medicinedocs/collect/medicinedocs/pdf/h3011e/h3011e.pdf?ua=1. Accessed 28 Oct 20.
Funding
The “Young Talent Support Plan” of Xi’an Jiaotong University; the China Medical Board Open Competition Program (14–196).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ye, D., Chang, J., Yang, C. et al. How does the general public view antibiotic use in China? Result from a cross-sectional survey. Int J Clin Pharm 39, 927–934 (2017). https://doi.org/10.1007/s11096-017-0472-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-017-0472-0