Abstract
Background Geriatric falls are leading causes of hospital trauma admissions and injury-related deaths. Medication use is a crucial element among extrinsic risk factors for falls. To reduce fall risk and the prevalence of adverse drug reactions, potentially inappropriate medication (PIM) lists are widely used. Objective Our aim was to investigate the possible predictors of geriatric falls annualized over a 5-year-long period, as well as to evaluate the medication use of nursing home residents. Setting Nursing home residents were recruited from the same institution between 2010 and 2015 in Szeged, Hungary. Method A retrospective epidemiological study was performed. Patient data were analysed for the first 12 months of residency. Chi-squared test and Fisher’s-test were applied to compare the categorical variables, Student’s t test to compare the continuous variables between groups. Binary logistic regression analysis was carried out to determine the association of falls with other variables found significant in univariate analysis. Microsoft Excel, IBM SPSS Statistics (version 23) and R (3.2.2) programs were used for data analysis. Main outcome measure Falls affected by age, gender, number of chronic medications, polypharmacy, PIM meds. Results A total of 197 nursing home residents were included, 150 (76.2%) women and 47 (23.8%) men, 55 fallers (annual fall prevalence rate was 27.9%) and 142 non-fallers. Gender was not a predisposing factor for falls (prevalence in males: 23.4 vs 29.3% in females, p > 0.05). Fallers were older (mean years ± SD; 84.0 ± 7.0) than non-fallers (80.1 ± 9.3, p < 0.01). The age ≥80 years was a significant risk factor for falls (p < 0.001). The number of chronic medications was higher in male fallers (12.4 ± 4.0) than in non-fallers (6.9 ± 4.2, p < 0.001). Polypharmacy (taking four or more chronic medications) was a significant risk factor of falls (p < 0.01). Those PIMs carrying fall risk were taken by 70.9% of fallers and 75.3% of non-fallers (p > 0.05). Taking pantoprazole, vinpocetine or trimetazidine was a significant risk factor for falls. Conclusion Older age, polypharmacy and the independent use of pantoprazole, vinpocetine, and trimetazidine were found to be major risk factors for falls. Further real-life epidemiological studies are necessary to confirm the role of particular active agents, and to help professionals prescribe, evaluate and review geriatric medication use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
Older age (above 80 years) is a main risk factor for falls among nursing home residents.
-
Polypharmacy is an independent risk factor for falls.
-
Taking pantoprazole, vinpocetine or trimetazidine is significant risk factors for falls; therefore patients using these medications may require special attention during the medication reviews (the role of trimetazidine as a risk factor for falls was confirmed only by univariate analysis).
Introduction
Falls of the elderly are one of the leading causes of hospital trauma admissions and injury-related deaths [1]. Approximately one-third of community-dwelling elderly above the age of 65, and approximately 30–50% of people living in long-term care institutions fall each year, resulting in bone fractures, worsened quality of life, loss of independence, fear of falling, disability and early death [2, 3].
Amongst fall-related low-energy bone fractures, hip fractures are responsible for the greatest costs and high mortality rates: nearly 20% of people with hip fracture will die within one year. Although falls are more common among older women than men, in the case of hip fracture, the mortality rate is almost double in males than in females (31 vs 17%) [4–6]. Therefore guidelines and policies on fall prevention need to be adverted on gender perspective, as well as on populations under the greatest risk, such as nursing home residents. According to the Centers for Disease Control and Prevention (CDC), approximately 5% of adults above 65 years live in nursing homes, but these residents account for about 20% of deaths from falls in this age group. Although many falls remain unreported, patients often fall more than once a year. In a typical nursing home, the annual average number of falls is 2.6 per patient [1].
Many studies have revealed a variety of factors or conditions that can increase the risk of falling in elderly patients, such as older age, comorbidities, vision disturbance, diabetes and depression [5, 7, 8]. Also, medication use is a crucial element among extrinsic risk factors for falls. Although comorbidities in older people often require taking numerous prescription drugs, taking four or more chronic medications (defined as polypharmacy) was found to be an independent risk factor for falls [8, 9]. Polypharmacy (PP) also increases the prevalence of drug-related problems (DRPs), such as drug–drug interactions, adverse drug reactions (ADRs), prescription errors and non-adherence [10, 11]. Though there is no consensus about the exact cut-off value for polypharmacy, usually it is defined as the concomitant use of more than or equal to 4–8 chronic medications [7, 12, 13]. Polypharmacy is quite common in geriatric patients: the prevalence in the U.S. is around 57%, while a large European study reported 51% [14, 15].
To reduce the risk of falls and to minimize the prevalence of adverse drug reactions, potentially inappropriate medication (PIM) lists have been implemented, among which the ‘Beers criteria’ is the most widely used, outstarter list [16]. Originally its use was restricted for nursing home residents, then it was extended for any geriatric patients. The most recently updated (2015) list identifies not only the potentially inappropriate drugs, but also offers recommendation on alternative medications or therapies [17].
Following the Beers criteria, numerous countries have created their specific national PIM list, adding or withdrawing medications, adapted to the country’s therapeutic practice and pharmaceutical market. Using these medication lists is a substantial strategy to reduce the risk of adverse events and falls in older adults; however, the lists are hardly confirmed by real epidemiological data.
Aim of the study
The aim of the study was to investigate the possible predictors of geriatric falls annualized over a 5-year-long period, as well as to evaluate the medication use of nursing home residents.
Ethics approval
The present study was approved by the Regional Human Biomedical Research Ethics Committee of the University of Szeged. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Methods
A retrospective analysis was done regarding the medication use and fall prevalence in nursing home residents, all recruited from the same institution, between August 2010 and August 2015 in Szeged, Hungary. The main outcome measures were falls affected by age, gender, number of chronic medications, polypharmacy and PIM meds.
Patients and setting
Every patient who was the resident of the investigated nursing home for at least 12 months was included into the study. Patient data were recorded and analysed for the first 12 months of residency, starting from the date of admission. Relevant medication lists and demographic information were collected from the patient medical documentation of the facility. Detailed data on falls were available from hospital discharge documents since, after noticed falls, all residents were admitted to hospital for further investigation according to the nursing home protocol.
The nursing home provides residential accommodation, meals and 24-hour personal care (residential nursing) for those who find it difficult to cope without assistance. The facility is fully accessible and barrier-free. Daily medical supervision is also ensured (neurologist and gerontologist).
Due to the local policy, deceased patients were excluded from this study, since we had no data access on those patients’ medical information.
Data analysis and statistical methods
Microsoft Excel (Microsoft Office 2010, Microsoft Corporation, Redmond, WA), IBM SPSS Statistics for Windows (version 23, IBM Corporation, Armonk, NY) and R (version 3.2.2, R Foundation for Statistical Computing, Vienna, Austria) programs were used for data management and analysis.
A Chi-squared test was applied to compare the categorical variables (e.g. gender) between the investigated groups, and Fisher’s test in case of polypharmacy. Student’s t test was performed to compare the continuous variables (e.g., age, number of medications) between groups. Polypharmacy is defined as the concomitant use of equal to or more than four chronic medications.
Positive predictive value (PPV)
We examined the prevalence and PPV with 95% confidence intervals, to estimate the possible impact of each medication (active substance) on risk of falls by the widely used, basic architecture (2 by 2 contingency table) of cohort studies [18].
PPV is the proportion of patients taking a particular (investigated) drug and who had fall(s). In other words it shows the probability of an outcome (fall) if the patient has the tested condition (takes the particular drug). These proportions only have limited validity in clinical practice, however. The predictive values of a clinical test depend critically on the prevalence of the condition (falls) in the patients being tested within a particular environment. [19].
Number needed to harm (NNH)
NNH was calculated for those active agents which have high PPV, and where the lower CI 95% value exceeded the annual fall prevalence rate. The NNH index expresses how many patients need to be exposed to a certain risk-factor (drug) to cause harmful effect (fall) in one patient over a specific time period (1 year) [20, 21]. Nevertheless, NNH values calculated in our study cannot be extended for the entire population of elderly people; they are valid only for those nursing home residents involved in this analysis.
Binary logistic regression analysis
Binary logistic regression analysis was carried out to determine the association of falls with other variables found significant in univariate analysis. Logistic regression was characterized by the accuracy of test [20, 21].
Potentially inappropriate medications
To identify the potentially inappropriate medications, four commonly used PIM lists have been adopted to the Hungarian drug market and to our data on medication use, i.e. the updated Beers criteria (2015), the French LaRoche list (2007), the German Priscus list (2010) and the Austrian Mann list (2012) [17, 22–24]. The adopted list consists of 94 drugs or active ingredients (PIMs), out of which 54 drugs (PIM fall risk) were considered high-risk drugs in terms of falls (based on the rationale of the original lists). The prevalence of exposure to these medicines was illustrated by Venn diagram [25].
Results
Demography
A total of 197 nursing home residents were included in the study, 150 (76.2%) women and 47 (23.8%) men (Table 1.) Among the 55 fallers (so the annual fall prevalence rate was 27.9%), 44 were females and 11 were males. Out of the 142 non-faller residents, 106 were females and 36 were males. The gender was not found to be a predisposing factor for falls (prevalence in males: 23.4 vs 29.3% in females, p > 0.05). Bone fractures occurred in 24 patients (5 males and 19 females, 43.6% of fallers).
Regarding age, fallers were older (84.0 ± 7.0 years) than non-fallers (80.1 ± 9.3 years, p < 0.01). The age above or equal to 80 years was found to be a significant risk factor for falls (p < 0.001). Among fallers, 47 residents (85.5%) were 80 years old or older, and all the 13 multiple fallers (more than 1 fall per year) were in this group.
Medication patterns
The number of chronic medications taken did not significantly differ between fallers and non-fallers (9.1 ± 3.8 vs 8.0 ± 3.9, p > 0.05) (Table 1), but did differ among male patients (fallers 12.4 ± 4.0 vs non-fallers 6.9 ± 4.2, p < 0.001). Also, polypharmacy (taking four or more chronic medications) was a significant risk factor of falls (p = 0.010).
Potentially inappropriate medications
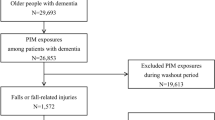
Regarding the prevalence of PIM medication use, 77.2% of the residents took one or more PIM-list drugs, and there was no significance in prevalence between fallers and non- fallers (72.7 vs 78.9%, p > 0.05). Those PIMs carrying risk of falls were taken by 70.9% of fallers and 75.3% of non-fallers (p > 0.05). Comparing to PIM prevalence, polypharmacy occurred in 85.9% non-faller patients, but in 98.2% fallers (p < 0.01). PIM use was illustrated on the Venn diagram (Fig. 1a, b). To provide better understanding, we also included the age dimension into this visualisation.
a Venn diagram illustrates the populations (sets) that were subject to multiple drug use: residents taking potentially inappropriate medications (PIM) with fall risk; fallers; patients who were 80 years old or older, and those who were not part of the other three sets. b Venn diagram illustrates the populations (sets) that were subject to multiple drug use: those residents taking four or more chronic drugs (Polypharmacy); fallers; patients who were 80 years old or older, and those who were not part of the other three sets
Drugs and falls
Except for two non-medicated residents, 195 were taking 227 different drugs, out of which 22 drugs were taken by at least 10% of the patients (minimum 20 individuals, Table 2).
For the most prevalent drugs, positive predictive values (with 95% confidence intervals) were calculated to estimate the impact of each medication on fall risk. Considering the 27.9% annual fall prevalence rate in the nursing home, the lower confidence interval exceeded this margin in case of trimetazidine (PPV (95% CI), 0.48, (0.30–0.66), vinpocetine 0.44 (0.31–0.59) and pantoprazole 0.40 (0.30–0.52). Hence, those drugs seem to be significant risk factors for falls (Table 2; Fig. 2). Giving an example for better understanding, expanding the definition of PPV, the 0.40 PPV of pantoprazole shows the proportion of patients who used pantoprazole and who had fall(s). This means that taking the drug increases the fall prevalence rate by approximately 12% (compared to the annual 27.9% fall prevalence rate).
For the same drugs, the number needed to harm (NNH, 95% CI) was calculated (groups were the following: particular drug user or non-user, and the outcome/risk was falls). Accordingly, approximately 4–5 patients are needed to be exposed to trimetazidine and vinpocetine use to sustain a fall, while this number is about 6 in the case of pantoprazole exposure (Table 3). These numbers are clinically remarkable. We would like to emphasize that the NNH values calculated above cannot be extended for the entire population of older adults; they are valid only for the involved nursing home residents.
The variables of the binary logistic regression model were the following: age group 80 years and above, persons taking pantoprazole, vinpocetine or trimetazidine. Binary logistic regression confirmed the significant impact of the 80+ age group, pantoprazole, and vinpocetine on fall risk, odd ratios were respectively 3.92, 2.59 and 2.32, with 73.6% accuracy detected, but did not confirm the impact of trimetazidine (Table 4).
Discussion
This retrospective cohort study was carried out over a period of five years (2010–2015) regarding the medication use and fall prevalence among nursing home residents in Szeged, Hungary. We found 27.9% annual fall prevalence rate among nursing home residents, which is slightly lower than the literature data. According to CDC and WHO reports, approximately 30–50% of people living in long-term care institutions fall each year, which is twice the rate of falls among community-dwelling older adults, and the frequency of falls increases with age [1, 2, 26]. Our results correspond to these findings: the age of 80 years or above was found to be statistically significant risk factor of falls, and fallers were 4 years older than non-faller residents on average. Therefore, attention should be paid to the 80+ population, since they had almost a fourfold risk of falling (odds ratio 3.92) compared to those who were under the age of 80 years.
Although many geriatricians consider polypharmacy (defined as taking four or more chronic medications) to be unavoidable among older patients, PP was a significant risk factor of falls in our study, as it is supported by different surveys and reviews [5, 7, 13].
Higher numbers of chronic medications was a predisposing factor for falls in male patients. This is an important finding, since fatal fall outcome rates are much higher in men (46%) than in women (27%) over the age of 65 years [27]. The underlying causes of higher incidence in men are not obvious. Some studies found that males suffer from more co-morbid conditions or they may fall from greater heights and, having poorer health status, they are less likely to survive a fall-related injury than women of comparable age [27, 28]. Among the potential causes, the greater rates of smoking and alcohol abuse in men, along with commoner causes of secondary osteoporosis (e.g., glucocorticoid excess and hypogonadism) can be mentioned [29, 30]. As was highlighted earlier, the mortality rates are also nearly double in men than in women after sustaining a hip fracture [4–6]. Thus guidelines and policies on fall prevention need to be deigned on gender perspective, particularly in vulnerable nursing home populations.
As the most serious non-fatal consequence of falls, bone fractures occurred in 24 patients (43.6% among fallers). Although huge differences can be seen in fracture rates worldwide, our study reports higher percentages than a Sweden study (1–33%) or a US study (10–25%) do, and lower than the one identified in a recent Australian paper (about 48%) [31–33].
One possible way of reducing fall risk (and consequences) of elderly patients is the frequent and regular medication review, as some of the medications are considered potentially inappropriate for elderly people [17, 22–24]. Although our results did not show a difference in the number of overall PIM-use between fallers and non-fallers, three active agents have emerged from the others. Neither trimetazidine nor vinpocetine have been considered as PIM agents in the literature previously. Pantoprazole was included in the 2015 Beers criteria, but was not included in any PIM lists before. The updated Beers criteria suggests the avoidance of the use of pantoprazole beyond 8 weeks without justification, since long-term proton-pump inhibitor exposure carries high risk of Clostridium difficile infection, bone loss and fractures. Thus, our empirical findings extend the relevancy of pantoprazole being mentioned as a PIM agent with a new aspect: its use showed 2.5-fold risk of falls compared to non-takers, and one in every six patients would be expected to result in a fall (NNH value 5.9). As stated in the summary of product characteristics (SPC), severe hypomagnesaemia has been reported in patients, causing fatigue, tetany, delirium, convulsions and dizziness, especially on long-term use (more than 3 months), which can directly lead to geriatric falls [34]. As pantoprazole is an extensively used proton pump inhibitor, its side effects are widely studied. In fact, several recent articles suggest that its use in high doses over long durations (>1 year) may modestly increase the risk of bone fractures; thus, patients at risk of osteoporosis should receive adequate intake of vitamin D and calcium, and should be kept under regular surveillance [34, 35].
Both vinpocetine (nootropic agent) and trimetazidine (anti-anginal agent) can have side effects that may increase the risk of falls, such as tremors, gait instability and dizziness [36–38]. However, we could not find any research that would confirm the direct association between falls and the use of these medications. Our results from the binary logistic regression analysis revealed that taking vinpocetine will double the risk of falls (odds ratio 2.32), and the obtained NNH values suggest that every fourth or fifth exposure to trimetazidine or vinpocetine will result in a fall—within the given circumstances. We would like to emphasize that the role of trimetazidine as a risk factor for falls was confirmed only by univariate analysis (Table 2). Larger patient numbers are necessary to support this finding, since the more robust multivariate analysis did not confirm this result (Table 4).
The use of tiapride PPV (CI 95%) 0.43 (0.27–0.60), atorvastatin 0.41 (0.27–0.58) or isosorbide mononitrate 0.45 (0.26–0.65) was found to be a statistically non-significant (as the confidence interval overlap the average annual fall rate), but still mentionable, risk for falls.
Our methods applied in this study would fit in larger population analysis as well, and it may allow us deeper understanding of the role of each medication (or their combinations) concerning falls, especially as geriatric falls are multifactorial. Hence an explicit detachment of the causative circumstances is challenging. Physical state, impaired balance and gait, older age, visual impairment, cognitive decline and environmental factors all carry remarkable fall risk [5, 7]. Despite these facts, the most broadly examined iatrogenic risk factors are polypharmacy and PIM use, since those are closely associated with ageing [9, 13–15, 17, 39]. As mentioned earlier, wider, comprehensive epidemiological studies would be necessary to confirm the role of particular active agents, and to help professionals prescribe, evaluate and review geriatric medication use by real-life epidemiological data. Our results may contribute to and inspire further research in this field.
Limitations of the study
The source of data for our analysis performed came from the same nursing home, and we did not have access to the medical information of deceased patients. This limitation may cause some distortion in our results. Furthermore, while some falls may have remained hidden and unreported for any reason, the documented cases were well-established. Finally, larger patient data are needed to confirm our findings, since we had relatively small sample sizes for epidemiological analyses.
Conclusions
A retrospective cohort study was performed regarding medication use and fall risk among nursing home residents. Older age (80 years or above), polypharmacy, and the independent use of three active agents (pantoprazole, vinpocetine, or trimetazidine) were found to be major risk factors for falls. High numbers of chronic medications taken was a significant risk factor in male patients. Our results showed that polypharmacy itself could be defined as an independent risk factor for falls. Nevertheless, the benefit-to-risk ratio of fall-risk drugs also should be taken into account for safe prescribing. Drug-related problems can be reduced by means of the potentially inappropriate medication lists; however, these theoretical criteria need to be confirmed by real-life epidemiological data. Our methods and results could serve as a strong base for further research in this field, as well as they can attract health care professionals’ attention to the most vulnerable populations of elderly patients in terms of falls.
References
Centers for Disease Control and Prevention Falls in Nursing Homes. Updated 2015 June 30. http://www.cdc.gov/HomeandRecreationalSafety/Falls/nursing.html. Accessed 2 Feb 2016.
World Health Organization Global Report on Falls Prevention in Older Age. 2007. http://www.who.int/ageing/projects/falls_prevention_older_age/en/. Accessed 22 Jan 2016.
Ambrose AF, Cruz L, Paul G. Falls and fractures: a systematic approach to screening and prevention. Maturitas. 2015;82:85–93.
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8:136.
Cawthon PM. Gender differences in osteoporosis and fractures. Clin Orthop Relat Res. 2011;469:1900–5.
Bor A, Matuz M, Gyimesi N, Biczok Z, Soos G, Doro P. Gender inequalities in the treatment of osteoporosis. Maturitas. 2015;80:162–9.
Freeland KN, Thompson AN, Zhao Y, Leal JE, Mauldin PD, Moran WP. Medication use and associated risk of falling in a geriatric outpatient population. Ann Pharmacother. 2012;46:1188–92.
Wu TY, Chie WC, Yang RS, Liu JP, Kuo KL, Wong WK, et al. Factors associated with falls among community-dwelling older people in Taiwan. Ann Acad Med Singap. 2013;42:320–7.
Weber V, White A, McIlvried R. An electronic medical record (EMR)-based intervention to reduce polypharmacy and falls in an ambulatory rural elderly population. J Gen Intern Med. 2008;23:399–404.
Willeboordse F, Grundeken LH, van den Eijkel LP, Schellevis FG, Elders PJ, Hugtenburg JG. Information on actual medication use and drug-related problems in older patients: questionnaire or interview? Int J Clin Pharm. 2016;38:380–7.
Chau SH, Jansen AP, van de Ven PM, Hoogland P, Elders PJ, Hugtenburg JG. Clinical medication reviews in elderly patients with polypharmacy: a cross-sectional study on drug-related problems in the Netherlands. Int J Clin Pharm. 2016;38:46–53.
Ziere G, Dieleman JP, Hofman A, Pols HA, van der Cammen TJ, Stricker BH. Polypharmacy and falls in the middle age and elderly population. Br J Clin Pharmacol. 2006;61:218–23.
Zia A, Kamaruzzaman SB, Tan MP. Polypharmacy and falls in older people: balancing evidence-based medicine against falls risk. Postgrad Med. 2015;127:330–7.
Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5:345–51.
Fialova D, Topinkova E, Gambassi G, Finne-Soveri H, Jonsson PV, Carpenter I, et al. Potentially inappropriate medication use among elderly home care patients in Europe. JAMA. 2005;293:1348–58.
Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine. Arch Intern Med. 1991;151:1825–32.
American Geriatrics Society. Updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;2015(63):2227–46.
Mercaldo ND, Lau KF, Zhou XH. Confidence intervals for predictive values with an emphasis to case-control studies. Stat Med. 2007;26:2170–83.
Altman DG, Bland JM. Diagnostic tests 2: predictive values. BMJ. 1994;309:102.
Agresti A. Categorical Data Analysis. 2nd ed. New York: Wiley; 2002.
Agresti A, Caffo B. Simple and effective confidence intervals for proportions and difference of proportions result from adding two successes and two failures. Am Stat. 2000;54:280–8.
Laroche ML, Charmes JP, Merle L. Potentially inappropriate medications in the elderly: a French consensus panel list. Eur J Clin Pharmacol. 2007;63:725–31.
Holt S, Schmiedl S, Thurmann PA. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int. 2010;107:543–51.
Mann E, Bohmdorfer B, Fruhwald T, Roller-Wirnsberger RE, Dovjak P, Duckelmann-Hofer C, et al. Potentially inappropriate medication in geriatric patients: the Austrian consensus panel list. Wien Klin Wochenschr. 2012;124:160–9.
Bjerrum L, Rosholm JU, Hallas J, Kragstrup J. Methods for estimating the occurrence of polypharmacy by means of a prescription database. Eur J Clin Pharmacol. 1997;53:7–11.
Rubenstein LZ. Preventing falls in the nursing home. JAMA. 1997;278:595–6.
Stevens JA. Falls among older adults-risk factors and prevention strategies. J Safety Res. 2005;36:409–11.
Centers for Disease Control and Prevention (CDC). Fatalities and injuries from falls among older adults–United States, 1993–2003 and 2001–2005. MMWR Morb Mortal Wkly Rep. 2006;55:1221–1224.
Laurent M, Gielen E, Claessens F, Boonen S, Vanderschueren D. Osteoporosis in older men: recent advances in pathophysiology and treatment. Best Pract Res Clin Endocrinol Metab. 2013;27:527–39.
Gielen E, Vanderschueren D, Callewaert F, Boonen S. Osteoporosis in men. Best Pract Res Clin Endocrinol Metab. 2011;25:321–35.
Fonad E, Wahlin TB, Winblad B, Emami A, Sandmark H. Falls and fall risk among nursing home residents. J Clin Nurs. 2008;17:126–34.
Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–41.
Russell M, Clapperton A, Vu T, Day L. Trends in fall-related hospitalisations in older people living in aged care facilities. Osteoporos Int. 2015;26:1219–24.
Pantoprazole Summary of Product Characteristics. https://www.medicines.org.uk/emc/medicine/2518. Accessed 23 Feb 2016.
Ozdil K, Kahraman R, Sahin A, Calhan T, Gozden EH, Akyuz U, et al. Bone density in proton pump inhibitors users: a prospective study. Rheumatol Int. 2013;33:2255–60.
Vinpocetine Summary of Product Characteristics. https://www.ogyei.gov.hu/gyogyszeradatbazis/index.php?action=show_details&item=16779. Accessed 24 Feb 2016.
Trimetazidine Summary of Product Characteristics. https://www.ogyei.gov.hu/gyogyszeradatbazis/index.php?action=show_details&item=27756. Accessed 24 Feb 2016.
European Medicines Agency Recommendation on restricted use of trime-tazidine-containing medicines. 2012. http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2012/06/news_detail_001541.jsp&mid=WC0b01ac058004d5c1. Accessed 24 Feb 2016.
Bor A, Matuz M, Doro P, Viola R, Soos G. Drug-related problems in the elderly. Orv Hetil. 2012;153:1926–36.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bor, A., Matuz, M., Csatordai, M. et al. Medication use and risk of falls among nursing home residents: a retrospective cohort study. Int J Clin Pharm 39, 408–415 (2017). https://doi.org/10.1007/s11096-017-0426-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-017-0426-6