Abstract
Background Voriconazole is an antifungal drug essentially metabolized by cytochrome P450 (CYP2C19) isozyme. Plasma voriconazole levels exhibit wide inter-individual variability due to several factors like age, weight, food or drug interactions or CYP2C19 polymorphisms. Objective In the present study, we assessed the correlation of voriconazole levels with CYP2C19 genotype in patients on voriconazole therapy. Setting Biochemistry Department of a 480 inpatient bed tertiary care hospital in India. Methods Plasma voriconazole estimation was done in seventy-two patients on standard weight based voriconazole therapy by High Performance Liquid Chromatography (HPLC) while genotype assessment for the CYP2C19*2 and *3 was done by PCR–RFLP and *17 by ARMS-PCR. Statistical analysis and genotype-phenotype correlation was done by comparing the drug levels with the CYP2C19 genotype. Main outcome measure CYP2C19 polymorphisms influence voriconazole metabolism. Results A wide variability is seen in plasma levels with only 51 % attaining therapeutic levels. The allele frequency of *2, *3 and *17 variant were found to be 33.3, 0.7 and 18 % respectively. The drug levels in carriers of *2 allele (poor metabolizers) was twofold higher than that in extensive metabolizers. However, the influence of *2 allele was compromised in presence of *17 allele and patients had low voriconazole levels. In addition to the genotype, co-medication and clinical condition remarkably influenced voriconazole concentration. Conclusion Plasma voriconazole levels are influenced by CYP2C19 variants, drug interactions and clinical condition of the patient. Genotype assessment at initiation of therapy followed by drug monitoring would help optimizing therapeutic efficacy and minimizing toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practise
-
CYP2C19 genotype analysis and voriconazole monitoring at initiation of therapy followed by voriconazole level estimation at regular intervals is required to achieve therapeutic targets.
-
Indians show a high prevalence of CYP2C19*2 genotype unlike Caucasians, hence may warrant reassessment of voriconazole dose.
-
Inter-individual variability in voriconazole metabolism across different CYP2C19 genotypes is widely seen amongst Indians.
Introduction
Voriconazole (Vrc), a second-generation triazole with broad-spectrum antifungal activity has an enhanced potency against Aspergillus, Candida, Scedosporium apiospermum and Fusarium species [1, 2]. It is metabolized by hepatic cytochrome P450 (CYP) primarily by CYP2C19 isoenzyme while CYP2C9 and CYP3A4 contribute to a minor extent [3, 4]. Pharmacokinetic variability with a narrow therapeutic index and large inter- and intra-individual variability in plasma voriconazole concentrations regardless of the route of administration have been well documented [3–10]. Factors associated with this variability include liver dysfunction, gastrointestinal abnormalities (e.g., mucositis or diarrhea), past alcohol abuse, concomitant use of potent CYP450 inducers or inhibitors, CYP2C19 genetic polymorphism and intake with or without food; thus rationalizing the necessity for therapeutic drug monitoring (TDM) of voriconazole. [7, 11, 12]. Genetic polymorphism of CYP2C19 account for 30 % of the variability while 70 % may be due to other above mentioned factors [8, 13, 14]. Table 1 mentions the influence of CYP2C19 variants on voriconazole metabolism wherein *2 & *3 are poor metabolizers while *17 are ultra-rapid metabolizers [4, 14]. A high frequency of poor metabolizers (especially *2) has been reported amongst Indians (35 %) as compared to Caucasians (5–10 %) [15] while the frequency of ultra-rapid metabolizers *17 is in keeping with the Caucasian i.e. (15–20 %) [16].
Aim of the study
To describe and assess the effect of CYP2C19 genotype on plasma voriconazole levels amongst Indians.
Ethical approval
The retrospective data analysis of plasma voriconazole levels and CYP2C19 genotyping for all samples referred to the laboratory was approved by the Institutional Review Board. All patients in the study were on a standard weight based voriconazole dose. A pre-determined proforma was filled to obtain clinical details and consent for genotype analysis at the time of sample collection.
Methods
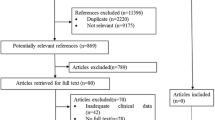
The laboratory offers TDM of Vrc and CYP2C19 genotype analysis as a routine clinical service for referrals from both in-patients and other centres. Due to the high prevalence of CYP2C19 variants in Idia, and the paucity of published data on effect of CYP2C19 genotype on plasma voriconazole levels amongst Indians, the present retrospective study was undertaken.
Clinical characteristics of patients
Voriconazole drug analysis was performed in 72 patients (44 males and 28 females) either suffering from invasive fungal infections or were on empirical treatment for at least 4 days.
Sample collection and processing
Plasma separated from EDTA blood was used for drug analysis while the buffy coat containing leukocytes was used for DNA isolation and CYP2C19 genotyping. Voriconazole level was estimated using a commercially available HPLC kit from CHROMSYSTEMS (Catalogue no. 27037, Chromsystems GmbH, Munich, Germany). A Waters 1525 multisolvent delivery system pump with Waters 2475 fluorescence detector was used for estimation. Based on guidelines for method validation, analytical sensitivity of the method was verified to have a limit of quantification of 0.2 mg/L (0.57 µmol/L) with a linearity of 0.2–20 mg/L (0.57–57.2 µmol/L) [17].
Literature suggests variable therapeutic range primarily spanning between 1.5 and 6 mg/L [9, 10, 18]. In our laboratory a trough level between 2 and 6 mg/L (5.72–17.16 µmol/L) was considered optimal for both treatment and prophylaxis [19, 20].
CYP2C19 genotyping
DNA was extracted using salting out method [21]. Genotyping for CYP2C19*2 and CYP2C19*3 alleles was done using polymerase chain reaction (PCR)—restriction fragment length polymorphism (RFLP) [22] while CYP2C19*17 alleles were analyzed using amplification refractory mutation system (ARMS–PCR) [16]. Restriction enzymes SmaI and BamHI are used for CYP2C19*2 and CYP2C19*3 genotyping respectively. The wild type, homozygous and heterozygous genotypes of each allele was confirmed by Sanger sequencing (Fig. 1). The characteristic of each genotype was determined as mentioned in Table 1. The PCR was carried out as per reported protocols by Ghodke et al. [22] and Anichavezhi et al. [16] with slight modifications. The amplified PCR products were analyzed on 3 % agarose gel (Fig. 1).
Representative gel picture and chromatogram showing CYP2C19 genotypes. 1a, 1b Agarose gel (3 %) showing CYP2C19*2 and *3 genotypes (Lane 1-Wild type, Lane 2-Heterozygous and Lane 3-Homozygous mutant), 1c Agarose gel (3 %) showing CYP2C19*17 genotypes (Lane 1A/1B-Wild type, Lane 2A/2B- Heterozygous and Lane 3A/3B- Homozygous mutant). 2a–2c DNA chromatogram for CYP2C19*2, *3 and *17 respectively. (Sequencing for CYP2C19*3 variation with reverse primer). M 50 base pair marker, NC negative control, UD undigested control, bp base pair
Statistical analysis
The demographic details and voriconazole levels are expressed as median (range). Statistical analysis using Mann–Whitney test and multivariate regression analysis was carried out for the confounding factors like age, gender, weight, dose and duration of therapy with Vrc levels. The entire statistical analysis was performed using Medcalc version 13.0.4.0 (MedCalc Software, Acacialaan, Ostend, Belgium) and a p value of <0.05 was considered to be statistically significant.
Results
Clinical condition and patient characteristics
Amongst the study group, patients were suffering from co-conditions like cancer (n = 12, 22 %), solid-organ transplant (n = 10, 18 %), post-operative infections (n = 4, 7 %) and others including tuberculosis, nasal or oral infections, alcoholic liver disease, diabetes, granulomatosis etc. (n = 15, 27 %) while 14 suffered only from IFI. These patients were on therapy either for prophylaxis (n = 9) or for therapy of proven or probable infections.
Voriconazole drug level in patients
Out of the 72 patients, 17 patients were excluded from data analysis as Vrc levels were performed at random time points. The remaining study population wherein trough levels were collected (n = 55) was divided according to the Vrc levels in the sub-therapeutic, therapeutic or toxic drug level. The demographic details and plasma levels of these patients are shown in Table 2. It is evident from the table that inspite of all patients achieving their steady state concentrations, only 28 patients (51 %) attained a therapeutic level while 20 patients (37 %) remained in sub therapeutic range and 7 patients (13 %) showed toxicity within the first month of therapy. One patient remained in the sub-therapeutic range even after 455 days of therapy.
Multivariate regression analysis of plasma voriconazole level was significant only for dose (p < 0.004) while other factors like age (p = 0.84), gender (p = 0.77), weight (p = 0.25) and duration of therapy (p = 0.95) were statistically insignificant.
CYP2C19 genotype
Genotype analysis was performed in all patients with conventional PCR methods. The representative gel pictures and the chromatograms are shown in Fig. 1. CYP2C19*1 was most common allele with a frequency of 51 % followed by *2 (30 %) and *17 (18.1 %) alleles while *3 (0.9 %) allele was found in heterozygous condition only in 1 patient. The observed frequencies of the CYP2C19 genotypes are shown in Table 3.
Trough Vrc level in different genotypes
A substantial influence of CYP2C19 allelic variants on plasma voriconazole levels is noted across all genotypes observed in the study group. Majority of patients with the *1/*1 genotype i.e. extensive metabolizers were in the therapeutic range. In presence of *2 allele, a poor metabolizer, the median Vrc levels increased by 1.3 times in wild type heterozygous (n = 17) and 1.9 times in homozygous (n = 4) conditions. In case of *17 allele, an ultra-rapid metabolizer, comparatively low drug levels were seen in heterozygous condition with *2 (n = 8) and *1 (n = 10). The influence of genotype on Vrc levels is mentioned in Fig. 2a. The homozygous mutant of *17, despite suggestive of an Ultra-rapid metabolizer had Vrc levels in therapeutic range. Poor metabolizer *3 allele was present in heterozygous condition only in one patient. The patient had attained toxic trough level of 33.4 mg/L.
Trough voriconazole level and CYP2C19 genotype. a All patients (n = 53) and b Standard Dose i.e. 400 mg/day (n = 37). The graph represents the trend of median voriconazole levels across the different genotypes observed. The error bars represent the inter-quartile range. The genotypes *1/*3 and *17/*17 are not included in the above figure as only one patient was seen in each case
Since Vrc dose significantly influenced (p < 0.004) Vrc levels, the genotype-phenotype influence was also assessed in patients receiving standard Vrc dose i.e. 400 mg/day. In our study, 37 patients received 400 mg/day. Vrc levels in these patients also showed a similar genotypic influence (Fig. 2b), however, a statistical significant difference (p = 0.01) was seen in only *2/*2 genotype while others *1/*2 (p = 0.23), *2/*17 (p = 0.57) and *1/*17 (p = 0.97) were statistically insignificant.
Discussion
Voriconazole is an ideal candidate for TDM due to its wide inter- and intra-individual variability and drug–drug interaction. Drug monitoring reflects the attained therapeutic efficacy or adverse effects, if any, observed and may warrant the need for necessary dose adjustments. The human cytochrome P450 (CYP450) enzymes i.e. CYP2C9, CYP2C19 and CYP3A4 metabolising various drugs are highly polymorphic and exhibit varied phenotypes depending on the variant [14]. In this study plasma voriconazole levels are correlated with CYP2C19 genotype.
The inter-individual and inter-ethnic variability in the pharmacokinetics of voriconazole due to the genetic polymorphisms of the CYP2C19 enzyme has been widely reported [14, 23, 24]. CYP2C19*1 represents the wild-type allele i.e. extensive metabolizers. In poor metabolizers, *2 and *3 alleles result in a truncated protein and an inactive enzyme reducing the clearance of voriconazole [14, 22]. The variation −806C > T in the promoter region (CYP2C19*17) causes an increase in gene transcription and enzyme activity resulting in an ultra-rapid metabolism of voriconazole [25, 26]. The allele frequency of 30, 18.1 and 0.9 % obtained for *2, *17 and *3 allele respectively in our study are in concurrence with those reported from other parts of India in the Clinical Pharmacogenetics Implementation Consortium (CPIC) [16, 27].
Plasma voriconazole levels observed in our study group reflect a wide inter-individual variability and warrant the need for TDM. Our patients *1/*2 and *2/*2 had median Vrc levels about 1.3 and 1.9 times higher as compared to extensive metabolizers respectively (Fig. 2). A similar influence of *2 allele has been reported wherein the poor metabolizer had threefold–fourfold higher voriconazole level as compared to extensive metabolizer [3, 7, 12]. The direct influence of *2 variant is however compromised in presence of *17 allele. In such intermediate metabolizers i.e. *2/*17 individuals, the *17 allele has been reported to mask the effect of *2 allele with an increased metabolic rate of the enzyme [16]. However, due to lack of evidence of intermediate metabolizers in Caucasians & scarce literature available amongst Asians, the definite role of this genotype is left unexplained. The *17/*17 genotype though suggestive of ultra-rapid metabolism unexpectedly showed Vrc level in therapeutic range in the only single patient seen in our study group. CYP2C19*3 (poor metabolizer) was uncommon and seen in heterozygous condition in 1 patient only wherein a toxic Vrc level of 33.4 mg/L was obtained. The literature reports of this variant’s influence on voriconazole metabolism are scarce however its effect on clopidogrel metabolism is well documented [28].
Other influencing factors like clinical conditions, food or drug interactions have also been reported to influence plasma levels [11–13]. In our study group, these influencing factors were seen individually in very few patients (n = 5) and hence no definite correlation could be established.
In conclusion, we report a statistically significant correlation of voriconazole level and CYP2C19 genotype. The *2 allele has a profound effect on the drug level while the immediate influence of other genotypes cannot be elucidated due to small sample size. A high prevalence of poor metabolizer amongst Indians and genotype-phenotype correlation seen in our study suggests that Vrc monitoring and genotype analysis may assist in clinical practice and better patient care.
References
VFEND® I.V. (voriconazole) for injection, VFEND® tablets (voriconazole), VFEND® (voriconazole) for oral suspension [US physician prescribing information] New York (NY) Roerig Division of Pfizer Inc; revised 2008 Mar [cited 2008 Sep 3]. http://media.pfizer.com/files/products/uspi_vfend.pdf. Last Accessed 5 Dec 2013.
Briefing document for voriconazole (oral and intravenous formulations). Prepared for submission to US Food and Drug Administration, Food and Drugs Advisory Committee. Pfizer; 2001 Oct 4 [cited 2008 Sep 3]. http://www.fda.gov/ohrms/dockets/ac/01/briefing/3792b2_01_Pfizer.pdf. Last Accessed 20 Jan 2014.
Scholz I, Oberwittler H, Riedel K, et al. Pharmacokinetics, metabolism and bioavailability of the triazole antifungal agent voriconazole in relation to CYP2C19 genotype. Br J Clin Pharmacol. 2009;68(6):906–15. doi:10.1111/j.1365-2125.2009.03534.x.
Li-Wan-Po A, Girard T, Farndon P, Cooley C, Lithgow J. Pharmacogenetics of CYP2C19: functional and clinical implications of a new variant CYP2C19*17. Br J Clin Pharmacol. 2010;69(3):222–30. doi:10.1111/j.1365-2125.2009.03578.x.
Hussaini T, Ruping M, Farowski F, Vehreschild J, Cornely O. Therapeutic drug monitoring of voriconazole and posaconazole. Pharmacotherapy. 2011;31(2):214–25. doi:10.1592/phco.31.2.214.
Pasqualotto A, Xavier M, Andreolla H, Linden R. Voriconazole therapeutic drug monitoring: focus on safety. Expert Opin Drug Saf. 2010;9(1):125–37. doi:10.1517/14740330903485637.
Han K, Bies R, Johnson H, Capitano B, Venkataramanan R. Population pharmacokinetic evaluation with external validation and bayesian estimator of voriconazole in liver transplant recipients. Clin Pharm. 2011;50(3):201–14. doi:10.2165/11538690-000000000-00000.
Leveque D, Nivoix Y, Jehl F, Herbrecht R. Clinical pharmacokinetics of voriconazole. Int J Antimicrob Agents. 2006;27(4):274–84. doi:10.1016/j.ijantimicag.2006.01.003.
Perea S, Pennick G, Modak A, et al. Comparison of high-performance liquid chromatographic and microbiological methods for determination of voriconazole levels in plasma. Antimicrob Agents Chemother. 2000;44(5):1209–13. doi:10.1128/aac.44.5.1209-1213.2000.
Pascual A, Calandra T, Bolay S, Buclin T, Bille J, Marchetti O. Voriconazole therapeutic drug monitoring in patients with invasive mycoses improves efficacy and safety outcomes. Clin Infect Dis. 2008;46(2):201–11. doi:10.1086/524669.
Koselke E, Kraft S, Smith J, Nagel J. Evaluation of the effect of obesity on voriconazole serum concentrations. J Antimicrob Chemother. 2012;67(12):2957–62. doi:10.1093/jac/dks312.
Sandherr M, Maschmeyer G. Pharmacology and metabolism of voriconazole and posaconazole in the treatment of invasive aspergillosis-review of the literature. Eur J Med Res. 2011;16(4):139. doi:10.1186/2047-783x-16-4-139.
Johnson L, Kauffman C. Voriconazole: a new triazole antifungal agent. Clin Infect Dis. 2003;36(5):630–7. doi:10.1086/367933.
Weiss J, ten Hoevel M, Burhenne J, et al. CYP2C19 genotype is a major factor contributing to the highly variable pharmacokinetics of voriconazole. J Clin Pharmacol. 2009;49(2):196–204. doi:10.1177/0091270008327537.
Scott S, Sangkuhl K, Stein C, et al. Clinical pharmacogenetics implementation consortium guidelines for CYP2C19 genotype and clopidogrel therapy: 2013 update. Clin Pharmacol Ther. 2013;94(3):317–23. doi:10.1038/clpt.2013.105.
Anichavezhi D, Chakradhara Rao U, Shewade D, Krishnamoorthy R, Adithan C. Distribution of CYP2C19*17 allele and genotypes in an Indian population. J Clin Pharm Ther. 2011;37(3):313–8. doi:10.1111/j.1365-2710.2011.01294.x.
Guidance for the Industry: Bioanalytical Method Validation. Washington, DC: US Department of health and Human Services, FDA, CDER and CVM; 2001 BP.
Husain S, Paterson D, Studer S, et al. Voriconazole prophylaxis in lung transplant recipients. Am J Transpl. 2006;6(12):3008–16. doi:10.1111/j.1600-6143.2006.01548.x.
Trifilio S, Pennick G, Pi J, et al. Monitoring plasma voriconazole levels may be necessary to avoid subtherapeutic levels in hematopoietic stem cell transplant recipients. Cancer. 2007;109(8):1532–5. doi:10.1002/cncr.22568.
Neely M, Rushing T, Kovacs A, Jelliffe R, Hoffman J. Voriconazole pharmacokinetics and pharmacodynamics in children. Clin Infect Dis. 2010;50(1):27–36. doi:10.1086/648679.
Miller S, Dykes D, Polesky H. A simple salting out procedure for extracting DNA from human nucleated cells. Nucl Acids Res. 1988;16(3):1215. doi:10.1093/nar/16.3.1215.
Ghodke Y, Joshi K, Arya Y, et al. Genetic polymorphism of CYP2C19 in Maharashtrian population. Eur J Epidemiol. 2007;22(12):907–15. doi:10.1007/s10654-007-9196-0.
Berge M, Guillemain R, Trégouet D, et al. Effect of cytochrome P450 2C19 genotype on voriconazole exposure in cystic fibrosis lung transplant patients. Eur J Clin Pharmacol. 2010;67(3):253–60. doi:10.1007/s00228-010-0914-2.
Matsumoto K, Ikawa K, Abematsu K, et al. Correlation between voriconazole trough plasma concentration and hepatotoxicity in patients with different CYP2C19 genotypes. Int J Antimicrob Agents. 2009;34(1):91–4. doi:10.1016/j.ijantimicag.2009.01.008.
Dolton M, McLachlan A. Clinical importance of the CYP2C19*17 variant allele for voriconazole. Br J Clin Pharmacol. 2010;71(1):137–8. doi:10.1111/j.1365-2125.2010.03801.x.
Wang G, Lei H, Li Z, et al. The CYP2C19 ultra-rapid metabolizer genotype influences the pharmacokinetics of voriconazole in healthy male volunteers. Eur J Clin Pharmacol. 2008;65(3):281–5. doi:10.1007/s00228-008-0574-7.
Jose R, Chandrasekaran A, Sam S, et al. CYP2C9 and CYP2C19 genetic polymorphisms: frequencies in the south Indian population. Fundam Clin Pharmacol. 2005;19(1):101–5. doi:10.1111/j.1472-8206.2004.00307.x.
Jeong Y, Tantry U, Kim I et al. Effect of CYP2C19*2 and *3 loss-of-function alleles on platelet reactivity and adverse clinical events in East Asian acute myocardial infarction survivors treated with clopidogrel and aspirin. Circ Cardiovasc Interv. 2011;4(6):585–94. doi:10.1161/circinterventions.111.962555.
Acknowledgments
We acknowledge National Health and Education Society (NHES) of P. D. Hinduja Hospital and Medical Research Centre for all their help.
Funding
No specific funding was obtained for the study.
Conflicts of interest
All authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chawla, P.K., Nanday, S.R., Dherai, A.J. et al. Correlation of CYP2C19 genotype with plasma voriconazole levels: a preliminary retrospective study in Indians. Int J Clin Pharm 37, 925–930 (2015). https://doi.org/10.1007/s11096-015-0143-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-015-0143-y