Abstract
Background Recommendations on drug dose adjustment in patients with renal impairment may vary between the references. It is often unknown which approach the dosing schemes were based on and what drug exposure is likely to be achieved. Objective To develop a simple method to evaluate recommended dosing schemes for patients with renal impairment, to apply this method to selected antibacterial drugs in order to evaluate expected drug concentrations using dosing schemes recommended for patients with severe infections, and to evaluate the expected consequences. Setting This was a theoretical study, which was based on data from published clinical trials. Methods Clinically established dosing schemes for 46 antibacterial drugs, as recommended for patients with renal impairment in the Summary of Product Characteristics, were analysed using a newly developed graphical method. Consistency of the dosing schemes with two general dose adjustment rules, the proportional rule and the eliminated fraction rule, was determined and drug exposure was predicted. Main outcome measure Predicted drug exposure. Consistency of recommended dosing schemes with the general dose adjustment rules. Results Only 30 % of the recommended dosing schemes were associated with similar average concentrations as expected in patients with normal renal function (44 % were associated with higher and 26 % with lower concentrations). The highest median exposure was found in beta-lactams (170 %, range 58–443 %, for creatinine clearance of <15 ml/min, and 155 %, range 54–232 %, for creatinine clearance of 15 to <30 ml/min), where the medians were significantly different from 100 % (P < 0.02). Consistency with a dosing rule was found in 59 % of the dosing schemes (proportional rule 46 %, eliminated fraction rule 50 %, both rules 4 %). Conclusions Relative low exposure was found for several drugs, including ceftazidime, cefotaxime, imipenem, erythromycin, ciprofloxacin, levofloxacin, and teicoplanin, where dosing schemes should be reconsidered or used only in clinical situations where a lower than maximum exposure appears adequate. General application of the proportional rule for calculating drug dose adjustments would lead to lower than clinically established dose practice for 44 % of drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impact of findings on practice
-
Recommended dosing schemes for patients with renal impairment can be evaluated and compared by using a graphical method based on published pharmacokinetic data.
-
Dosing schemes for renal impairment recommended in the summary of product characteristics for ceftazidime, cefotaxime, imipenem, erythromycin, ciprofloxacin, levofloxacin, and teicoplanin should be reconsidered or used only in clinical situations where a lower than maximum exposure appears adequate.
-
The proportional rule for calculating drug dose adjustments is leading to lower than clinically established dosing schemes for many antibacterials.
Introduction
Drug dose adjustment in patients with renal impairment is advisable for many drugs in order to avoid excessively high concentrations and toxicity. However, drug dose adjustment should not lead to low concentrations and reduced effectiveness. Unfortunately, there is no general algorithm on how to adjust drug doses and/or dosing intervals. Actual recommendations are usually based on calculations (considering pharmacokinetics and pharmacodynamics of a drug) and expert consensus, but the experience from clinical studies is limited [1].
The most general approach to drug dose adjustment is to reduce the dose or to prolong the dosing interval in proportion to the reduced elimination capacity of a patient (proportional rule of Dettli), leading to approximately normal average drug concentrations (or area under the curve) as compared to patients with normal renal function [2, 3]. This approach is commonly used, but could be inadequate, e.g. for drugs with “concentration-dependent” action, because peak concentrations will be lower (when reducing the dose) or appear much less often (when the prolonging the dosing interval) than normal [4].
Another general approach to drug dose adjustment is to replace the amount of drug that has been eliminated within a dosing interval (eliminated fraction rule), leading to approximately normal peak concentrations that may occur more often compared to the proportional rule [3, 5]. This approach was first applied by Kunin and is recommended for severely ill patients, but could be inadequate for drugs with a close association between average drug concentrations (or area under the curve) and toxicity, because average drug concentrations may be higher than normal [4].
Specific recommendations on drug dose adjustment are available from various sources, such as the summary of product characteristics (SmPC), which provides recommendations from the pharmaceutical manufacturer as approved by the competent authorities. Other sources are published studies from the scientific literature and reference books. However, recommendations may considerably vary between the sources [6], and it is often unknown which approach the proposed dosing schemes, as calculated or used in clinical studies, were based on and what drug exposure is likely to be achieved.
Unfortunately, there is no simple method to evaluate dosing schemes recommended for patients with renal impairment. Such a method could be useful to compare specific recommendations, to identify dosing schemes which might be at risk for over- or underdosing and to select a dosing scheme where various recommendations are available. Furthermore, classification of practically used dosing schemes as being consistent with one of the general dose adjustment rules would facilitate implementation in electronic clinical decision support systems, where drug dose recommendations may be calculated on a continuous scale.
Aims of the Study
The aims of the present study were (1) to develop a simple method to evaluate dosing schemes recommended for patients with renal impairment, (2) to apply this method to selected antibacterial drugs in order to evaluate expected drug concentrations using dosing schemes recommended in the SmPC for patients with severe infections, and (3) to evaluate the expected consequences of sole application of the proportional rule for calculating drug dose adjustments.
Ethical approval
Approval by an ethics committee and written informed consent were not required for this theoretical study, which was based on data from published clinical trials.
Methods
A list of antibacterial drugs was compiled based on the “WHO Model List of Essential Medicines” [7], and the antibacterial drugs commonly used in the University Hospital Ulm when this analysis was started. Dose adjustment recommendations for patients with renal impairment were independently extracted from German SmPCs (“Fachinformation”) by two medical experts (MS, DC). Any discrepancies in interpretation were solved by discussion. In case of more than one applicable dosing recommendation, a dosing scheme for intravenous administration and for severe infections was selected. In some cases, more than one recommendation was selected for further analysis, e.g. if more than one dosing scheme was specified by a pharmaceutical manufacturer or different schemes were specified by different manufacturers of the same drug. Dosing schemes for creatinine clearance levels of <5 ml/min were ignored, because patients with such creatinine clearance levels need renal replacement therapy.
Pharmacokinetic parameters were extracted from our pharmacokinetic database PKnephro (please see supplemental appendix for details), as used before [8, 9]. For calculations we used the reported pharmacokinetic parameter values as measured in patients with renal failure (RF), wherever possible. The primary parameters were systemic drug clearance (CL), apparent systemic drug clearance after oral administration (CL/F) and half-life (t1/2). Missing parameter values were predicted by using renal clearance (CLren), urinary recovery of unchanged drug after intravenous administration (fu,iv), and systemically available fraction (F), where applicable (Table S1) [8–10].
Pharmacokinetic parameter values for a given creatinine clearance were calculated by linear interpolation between the population extremes (normal vs. renal failure) using Eqs. 1 and 2 for drug clearance and elimination rate constant (k = ln(2)/t1/2).
Creatinine clearance (CLcrea) was the renal function of interest, whereas CLcrea,norm and CLcrea,RF were the average of the creatinine-clearance values in normal renal function and in renal failure as recorded in the PKnephro database. Subtracting CLcrea,RF in Eqs. 1 and 2 implies some degree of extrapolation for very low creatinine clearance values, when patients with renal failure in the original studies had residual renal function.
Theoretical dose adjustment schemes were calculated using the proportional rule (Eq. 3), as used by Dettli [3], and a general form of the eliminated fraction rule (Eq. 4), where D is the maintenance dose and τ the dosing interval.
Loading doses, which are commonly used when a rapid achievement of steady-state concentrations is desired, were not analysed in the present study. The first term in Eq. 4 can be used to calculate a loading dose and was used here as a starting point for dose calculations. The second term in Eq. 4 estimates the amount of drug that is eliminated within a dosing interval.
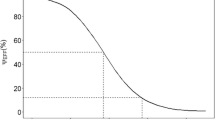
A new graphical method to compare recommended dosing schemes was developed, where the dosing interval and the maintenance dose were related to the x-axis and y-axis, respectively. Recommended dosing schemes were indicated by a circle, whereas calculated dose adjustment schemes were plotted as a line, because both general rules lead to a continuum of possible dosing schemes for a given creatinine clearance (Fig. 1).
Dosing schemes for normal renal function (large circle) and impaired renal function (small circle) as recommended in the SmPC. The broken lines indicate dosing schemes calculated with the proportional rule, leading to normal average concentrations (or area under the curve). The continuous lines indicate dosing schemes calculated with the eliminated fraction rule, leading to normal peak concentrations. The thin grey lines indicate the respective 80–125 % range. For amoxicillin, the recommended dosing scheme is less and in agreement with the proportional rule, whereas for ampicillin, the recommended dosing scheme is higher and in agreement with the eliminated fraction rule. The differences in creatinine clearance between amoxicillin and ampicillin reflect differences in creatinine clearance ranges as used in the SmPC
In order to analyse average concentrations (or area under the curve) in patients with renal impairment, SmPC-recommended total-daily doses were expressed as percentage of the total-daily dose as calculated with the proportional rule.
Statistics
All analyses were done in an explorative and descriptive manner. SmPC-derived dose recommendations for creatinine clearance of <15 ml/min and 15 to <30 ml/min, where available, were compared to the rule-based dosing schemes. When the SmPC-derived dosing recommendation referred to a creatinine clearance range, an average creatinine clearance was used for calculations in order to capture the general trend (e.g. a creatinine clearance of 9.5 ml/min was used for a dosing scheme proposed for patients with a creatinine clearance of 5–14 ml/min). Consistency of a dosing recommendation with a general rule was assumed when the recommended dose was in the calculated 80–125 % range, in analogy to the commonly applied bioequivalence range, as also used in the guidelines of the European Medicines Agency (CPMP/EWP/QWP/1401/98).
A Wilcoxon signed-rank test for comparison of column medians to a hypothetical value was used to analyse whether the SmPC-recommended total-daily doses (as percentage of calculated total-daily doses using the proportional rule) were significantly different from 100 %, which was concluded at P < 0.05.
Software
Calculations were done with Microsoft® Excel 2010 (Microsoft Corporation, Redmond, WA, USA). In order to detect potential transcription errors in the extracted dosing schemes or pharmacokinetic parameters, predicted concentration–time curves were calculated for various degrees of renal function, based on a one-compartment model, and the resulting plots visually checked for plausibility.
Statistical analysis was done with GraphPad Prism Version 5.01 (GraphPad Software, San Diego, CA, USA).
Results
Recommendations for drug dose adjustment in patients with renal impairment were extracted from SmPCs for 46 drugs (Table S2). Overall, “no adjustment” was recommended for 8 of these drugs (17 %). In addition, a recommendation of “do not use” was given for 3 drugs.
Recommended dosing schemes were evaluated for consistency with the general dosing rules using our graphical method (example in Fig. 1). Overall, 88 dosing schemes were available, counting trimethoprim and sulfamethoxazole separately, and 52 of them (59 %) could be attributed to one of the general dosing rules (Table 1).
From 40 dosing recommendations for creatinine clearance values below 15 ml/min, 8 were consistent with the proportional rule and 11 with the eliminated fraction rule. In case of penicillins and cephalosporins, however, only 2 of the proposed dosing schemes were consistent with the proportional rule and 10 were consistent with the eliminated fraction rule, indicating higher than normal average concentrations. From those dosing schemes which could not be related to a dosing rule, 7 lay in between the dosing lines, 10 had lower and 4 had higher doses as calculated by both rules (Table 1).
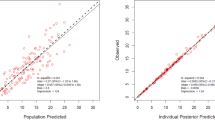
When comparing SmPC-recommended total-daily doses to calculated total-daily doses using the proportional rule, a median expected exposure of 139 % with a large range from 20 to 549 % was found, where the median exposure was significantly different from 100 % (P < 0.01). Only 8 (20 %) were within the 80–125 % range, whereas 10 (25 %) were lower and 22 (55 %) were higher (Fig. 2). When looking at drug classes, the highest median exposure was found in beta-lactams (170 %, range 58–443 %), where the median was significantly different from 100 % (P < 0.01).
Recommended total daily dose in patients with impaired renal function according to the SmPC, shown as % of the calculated total daily dose using the proportional rule. Values within the 80–125 % range indicate consistency with the proportional rule. Black and grey filled columns represent the two lowest creatinine clearance levels, where more than one recommendation was available for creatinine clearance of <30 ml/min. White columns indicate recommendation of the normal dose. Shaded areas indicate oral drug administration (PO)
Relatively low exposures were found for ceftazidime (58, 58 %), one of the cefadroxil schemes (72 %), imipenem (44, 62, 65 %), levofloxacin (46, 72 %), netilmicin (75 %), and teicoplanin (20 %), indicating potential underdosage in patients with renal failure. In addition, a very low exposure was noted for a cefotaxime scheme (28 %), which, however, was not included in further analyses, because the recommendation referred to a creatinine clearance of <5 ml/min.
For creatinine clearance values of 15 to <30 ml/min the results were similar. From 48 dosing recommendations, 16 were consistent with the proportional rule, 15 with the eliminated fraction rule, and 2 with both rules. In case of penicillins and cephalosporins, only 2 of the proposed dosing schemes were consistent with the proportional rule and 8 were consistent with the eliminated fraction rule, indicating higher than normal average concentrations. From those dosing schemes which could not be related to a dosing rule, 3 lay in between the dosing lines, 11 had lower and 1 had higher doses as calculated by both rules (Table 1).
When comparing SmPC-recommended total-daily doses to calculated total-daily doses using the proportional rule, a median expected exposure of 96 % with a large range from 29 to 345 % was found, where the median exposure was not significantly different from 100 %. Only 18 (38 %) were within the 80–125 % range, whereas 13 (27 %) were lower and 17 (35 %) were higher (Fig. 2). When looking at drug classes, the highest median exposure was found in beta-lactams (155 %, range 54–232 %), where the median was significantly different from 100 % (P = 0.019).
Relatively low exposures were found for amoxicillin (77 %), ceftazidime (77, 77 %), one of the cefadroxil schemes (54 %), imipenem (68, 77 %), erythromycin (54 %), ciprofloxacin (57 %), and teicoplanin (29, 37, 44 %).
For the 8 drugs where “no dose adjustment” was recommended in the SmPC, a median expected exposure of 142 % (range 73–335 %) was calculated for patients with renal failure. The highest value was found for orally administered cefaclor (335 %), whereas the other values were below 179 %.
In an additional analysis selected dosing schemes from other sources were analysed for drugs where relatively low exposure was found for SmPC-recommended doses (Table 2).
When analysing pharmacokinetic variability, by comparing pooled standard deviation values in patients with normal renal function and renal failure (Table S1), the median increase in coefficient of variation was 1.9-fold for drug clearance and 1.3-fold for half-life.
Discussion
For drug dose adjustment in patients with renal impairment there is no general algorithm on how to adjust drug doses or dosing intervals and, therefore, recommendations vary between the sources. It is usually unknown how these recommendations were derived and what drug exposure can be expected. Using a newly developed method, we found that only 30 % of the recommended dosing schemes are predicted to lead to similar average concentrations, whereas 44 % lead to higher and 26 % lead to lower average concentrations, as expected in patients with normal renal function treated with doses as recommended for severe infections.
Overall, 59 % of the dosing schemes were consistent with one of the general dosing rules. Consistency with a dosing rule implies expected concentrations in patients with renal impairment and that this rule might have been originally used to develop the dosing scheme. For example, 50 % of these dosing schemes were consistent with the eliminated fraction rule (82 % when looking only at beta-lactams), usually indicating more frequent peaks and higher average concentrations. An exception are dosing schemes with relatively long administration intervals (to the right of the crossing point of the dosing lines in our diagram), which is, however, rarely used and was the case only for two drugs (erythromycin and ciprofloxacin).
Surprisingly, we found a relatively low exposure for several dosing schemes, including ceftazidime, cefotaxime, imipenem, erythromycin, ciprofloxacin, levofloxacin, and teicoplanin, indicating potential underdosage. However, recommended dosing schemes for impaired renal function commonly have the character of maximum recommended doses. Only some of them might have been developed to provide an exposure similar to doses that are lower compared to the presently used maximum doses in patients with normal renal function. A relatively low exposure might have been suspected based on previous publications [11, 13, 16, 17, 19].
For ceftazidime, a dosing scheme as proposed by van Dalen [11] leads to predicted exposures of 100–112 % (Table 2) and would be in the range as recommended by clinical experts [12]. Thus, dosing schemes for ceftazidime in patients with renal impairment should be reconsidered and, ideally, evaluated in a clinical study.
For cefotaxime, a dosing scheme as currently approved by the Food and Drug Administration leads to a predicted exposure of 143–169 % (Table 2) and lies between the dosing lines of our diagram. Thus, the SmPC recommendation of 500 mg every 12 h for creatinine clearance of <5 ml/min should not be used in patients with severe infections, unless an equivalent exposure as achieved with 1000 mg every 12 h in patients with normal renal function is desired. Alternatively, the metabolite desacetylcefotaxime might have been influencing dose recommendations, because desacetylcefotaxime accumulation in renal impairment appears to be more pronounced compared to cefotaxime.
For imipenem, dosing recommendations have been modified very recently in some SmPCs and the dosing schemes leading to very low exposure are no longer recommended. Thus, 65 % is expected by using current SmPC recommendations. A dosing scheme as proposed by Verpooten [13] leads to a predicted exposure of 137 % (Table 2) and would be higher as usually recommended. Lower recommendations might be due to pharmacodynamic reasons, because tolerance of imipenem could be lower in uremic patients, as indicated in a case series of 6 patients [14]. Alternatively, cilastatin might have been influencing dose recommendations, because cilastatin accumulation in renal impairment appears to be more pronounced compared to imipenem (Table 2).
For erythromycin, the maximum recommended daily dose is 2000 mg per day in patients with creatinine higher than 2 mg/dl, because of reports of reversible hearing loss occurring in patients with renal insufficiency and in patients receiving high doses of erythromycin [15]. Thus, when a daily dose of 4000 mg is clinically required, another drug should be considered in patients with renal impairment.
For ciprofloxacin, dose adjustment in renal impairment has been discussed controversially. Our present calculations indicate an average exposure of 57 % in patients with severe renal impairment compared to the maximum recommended thrice-daily dose in patients with normal renal function. According to our calculations (Table 2), 400 mg twice-daily might be considered the maximum dose in patients with renal impairment, which would be consistent with recommendations by others [16–18]. The SmPC recommendation of 400 mg once-daily for creatinine clearance of <30 ml/min should be used only if an equivalent exposure as achieved with 400 mg every 12 h in patients with normal renal function is desired.
For levofloxacin, 250 mg once daily should be considered the dose in patients with creatinine clearance of <10 ml/min according to our calculations (Table 2), which would be in the range as recommended by clinical experts [12]. A dose of 125 mg once daily should be used only when an equivalent exposure as achieved with 500 mg once daily in patients with normal renal function is desired.
For teicoplanin, dosing recommendations have been modified very recently and the dosing schemes leading to very low exposures are no longer recommended. Apparently, the previous scheme was based on the assumption that teicoplanin is eliminated almost exclusively as unchanged drug by the renal route. The true value is difficult to define due to the long terminal half-life, but appears to be around 80 % [19]. The current recommendation for severe renal impairment (normal doses for four days, then 1/3 dose per day or a normal dose every three days) leads to an expected exposure of 65 %, which might be considered acceptable, because low concentrations would be detected by therapeutic drug monitoring in the individual.
For beta-lactams administered in combination with a beta-lactamase inhibitor, the concentrations of the inhibitor should also be considered. In case of amoxicillin/clavulanic acid, the expected exposure of clavulanic acid was only 63 %, despite the altered proportion in preparations recommended for patients with renal impairment (5:1 versus 10:1). This can be explained by less dependency of clavulanic acid elimination on renal function. Thus higher doses or shorter dosing intervals might be considered (Table 2).The expected exposure of sulbactam and tazobactam appeared adequate.
Our results are in line with a previous analysis, where it was found that the recommended total daily doses for three beta-lactam antibacterials were up to two-times higher compared to those calculated by the proportional rule, indicating higher than normal average concentrations [20]. In contrast, the recommended daily doses for a carbapenem and a fluoroquinolone were lower, indicating lower than normal average concentrations [20].
The established use of a specific dose adjustment rule (or application of a dosing scheme consistent with that rule) might be related to the therapeutic range of a drug, because the proportional rule is associated with normal average concentrations, whereas the eliminated fraction rule usually produces increased average concentrations [2–5]. This assumption would be in line with our finding that consistency of SmPC-derived dosing schemes with the eliminated fraction rule was most commonly found for penicillins and cephalosporins, whereas the proportional rule was predominant for aminoglycosides. In case of betalactams higher concentrations may be acceptable (considering the broad therapeutic window) but not in case of toxic drugs like the aminoglycosides. When the proportional rule would be generally applied for calculating drug dose adjustments in patients with renal impairment, patients would sometimes receive lower doses as compared to clinically established doses as recommended in the SmPC. For example, ampicillin doses would be, on average, 41 to 46 % lower.
Our graphical method allowed for analysis of recommended dosing schemes using basic pharmacokinetic parameters. However, analyses based on mean population values do not consider variability, which may be increased in patients with renal impairment. In our present analysis, comparing pharmacokinetics in patients with normal renal function and renal failure, variability of clearance and half-life was only moderately increased and it is unclear whether this increase is clinically relevant. A more advanced analysis of dosing schemes, including analysis of variability, has been proposed using model-based predictions [21, 22]. However, such an analysis requires a specific population-pharmacokinetic model validated for application in renal impairment and a meaningful pharmacodynamic marker for each drug. Interestingly, meropenem doses of 2000 mg every 8 h (creatinine clearance 50–120 ml/min), 1000 mg every 8 h (creatinine clearance 30–49 ml/min) and 500 mg every 6 h (creatinine clearance 10–29 ml/min) led to quite similar probabilities of target attainment as calculated for critically ill patients [21]. When analysed according to our method, the latter two dosing schemes correspond quite closely to drug dose adjustment using the proportional rule (Table 2). Additional sources of variability include inaccurate estimates of renal function, especially in adipose patients or patients with acute kidney injury. Such variability could also be analysed using population-pharmacokinetic models.
Our study has several limitations. First, our analysis focuses primarily on pharmacokinetics and expected drug exposure. The effectiveness of a drug, however, might be reduced despite apparently adequate average drug concentrations. Specifically, aminoglycoside dosing schemes using low doses and short dosing intervals can be suspected as suboptimal according to the current pharmacodynamic knowledge [23, 24]. Adequate maximum concentrations, which may be related to the antimicrobial effect of aminoglycosides also in patients with renal failure [25], can be achieved best by prolonging the dosing interval and by therapeutic drug monitoring.
Second, pharmacokinetic parameters for patients with renal failure were largely based on studies including patients with end-stage renal disease. Thus, our results might not be directly applicable to patients with acute renal failure, because such patients may require higher doses due to additional disease-related pharmacokinetic changes, e.g. overhydration [26, 27].
Third, linear models were used to predict pharmacokinetic parameter values for a given level of renal function based on the population extremes (normal renal function vs. renal failure). However, deviation from linearity, if present, is usually quite small in dedicated pharmacokinetic studies including patients with various degrees of renal impairment. By using only the population extremes, the problem of negative pharmacokinetic parameter values at low creatinine clearance values is avoided, which may occur when extrapolating by using linear regression and data from patients with moderately impaired renal function.
Forth, predicted pharmacokinetic parameter values were used for some drugs, where measured values were not available (Table S1). In such cases implicit assumptions apply, e.g. unchanged systemic availability when pharmacokinetic parameters were found only after intravenous administration for an orally administered drug. However, new pharmacokinetic studies would be required to verify such assumptions.
Fifth, our calculations depend on accurate pharmacokinetic parameter estimates for a population, especially calculations for low creatinine clearance values. However, pharmacokinetic parameter estimates from the PKnephro database were usually based on several primary studies and were, thus, considered quite robust. Nevertheless, two specific values were suspected as potentially imprecise (i.e. the CLRF of amikacin and fosfomycin), where only one primary study was available and the reported value appeared quite low. Furthermore, in some cases only pharmacokinetic studies using microbiological assays where available. However, data from such studies was used only when no studies with more accurate assays were available and the drug has no active metabolites.
Conclusion
In conclusion, our newly developed graphical model allowed for analysis of recommended dosing schemes for patients with renal impairment. Most importantly, a number of drugs were identified, where recommended dosing schemes should lead to a lower exposure compared to patients with normal renal function receiving doses for severe infections (i.e. ceftazidime, cefotaxime, imipenem, erythromycin, ciprofloxacin, levofloxacin, and teicoplanin). These drugs should be further analysed (e.g. by using population models), and the dosing schemes should be reconsidered or used only in clinical situations where a lower than maximum exposure appears adequate. In contrast, 44 % of the established dosing schemes lead to higher average concentrations. Thus, general application of the proportional rule for calculating drug dose adjustments, which is sometimes proposed, would lead to lower than clinically established dosing schemes for nearly every second drug.
References
Matzke GR, Aronoff GR, Atkinson AJ Jr, Bennett WM, Decker BS, Eckardt KU, et al. Drug dosing consideration in patients with acute and chronic kidney disease-a clinical update from Kidney Disease: improving Global Outcomes (KDIGO). Kidney Int. 2011;80:1122–37.
Dettli L. Drug dosage in renal disease. Clin Pharmacokinet. 1976;1:126–34.
Dettli L. The kidney in pre-clinical and clinical pharmacokinetics. Jpn J Clin Pharmacol. 1984;15:241–54.
Hartmann B, Czock D, Keller F. Drug therapy in patients with chronic renal failure. Dtsch Arztebl Int. 2010;107:647–55.
Kunin CM. A guide to use of antibiotics in patients with renal disease. A table of recommended doses and factors governing serum levels. Ann Intern Med 1967;67:151–8.
Vidal L, Shavit M, Fraser A, Paul M, Leibovici L. Systematic comparison of four sources of drug information regarding adjustment of dose for renal function. BMJ. 2005;331:263.
World Health Organization. The selection and use of essential medicines. World Health Organ Tech Rep Ser 2011; 965:i–xiv,1–249.
Czock D, Keller F, Paar WD, Thalhammer F. Renal replacement therapy in critically ill patients: how to dose antibiotics during continuous hemofiltration. Intensiv- und Notfallbehandlung. 2008;33:169–83.
Czock D, Keller F. Dosing adjustment according to Dettli’s rule: measured pharmacokinetics in kidney patients versus urinary recovery in healthy individuals [abstract]. Br J Clin Pharmacol. 2009;68(Suppl 1):22.
Obach RS, Lombardo F, Waters NJ. Trend analysis of a database of intravenous pharmacokinetic parameters in humans for 670 drug compounds. Drug Metab Dispos. 2008;36:1385–405.
van Dalen R, Vree TB, Baars AM, Termond E. Dosage adjustment for ceftazidime in patients with impaired renal function. Eur J Clin Pharmacol. 1986;30:597–605.
Aronoff GR, Bennett WM, Berns JS, Brier ME, Kasbekar N, Mueller BA, et al. Drug prescribing in renal failure. Philadelphia: American College of Physicians; 2007.
Verpooten GA, Verbist L, Buntinx AP, Entwistle LA, Jones KH, De Broe ME. The pharmacokinetics of imipenem (thienamycin-formamidine) and the renal dehydropeptidase inhibitor cilastatin sodium in normal subjects and patients with renal failure. Br J Clin Pharmacol. 1984;18:183–93.
Campise M. Neurological complication during imipenem/cilastatin therapy in uraemic patients. Nephrol Dial Transplant. 1998;13:1895–6.
Sacristán JA, Soto JA, de Cos MA. Erythromycin-induced hypoacusis: 11 new cases and literature review. Ann Pharmacother. 1993;27:950–5.
MacGowan AP, White LO, Brown NM, Lovering AM, McMullin CM, Reeves DS. Serum ciprofloxacin concentrations in patients with severe sepsis being treated with ciprofloxacin 200 mg i.v. bd irrespective of renal function. J Antimicrob Chemother. 1994;33:1051–4.
Jones EM, McMullin CM, Hedges AJ, Lovering AM, White LO, Reeves DS, et al. The pharmacokinetics of intravenous ciprofloxacin 400 mg 12 hourly in patients with severe sepsis: the effect of renal function and intra-abdominal disease. J Antimicrob Chemother. 1997;40:121–4.
Pea F, Poz D, Viale P, Pavan F, Furlanut M. Which reliable pharmacodynamic breakpoint should be advised for ciprofloxacin monotherapy in the hospital setting? A TDM-based retrospective perspective. J Antimicrob Chemother. 2006;58:380–6.
Derbyshire N, Webb DB, Roberts D, Glew D, Williams JD. Pharmacokinetics of teicoplanin in subjects with varying degrees of renal function. J Antimicrob Chemother. 1989;23:869–76.
Martin-Facklam M, Rengelshausen J, Tayrouz Y, Ketabi-Kiyanvash N, Lindenmaier H, Schneider V, et al. Dose individualisation in patients with renal insufficiency: does drug labelling support optimal management? Eur J Clin Pharmacol. 2005;60:807–11.
Crandon JL, Ariano RE, Zelenitsky SA, Nicasio AM, Kuti JL, Nicolau DP. Optimization of meropenem dosage in the critically ill population based on renal function. Intensive Care Med. 2011;37:632–8.
Patel N, Scheetz MH, Drusano GL, Lodise TP. Identification of optimal renal dosage adjustments for traditional and extended-infusion piperacillin-tazobactam dosing regimens in hospitalized patients. Antimicrob Agents Chemother. 2010;54:460–5.
Eyler RF, Mueller BA. Antibiotic pharmacokinetic and pharmacodynamic considerations in patients with kidney disease. Adv Chronic Kidney Dis. 2010;17:392–403.
Czock D, Markert C, Hartman B, Keller F. Pharmacokinetics and pharmacodynamics of antimicrobial drugs. Expert Opin Drug Metab Toxicol. 2009;5:475–87.
Keller F, Borner K, Schwarz A, Offermann G, Lode H. Therapeutic aminoglycoside monitoring in renal failure patients. Ther Drug Monit. 1987;9:148–53.
Eyler RF, Mueller BA. Antibiotic dosing in critically ill patients with acute kidney injury. Nat Rev Nephrol. 2011;7:226–35.
Pea F, Viale P, Furlanut M. Antimicrobial therapy in critically ill patients: a review of pathophysiological conditions responsible for altered disposition and pharmacokinetic variability. Clin Pharmacokinet. 2005;44:1009–34.
Funding
The authors received no funding for the present study.
Conflicts of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Czock, D., Spitaletta, M. & Keller, F. Suboptimal antimicrobial drug exposure in patients with renal impairment. Int J Clin Pharm 37, 906–916 (2015). https://doi.org/10.1007/s11096-015-0141-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-015-0141-0