Abstract
Purpose
We aimed to assess intranasal (IN) epinephrine effects on cerebrospinal fluid (CSF) absorption, nasal mucosa quality, plasma epinephrine pharmacokinetics (PK), and cardiovascular changes in dogs.
Methods
CSF epinephrine concentration was measured and nasal mucosa quality was evaluated after IN epinephrine 4 mg and one or two 4 mg doses (21 min apart), respectively. Maximum plasma concentration [Cmax], time to Cmax [Tmax], area under the curve from 0 to 120 min [AUC0–120], and cardiovascular effects were evaluated after epinephrine IN (4 and 5 mg) and intramuscular (IM; 0.3 mg). Clinical observations were assessed.
Results
After epinephrine IN, there were no changes in CSF epinephrine or nasal mucosa. Cmax, Tmax, and AUC1–120 were similar following epinephrine IN and IM. Epinephrine IN versus IM increased plasma epinephrine at 1 min (mean ± SEM, 1.15 ± 0.48 for 4 mg IN and 1.7 ± 0.72 for 5 mg IN versus 0.47 ± 0.11 ng/mL for 0.3 mg IM). Epinephrine IN and IM produced similar heart rate and ECG results. Clinical observations included salivation and vomiting.
Conclusions
Epinephrine IN did not alter CSF epinephrine or nasal tissue and had similar cardiovascular effects as epinephrine IM. Epinephrine IN rapidly increased plasma epinephrine concentration versus epinephrine IM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epinephrine is the first-line therapy for the treatment of severe allergy and anaphylaxis, acting through alpha-adrenergic–mediated vasoconstrictive mechanisms to alleviate allergic symptoms (1,2,3,4). Immediate epinephrine treatment in anaphylaxis prevents life-threatening effects and leads to decreased airway resistance, bronchodilation, reversal of hypotension, and protective chronotropic and ionotropic cardiac effects (5). Autoinjectors, such as the prescribed EpiPen® (Mylan Specialty, LP, Basking Ridge, NJ, USA), are effective in reducing anaphylactic symptoms. However, autoinjectors require regular training for use and have been associated with injuries, administration anxiety, and delayed treatment (3,6,7,8,9). Alternative routes of administration and devices are needed for epinephrine delivery in the treatment of severe allergy and anaphylaxis.
The intranasal (IN) route of administration has become increasingly used for drugs requiring a rapid onset of action (10). The high vascularization and tissue permeability of the nasal mucosa allows for fast absorption into the bloodstream and delivery to target areas (11). IN administration has been explored with opioids for pain treatment, opioid antagonists for reversal of heroin overdose, treatments for Alzheimer’s disease, glucagon for hypoglycemia, and benzodiazepines for seizures (12,13,14,15,16,17,18,19,20). IN delivery of these drugs leads to drug delivery to the brain, where they can exert their therapeutic effects (12,13,14,15,16,17,18,19,20). For example, in the treatment of opioid overdose, naloxone IN rapidly reverses the respiratory and central nervous system (CNS)-depressant effects (14,15,16). The rapid absorption and delivery to the brain after IN administration is desirable for drugs like naloxone, because of their intended therapeutic effects elicited by brain mechanisms (12,13,14,15,16,17,18,19,20).
If able to penetrate the blood–cerebrospinal fluid (CSF) barrier and blood–brain barrier following IN administration, epinephrine could have potential CNS effects that differ from the desired peripheral effects of bronchodilation and vasoconstriction in the treatment of severe allergy and anaphylaxis. Endogenous brain epinephrine acts at adrenergic receptors to mediate behaviors associated with anxiety, stress, and hyperactivity (21,22,23). In turn, stress and anxiety associated with autoinjector use can be heightened through CNS epinephrine and could potentially exacerbate allergic symptoms (6,22,24). However, due to the ionic state of epinephrine in an IN solution, it should avoid CNS entry and exert effects throughout the respiratory and cardiovascular systems only, as intended for treating allergy and anaphylaxis (25).
Another concern with IN drug administration is the irritation of the nasal cavity and, specifically, the nasal mucosa. The nasal mucosa is highly sensitive to both mechanical and chemical foreign bodies and may be prone to irritation or damage upon exposure (26). Safety parameters aside from nasal cavity changes have been assessed previously with epinephrine IN under non–good laboratory practice (non-GLP) parameters (27). We have previously reported that epinephrine IN was well tolerated in dogs in doses ranging from 2 to 10 mg while postdose vomiting was observed at a dose of 20 mg. Further, we have previously reported the bioequivalence of epinephrine 4 and 5 mg IN to 0.3 mg intramuscular (IM) in dogs under non-GLP parameters in a limited number of animals (n = 6). We found no significant differences in pharmacokinetic (PK) exposure parameters but a significant increase in plasma epinephrine at 1 min with epinephrine IN versus IM (27).
In these three preclinical studies, we evaluated the effects of epinephrine IN administration on CSF epinephrine delivery, on the nasal mucosa tissue quality, and on plasma epinephrine PK and cardiovascular changes. The pharmacokinetic and cardiovascular study was conducted under GLP conditions with an expanded number of dogs per group.
Materials and Methods
Dogs
General procedures for dog care and housing for all studies were in accordance with the Guide for the Care and Use of Laboratory Animals (28). Experiments were approved by the Institutional Animal Care and Use Committee of MRIGlobal (Kansas City, MO, USA) before dog procurement from a United States Department of Agriculture (USDA)-certified vendor. Male and female dogs between 5 and 7 months of age and weighing approximately 8 to 11 kg were used. Dogs were individually housed indoors in primary enclosures (cage banks, Shor-line) that provided floor space either meeting or exceeding specifications of the USDA Animal Welfare Act and as described in the Guide for the Care and Use of Laboratory Animals (28). Dogs were housed under controlled environmental conditions with a standard 12-h light/dark cycle, with free access to food and water, provided daily interaction with MRIGlobal staff, and exercised on a regular weekly basis.
Formulation
Epinephrine (United States Pharmacopeia [USP] Grade) was purchased from Spectrum Chemicals & Laboratory Products and Millipore Sigma (St. Louis, MO, USA). Two dosing concentrations of epinephrine (4 mg/100 μL and 5 mg/100 μL) were formulated. The epinephrine formulation for IN administration was based on the injectable product with appropriate modifications suitable for IN administration. In addition to water for injection, sodium metabisulfite (SMBS), and sodium chloride, the formulation included a viscosity modifier, preservative, and buffer. The final formulation had a pH of 5.0 ± 0.5. The prepared epinephrine formulation for IN administration was stored at 5 ± 3°C protected from light in amber glassware. The EpiPen Adult (0.3 mg) was used as the control. The EpiPens were procured from local pharmacies and stored at room temperature (20–25°C) protected from light.
CSF and Plasma Epinephrine PK Study
The objective of the CSF epinephrine PK study was to evaluate CSF epinephrine concentration compared with plasma epinephrine concentration after epinephrine IN administration. Each individual dog received one epinephrine IN administration. Dogs were sedated with buprenorphine (0.01 mg/kg IM). An intravenous catheter was placed and propofol (6 mg/kg) was given to effect. Once dogs reached a surgical plane of anesthesia, they were intubated, placed on isoflurane, and kept warm. Oxygen flow rates were at 10 mL/kg/min and isoflurane concentration was set between 0.5% and 5%.
Monitoring included pulse oximetry, electrocardiogram, end tidal CO2, oscillometric blood pressure, and body temperature. Additionally, mucous membrane color and capillary refill time was measured. All measurements were taken every 5 to 10 min. Intravenous fluids (0.9% sterile saline) were administered at 5 mL/kg/h. Additional boluses (at 10 mL/kg increments) were administered if hypotension developed (<60 mmHg mean arterial blood pressure).
Once anesthetized, dogs were placed in right lateral recumbency. A rectangular shaped area (approximately 4–6 in. long × 3–5 in. wide) was shaved on the lower back area. The area was cleansed with chlorhexidine scrub and wiped with alcohol to prepare a sterile field. A nonsterile assistant flexed the dog’s spine to widen the proposed site of needle insertion. A sterile veterinarian inserted a 22-gauge (2.5-in.) spinal needle into approximately the L4-L5 intervertebral space. The stylet of the needle was removed to check for the presence of CSF. A minimum of 0.2 mL (up to 0.5 mL) was collected.
Plasma and CSF samples were collected twice: immediately before (0 min) and 15 min after epinephrine 4 mg IN (Table I). Samples were analyzed for epinephrine concentration. Plasma samples were analyzed as described below with a calibrator range of 1 to 32 ng/mL, and quality control samples of 4, 12, and 24 ng/mL, or a calibrator range of 0.4 to 10 ng/mL, and quality control samples of 1, 3, and 5 ng/mL. Control plasma was heat treated (55°C for ~8 days) and stabilized with SMBS (~317 mg/mL) (plasma/SMBS = 98:2, v/v) before use. Calibrators, quality controls, blanks, and incurred samples were prepared by solid-phase extraction using 96-well plates (Biotage Evolute Express WCX, Charlotte, NC, USA) and epinephrine-d6 as a true internal standard. The obtained extracts were analyzed by liquid chromatography tandem-mass spectrometry (LC-MS/MS) using a C18-pentafluorophenyl phase column. LC-MS/MS analysis was performed in positive electrospray ionization mode using multiple reaction monitoring scanning.
Otoscopic Evaluation Study
The otoscopic evaluation study utilized otoscopic evaluation techniques to identify the potential impact of IN epinephrine on nasal mucosa quality. Each individual dog received one or two epinephrine IN administrations. Dogs were first sedated with dexmedetomidine at 5 μg/kg and buprenorphine HCl at 0.01 mg/kg intravenously. A standard otoscope with light source and magnification was used for the examination. A small nose cone was placed on the end of the scope and gently passed into the nares. No lubricant was used for passage of the nose cone. The right nares and nasal cavity was examined in all animals; this is the same side that was dosed with epinephrine IN. The nose cone was inserted approximately 2 cm to allow adequate visualization of the nasal mucosa. No appreciable trauma occurred to the nares or nasal cavity during the examinations. The majority of dogs were adequately sedated for the examination through administration of dexmedetomidine and buprenorphine for 5 min. Examination duration was approximately 30 to 90 s. Following the otoscopic examination, IM atipamezole was administered to reverse dexmedetomidine, and all animals recovered uneventfully. Dogs received either one IN epinephrine administration (4 mg) or two doses of IN epinephrine (4 mg each) 21 min apart.
For otoscopic evaluation, a scoring system was used to capture normal versus abnormal findings on examination. The otoscopic scoring system was applied to the evaluation of erythema, edema, and capillary bed quality. Erythema scores included N = normal or + 1 = slightly increased redness, or + 2 = significantly increased redness. Edema scores included N = normal (no edema) or + 1 = edematous. Capillary scores included N = normal or + 1 = hypervascular or − 1 = hypovascular or 0 = not visible. A typical dog had normal pink to red coloration, smooth surface, no abnormal secretions, normal appearing vascularity, and no appreciable swelling. Any abnormal finding was documented in the comments section.
Plasma PK and Cardiovascular Study
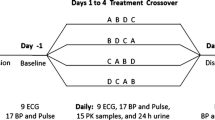
The plasma PK and cardiovascular study aimed to repeat the evaluation of both PK and cardiovascular effects of epinephrine IN versus IM under GLP regulations (29). Each individual dog received one epinephrine IN or IM administration. Before epinephrine IM administration, dogs were shaved on the right thigh. PK parameters were obtained for each dog before and after either a single epinephrine 4 or 5 mg IN or 0.3 mg IM administration (Table I).
For epinephrine IN, a technician lightly restrained conscious dogs held in a prone position, while a second technician delivered 100 μL epinephrine in a 200-μL capacity cannula (pipette tip) that was attached to a 100-μl calibrated pipette. No dead space was present in the cannula following dose delivery. The entire dose of epinephrine (4 mg or 5 mg in 100 μL) was delivered at a depth of three quarters of an inch into each dog’s right nostril. For epinephrine IM, EpiPen instructions from the manufacturer were followed.
Approximately 2 mL of whole blood was collected at the following time points: before dosing (60, 15, 2–3 min before time zero) and at 1, 5, 10, 15, 20, 25, 30, 60, 90, and 120 min postdose (±10% of target time point) (Table I). Whole blood was collected into dipotassium ethylenediaminetetraacetic acid tubes and processed to plasma. Blood samples were immediately placed on wet ice, and the tubes were centrifuged to separate the plasma from the heavier elements (i.e., red blood cells). SMBS was added to the plasma samples to prevent oxidation of epinephrine. The processed samples were stored in individually labeled tubes at −80°C ± 10°C until LC-MS/MS analysis.
Before PK data analysis, the three predose (taken at 60, 15, and 2 min before time zero) plasma epinephrine concentration values for each dog were averaged, then this average was subtracted from the postdose plasma epinephrine concentration values reported at 1, 5, 10, 15, 20, 25, 30, 60, 90, and 120 min postdose (±10% of target time point). If one or more of the predose samples fell beneath the limit of quantification, the mean of the remaining quantifiable values was used for baseline correction. If all three predose samples fell under the limit of detection (i.e., values not determined), no baseline correction was performed on the postdose samples. If the postdose values were negative after baseline correction, these values were changed to zero for subsequent PK analysis. PK parameters of maximum plasma concentration (Cmax), time to reach maximum plasma concentration (Tmax), and area under the curve from 0 to 120 min (AUC0–120) were compared between IN epinephrine (4 and 5 mg) and epinephrine IM via autoinjector (0.3 mg). Plasma concentration-time data were first analyzed for the individual dog, and then PK measurements (Cmax, Tmax, and AUC0–120) were averaged within a group. Mean residence time (MRTlast) measurements for epinephrine following epinephrine 4 and 5 mg IN versus epinephrine 0.3 mg IM was evaluated.
All plasma samples were analyzed to determine epinephrine concentrations, using an approved bioanalytical method. Values that were inconsistent with the values in that same group (either from this study or from previously performed non-GLP studies) were assessed as potential outliers using a statistical outlier test in accordance with MRIGlobal Standard Operating Procedure (MRI-0030). If the value was considered an outlier, the outlying data point was excluded from the data set. Any data points that were excluded were subjected to reanalysis using the remaining aliquot of plasma, and the data point from reanalysis replaced that of the excluded data point within the study. If the second data point from the reanalysis was still considered an outlier, then those dogs were repeated with dosing and all PK blood collection time points. Another veterinary examination of these dogs was performed both before and after dose administration.
PK data analysis and evaluation of plasma concentration-time curves were performed using Phoenix32 WinNonlin software (Version 6.3; Pharsight Corporation, St. Louis, MO, USA). Individual plasma epinephrine concentration-time curves were analyzed using model-independent methods. Concentrations less than the lower limit of quantitation (<0.4 ng/mL) were set to zero for PK analysis. Coefficient of variation analyses were performed.
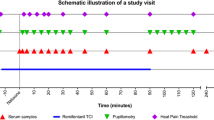
Cardiovascular analyses were performed under GLP regulations (29). Before dose administration, dogs were shaved for electrode placement on the left and right chest and for epinephrine IM injection in the right thigh. Telemetric collection jackets were placed on dogs and electrocardiogram (ECG) and heart rate measurements were obtained at predose time points (60, 12, and 2–3 min prior to time zero) and at 1, 5, 10, 15, 20, 30, 60, 90, and 120 min after epinephrine administration (Table I). The ECG parameters that were evaluated included PR, QRS, QT, and RR. A 6 s ECG was reported at the Cmax for epinephrine for each dog to evaluate the ECG parameters listed above. Data collection points occurred 60 min before dose administration (baseline) and through the 120-min endpoint for a total collection time of 180 min.
Clinical Observations
In both the plasma PK and heart rate study and the otoscopic evaluation study, clinical observations were recorded. Clinical observations were recorded at approximately 1 h before epinephrine administration and 1 h after epinephrine administration.
Results
CSF and Plasma Epinephrine PK Study
The changes in CSF and plasma epinephrine concentrations before and after epinephrine 4 mg IN were evaluated to determine whether epinephrine enters the CNS following epinephrine IN. Dogs between 10 to 13 months of age and weighing approximately 7 to 14 kg were used. Four dogs were evaluated for CSF and plasma epinephrine following epinephrine IN administration. At the predose time point, there was no measurable epinephrine concentration in CSF, and no change was detected at 15 min after epinephrine 4 mg IN (Fig. 1). Average plasma epinephrine concentration increased from 0.214 ng/mL to 1.123 ng/mL after epinephrine 4 mg IN (Fig. 1).
Otoscopic Evaluation Study
Otoscopic evaluations were performed both before and after epinephrine IN to evaluate the potential effects of epinephrine IN on irritation or adverse effect to the nares. Dogs between 5 to 7 months of age and weighing approximately 8 to 11 kg were used in the otoscopic evaluation study. Four dogs were evaluated after one single nostril dose of epinephrine 4 mg IN, and four dogs were evaluated following two single nostril doses of epinephrine 4 mg IN 21 min apart. During the pre-epinephrine IN examinations, there were no significant findings. All dogs received normal scores in levels of erythema, edema, and capillary assessment. At 90 min following a single dose of epinephrine 4 mg IN, one dog had a linear mark of fresh blood near a large capillary; however, the remaining vasculature appeared normal and there was no active bleeding (Table II). At 90 min following two doses of epinephrine 4 mg IN, the results were as follows: one dog was normal with no change, one dog had a slight increase in redness on the surface of the nasal mucosa (+1 erythema score), one dog had a small red line or mark on the mucosa with normal erythema score, and one dog had a + 1 erythema score with slight redness and + 1 capillary score indicated by pronounced vasculature (Table II). Overall, there were no consistent adverse effects noted on otoscopic examination following one or two administrations of IN epinephrine.
Plasma PK and Cardiovascular Study
The plasma PK parameters and plasma concentration-time curves of epinephrine were evaluated following IN or IM epinephrine administration. Dogs between 5 to 7 months of age and weighing approximately 8 to 11 kg were used in the plasma PK study. Sixteen dogs were included per dosage group. There were no differences in predose epinephrine measurements after epinephrine 4 mg and 5 mg IN or 0.3 mg IM (mean ± standard error of the mean [SEM] 60 min predose: 0.38 ± 0.06, 0.38 ± 0.06, 0.35 ± 0.07, respectively; 15 min predose: 0.36 ± 0.05, 0.38 ± 0.07, 0.35 ± 0.02; 2 min predose: 0.30 ± 0.02, 0.35 ± 0.07, 0.31 ± 0.02).
Following epinephrine IN, Cmax progressively increased with epinephrine 4 and 5 mg IN (mean Cmax ± SEM: 2.48 ± 0.57 and 3.01 ± 0.74 ng/mL). After epinephrine 0.3 mg IM, the average Cmax was 2.76 ± 0.70 ng/mL (Table III). Overall, there were no significant differences in Cmax between epinephrine 4 mg IN or 5 mg IN and epinephrine 0.3 mg IM (p = 0.75 and p = 0.81). There were no significant differences in Tmax with epinephrine 4 and 5 mg IN versus epinephrine 0.3 mg IM (median [range], 20 [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30] and 15 [1–90] versus 25 [5–60] minutes) (Table III). Mean AUC0–120 was 75.0 ± 13.45 and 81.8 ± 11.58 ng*minutes/mL after epinephrine 4 and 5 mg IN, respectively, compared with 110 ± 10.53 ng*minutes/mL after epinephrine 0.3 mg IM (Table III). MRTlast measurements for epinephrine following epinephrine 4 and 5 mg IN versus epinephrine 0.3 mg IM were 51.1 and 53.9 min versus 50.4 min.
Epinephrine 4 and 5 mg IN produced similar plasma concentration-time curves (Fig. 2). At 1 min after epinephrine administration, the changes in plasma epinephrine concentrations from baseline were increased with epinephrine 4 and 5 mg IN versus epinephrine 0.3 mg IM (mean ± SEM, 1.15 ± 0.48 and 1.7 ± 0.72 versus 0.47 ± 0.11 ng/mL, respectively) (Fig. 2). At 5 min after epinephrine administration, the change in plasma epinephrine concentrations from baseline were lower with epinephrine 4 and 5 mg IN versus epinephrine 0.3 mg IM (mean ± SEM, 0.64 ± 0.14 and 0.88 ± 0.23 versus 1.77 ± 0.78 ng/mL, respectively) (Fig. 2).
The variability in mean plasma epinephrine concentrations, as measured by coefficient of variation, ranged from 53.4% to 170% with epinephrine IN (4 or 5 mg) and from 48.7% to 174% with IM epinephrine (0.3 mg). Epinephrine was quantifiable up to 120 min postdose after epinephrine 4 mg IN, up to 30- or 120-min postdose after epinephrine 5 mg IN, and up to 120 min postdose after epinephrine 0.3 mg IM. Individual peak plasma epinephrine concentrations were observed between 1 and 30 min after epinephrine 4 mg IN, between 1 and 90 min after epinephrine 5 mg IN, and between 5 and 60 min after epinephrine 0.3 mg IM (Fig. 3).
Individual plasma epinephrine concentrations in dogs after epinephrine 4 mg IN (A) 5 mg IN (B) and 0.3 mg IM (C) dosing (n=16/group). IM, intramuscular; IN, intranasal. aIn one dog, the plasma epinephrine concentration was below quantifiable concentrations at 1 min after dosing with epinephrine 4 mg IN. bIn one dog, the plasma epinephrine concentration was below quantifiable concentrations 90 min after dosing with epinephrine 5 mg IN
There were no sex differences in systemic epinephrine exposure following IN or IM epinephrine. The female-to-male ratios for area under the curve from 0 to 24 h (AUC0–24) were 0.711, 1.20, and 1.27 ng*minutes/mL after epinephrine 4 mg IN, 5 mg IN, and 0.3 mg IM, respectively. Therefore, all data presented are combined male and female data.
The effects of IN epinephrine administration on heart rate were evaluated compared to the heart rate effects of IM epinephrine administration. Dogs were between 5 to 7 months of age and weighed approximately 8 to 11 kg. Sixteen dogs were included per dosage group. Changes in heart rate after epinephrine 4 or 5 mg IN epinephrine doses were similar (Fig. 4). Heart rate increased following epinephrine 4 mg IN administration from 127 beats per minute (bpm) at 60 min before epinephrine administration to a maximum of 132 bpm at 10 min (Fig. 4). Heart rate increased following epinephrine 5 mg IN from 124 bpm at 60 min before epinephrine administration to a maximum of 132 bpm at 1 min after epinephrine administration (Fig. 4).
Average heart rate increased after epinephrine 0.3 mg IM from a baseline of 103 bpm at 60 min before epinephrine administration to a maximum of 167 bpm at 90 min after epinephrine administration (Fig. 4). The increase in heart rate following IM epinephrine (0.3 mg) remained steady throughout 120 min after IM epinephrine administration (Fig. 4).
There were no differences in average PR, QRS, QT, or RR intervals after epinephrine 4 or 5 mg IN versus epinephrine 0.3 mg IM (Fig. 5). Following epinephrine 4 or 5 mg IN or epinephrine 0.3 mg IM, the mean intervals (mm) were as follows: PR, 93.17, 84.48, 89.29; QRS, 29.38, 31.38, and 30.56; QT, 216.00, 218.89, 220.95; RR, 551.20, 492.77, and 426.30 (Fig. 5).
Clinical Observations
In the plasma PK and heart rate study, minor dose-related observations were noted immediately after dosing with epinephrine 4 and 5 mg IN. Nine dogs were reported licking the nose or muzzle immediately following epinephrine IN, whereas one dog (epinephrine 5 mg IN) exhibited increased salivation 1 min after administration. There were epinephrine-related clinical observations noted following epinephrine 4 or 5 mg IN and epinephrine 0.3 mg IM. After epinephrine 4 mg IN, one dog exhibited white and yellow emesis (~2 mL) approximately 30 min postdose and one dog exhibited salivation. After epinephrine 5 mg IN, emesis and/or retching was observed in four dogs an hour postdose and one dog was observed sleeping. After epinephrine 0.3 mg IM, 11 dogs exhibited epinephrine-related observations ~45 min to an hour postdose. These observations included vocalization, whining, restlessness, pacing, mild to heavy salivation, and bruising on neck.
Clinical observations from the otoscopic evaluation study were mild or excessive salivation after one dose of epinephrine 4 mg IN. There were no clinical observations following two doses of epinephrine 4 mg IN.
Discussion
After epinephrine IN, there were no changes in CSF epinephrine concentration or otoscopic evaluation, and increased plasma epinephrine concentration at 1 min and slightly increased heart rate as compared to epinephrine IM. No major adverse events were noted with either epinephrine IN dose. These results are consistent with our prior publication that showed no adverse effects with doses of epinephrine 2 to 10 mg IN (27). However, a dose of epinephrine 20 mg IN was typically associated with vomiting. The IN route of administration is a potential option for the use of epinephrine in the treatment of severe allergy and anaphylaxis.
Autoinjector use is associated with administration challenges and access issues (3,6,7,8,9). The IN route of administration has become increasingly routine for convenience and rapid delivery in prehospital, emergency, and outpatient settings (30,31). If the intended therapeutic effects of drugs are mediated by the CNS, drug formulations can be specifically tailored to reach the olfactory epithelium of the nasal cavity and target brain delivery (25). Endogenous epinephrine has well-established CNS effects on mood and behavior that differ from the desired peripheral effects in the treatment of anaphylaxis (21,23). Thus, the goal in treating severe allergy and anaphylaxis would be to avoid CNS epinephrine entry, potentially through delivery to the respiratory epithelium of the nasal cavity (25). Epinephrine IN demonstrated increased plasma epinephrine, but there was no change in CSF epinephrine concentration, which was undetectable at baseline. The lack of epinephrine delivery to CSF following epinephrine IN is supported by the well-established blood–CSF barrier and blood–brain barrier blockades of epinephrine due to its polar nature (32,33). Epinephrine delivered intranasally is unable to penetrate the blood–brain barrier and, thus, is not able to influence brain neurotransmitter systems in the modulation of emotion and behavior (32,33).
Otoscopic evaluations showed that epinephrine IN had no effects on the integrity of the nasal mucosa. The nasal mucosa has a small area with heightened sensitivity that is prone to damage with direct contact or mechanical stress (26). Damage to the nasal mucosa following IN administration of drugs can present as nosebleeds and crusting, and potentially erosions or perforation, leading to long-term tissue injury (26). In addition, exposure to chemicals or particles in the nasal cavity can lead to irritation or pain (34). However, there were no effects observed in the otoscopic evaluation study that showed irritation or decreased tissue integrity following epinephrine IN administration. Erythema and edema were observed at low levels in only some of the dogs, and the capillary beds of all dogs were normal following epinephrine IN administration. Gross observations of the nasal mucosa were performed because changes in histology are not expected after one dose. These findings support the safe and convenient use of IN delivery of epinephrine in the treatment of severe allergy and anaphylaxis.
IN epinephrine produced PK similar to IM epinephrine via EpiPen Adult. There were no statistically significant differences in the Cmax (t-test, p > 0.05) between epinephrine 4 and 5 mg IN and epinephrine 0.3 mg IM. The Tmax and AUC0–120 values were also similar between groups. This confirms previous findings from our non-GLP studies on the bioequivalence between epinephrine 4 and 5 mg IN and 0.3 mg IM (27). The change in plasma epinephrine concentration was greater at 1 min after epinephrine 4 and 5 mg IN compared with 0.3 mg IM. The increased epinephrine absorption at 1 min after epinephrine IN versus IM is also consistent with the previous findings from the non-GLP study comparing 4 and 5 mg IN to 0.3 mg IM epinephrine (27). However, at 5 min, in the current study, the opposite effect occurred with a smaller change in plasma epinephrine concentration with epinephrine 4 or 5 mg IN versus 0.3 mg IM, a difference that was observed at 15 min post administration in previous studies comparing epinephrine 5 mg IN to 0.3 mg IM (27).
Heart rate increases after epinephrine 4 and 5 mg IN were similar in magnitude and duration, and similar as well to results from non-GLP studies (27). After epinephrine 0.3 mg IM, elevated heart rates continued to increase throughout 120 min after epinephrine administration, as was similarly reported in a non-GLP study (27). After epinephrine 0.3 mg IM, the maximum epinephrine concentrations were within the 60- to 120-min time frame. There was no association between the plasma epinephrine concentrations and heart rate changes, as the highest heart rates were observed at times when plasma epinephrine concentrations had decreased below peak concentrations. In addition, the ECG patterns after epinephrine 4 and 5 mg IN and 0.3 mg IM were similar. Thus, epinephrine IN was not associated with abnormal effects on cardiac electrophysiology.
The PK and cardiovascular study results are in line with other studies aside from ours showing PK and pharmacodynamic effects with IN epinephrine in preclinical and clinical models (35,36,37). In a canine model of cardiac arrest, Bleske and colleagues found rapidly increased epinephrine concentrations and improvements in coronary perfusion following epinephrine IN administration (35,36). In these studies by Bleske and colleagues, the addition of the alpha-adrenergic blocker phentolamine was necessary for epinephrine absorption after epinephrine IN (35,36). A preliminary clinical study with five adult participants reported bioequivalence between epinephrine 5 mg IN and 0.3 mg IM. In opposition from the previous non-GLP studies, Srisawat and colleagues did not observe significant absorption of low-dose epinephrine (0.3 to 2.5 mg) IN (37).
Epinephrine IN was well tolerated. The only effects observed following epinephrine IN were nose licking and excess salivation. Epinephrine IM was associated with injection site pain as indicated by vocalizations, whining, restlessness, and pacing. Injection site pain with epinephrine IM is a commonly reported adverse effect in patients being treated for anaphylaxis in clinical studies (9,38). The issues associated with autoinjector use emphasize the need for an alternative route of epinephrine administration in the treatment of severe allergy and anaphylaxis.
In the current studies, epinephrine was delivered as a 100 μL bolus. It is possible that absorption may have been different had a device with a smaller droplet size been used. In the CSF and plasma epinephrine study, a potential limitation was the time point for epinephrine measurement. The 15-min time point for CSF and plasma epinephrine was selected based on standard practice. However, because epinephrine is in ionized form, it is possible that slower transport during absorption may lead to plasma or CSF epinephrine concentration changes at later time points. Future studies could expand the time frame for monitoring epinephrine in CSF. In addition, the exact nasal cavity area of delivery was not assessed in the otoscopic evaluation study and provides area for further exploration in future studies.
Other limitations of these studies include the number of dogs for the CSF and otoscopic evaluation studies, and the homogenous population of dogs, limiting the scope and interpretation of epinephrine IN versus IM administration. Additionally, there were no comparisons between IN and IM epinephrine or between IN epinephrine and no administration in the CSF and PK and otoscopic evaluation studies. The population for all studies was a homogenous population of dogs, limiting the scope and interpretation of IN versus IM epinephrine administration. Differences in weight and age may affect the PK of IN epinephrine when applied in a clinical setting. There were no comparisons to saline-administration controls made throughout the studies, which may have impacted interpretation of results, particularly the otoscopic evaluation results. Likewise, the clinical observations were evaluated in two studies only. Additional information may also have been gained by including a histological examination of the nasal mucosa.
The lack of epinephrine delivery to the CNS after epinephrine IN administration suggests that when administered intranasally, epinephrine is not able to penetrate the blood–brain barrier. In dogs, epinephrine IN produced more rapid increases in plasma epinephrine concentration at both doses tested (4 and 5 mg) versus IM administration with the EpiPen (0.3 mg). The rapid increase in plasma epinephrine concentration with IN administration has implications for the treatment of anaphylaxis, in which quick administration is critical. All other PK parameters were similar between epinephrine IN and IM. Thus, no overall differences in exposure are noted with epinephrine IN versus IM. Future studies could aim to identify the target area of delivery in the nasal cavity to further support the lack of CNS delivery and optimal absorption with lack of nasal mucosa damage. These studies show that epinephrine IN does not produce epinephrine CSF entry or nasal mucosa irritation following epinephrine IN. The studies confirm previous non-GLP studies showing bioequivalence between epinephrine 4 or 5 mg IN and 0.3 mg IM. These studies provide a foundation for the use of epinephrine IN administration to be further explored in clinical trials. The use of epinephrine IN has potential to become the new standard of care in the treatment of severe allergy and anaphylaxis, which would contribute to the alleviation of patient or caregiver concerns with autoinjector use.
Conclusions
Epinephrine IN did not result in epinephrine CSF delivery in dogs. Epinephrine IN increased plasma epinephrine concentration at a more rapid rate than epinephrine IM. There were no differences in heart rate alterations between epinephrine IN and IM. No adverse effects were noted intranasally, including direct effects on the nasal mucosa. Thus, the IN delivery of epinephrine is ideal for anaphylaxis treatment, where speed of delivery and minimal adverse effects are essential.
Acknowledgements and Disclosures
Writing and editing assistance was provided by Caryne Craige, PhD, of Fishawack Communications Inc. This support was funded by Bryn Pharma, LLC. The authors declare that they have no conflicts of interest. All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Abbreviations
- AUC0–120 :
-
area under the curve from 0 to 120 min
- AUC0–24 :
-
area under the curve from 0 to 24 h; bpm, beats per minute
- Cmax :
-
maximum plasma concentration
- CNS:
-
central nervous system
- CSF:
-
cerebrospinal fluid
- GLP:
-
good laboratory practice
- IM:
-
intramuscular
- IN:
-
intranasal
- LC-MS/MS:
-
liquid chromatography tandem-mass spectrometry
- MRTlast :
-
mean residence time
- PK:
-
pharmacokinetics
- SEM:
-
standard error of the mean
- SMBS:
-
sodium metabisulfite
- Tmax :
-
time to reach maximum plasma concentration
- USDA:
-
United States Department of Agriculture
- USP:
-
United States Pharmacopeia
References
Lieberman P, Nicklas RA, Randolph C, Oppenheimer J, Bernstein D, Bernstein J, et al. Anaphylaxis--a practice parameter update 2015. Ann Allergy Asthma Immunol. 2015;115(5):341–84.
Sampson HA, Munoz-Furlong A, Campbell RL, Adkinson NF Jr, Bock SA, Branum A, et al. Second symposium on the definition and management of anaphylaxis: summary report--second National Institute of allergy and infectious disease/Food Allergy and Anaphylaxis Network symposium. Ann Emerg Med. 2006;47(4):373–80.
Simons FE, Ebisawa M, Sanchez-Borges M, Thong BY, Worm M, Tanno LK, et al. 2015 update of the evidence base: world allergy organization anaphylaxis guidelines. World Allergy Organ J. 2015;8(1):32.
Taylor BN, Cassagnol M. Alpha adrenergic receptors. StatPearls: Treasure Island, FL; 2019.
Sicherer SH, FER S. Section on Allergy and Immunology. Epinephrine for first-aid management of anaphylaxis. Pediatrics. 2017;139(3):e20164006.
Bellanti JA, Settipane RA. Quality of life issues ranging from the burden of ocular and nasal allergies to the anxiety associated with having to carry self-injectable epinephrine for insect sting allergy. Allergy Asthma Proc. 2014;35(3):195–6.
Turner PJ, DunnGalvin A, Hourihane JO. The emperor has no symptoms: the risks of a blanket approach to using epinephrine autoinjectors for all allergic reactions. J Allergy Clin Immunol Pract. 2016;4(6):1143–6.
Ku MS. Recent trends in specialty pharma business model. J Food Drug Anal. 2015;23(4):595–608.
Posner LS, Camargo CA Jr. Update on the usage and safety of epinephrine auto-injectors, 2017. Drug Healthc Patient Saf. 2017;9:9–18.
Erdo F, Bors LA, Farkas D, Bajza A, Gizurarson S. Evaluation of intranasal delivery route of drug administration for brain targeting. Brain Res Bull. 2018;143:155–70.
Pires A, Fortuna A, Alves G, Falcao A. Intranasal drug delivery: how, why and what for? J Pharm Pharm Sci. 2009;12(3):288–311.
Pieper L, Wager J, Zernikow B. Intranasal fentanyl for respiratory distress in children and adolescents with life-limiting conditions. BMC Palliat Care. 2018;17(1):106.
Webster LR, Pantaleon C, Iverson M, Smith MD, Kinzler ER, Aigner S. Intranasal pharmacokinetics of morphine ARER, a novel abuse-deterrent formulation: results from a randomized, double-blind, four-way crossover study in nondependent, opioid-experienced subjects. Pain Res Manag. 2018;2018:7276021.
Kerr D, Kelly AM, Dietze P, Jolley D, Barger B. Randomized controlled trial comparing the effectiveness and safety of intranasal and intramuscular naloxone for the treatment of suspected heroin overdose. Addiction. 2009;104(12):2067–74.
McDonald R, Lorch U, Woodward J, Bosse B, Dooner H, Mundin G, et al. Pharmacokinetics of concentrated naloxone nasal spray for opioid overdose reversal: phase I healthy volunteer study. Addiction. 2018;113(3):484–93.
Robinson A, Wermeling DP. Intranasal naloxone administration for treatment of opioid overdose. Am J Health Syst Pharm. 2014;71(24):2129–35.
Al Harthi S, Alavi SE, Radwan MA, El Khatib MM, AlSarra IA. Nasal delivery of donepezil HCl-loaded hydrogels for the treatment of Alzheimer's disease. Sci Rep. 2019;9(1):9563.
Krieter P, Gyaw S, Crystal R, Skolnick P. Fighting fire with fire: development of intranasal nalmefene to treat synthetic opioid overdose. J Pharmacol Exp Ther. 2019;371:409–15.
Seaquist ER, Dulude H, Zhang XM, Rabasa-Lhoret R, Tsoukas GM, Conway JR, et al. Prospective study evaluating the use of nasal glucagon for the treatment of moderate to severe hypoglycaemia in adults with type 1 diabetes in a real-world setting. Diabetes Obes Metab. 2018;20(5):1316–20.
Berg AK, Myrvik MJ, Van Ess PJ. Pharmacokinetics, pharmacodynamics, and tolerability of USL261, midazolam nasal spray: Randomized study in healthy geriatric and non-geriatric adults. Epilepsy Behav. 2017;71(Pt A):51–9.
Anderson GM, Dover MA, Yang BP, Holahan JM, Shaywitz SE, Marchione KE, et al. Adrenomedullary function during cognitive testing in attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2000;39(5):635–43.
Ohno I. Neuropsychiatry phenotype in asthma: psychological stress-induced alterations of the neuroendocrine-immune system in allergic airway inflammation. Allergol Int. 2017;66S:S2–8.
Bastos DB, Sarafim-Silva BAM, Sundefeld M, Ribeiro AA, Brandao JDP, Biasoli ER, et al. Circulating catecholamines are associated with biobehavioral factors and anxiety symptoms in head and neck cancer patients. PLoS One. 2018;13(8):e0202515.
Miyasaka T, Dobashi-Okuyama K, Takahashi T, Takayanagi M, Ohno I. The interplay between neuroendocrine activity and psychological stress-induced exacerbation of allergic asthma. Allergol Int. 2018;67(1):32–42.
Ganger S, Schindowski K. Tailoring formulations for intranasal nose-to-brain delivery: a review on architecture, physico-chemical characteristics and mucociliary clearance of the nasal olfactory mucosa. Pharmaceutics. 2018;10(3).
Djupesland PG. Nasal drug delivery devices: characteristics and performance in a clinical perspective-a review. Drug Deliv Transl Res. 2013;3(1):42–62.
Dretchen KL, Mesa Z, Robben M, Slade D, Hill S, Croutch C, et al. Intranasal epinephrine in dogs: Pharmacokinetic and heart rate effects. Pharmacology Research & Perspectives. 2020;e00587.
Committee for the Update of the Guide for the Care and Use of Laboratory Animals, Institute for Laboratory Animal Research, Division on Earth and Life Studies, National Research Council of the National Academies. Guide for the care and use of laboratory animals, 8th edition. Washington, DC: National Academic Press; 2011.
US Food and Drug Administration. Good Laboratory Practice for Nonclinical Laboratory Studies, 21 CFR Part 58 [Available from: http://academy.gmp-compliance.org/guidemgr/files/CFR_2018/CFR-2018-TITLE21-VOL1-PART58.PDF].
Bailey AM, Baum RA, Horn K, Lewis T, Morizio K, Schultz A, et al. Review of intranasally administered medications for use in the emergency department. J Emerg Med. 2017;53(1):38–48.
Corrigan M, Wilson SS, Hampton J. Safety and efficacy of intranasally administered medications in the emergency department and prehospital settings. Am J Health Syst Pharm. 2015;72(18):1544–54.
Cooper GM. The cell: a molecular approach. 2nd edition. Sunderland, MA: Sinauer Associates; 2000.
Kostrzewa RM. The blood-brain barrier for catecholamines - revisited. Neurotox Res. 2007;11(3–4):261–71.
Hummel T, Livermore A. Intranasal chemosensory function of the trigeminal nerve and aspects of its relation to olfaction. Int Arch Occup Environ Health. 2002;75(5):305–13.
Bleske BE, Rice TL, Warren EW, Giacherio DA, Gilligan LJ, Massey KD, et al. Effect of dose on the nasal absorption of epinephrine during cardiopulmonary resuscitation. Am J Emerg Med. 1996;14(2):133–8.
Bleske BE, Warren EW, Rice TL, Shea MJ, Amidon G, Knight P. Comparison of intravenous and intranasal administration of epinephrine during CPR in a canine model. Ann Emerg Med. 1992;21(9):1125–30.
Srisawat C, Nakponetong K, Benjasupattananun P, Suratannon C, Wachirutmanggur L, Boonchoo S, et al. A preliminary study of intranasal epinephrine administration as a potential route for anaphylaxis treatment. Asian Pac J Allergy Immunol. 2016;34(1):38–43.
Brown JC, Tuuri RE, Akhter S, Guerra LD, Goodman IS, Myers SR, et al. Lacerations and embedded needles caused by epinephrine autoinjector use in children. Ann Emerg Med. 2016;67(3):307–15 e8.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dretchen, K.L., Mesa, Z., Robben, M. et al. Effects of Intranasal Epinephrine on Cerebrospinal Fluid Epinephrine Pharmacokinetics, Nasal Mucosa, Plasma Epinephrine Pharmacokinetics, and Cardiovascular Changes. Pharm Res 37, 103 (2020). https://doi.org/10.1007/s11095-020-02829-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-020-02829-5