ABSTRACT
Purpose
The main aim of present study was to prepare the oxaliplatin (OXL)-loaded D-α-Tocopherol polyethylene glycol 1000 succinate (TPGS)-based lipid nanoparticles to enhance the anticancer effect in colon cancer cells.
Methods
The nanoparticles were nanosized and spherical shaped and exhibited controlled release kinetics. Flow cytometer and confocal laser scanning microscopy (CLSM) showed a remarkable uptake of nanoparticles in cancer cells in a time-dependent manner.
Results
The presence of TPGS remarkably increased the anticancer effect of OXL in HT-29 colon cancer cells. The IC50 value of free OXL was 4.25 μg/ml whereas IC50 value of OXL-loaded TPGS-based lipid nanoparticles (OXL/TLNP) was 1.12 μg/ml. The 3-fold lower IC50 value of OXL/TLNP indicates the superior anticancer effect of nanoparticle-based OXL. Consistently, OXL/TLNP induced a remarkable apoptosis of cancer cells. Approximately, ~52% of cells were in early apoptosis phase and ~13% of cells were in late apoptosis phase indicating the potent anticancer effect of the formulations. The findings from this study provide novel insights into the use of TPGS and lipid nanoparticle together for the better antitumor effect in colon cancers. Future studies will involve the detailed in vitro and in vivo studies on clinically relevant animals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Cancer is one of the deadliest diseases with high rate of mortality and mortality across the world with an estimated 15 million new cases diagnosed every year (1). According to world health organization (WHO), number of cancer cases will increase 70% from around 15 million to 23 million in next two decades. Among all the cancers, colorectal cancers accounts for nearly 700,000 deaths every year (2,3). The rate of death due to colorectal cancers kept increasing year by year. Chemotherapy is mainstay therapy in the clinics however little success was achieved despite the significant advancement in the biology and technology (4,5). There is a need to properly choose the anticancer drug and target it to the colon cancers with maximum efficacy.
Oxaliplatin ((cis-[(1R,2R)-1,2-cyclohexanediamine-N,N′] [oxalato(2)-O,O′] platinum, OXA) is a third generation platinum based anticancer therapeutics has been indicated in the treatment of colon cancers (6,7). The OXL acts by interfering with the DNA replication machinery and forms the DNA adducts. The Pt-DNA adducts will induce the apoptosis pathways in cancer cells (8). The OXL has been combine with 5-fluorouracil as a first line therapy for colon cancer and moreover USFDA has approved OXL combination with 5-fluorouracil and leucovorin as a standard therapy for metastatic colon cancer (9,10). Despite its potent anticancer effect, OXL produce severe toxic effects in the body including peripheral neuropathy, low blood counts and nausea and so on (11). Therefore effective strategies need to be designed to improve the anticancer effect of OXL while minimizing its toxic effect in the body.
Among the different carriers, lipid nanoparticles has gained significant attentions of researchers worldwide due to several interesting features including excellent biocompatibility, excellent biodegradability, long blood circulation, immunogenic, high drug loading capacity, surface modification properties, passive cancer targeting ability by enhanced permeation and retention (EPR) effect and non-toxic to body tissues (12,13,14,15). The lipid nanoparticles could be surface modified with polyethylene glycol (PEG) to increase the blood circulation properties. These lipid nanoparticles possess highly hydrophobic core and drug can be stably incorporated in the core and presents excellent colloidal stability in the systemic environment (16,17,18). In the present study, we have employed d-α-tocopheryl polyethylene glycol 1000 succinate (TPGS) as an additional component. TPGS could be used as an emulsifier, solubility enhancer in lipid nanoparticles (19). Importantly, TPGS has been reported to inhibit the p-glycoprotein (p-gp) efflux pumps and effectively overcome the multidrug resistance (MDR) in the cancer cells (20). Recently, TPGS was combined with PLGA NP to enhance the anticancer effect in multidrug resistant cancers (21). Based on all this facts, we expected that when we combine the TPGS as a structural component in the lipid nanoparticles, it will enhance the anticancer effect of OXL which is incorporated in the lipid nanoparticles.
In the present study, OXL-loaded TPGS combined lipid nanoparticle was prepared to improve the anticancer efficacy in colon cancers. We hypothesized that combination of TPGS in the lipid system will enhance or synergize the anticancer effect of OXL in the nanoparticle system. We have performed several studies demonstrating the synergistic effect of TPGS along with OXL. Overall, we expected that the present OXL-loaded lipid nanoparticle will be great addition in the nanomedicine strategy towards colon cancer treatment.
MATERIALS AND METHODS
Materials
Suppocire NB was donated by Gattefossé (Saint Priest, France). Lipoïd s75 (soybean lecithin at >75% phosphatidylcholine) is purchased from Lipoid GmbH (Ludwigshafen, Germany). Myrj s40 (PEGylated stearate) and soybean oil was obtained from Croda Uniqema (France). Oxaliplatin and d-α-tocopheryl polyethylene glycol 1000 succinate (TPGS) were purchased from Sigma-Aldrich. All other chemicals were of reagent grade and used without further modifications.
Preparation of OXL-Loaded Lipid Nanoparticles
The lipid nanoparticle was prepared by hot homogenization method. The lipid nanoparticle comprised of a lipid core which has phospholipid and surrounded by PEGylated surface. The lipid phase and aqueous phase were separately prepared. All the lipids, oils, TPGS, and OXL were mixed together and heated at above 70°C and kept at molten state. On the other side, Myrj s40 was dissolved in 10 ml of water and heated to the same temperature. The surfactant phase was added to the lipid phase and immediately homogenized (13,000 rpm for 5 min) and followed by subjected to probe sonication (80 W) for 5 min. The formulations were cooled and we can clearly see the dispersion. The free OXL was removed by dialysis against large volume of distilled water using dialysis membrane (MW-3500 Da) for 24 h. The drug-loaded NP was stored in refrigerator until further use. The amount of drug loaded in the nanoparticle was calculated by HPLC method. The HPLC system (LC-20 AD model, Shimadzu, Kyoto, Japan) consisted of two pumps (LC 20-AT model), an automatic injector (9SIL-20 AD model), an oven (CTO-20AS model), a spectrophotometric detector (SPD-M20A model), and a computer equipped with the analysis software Shimadzu LC. A reverse-phase C18 column (150 mm × 4.6 mm, 5 μm) was used. The mobile phae consisted of methanol: ACN (75: 25 v/v) and the flow rate maintained at 1 ml/min. The detection wavelength was set at 245 nm. The validation parameters includes; linearity – 0.025-2 μg/ml, slope (238 ± 1.6), %RSD (0.95), Correlation coefficient (r2) (0.9995 ± 0.012), LOD – 0.050 μg/ml and LOQ – 0.152 μg/ml, respectively.
Particle Size Analysis
The particle size was measured using dynamic light scattering (DLS) method using (Zetasizer Nano ZS, Malvern Instruments. At least 3 measurements were performed for individual formulations. The formulations were diluted adequately and measured at 25°C.
Transmission Electron Microscopic (TEM) Imaging
The morphology of nanoparticle was evaluated using transmission electron microscope (TEM) JEOL 1010 microscope operated at 100 kV. The formulations were adequately diluted and placed a drop in the carbon coated copper grid. The sample was allowed to dry and negatively stained with phosphotungistic acid (PTA). The samples were then dried well before observing by TEM.
In vitro Drug Release Study
The in vitro release study was performed by dialysis method. Briefly, 1 ml of formulations containing 1 mg of equivalent drug was transferred to a dialysis bag (MW~3500 Da) and both ends were sealed. The sealed dialysis bag was placed in a 30 ml of release buffer (PBS, pH 7.4 and ABS, pH 5.0) in a closed tube and the entire assembly was placed in a shaker bath operating at 100 rpm at 37°C. Attention should be paid in the packing of formulations in the dialysis bag and the shaker bath. 1 ml of release buffer was withdrawn at each pre-determined time interval (1,2,4,8,12,24,36,48,60, and 72 h). The sample was replaced with equal amount of fresh buffer and the process was continued until the end of the study period. The sample was filtered using 0.45 μm filter and subjected to HPLC analysis to determine the amount of drug released at each time interval.
Cellular Uptake Analysis
The HT29 colon cancer cells were cultured and kept in ambient conditions of incubator until further analysis. The cellular uptake was first evaluated by confocal laser scanning microscope (CLSM). The 6-well plate was covered with a cover slip and 1 ml of media was added to the each well of the 6-well plate. The cells in a density of 2 × 105 cells/well was seeded to the each well and allowed to attach for 24 h. Next day, cells were treated with TLNP and incubated for 2 h. The TLNP was loaded with rhodamine B as a fluorescent dye to track its internalization in the cancer cells. The cells were then stained with lysotracker Green as a lysosome staining agent and incubated for 10 min. The cells were then washed two times and fixed with 4% paraformaldehyde solution for 20 min. The cells were then observed under CLSM microscope (Leica TCS SP5, Germany).
The cellular uptake was further evaluated by flow cytometer (FACS). The 6-well plate was added with 1 ml of media to the each well of the 6-well plate. The cells in a density of 2 × 105 cells/well was seeded to the each well and allowed to attach for 24 h. Next day, cells were treated with TLNP and incubated for 1 h and 3 h, respectively. After the required time, cells were washed two times carefully and cells were extracted and collected in a FACS tube. The volume was made up to 1 ml using PBS buffer. The cells were then analyzed using flow cytometer.
Cytotoxicity Assay
The HT-29 colon cancer cell was purchased from ATCC, USA. The cell was cultured in RPMI-1640 growth media supplemented with 10% of fetal bovine serum (FBS) and 100 U/mL penicillin and 100 g/mL streptomycin. The cells were maintained at the ambient conditions of incubator at 37°C. The cytotoxicity potential of free drugs and nanoparticles were evaluated by MTT assay. The cells when they are at logarithmic phase are harvested and seeded in a 96-well plate at a density of 105 cells/well. The cells were incubated for 24 h and then exposed with various concentrations of free drug and drug-loaded nanoparticles. The incubation was kept for additional 24 h. The media was carefully removed and replaced with fresh buffer containing MTT powder. The MTT solution was prepared in serum-free media and incubated for 4 h. The final concentration of MTT in each well was 125 μg/ml. The cells were treated with DMSO to extract the formazan salt and shaken in a shaker for 15 min. The absorbance of each well was measured by a plate-reader at 570 nm. The dose-response curve was made from the absorption values. IC50 value of individual formulation was analyzed by GraphPad Prism software.
Annexin V/PI-Based Apoptosis Assay
The apoptosis inducing ability of chemotherapeutic agent was determined by Annexin V/PI based assay which is analyzed by flow cytometer. Briefly, 1 × 106 cells were seeded in a 6-well plate and incubated for 24 h. The cells were treated with blank NP, free OXL, TLNP, and OXL/TLNP and incubated for 24 h. Next day, cells were extracted using trypsinization and cells were washed two times with PBS buffer. The cells were stained with annexin V-FITC and PI for 15 min at room temperature and analyzed using flow cytometry using a FACS CaliburTM instrument (BD Biosciences). The software will locate the percentage of cells in each quadrant.
Hoechst 33342 Staining
The apoptosis was further confirmed by Hoechst 33342 which is a nuclear staining dye. Briefly, 1 × 106 cells were seeded in a 6-well plate and incubated for 24 h. The cells were treated with blank NP, free OXL, TLNP, and OXL/TLNP and incubated for 24 h. The cells were washed two times and fixed with 4% paraformaldehyde (PFA) for 20 min. The cells were washed again and incubated with 10 μg/ml of Hoechst 33342 staining dye. The images were then captured by fluorescent microscope (Olympus® 1X71, Japan).
Statistical Analysis
The statistical analysis was performed using student’s t-test method. *p < 0.05 was considered statistically significant factor. All experiments were performed in triplicate unless and otherwise mentioned in the reported method section.
RESULTS AND DISCUSSION
Oxaliplatin is a platinum based anticancer therapeutics indicated in the treatment of colon cancers. The OXL has been combine with 5-fluorouracil as a first line therapy for colon cancer and moreover USFDA has approved OXL combination with 5-fluorouracil and leucovorin as a standard therapy for metastatic colon cancer. Despite its potent anticancer effect, OXL produce severe toxic effects in the body including peripheral neuropathy, low blood counts and nausea and so on. In this study, therefore, we attempted to increase the anticancer effect of OXL by stably incorporating in a nanoparticle carrier. In addition, we have used TPGS as an additional component to enhance the cytotoxic potential of OXL in colon cancer cells (Fig. 1). Our objective was to enhance the therapeutic efficacy in colon cancer cells by incorporating in lipid nanoparticles.
Physicochemical Characterization of OXL-Loaded Lipid Nanoparticles
The OXL-loaded lipid nanoparticle was prepared by hot homogenization method. The nanoparticle internalization in cancer cell is one of the rate determining steps in the clinical efficacy. In this regard, physicochemical characteristics such as particle size and surface charge of particles play important role in the antitumor efficacy. In the present study, mean size of LNP was 126 ± 2.35 nm while the particle size slightly increased to 158 ± 3.15 nm after drug loading (Fig. 2a). The particles were monodispersed and the increase in the particle size after drug loading was attributed to the increase the hydrophobic core volume. A particle size around 150 nm is ideal for cancer targeting applications as it is ideal for cell penetration, prolonged blood circulation and escape from reticuloendothelial (RES) system (22). The overall surface charge was −11.5 ± 2.3 mV indicating that it will escape form the RES system due to the slight negative charge. It has been reported that lipid nanoparticles bear strong negative charge due to phospholipid molecules however in this case a slight charge was attributed to the surface PEGylation. The surface PEGylation affects the zeta potential of the particle.
The morphology of the particle was determined using transmission electron microscope (TEM) (Fig. 2b). As seen, particles were spherical shaped and dispersed uniformly on the copper grid. The particles were blacker on the core or center and slightly greyish on the border. It could be attributed to the surface PEGylation on the borders. The size of the particle measured by TEM was more or less equal as measured by DLS method.
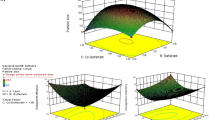
In vitro Drug Release
The OXL/TLNP showed a high entrapment efficiency of more than 95% with an active drug loading of 9.5 ± 1.65%w/w. The high drug loading was mainly attributed to the hydrophobic nature of the OXL. The high entrapment efficiency also means that all of the drug loaded in the hydrophobic core (Fig. 3). The in vitro drug release study was performed to evaluate or simulate the in vivo performance of the delivery system. Although, nanoparticle did not contain any pH-responsive component, nevertheless, we have checked the release of drugs in two different pH conditions in order to simulate tumor and physiological environment. The release study was performed by dialysis method and the study was continued for 72 h until 80% of the drug released. As seen, a controlled release pattern of the drug was observed at pH 7.4 and pH 5.0. Approximately, 35% of the drug was released by the end of 24 h indicating the controlled release kinetics. The release of drug continued until 72 h whereby almost 80% of the encapsulated drug released. It should be noted that no burst release of drug was observed indicating that all of the drug was stably incorporated in the core of the nanoparticles. Furthermore, it is also worth noting that no difference in drug release was observed in both the pH conditions indicating the lack of pH responsiveness. Mathematical modeling was carried out to investigate the kinetics of drug release. As seen, drug release very much correlated with Higuchi model at both the pH conditions indicating a more controlled mode of drug release from the nanoparticle system (Fig. S1). A controlled release of drug from lipid nanoparticle was mainly attributed to the highly hydrophobic nature of the nanoparticles. Although OXL is one of the main line drug for the treatment of colon cancers, the intravenous administration of OXL results in severe systemic adverse effects owing to distribution of the drug throughout the body via the bloodstream. Therefore, present nanoparticle system which releases the drug in a sustained manner is important to minimizing the adverse effects to normal tissues. A controlled and slow release of drug is beneficial for the cancer targeting applications (16).
Cellular Uptake Efficiency
The TLNP nanoparticle was loaded with rhodamine B as a fluorescent molecule to observe the cellular uptake efficiency of the carrier system. First, cellular uptake was observed by flow cytometer (FACS) (Fig. 4a). The cancer cells were incubated with TLNP for 1 h and 3 h respectively to observe a time-dependent cellular uptake. As seen, remarkable increase in the fluorescence intensity was observed after 1 h incubation. The fluorescence intensity further increased after 3 h incubation indicating a typical time-dependent cellular internalization. A time-dependent internalization means that nanoparticle will be gradually enters the cancer cells when incubated for long time.
The cellular uptake was further analyzed by CLSM experiment (Fig. 4b). The lysosome was stained with Lysotracker Green to track the nanoparticle presence in the lysosome. As seen, nanoparticles were seen internalized by the cancer cells by a typical endocytosis process. The particles were largely present in the lysosome indicating the endocytosis process and lack of any red fluorescence in the nucleus indicates that the drug is not released after 1 h incubation. A predominant presence of nanoparticle in cell cytoplasm indicates that the drug will be released and travel to the desired site of action in the intracellular environment (23).
In vitro Cytotoxicity
The in vitro cytotoxicity of individual formulation was determined by MTT assay. Prior to check to the cytotoxic potential of drug-loaded nanoparticles, cytotoxic potential of blank nanoparticle (devoid of TPGS) was evaluated (Fig. 5). As seen, blank nanoparticle did not show any cytotoxicity to the cancer cells even at higher concentration indicating its high non-toxic nature. The high biocompatibility of LNP was mainly attributed to the physiological lipids which were employed to prepare nanoparticles. On the contrary, treatment of free drug and drug-loaded formulations resulted in significant decrease in the cell viability. As seen, free OXL and OXL/TLNP showed a typical concentration-dependent cell killing effect in HT-29 cancer cells. IC50 value was calculated to quantitatively differentiate the free drug and drug-loaded nanoparticles. The IC50 value of free OXL was 4.25 μg/ml whereas IC50 value of OXL/TLNP was 1.12 μg/ml. The 3-fold lower IC50 value of OXL/TLNP indicates the superior anticancer effect of nanoparticle-based OXL. The possible reason for the higher anticancer effect of OXL/TLNP was due (a) nanoparticle encapsulation of OXL increased the solubility of free OXL (b) TPGS might increase the cellular uptake and might inhibited MDR by acting on the p-gp efflux pump (c) enhanced endocytosis-mediated cellular uptake might increase the intracellular concentration of the anticancer drugs which might increase the therapeutic efficacy in the cancer cells (24, 25).
Cellular Apoptosis Assay
The cell apoptosis potential of individual formulation was determined by Annexin V/PI-based staining assay. The cell which is undergoing apoptosis will flip phosphatidylserine (PS) from inner membrane to outer membrane and making it accessible to Annexin-V dye. The PI is a nuclear staining dye and detects the cell necrosis. Therefore, by using Annexin-V/PI kit, we can easily detect the different stages of cell apoptosis (Fig. 6). Flow cytometer will reveal the iea of 4 phenotypes; (a) viable cells (b) early apoptosis (c) late apoptosis and (d) necrosis. As seen, untreated cells largely remained in the viable chamber indicating the lack of any apoptosis action. Consistently, blank nanoparticle also did not induce any apoptosis of cancer cells and largely remained in the viable quadrant. The TNP (without OXL with TPGS) did induce certain early apoptosis of cancer cells however 90% of cell remained viable. The OXL induced a significantly higher apoptosis compared to that of blank NP and control. Approximately, `20% of cells was early apoptosis while ~3% of cells were in late apoptosis stage. Importantly, OXL/TLNP induced a remarkable apoptosis of cancer cells. Approximately, ~52% of cells were in early apoptosis phase and ~13% of cells were in late apoptosis phase indicating the potent anticancer effect of the formulations. The apoptosis assay further proved the synergistic action of TPGS and OXL and the fact that TPGS could potential increase the anticancer effect of the anticancer drug.
Hoechst 33342-Based Nuclear Staining
The apoptosis of cancer cell was further confirmed by Hoechst 33342-based nuclear staining. The cells were treated with respective formulations and incubated for 24 h. The cells were then stained with Hoechst 33342 staining dye. As seen, control and cells treated with blank NP were intact and the nuclei of these cells were in good conditions (Fig. 7). The OXL and OXL/TLNP treated cells however resulted in distorted morphology. The blebbing of nucleus and fragmentation of nucleus are the hallmark features of apoptotic cells. Hoechst staining measured the morphological changes and nuclear condensation. The study reveals that control cells were intact whereas OXL/TLNP treated cells resulted in remarkable condensation of nucleus and morphology changes. It is worth noting that during apoptosis process, DNA breaks into oligonucleotides. As said above, remarkable apoptosis effect of OXL/TLNP was mainly attributed to the synergistic effect of TPGS and OXL combined in a single nanoparticle system.
CONCLUSION
In summary, OXL-loaded TPGS-based lipid nanoparticles was prepared and observed to exhibit excellent anticancer effect in colon cancer cells. Remarkable uptake of nanoparticles in cancer cells was observed as shown by flow cytometer and CLSM. TPGS embedded in the nanoparticle remarkably increased the anticancer effect of OXL in HT-29 colon cancer cells. OXL/TLNP showed a 3-fold lower IC50 value compared to free drugs indicates the superior anticancer effect of nanoparticle-based OXL. OXL/TLNP induced a remarkable apoptosis of cancer cells as shown by the flow cytometer analysis with ~52% of cells early apoptosis and ~13% in late apoptosis phase. Present study provides novel insights into the use of TPGS and lipid nanoparticle together for the enhanced anticancer effect in colon cancers.
Abbreviations
- EPR:
-
Enhanced permeation and retention effect
- MDR:
-
Multidrug resistance
- NP:
-
Nanoparticles
- OXL:
-
Oxaliplatin
- OXL/TLNP:
-
OXL-loaded TLNP
- TLNP:
-
TPGS-embedded lipid nanoparticles
- TPGS:
-
d-α-tocopheryl polyethylene glycol 1000 succinate
REFERENCES
GLOBACON. Estimated Cancer incidence, mortality and prevalence worldwide in 2012. 2012. http://globocan.iarc.fr/Pages/ fact_sheets_cancer.aspx. Accessed 14 Feb 2015.
Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JM, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomized controlled trial. Lancet. 2010;375:1624–33.
Twelves C, Wong A, Nowacki MP, Burris H, Carrato A, Cassidy J, et al. Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med. 2005;352:2696e704.
Terzic J, Grivennikov S, Karin E, Karin M. Inflammation and colon cancer. Gastroenterology. 2010;138:2101e14. e5.
Haller DG, Tabernero J, Maroun J, de Braud F, Price T, Van Cutsem E, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol. 2011;29:1465e71.
Raymond E, Faivre S, Woynarowski JM, Chaney SG. Oxaliplatin: mechanism of action and antineoplastic activity. Semin Oncol. 1998;25:4–12.
Woynarowski JM, Chapman WG, Napier C, Herzig MC, Juniewicz P. Sequence- and region-specifcity of oxaliplatin adducts in naked andcellular DNA. Mol Pharmacol. 1998;54:770–7.
Raymond E, Faivre S, Chaney S, Woynarowski J, Cvitkovic E. Cellular and molecular pharmacology of oxaliplatin. Mol Cancer Ther. 2002;1:227–35.
Alian OM, Azmi AS, Mohammad RM. Network insights on oxaliplatinanti-cancer mechanisms. Clin Transl Med. 2012;1:26.
Giacchetti S, Perpoint B, Zidani R, et al. Phase III multicenter randomized trial of oxaliplatin added to chronomodulated fluorouracilleucovorin as frst-line treatment of metastatic colorectal cancer. J Clin Oncol. 2000;18:136–47.
André T, Boni C, Mounedji-Boudiaf L, et al. Multicenter International Study of Oxaliplatin/5-Fluorouracil/Leucovorin in the Adjuvant Treatment of Colon Cancer (MOSAIC) Investigators. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med. 2004;350:2343–51.
Maeda H. The enhanced permeability and retention (EPR) effect in tumor vasculature: the key role of tumor-selective macromolecular drug targeting. Adv Enzym Regul. 2001;41:189–207.
Fang J, Sawa T, Maeda H. Factors and mechanism of EPR effect and the enhanced antitumor effects of macromolecular drugs including SMANCS. Adv Exp Med Biol. 2003;519:29–49.
Swarnakar NK, Jain AK, Singh RP, Godugu C, Das M, Jain S. Oral bioavailability, therapeutic efficacy and reactive oxygen species scavengingproperties of coenzyme Q10-loaded polymeric nanoparticles. Biomaterials. 2011;32:6860–74.
Ramasamy T, Khandasami US, Ruttala H, Shanmugam S. Development of solid lipid nanoparticles enriched hydrogels for topical delivery of anti-fungal agent. Macromol Res. 2012;20:682–92.
Ramasamy T, Ruttala HB, Choi JY, et al. Engineering of a lipid-polymer nanoarchitectural platform for highly effective combination therapy of doxorubicin and irinotecan. Chem Commun. 2015;51:5758–61.
Tran TH, Ramasamy T, Truong DH, et al. Development of vorinostat-loaded solid lipid nanoparticles to enhance pharmacokinetics and efficacy against multidrug-resistant cancer cells. Pharm Res. 2014;31:1978–88.
Coimbra M, Isacchi B, van Bloois L, Torano JS, Ket A, Wu X, et al. Improving solubility and chemical stability of natural compounds for medicinal use by incorporation into liposomes. Int J Pharm. 2011;416:433–42.
Wang Y, Fan W, Dai X, et al. Enhanced tumor delivery of gemcitabine viaPEG-DSPE/TPGS mixed micelles. Mol Pharm. 2014;11:1140–50.
Dintaman JM, Silverman JA. Inhibition of P-glycoprotein by d-α- tocopheryl polyethylene glycol 1000 succinate (TPGS). Pharm Res. 1999;16:1550–6.
Zhang Z, Tan S, Feng SS. Vitamin E TPGS as a molecular biomaterialfor drug delivery. Biomaterials. 2012;33:4889–906.
Iversen TG, Skotland T, Sandvig K. Endocytosis and intracellular transport of nanoparticles: present knowledge and need for future studies. Nano Today. 2011;6:176–85.
Khalil IA, Kogure K, Akita H, Harashima H. Uptake pathways and subsequent intracellular trafficking in nonviral gene delivery. Pharmacol Rev. 2006;58:32–45.
Ramasamy T, Ruttala HB, Gupta B, Poudel BK, Choi HG, Yong CS, et al. Smart chemistry-based nanosized drug delivery systems for systemic applications: A comprehensive review. J Control Release. 2017;258:226–53.
Shen R, et al. Development and evaluation of vitamin e d-α-tocopheryl polyethylene glycol 1000 succinatemixed polymeric phospholipid micelles of berberine as an anticancer nanopharmaceutical. Int J Nanomedicine. 2016;11:1687–700.
ACKNOWLEDGMENTS AND DISCLOSURES
The study was funded from the research grant of Qilu Hospital of Shandong University, China.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1
(DOCX 125 kb)
Rights and permissions
About this article
Cite this article
Wang, Y., Zhang, X., Zhang, W. et al. Combination of Oxaliplatin and Vit.E-TPGS in Lipid Nanosystem for Enhanced Therapeutic Efficacy in Colon Cancers. Pharm Res 35, 27 (2018). https://doi.org/10.1007/s11095-017-2297-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-017-2297-x