Abstract
Purpose
At elevated temperatures, the rate of drug release and skin permeation from transdermal delivery systems (TDS) may be higher than at a normal skin temperature. The aim of this study was to compare the effect of heat on the transdermal delivery of two model drugs, nicotine and fentanyl, from matrix-type TDSs with different formulations, using in vitro permeation tests (IVPT).
Methods
IVPT experiments using pig skin were performed on two nicotine and three fentanyl TDSs. Both continuous and transient heat exposures were investigated by applying heat either for the maximum recommended TDS wear duration or for short duration.
Results
Continuous heat exposure for the two nicotine TDSs resulted in different effects, showing a prolonged heat effect for one product but not the other. The Jmax enhancement ratio due to the continuous heat effect was comparable between the two nicotine TDS, but significantly different (p < 0.05) among the three fentanyl TDSs. The Jmax enhancement ratios due to transient heat exposure were significantly different for the two nicotine TDSs, but not for the three fentanyl TDSs. Furthermore, the transient heat exposure affected the clearance of drug from the skin depot after TDS removal differently for two drugs, with fentanyl exhibiting a longer heat effect.
Conclusions
This exploratory work suggests that an IVPT study may be able to discriminate differences in transdermal drug delivery when different TDS are exposed to elevated temperatures. However, the clinical significance of IVPT heat effects studies should be further explored by conducting in vivo clinical studies with similar study designs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the approval of the first transdermal system by the United States Food and Drug Administration (FDA) in 1979, there have been numerous advances in the development and understanding of transdermal delivery systems (TDS) [1]. Many TDS products with drugs from diverse classes and utility in a variety of therapeutic areas are available on the market today. Generic drug products have also been developed for some TDS, referencing the innovator, or reference listed drug (RLD) product [1, 2]. However, most generic TDS differ in design, drug load and inactive ingredient composition relative to their corresponding RLD products; the formulation composition of generic TDS products is not required to be qualitatively (Q1) and quantitatively (Q2) the same compared to their respective RLD [3]. Additionally, some drugs such as nicotine have more than one innovator TDS product approved, which collectively results in substantial diversity in the product design and compositional characteristics among marketed TDS products.
In vitro and in vivo studies have shown that the drug release and skin permeation from TDS can be affected by many factors, including skin condition, skin type, humidity, temperature, inactive ingredients and product design [4,5,6,7,8,9,10]. Among these factors, temperature has received considerable attention from clinicians and regulatory authorities due to reports of life-threatening adverse events related to the off-label application of heat on fentanyl TDS [11,12,13,14,15]. There are many circumstances in which patients wearing a TDS can be exposed to elevated temperatures during the normal course of daily life, potentially from heating pads, tropical climates, strenuous exercise, saunas and fever. One case report involved a heating pad which accidently slipped directly over the fentanyl TDS on a hospitalized patient [14]. Since heating pad usage may be a part of routine nursing care for pain treatment, the risk of a TDS being in contact with a heating source exists even in hospital settings under supervision of healthcare professionals.
Several studies have looked at the effect of heat on various TDS, both in vitro and in vivo [5, 7,8,9, 16,17,18]. These studies demonstrated that when the skin temperature is higher than the normal physiological skin temperature of approximately 32°C, a higher amount of drug is released from the TDS in most cases, and more drug permeates into and across the skin to become systemically bioavailable. For a nicotine TDS, intermittent controlled heat (43°C) application over 30 min resulted in an approximately 9-fold increase in blood perfusion of the skin by the local vasculature and 13-fold increase in nicotine uptake in human subjects [8]. In addition, several other studies investigated the effect of heat on physiology of skin such as vasomotor response, which may explain the increased drug delivery and absorption due to heat. Gazerani and Arendt-Nielsen investigated cutaneous vasomotor reactions in response to heat application in healthy subjects [19]. They found that a single exposure to 43°C for 1 min resulted in a 2-fold increase in perfusion of the skin by the local vasculature and 5°C increase in skin temperature, with its effect lasting for 15 min after the heat stimulus was terminated [19].
Given the potential risks of overdose and other medication errors associated with the effects of heat on TDS products dosed in vivo, it was of interest to develop a system to characterize these heat effects in vitro. One component of the research strategy was to evaluate the effect of controlled heat on a set of drug-in-adhesive matrix TDS products. Although each of the TDS products selected for nicotine or fentanyl has different construction designs and formulation components, they are expected to deliver the same nominal dose based upon their labeled strengths over the same period of time, under labeled use conditions. However, there was a possibility that these TDS might not continue to perform in a similar manner under controlled conditions of exposure to elevated temperature due to the differences in construction and formulation. There have been no other studies reported in the literature in which the effects of controlled heat application were compared for multiple, differently formulated, matrix-type TDS. Although Moore et al. and Prodduturi et al. have studied the influence of heat on two different fentanyl products, their focus was to compare the reservoir- and matrix-types of TDS [7, 9].
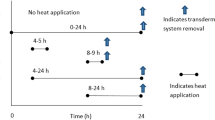
The main objective of the current study was to use an in vitro permeation test (IVPT) method to evaluate the change/increase in drug delivery caused by exposure to an elevated temperature among matrix-type TDS products (with formulation differences e.g., different adhesives). Nicotine and fentanyl TDS were chosen as model drugs because they are widely used in the United States and multiple TDS products with distinct formulations and system characteristics are available from different manufacturers (Tables I and II) for both molecules. Using the selected products, a series of proof-of-concept experiments were performed to optimize the in vitro setup and to understand the effects of heat on the drug delivery from these TDS. A typical heat exposure was mimicked in vitro by increasing the skin surface temperature to 42 ± 2°C [14]. The first set of experiments was conducted to evaluate whether differently formulated TDS deliver drug differently under long-term, continuous heat exposure (Fig. 1, Continuous Heat), compared to the normal temperature condition (Fig. 1, No Heat I). The second set of experiments was conducted to evaluate how short-term heat exposure at different time periods post-application would affect the skin permeation profiles of the drugs delivered by the TDS (Fig. 1, Early Heat and Late Heat) and to compare the results to those observed under normal temperature condition (Fig. 1, No Heat II). Finally, the third set of experiments was conducted to examine the effect of short-term heat exposure on drug release from the skin after TDS removal.
Materials and Methods
Materials
Nicotine TDS, 14 mg/24 h strength, NicoDerm CQ® (lot # EG022, exp. 05/2015) and Aveva (lot # 41302, exp. 05/2015), were purchased from Amazon.com, Inc. (Seattle, WA). Fentanyl TDS, 25 μg/h strength, Duragesic® (lot # 1304822, exp. 08/2015), Mylan (lot # 6E0194, exp. 01/2016) and Apotex (lot # 41863, exp. 11/2016) were purchased through the Department of Pharmacy Services at the University of Maryland Medical Center (Baltimore, MD). L-Nicotine (99 + %, Acros Organics), sodium chloride, methanol, acetonitrile, trimethylamine, perchloric acid and ethanol were purchased from Fisher Scientific Inc. (Fair Lawn, NJ). Fentanyl citrate salt (98 + %) was purchased from Sigma-Aldrich (St. Louis, MO). All reagents were of analytical grade or better. Nanopure water was obtained using a Milli-Q system (EMD Millipore; Billerica, MA).
Skin Preparation
Full thickness Yucatan miniature pig skin used for in vitro experiments was either harvested as approved by the University of Maryland, Baltimore Institutional Animal Care and Use Committee (IACUC) or purchased from Sinclair Bio Resources, LLC. (Auxvasse, MO). The skin was dermatomed to a thickness of 250 ± 50 μm, removing subcutaneous fat and keeping the outer layers of skin containing stratum corneum, viable epidermis and some dermis. The dermatomed skin was covered in aluminum foil, sealed in a plastic bag and stored at −20°C. On the day of the experiment, skin was cut into a 4.84 cm2 square to fit onto the diffusion cell and thawed for at least 30 min prior to use. A transepidermal water loss (TEWL) measurement was obtained using a cyberDerm RG-1 open chamber evaporimeter (cyberDERM, Inc.; Broomall, PA) to validate skin integrity for each skin piece prior to use in the skin permeation study. Skin pieces were excluded from the experiment if the TEWL value was higher than 15.0 g/m2·h. IVPT studies were conducted with skin from one porcine skin donor with 3–4 replicates per each study condition/product.
in Vitro Permeation Test (IVPT)
A PermeGear® flow-through In-Line diffusion system (Hellertown, PA) with a permeation area of 0.95 cm2 was used for IVPT experiments. Diffusion cells with membrane supports (PermeGear®) were utilized to prevent the skin from sinking into the receptor chamber due to the weight of the TDS. The receiver solution was 0.9% saline; 5% ethanol was added to the saline solution for the 72 h fentanyl experiments. The flow of the receptor solution was set to 7 rpm (5.70 ± 0.89 mL/h) for nicotine and to 1 rpm for fentanyl (0.82 ± 0.14 mL/h) experiments. The 4.84 cm2 square piece of skin was arranged in the diffusion cell with epidermis facing the donor compartment. Immediately before the experiment, TDS were cut into circular discs with an area of 0.95 cm2 to match the permeation area of the skin in the diffusion cell, and applied on top of the skin. Adhesion of the disc to the skin was ensured by gently rubbing the disc onto the skin surface using the flat bottom surface of a typical HPLC (high-performance liquid chromatography) vial three times. A 4.84 cm2 square piece of polypropylene knitted (non-occlusive) mesh (0.15 mm monofilament, 3.0 x 2.8 mm pores, 47 GSM; SurgicalMesh™ Division of Textile Development Associates, Inc.) was used to cover the skin membrane and TDS disc to prevent lifting of the disc during the experiment. Diffusion samples were collected into scintillation vials at predetermined time points using the fraction collector. All samples were analyzed by HPLC.
IVPT Experimental Designs
The IVPT experiments were performed in five different experimental designs for nicotine and fentanyl TDS (Fig. 1). In No Heat I and Continuous Heat designs, nicotine and fentanyl TDS were studied at normal (32 ± 1°C) and elevated (42 ± 2°C) skin surface temperatures respectively for the entire duration of the in vitro experiment: 24 h for nicotine (period of wear) and 72 h for fentanyl (period of wear). In Early Heat and Late Heat designs, skin was exposed to heat for a short duration (1 h for nicotine and 2 h for fentanyl) at different time points during the course of TDS application (4–5 h or 8–9 h for nicotine; 10–12 h or 17–19 h for fentanyl). The total time duration of No Heat II design for nicotine and fentanyl (Fig. 1) was the same as Early Heat and Late Heat designs for the respective drug, except that the skin surface was maintained at a normal temperature (32 ± 1°) without heat exposure. For Early Heat, Late Heat and No Heat II experimental designs in Fig. 1, IVPT samples were collected for three additional hours after TDS removal. For fentanyl TDS, an additional experiment (Early Heat-Extended, Late Heat-Extended, and No Heat II-Extended) was performed in which the permeation rate after TDS removal was investigated for up to 7 h following TDS removal, with 2 h of temporary heat application at different time points for Early Heat-Extended and Late Heat-Extended.
Temperature Control and Monitoring
A circulating water bath was used to modulate the temperature of the diffusion cells and thereby the temperature of the skin surface. For baseline control IVPT (No Heat I and No Heat II), the skin temperature was maintained at 32 ± 1°C to mimic normal in vivo skin temperature. A typical heat exposure scenario was simulated by heating the skin surface to 42 ± 2°C in Continuous Heat, Early Heat and Late Heat designs. For Early Heat and Late Heat designs where heat was applied for a short duration during the IVPT experiment, water inside the water bath was replaced with pre-heated water to facilitate a quick heating process. Likewise, ice was used to facilitate the cooling process and bring down the temperature. Surface temperature at the top of the TDS was monitored using an Oakton™ FEB insulated probe connected to a Temp 10 Type J thermocouple thermometer and/or a traceable® infrared thermometer. Separate testing was done to ensure no significant differences existed between the skin surface and the TDS surface temperatures. Apotex fentanyl TDS’s backing layer contains aluminum, and was the only product tested that showed lower TDS surface temperature compared to the skin temperature. Since a single water bath is used to control the temperature of all diffusion cells simultaneously, diffusion cells dosed with Apotex fentanyl TDS were excluded in determining the temperature setting to meet the target temperatures. The average time to reach the target temperature of 42 ± 2°C upon exposure to heat was 9.7 ± 2.4 min. The average time to reach the target temperature of 32 ± 1°C following heat exposure was 7.3 ± 0.5 min for experiments with the nicotine TDS (after 1 h of heat) and 16.7 ± 2.9 min for experiments with the fentanyl TDS (after 2 h of heat).
HPLC Analysis of IVPT Samples
The HPLC system consisted of a Waters® Alliance e2695 separations module and a Waters® 2489 dual-wavelength absorbance detector with Waters Empower™ software (Milford, MA). All IVPT samples and standards were injected in duplicate.
For nicotine IVPT samples, a Perkin Elmer Brownlee™ Spheri 5 VL C18 column (5 μm, 220 x 4.6 mm) with Brownlee™ NewGuard RP18 Aquapore ODS guard column (7 μm, 15 x 3.2 mm) was used to quantify nicotine at 260 nm. The mobile phase used was 80:20 (v/v) methanol:30 mM ammonium acetate, pH adjusted to 8.5 with triethylamine. The flow rate of the mobile phase was 1.2 mL/min. Nicotine IVPT samples were diluted with acetonitrile (1:1, v/v) prior to HPLC analysis. Standards were prepared in 0.9% saline: acetonitrile (1:1, v/v) and analyzed with each set of IVPT samples. Injection volume was 50 μL and the retention time was 3.99 ± 0.10 min. The concentration of nicotine standards ranged from 0.05 to 50 μg/mL and the precision for each concentration level, including lower limit of quantification (LLOQ), was within 15% of the nominal value. The limit of detection (LOD) and LLOQ of nicotine were 0.03 and 0.05 μg/mL, respectively.
For fentanyl IVPT samples, a Waters® Symmetry™ C18 column (3.5 μm, 4.6 x 75 mm) with a Phenomenex® SecurityGuard™ C18 cartridge (5 μm, 4 x 3.0 mm) was used to quantify fentanyl at 210 nm. The mobile phase was 35:65 (v/v) acetonitrile:10 mM sodium 1-heptanesulfonate, pH adjusted to 2.5 with perchloric acid. The flow rate of the mobile phase was 1.0 mL/min. The fentanyl IVPT samples were directly injected onto the HPLC column. Standards were prepared in 0.9% saline with 5% ethanol and analyzed with each set of IVPT samples. Injection volume was 50 μL and the retention time was 3.34 ± 0.02 min. The concentration of fentanyl standards ranged from 0.03 to 15.91 μg/mL and the precision for each concentration level, including LLOQ, was within 15% of the respective nominal value. The LOD and LLOQ of fentanyl were 0.02 and 0.03 μg/mL, respectively.
Data Analysis and Statistical Analysis
When TDS products of the same model drug were compared, the resultant values from IVPT studies were corrected to account for the differences in TDS size between the systems. The corrected values are labeled with the symbol, +.
Statistical analysis of the data was performed using GraphPad Prism® software (version 6.01, La Jolla, CA). Data for all experiments are expressed as mean ± SD. An unpaired Student’s t-test and one-way ANOVA test followed by Tukey’s post-hoc multiple pairwise comparisons were used for the data analysis. Differences were considered to be statistically significant when p < 0.05.
Results
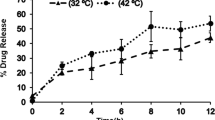
IVPT for Nicotine TDS
The first set of IVPT experiments was performed using two nicotine TDS (Table I) at two different temperatures for 24 h (the recommended maximum duration of TDS wear per the drug product label). At the normal physiological temperature of 32 ± 1°C (No Heat I in Fig. 1a), both TDS showed a controlled release of nicotine over 24 h (Fig. 2a). However, at the elevated temperature of 42 ± 2°C (Continuous Heat in Fig. 1a), the flux+ from one Nicotine TDS (comprised of a Polyisobutylene adhesive matrix) was much higher at the initial time point (2 h) relative to the flux+ from the other Nicotine TDS (comprised of a Polyacrylate/Silicone adhesive matrix), and continuously decreased thereafter. The maximum flux+ (Jmax +) at 42 ± 2°C was significantly higher compared to the Jmax + at 32 ± 1°C for both nicotine TDS (Fig. 2b). The difference in Jmax + between the normal and elevated temperature treatment groups was 2.5-fold for one Nicotine TDS (with Polyisobutylene) and 2.1-fold for the other Nicotine TDS (with Polyacrylate/Silicone) (Fig. 2b and Table III). There was an 8.9-fold difference in flux+ at the 2 h time point between the normal and elevated temperatures for the Nicotine TDS (with Polyisobutylene). The total amount of nicotine permeated, corrected for the size of the whole TDS, at two different temperatures was significantly different for both TDS (Fig. 2c) with a 2.2-fold increase for one Nicotine TDS (with Polyisobutylene) and a 1.6-fold increase for the other Nicotine TDS (with Polyacrylate/Silicone).
(a) Mean flux (± SD) profiles, (b) Jmax (± SD) and (c) the total amounts (± SD) of nicotine permeated over 24 h from two nicotine TDS at 32 ± 1°C (No Heat I) and 42 ± 2°C (Continuous Heat) (* p ≤ 0.05; ** p ≤ 0.01; *** p ≤ 0.001). (n = 3 replicates from the same donor). + Values corrected for TDS size.
Maximum nicotine flux+ during 1 h of heat exposure was significantly higher (p < 0.05) compared to the flux+ without heat exposure at the corresponding time point (No Heat II) for both TDS (Fig. 3a). This increase in flux+ was observed for both early and late heat exposures. The mean ratio of the increase in flux+ was significantly higher (p < 0.05) for the Nicotine TDS with Polyacrylate/Silicone compared to the Nicotine TDS with Polyisobutylene, during both early and late heat applications (Table III). Upon heat application from 4 h to 5 h for Early Heat design, there was a significant 1.6-fold increase in flux+ for both Nicotine TDS, compared to the flux+ before heat application (Fig. 3b). For Late Heat design, the increase of flux+ values from 8 h to 9 h was by 1.9- and 1.7-fold for Nicotine TDS (Polyisobutylene) and Nicotine TDS (Polyacrylate/Silicone), respectively (Fig. 3b). For Nicotine TDS (Polyisobutylene) under Early Heat design, flux+ at 6 h (after heat) was significantly higher (p < 0.05) than flux+ at 4 h (before heat), suggesting a prolonged heat effect (Fig. 3b). However, Nicotine TDS (Polyacrylate/Silicone) did not show such a prolonged effect at 6 h; the flux+ value returned to baseline quickly when the skin temperature returned back to normal, after 1 h of transient heat exposure (Fig. 3b). In Late Heat design where an additional variable is introduced by removing the TDS at the same time as the elevated temperature treatment is terminated, the flux+ for Nicotine TDS (Polyisobutylene) did not significantly decrease at 10 h (after heat and TDS removal) compared to 8 h (before heat), unlike the other product, Nicotine TDS (Polyacrylate/Silicone) (Fig. 3b). For Nicotine TDS (Polyisobutylene), no significant difference was observed in the total amount+ of nicotine permeated over 12 h from Early Heat, Late Heat and No Heat II designs (Fig. 4). For Nicotine TDS (Polyacrylate/Silicone), the total amount+ of nicotine permeated from Late Heat was significantly higher (p < 0.05) compared to the amounts+ from Early Heat and No Heat II.
(a) Mean flux (± SD) profiles of the two nicotine TDS over 12 h with early and late heat exposures (42 ± 2°C) for 1 h of duration compared to no heat exposure. TDS was removed after 9 h. The statistical significances were tested between flux value during 1 h of heat exposure and the flux value at the corresponding time point from No Heat II experiment (**** p ≤ 0.0001). (b) Mean flux (± SD) changes upon heat exposure for Early and Late Heat designs. The Before Heat, Heat and After Heat represent flux values at 4 h, 5 h and 6 h, respectively for Early Heat and 8 h, 9 h and 10 h, respectively for Late Heat. (** p ≤ 0.01; **** p ≤ 0.0001). (n = 4 replicates from the same donor). + Values corrected for TDS size.
The flux+ 1 h after TDS removal was significantly higher (p < 0.05) for Late Heat, compared to either Early Heat or No Heat II for both nicotine TDS (Fig. 5). For Nicotine TDS (Polyisobutylene), the flux+ was 1.7- and 1.3-fold higher when compared to Early Heat and No Heat II, respectively. For Nicotine TDS (Polyacrylate/Silicone), the flux+ was 2.0- and 1.5-fold higher when compared to Early Heat and No Heat, respectively. No significant difference (p > 0.05) of flux+ among the three experimental designs was found for the remaining time points.
IVPT for Fentanyl TDS
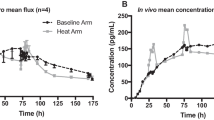
For the three fentanyl TDS studied (Table II), the IVPT study duration was 72 h, consistent with the recommended duration of TDS wear (No Heat I and Continuous Heat, Fig. 1b). The flux+ profiles from the three fentanyl TDS at a temperature of 32 ± 1°C showed a sustained flux+ of fentanyl through the skin over 72 h with similar flux+ values (Fig. 6a). At the elevated temperature of 42 ± 2°C, the initial flux+ values were higher for all three fentanyl TDS, but most notably for Fentanyl TDS (Polyacrylate) (Fig. 6a). Although the Jmax + at the elevated temperature was significantly (p < 0.05) higher for all of the three fentanyl TDS, Fentanyl TDS (Polyacrylate) exhibited a significantly higher heat enhancement ratio of Jmax +, compared to Fentanyl TDS (Silicone) and Fentanyl TDS (Polyisobutylene) (Fig. 6b, Table III). The total amounts+ of fentanyl permeated over 72 h were significantly higher (p < 0.05) at 42°C compared to the baseline temperature for all three fentanyl products, but most notably for Fentanyl TDS (Polyacrylate) at a 1.8-fold, compared to a 1.4-fold for Fentanyl TDS (Silicone) and a 1.3-fold for Fentanyl TDS (Polyisobutylene) (Fig. 6c).
During 2 h of heat exposure from both Early Heat and Late Heat designs, the flux+ values were higher compared to flux+ values without heat exposure (No Heat II) for all three fentanyl TDS (Fig. 7a). The increase in flux+ was approximately 2-fold, except for Fentanyl TDS (Polyisobutylene) that had the lowest increase in mean flux+ (1.5-fold) during Early Heat (Table III). Significant differences (p < 0.05) in flux+ values during heat application were observed only for Fentanyl TDS (Polyacrylate) and Fentanyl TDS (Polyisobutylene) from Late Heat design, compared to No Heat II design (Fig. 7a). However, there were no significant differences among the three fentanyl TDS in terms of heat enhancement ratios of flux+ during 2 h of early and late heat applications (Table III). When the flux+ values before, during and after the 2 h of transient heat exposure from Early Heat design were compared, no significant differences were found for the three fentanyl TDS (Fig. 7b). A significant difference (p < 0.05) in flux+ values was found for Fentanyl TDS (Polyacrylate) (2.0-fold) and Fentanyl TDS (Polyisobutylene) (1.8-fold) when heat was applied later (Late Heat) (Fig. 7b). In addition, Fentanyl TDS (Polyacrylate) and Fentanyl TDS (Silicone) did not show a significant decrease in flux+ after TDS and heat removal in Late Heat, unlike Fentanyl TDS (Polyisobutylene) (Fig. 7b). In terms of the total amounts+ of fentanyl permeated through skin over 22 h, the three fentanyl products did not show significant difference from the three designs (Early Heat, Late Heat and No Heat), despite the transient increases in flux+ due to heat exposures (Fig. 8).
(a) Mean flux (± SD) profiles of three fentanyl TDS over 22 h with early and late heat exposures (42 ± 2°C) for 2 h of duration compared to no heat exposure. TDS was removed after 19 h. The statistical significances were tested between flux value during 2 h of heat exposure and the flux value at the corresponding time point from No Heat II experiment (** p ≤ 0.01). (b) Mean flux (± SD) changes upon heat exposure for Early and Late Heat designs. The Before Heat, Heat and After Heat represent flux values at 10 h, 12 h and 14 h, respectively for Early Heat and 17 h, 19 h and 21 h, respectively for Late Heat. (* p ≤ 0.05; ** p ≤ 0.01; *** p ≤ 0.001). (n = 3–4 replicates from the same donor). + Values corrected for TDS size.
The flux+ after 1 h of TDS removal was significantly higher from Late Heat, compared to either Early Heat or No Heat II for all three fentanyl TDS (Fig. 9). Even after 2 h of TDS removal, a significant difference in flux+ was found between Late Heat and No Heat II for Fentanyl TDS (Polyacrylate) and Fentanyl TDS (Silicone). For Fentanyl TDS (Polyacrylate), significant differences in flux+ between Early Heat and No Heat II were found at 1 h and 2 h after TDS removal. Subsequently, the flux+ values from the Early Heat and Late Heat were higher than those from No Heat II up to 7 h after TDS removal for all three TDS, with significant differences (p < 0.05) found for most of the time points (Fig. 9).
Mean flux (± SD) after removal of fentanyl TDS from IVPT experiments with early (Early Heat-Extended), late (Late Heat-Extended) and no heat (No Heat II-Extended) exposures (* p ≤ 0.05; ** p ≤ 0.01; *** p ≤ 0.001; **** p ≤ 0.0001). (n = 3–4 replicates from the same donor). + Values corrected for TDS size.
Discussion
The present exploratory study indicated that the effect of heat on transdermal drug delivery from TDS of different designs and with different drugs can be discriminated and compared using an IVPT method. A significant influence of heat was observed when comparing the differently formulated TDS products with each of the two model drugs, nicotine and fentanyl. Using the IVPT model, it was possible to evaluate the effect of heat in vitro when heat was applied for the entire duration of the recommended TDS wear time, as well as when heat was applied for a short duration at different times.
It would be unusual for patients wearing TDS to be exposed to heat for the entire duration of TDS wear. Conceivably, it could happen that a patient wearing a nicotine TDS may sleep under a heated blanket for as long as 12 h, or that a patient wearing a fentanyl TDS may be outdoors in extreme heat for 3 days. However, these unusual situations were not the reason for the evaluation of the worst-case scenario of heat exposure. Rather, this approach was taken to evaluate the capabilities and/or limitations of the IVPT model as a sensitive method with which to evaluate differences in transdermal drug delivery under varied conditions of elevated heat – potentially even worst-case conditions. In addition, it was of interest to evaluate different study designs to gain insights into those heat exposure conditions that had the most discriminating influence on the drug delivery from different TDS; the prolonged depletion of the drug load at an elevated rate, due to heat, had the potential to impact later periods of drug delivery for different TDS differently.
The IVPT model has been widely used for several decades to characterize the permeation of compounds into and through the skin, and its advantages and limitations are well-understood [20,21,22]. For the current study, whose aim was to study heat effects on TDS using the IVPT model, there were several important experimental conditions to control and limitations to consider. For example, a non-occlusive mesh on top of the TDS disc was utilized to ensure adequate adhesion of the TDS on the skin in vitro throughout the experiment, and to mitigate the risk that the influence of the heat on the adhesion or surface contact of the TDS may introduce additional variables that might confound the interpretation of the results. A preliminary study (data not shown) indicated that without the mesh, IVPT results were considerably more variable at the elevated temperature compared to the baseline temperature, possibly due to heat disrupting TDS adhesion. In addition, replicating a typical in vivo heat exposure in vitro using the IVPT model was challenging.
The use of a water bath to modulate the temperature of the receptor solution beneath the skin, and to thereby modulate the temperatures at the skin surface and/or at the TDS surface, creates a heat gradient whereby it is warmer beneath the skin and cooler above the skin (in the ambient environment that is at room temperature). This is a relevant model for real-world scenarios involving an increase in core body temperature due to illness or strenuous exercise that can result in elevated temperatures at the surface of the skin and/or the TDS. In situations where the heat source is external (e.g., from a sauna or a heating blanket) the directionality of the heat gradient would be reversed. However, as long as the temperature is controlled at the skin surface, the actual temperatures at the rate-limiting stratum corneum and TDS are likely to be very similar in both scenarios, despite differences in the directionality of the gradient.
This water bath heating method provided adequate control of the skin surface temperature to modulate rapid and/or sustained temperature changes for the skin and the TDS, as verified by the measurement throughout the experiments of the skin surface and TDS surface temperatures, while in the diffusion cell setup. Additionally, the cooling process used for the IVPT study was very effective in decreasing the temperature rapidly to the baseline, following transient heat exposure periods (Early Heat and Late Heat designs). Further evaluation may be warranted to evaluate whether the rapid cooling method used in vitro is representative of the rate at which the skin and/or TDS surface temperatures changes in vivo after the exposure to an elevated temperature is terminated. The rate of cooling using this method could then be modulated appropriately.
The two nicotine TDS included in the current study have different adhesive types, along with other differences in product characteristics such as inactive ingredient composition, the size of the TDS and the expected drug delivery rate per unit area (Table I). Similarly, the three fentanyl TDS examined in this study each have distinctive characteristics (Table II). The varied magnitude of the resultant heat effects among differently formulated TDS observed in the current study indicated that TDS products containing the same active pharmaceutical ingredient and same nominal strength under conditions of labeled use could be affected differently by an increase in temperature. For example, change in the shape of flux+ profiles for Nicotine TDS (Polyisobutylene) was more pronounced compared to Nicotine TDS (Polyacrylate/Silicone), when heat was applied from the beginning of TDS application (Fig. 2a). The significantly higher (p < 0.05) flux+ at 42°C was continuously observed at every time point until the end of the 24 h experiment for Nicotine TDS (Polyisobutylene), whereas no significant differences in flux+ at two temperatures were found towards the end of the experiment for Nicotine TDS (Polyacrylate/Silicone). Also, the pronounced influence of 1 h transient heat lasted longer on Nicotine TDS (Polyisobutylene), taking a longer time for flux+ to return back to the baseline after heat, compared to Nicotine TDS (Polyacrylate/Silicone) in Early Heat (Fig. 3b). The Jmax + enhancement ratios due to 1 h, transient heat exposure on the two nicotine TDS were also significantly different, with a greater effect seen on Nicotine TDS (Polyacrylate/Silicone), compared to Nicotine TDS (Polyisobutylene) (Table III). While the two Nicotine TDS products were pharmaceutically equivalent, the Nicotine TDS (Polyacrylate/Silicone) is not a generic equivalent of the Nicotine TDS (Polyisobutylene) product and the two Nicotine TDS products were not necessarily designed to provide the same rate and extent of nicotine bioavailability under labeled use conditions (at skin surface temperature of approximately 32°C).
The effect of heat was also differentiated for the three fentanyl TDS, which are considered to be pharmaceutically equivalent, and the Fentanyl TDS (Silicone) and Fentanyl TDS (Polyisobutylene) are bioequivalent to Fentanyl TDS (Polyacrylate)). Among the three Fentanyl TDS, Fentanyl TDS (Polyacrylate) showed the most pronounced effect following continuous heat exposure with a significantly higher enhancement of Jmax + compared to the other two fentanyl TDS at 2.9-fold (Table III). However, it is beyond the scope of the current exploratory study (on skin from a single pig) to draw conclusions about the relative performance of the different TDS in vivo, and specifically in humans. Although the current results from the 3–4 replicates show relatively small standard deviations, a larger sample size with skin obtained from multiple donors would help to confirm the current findings related to the heat effects on TDS. The intention of this seminal exploratory study was to evaluate the potential of an IVPT model to evaluate differences in transdermal drug delivery at different temperatures (32°C vs. 42°C), and to be sensitive to distinctive responses to heat that may arise in situations where different TDS employ different formulation designs.
One potential consideration for the varied heat effects (i.e., varied increase in drug delivery) observed among the different matrix TDS that were evaluated is the physicochemical nature of the active pharmaceutical ingredient in the TDS. For example, the increase in flux+ upon transient exposure of the nicotine TDS to heat was significantly different for both Early Heat and Late Heat (Fig. 3b) relative to the baseline drug delivery at 32°C. However, such an increase was less evident for fentanyl TDS and the increase in flux+ relative to the baseline drug delivery at 32°C was not statistically significant for Early Heat, despite the longer duration (2 h vs. 1 h) of heat exposure for fentanyl (Fig. 7b). Also, significant differences in heat effect (based upon an assessment of the heat enhancement ratio relative to the baseline 32°C condition) were observed between the two nicotine TDS during the transient (1 h) heat exposure but not the continuous heat exposure (Table III). In contrast, significant differences among the three fentanyl TDS were observed only during continuous heat exposure, and not during the transient (2 h) heat exposure (Table III). Perhaps the physicochemical characteristics of nicotine (MW: 162.2 g/mol; log P: 1.2; melting point: −79°C), which has a more rapid permeation rate through skin compared to fentanyl (MW: 336.5 g/mol; log P: 4.1; melting point: 83–84°C), resulted in more rapid and distinct differences in response to heat exposure [2]. In addition, fentanyl may deposit in the upper skin layers and slowly diffuse from that depot into the deeper skin layers and beyond [23]. This skin depot might contribute to the effective lag in the heat effects on the permeation of fentanyl through the skin. Thus, it might be necessary to define the heat effect period for each drug molecule according to its rate of permeation and delay within skin layers when evaluating the effect of increased temperature on drug delivery and absorption from TDS.
Despite the significantly higher flux+ rate observed during heat exposure, relative to the baseline flux+, the total amount+ of fentanyl permeated over the entire duration of IVPT from Early Heat and Late Heat was not significantly different (p > 0.05) compared to the amount+ permeated from No Heat II without heat (Fig. 8). However, the amount+ of nicotine permeated from Nicotine TDS (Polyacrylate/Silicone) under Late Heat was significantly higher (p < 0.05) than the amount+ under either Early Heat and No Heat II (Fig. 4). It appeared that the difference for nicotine Late Heat arose predominantly from the anomalously higher flux+ observed for that set of replicate skin sections during the initial 4 h of the study (prior to any elevated temperature exposure, and therefore, unrelated to any heat effect) (Fig. 3a).
Overall, the finding from the current study related to the relatively minor impact of transient heat effects over the longer wear period of the TDS is consistent with the in vivo study results of Ashburn et al. That in vivo study demonstrated that no differences were observed in the mean area under the curve (AUC) of the concentration vs. time profile over 24 h between the two experimental scenarios: 4 h of heat exposure vs. no heat exposure [5]. It is not appropriate to conclude, however, that lack of a statistically significant difference in the total cumulative amount of drug permeated might indicate that there are no safety concerns associated with transient, significant increases in systemic concentrations of a drug. Rather, it is apparent that while a transient, significant difference begins to represent smaller proportions of an otherwise equivalent pharmacokinetic profile, the relative significance of that effect would be increasingly diluted until it becomes insignificant. That does not mean that the transient heat effect, somewhat analogous to “dose dumping”, may not be harmful, or even fatal. For drugs like nicotine and fentanyl, the peak drug level is often associated with serious adverse events, including respiratory depression and death for fentanyl, or heart arrhythmias for nicotine [24, 25].
The exploration of these study designs and analyses with the IVPT heat effect model suggests that rather than comparing the total amount of drug permeated between baseline conditions and a condition with transient heat exposure, a comparison of partial AUC and peak level may be more appropriate to evaluate the increase in drug delivery following exposure to elevated temperature conditions. The results of this study illustrate that transient heat exposure study designs can provide valuable insights into heat effects with TDS. Yet, even though continuous, prolonged exposure to elevated temperatures may not be the most clinically relevant scenario of heat application to a TDS, it may still be an appropriate IVPT study design to gain insights into the worst-case scenario.
The current study also investigated the effect of a transient exposure to an elevated temperature on the eventual nicotine and fentanyl clearance from the skin after TDS removal. For nicotine TDS, the 1 h heat exposure during the earlier time point (Early Heat) did not result in a higher clearance of nicotine from skin compared to baseline clearance amounts (No Heat II); rather, the clearance was higher from the baseline (No Heat II), compared to the Early Heat (Fig. 5). As expected, the release rate from Late Heat, in which the heat exposure occurred immediately prior to TDS removal, was higher than the release rates from Early Heat and No Heat II at 1 h after TDS removal. However, the release rate quickly decreased after 1 h. This suggests that the nicotine clears from the skin rapidly after 1 h heat exposure. In contrast, fentanyl TDS exhibited a sustained effect on the clearance of fentanyl from the skin following an exposure to the elevated temperature for 2 h prior to TDS removal (Fig. 9). Even 7 h after TDS removal, the clearance with Early Heat was higher than that with No Heat II (without heat). If such sustained effects were observed in vivo, even transient heat exposure may potentially be dangerous for fentanyl TDS, and other potent drugs that may have a significant skin depot effect.
Even though the results from the present study provide a comprehensive report on an exploratory IVPT method developed for the evaluation and comparison of TDS heat effects among differently formulated TDS, substantial further research is still needed to develop and characterize the IVPT heat effects model. It would be premature to draw conclusions related to any relative heat responses or effects for the various TDS evaluated in the current study.
The duration of transient heat exposure was intentionally increased for fentanyl compared to nicotine, in order to provide a sufficient exposure of the fentanyl TDS to the heat so that the relatively slowly permeating fentanyl could exhibit the heat effects observed for nicotine. However, this difference in heat exposure duration might also have contributed to the sustained heat effect on the drug release from the fentanyl skin depot. The effect of a time-course of heat duration should be investigated on skin depots of drugs/excipients of varying physicochemical properties in order to obtain a more thorough explanation.
Of particular note, the IVPT study was conducted using Yucatan miniature pig skin. Although pig skin is generally regarded as the closest animal skin surrogate for human skin in terms of the permeability of topically applied compounds, the applicability of the results reported here to drug permeation across human skin under the influence of heat is unclear, and the study was not intended to support such conclusions [26]. The decision to use pig skin for this proof-of-concept IVPT heat effects method development study was out of an expectation for lower intra-species (inter-individual) variability compared to human skin [26]. Indeed, inter-individual skin permeability was relatively similar during the current study. In fact, the skin used for longer (24 h for nicotine and 72 h for fentanyl) and shorter (12 h for nicotine and 22 h and 26 h for fentanyl) IVPT experiments (Fig. 1) were obtained from different donors, and yet the results were largely consistent. However, the difference between the donors may explain the occasional discrepancy between the baseline flux+ (No Heat II) and the flux+ at an elevated temperature (Early Heat and Late Heat) (Fig. 9a). Nonetheless, the data set presented in the current study supports the concept that it is feasible to design an adequately controlled and appropriately validated IVPT study, with which to evaluate the comparative heat effect on various TDS.
Conclusions
The results from the study indicate that adequate controls need to be implemented for the use of an IVPT model to evaluate and/or to compare the effects of heat on TDS products. The preliminary results from the TDS evaluated in this study using pig skin suggests that TDS with different compositions may behave differently when exposed to an elevated temperature. The results from the study suggest that some parameters of interest for further investigation are the magnitude of the heat effect on flux values, the total amount of drug permeation and the clearance of the drug from the skin depot after TDS removal. These parameters may vary for differently formulated TDS based on many factors, including but not limited to, different inactive ingredients (particularly adhesives) and different drugs. Ultimately, the observations in this exploratory study underscore the need for further evaluation of the potential risks arising from the exposure of some TDS to elevated temperatures. The present study illustrated, in principle, that IVPT could potentially be used to evaluate and/or compare the effects of heat on various matrix TDS with differences in their designs and inactive ingredients. To understand the clinical significance of IVPT heat effects studies, the results of future IVPT studies using human skin should be compared directly with the results of parallel in vivo clinical studies.
Abbreviations
- AUC:
-
Area under the curve
- FDA:
-
Food and drug administration
- HPLC:
-
High-performance liquid chromatography
- IVPT:
-
In vitro permeation tests
- Jmax :
-
Maximum flux
- LOD:
-
Limit of detection
- LLOQ:
-
Lower limit of quantification
- Q1:
-
Qualitatively
- Q2:
-
Quantitatively
- RLD:
-
Reference listed drug
- TDS:
-
Transdermal delivery systems
- TEWL:
-
Transepidermal water loss
References
Paudel KS, Milewski M, Swadley CL, Brogden NK, Ghosh P, Stinchcomb AL. Challenges and opportunities in dermal/transdermal delivery. Ther Deliv. 2010;1:109–31.
Wiedersberg S, Guy RH. Transdermal drug delivery: 30+ years of war and still fighting! J Control Release. 2014;190:150–6.
U.S. Food and Drug Administration. Guidance for Industry: topical Dermatologic Drug Products NDAs and ANDAs–In Vivo Bioavailability, Bioequivalence, In Vitro Release, and Associated Studies; 1998.
Aggarwal G, Dhawan S, Harikumar SL. Formulation, in vitro, and in vivo evaluation of matrix-type transdermal patches containing olanzapine. Pharm Dev Technol. 2013;18:916–25.
Ashburn MA, Ogden LL, Zhang J, Love G, Basta SV. The pharmacokinetics of transdermal fentanyl delivered with and without controlled heat. J Pain. 2003;4:291–7.
Park J-H, Lee J-W, Kim Y-C, Prausnitz MR. The effect of heat on skin permeability. Int J Pharm. 2008;359:94–103.
Moore KT, Sathyan G, Richarz U, Natarajan J, Vandenbossche J. Randomized 5-treatment crossover study to assess the effects of external heat on serum fentanyl concentrations during treatment with transdermal fentanyl systems. J Clin Pharmacol. 2012;52:1174–85.
Petersen KK, Rousing ML, Jensen C, Arendt-Nielsen L, Gazerani P. Effect of local controlled heat on transdermal delivery of nicotine. Int J Physiol Pathophysiol Pharmacol. 2011;3:236–42.
Prodduturi S, Sadrieh N, Wokovich AM, Doub WH, Westenberger BJ, Buhse LF. Transdermal delivery of fentanyl from matrix and reservoir systems: effect of heat and compromised skin. J Pharm Sci. 2010;99:2357–66.
Shomaker TS, Zhang J, Ashburn MA. Assessing the impact of heat on the systemic delivery of fentanyl through the transdermal fentanyl delivery system. Pain Med. 2000;1:225–30.
Carter KA. Heat-associated increase in transdermal fentanyl absorption. Am J Health Syst Pharm. 2003;60:191–2.
U.S. Food and Drug Administration. FDA issues second safety warning on fentanyl skin patch. Deaths and serious injuries from improper use; 2007; Available from: https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2007/ucm109046.htm.
Newshan G. Heat-related toxicity with the fentanyl transdermal patch. J Pain Symptom Manag. 1998;16:277–8.
Rose PG, Macfee MS, Boswell MV. Fentanyl transdermal system overdose secondary to cutaneous hyperthermia. Anesth Analg. 1993;77:390–1.
Sindali K, Sherry K, Sen S, Dheansa B. Life-threatening coma and full-thickness sunburn in a patient treated with transdermal fentanyl patches: a case report. J Med Case Rep. 2012;6:220.
Marriott TB, Charney MR, Stanworth S. Effects of application durations and heat on the pharmacokinetic properties of drug delivered by a lidocaine/tetracaine patch: a randomized, open-label, controlled study in healthy volunteers. Clin Ther. 2012;34:2174–83.
Otto DP, de Villiers MM. The experimental evaluation and molecular dynamics simulation of a heat-enhanced transdermal delivery system. AAPS PharmSciTech. 2013;14:111–20.
Vanakoski J, Seppälä T, Sievi E, Lunell E. Exposure to high ambient temperature increases absorption and plasma concentrations of transdermal nicotine. Clin Pharmacol Ther. 1996;60:308–15.
Gazerani P, Arendt-Nielsen L. Cutaneous vasomotor reactions in response to controlled heat applied on various body regions of healthy humans: evaluation of time course and application parameters. Int J Physiol Pathophysiol Pharmacol. 2011;3:202–9.
Bartosova L, Bajgar J. Transdermal drug delivery in vitro using diffusion cells. Curr Med Chem. 2012;19:4671–7.
Godin B, Touitou E. Transdermal skin delivery: predictions for humans from in vivo, ex vivo and animal models. Adv Drug Deliv Rev. 2007;59:1152–61.
Raney SG, Franz TJ, Lehman PA, Lionberger R, Chen ML. Pharmacokinetics-based approaches for bioequivalence evaluation of topical dermatological drug products. Clin Pharmacokinet. 2015;54:1095–106.
Muijsers RB, Wagstaff AJ. Transdermal fentanyl: an updated review of its pharmacological properties and therapeutic efficacy in chronic cancer pain control. Drugs. 2001;61:2289–307.
Product Information. Duragesic transdermal system patch. Janssen Pharmaceuticals, Inc: Titusville; 2014.
D'Alessandro A, Boeckelmann I, Hammwhöner M, Goette A. Nicotine, cigarette smoking and cardiac arrhythmia: an overview. European Journal of Preventive Cardiology SAGE Publications. 2012;19:297–305.
Barbero AM, Frasch HF. Pig and guinea pig skin as surrogates for human in vitro penetration studies: a quantitative review. Toxicol in Vitro. 2009;23:1–13.
ACKNOWLEDGEMENTS AND DISCLOSURES
Funding for this project was made possible, in part, by the Food and Drug Administration through grant U01FD004955. The views expressed in this paper do not reflect the official policies of the Department of Health and Human Services; nor does any mention of trade names, commercial practices, or organization imply endorsement by the United States Government.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Shin, S.H., Ghosh, P., Newman, B. et al. On the Road to Development of an in Vitro Permeation Test (IVPT) Model to Compare Heat Effects on Transdermal Delivery Systems: Exploratory Studies with Nicotine and Fentanyl. Pharm Res 34, 1817–1830 (2017). https://doi.org/10.1007/s11095-017-2189-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-017-2189-0