Valenta Pharm Co. compared the pharmacokinetic parameters in healthy volunteers of three prototype tizanidine dosage forms (delayed-release 6-mg tablets) and the reference drug sirdalud (2-mg tablets for a total dose of 6 mg, three tablets). This allowed the relative bioavailability of the three prototype tizanidine forms relative to sirdalud to be assessed. All three prototypes showed signs of delay based on MRT parameters of (2.217 ± 0.441) h for the sirdalud instant-release form and (6.529 ± 1.990), (5.951 ± 1.295), and (6.384 ± 2.339) h for prototypes T1, T2, and T3, respectively. High relative exposure levels of prototypes T1, T2, and T3 [AUC 103.80% (73.69 – 146.20), 124.14% (88.14 – 174.86), and 131.93% (93.66 – 185.82), respectively] with a significant decrease of C max (to 35.83, 38.78, and 40.79%, respectively) were demonstrated by analyzing the comparative bioavailability. A model pharmacokinetic study of the forms produced secondary modeling parameters that were similar to those obtained by an off-model method (89.19 – 122.71%). This confirmed that the developed model was acceptable for planning future clinical tests of these drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Tizanidine is a central myorelaxant that affects mainly the spinal cord. The drug stimulates presynaptic α2 receptors, thereby inhibiting the release of amino acids that stimulate N-methyl-D-aspartate receptors (NMDA-receptors). As a result, polysynaptic signal transduction is suppressed at the spinal-cord intermediate neuron level. Because just this mechanism is responsible for excessive muscle tone, muscle tone is diminished if it is suppressed. Tizanidine also has a central and moderate analgesic effect in addition to its myorelaxant properties.
Tizanidine is effective for acute painful muscle spasticity and for chronic spinal and cerebral spasticity. As a result, resistance to passive movements decreases and the number of active movements increases [1, 2].
Tizanidine is accumulated quickly and almost completely. The maximum plasma concentration is reached approximately 1 h after administration. The average bioavailability is ~34% because of extensive metabolism during the first pass through the liver. The average distribution volume at equilibrium after i.v. injection was 2.6 L/kg. Plasma-protein binding was 30%. Tizanidine pharmacokinetics were linear for doses from 4 to 20 mg. Considering the low variability among individuals of the pharmacokinetic parameters (in particular, the maximum concentration C max and the area under the concentration–time curve AUC), the tizanidine plasma concentration can be reliably predicted after internal administration. Sex had no effect on the pharmacokinetic parameters of tizanidine. Tizanidine was quickly and significantly metabolized in the liver. It was shown in vitro that tizanidine was metabolized mainly by isoenzyme 1A2 of the cytochrome P450 system. The metabolites were inactive. The average elimination half-life of tizanidine from systemic circulation was 2 – 4 h. The drug metabolites were eliminated primarily by the kidneys (~70% of the dose). The fraction of unaltered drug was only ~2.7% [1, 2].
The aforementioned pharmacokinetic data for the instant-release dosage form indicate that tizanidine is rapidly accumulated and metabolized and then quickly eliminated.
This creates the need to administer tizanidine at least three times per day. In many instances, this is inconvenient for patients. Furthermore, inconsistency in the administration times can cause significant oscillations of the tizanidine blood plasma concentration. This can preclude the selection and maintenance of an efficacious therapeutic dose.
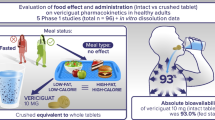
Three prototype tizanidine preparations were developed by Doppel Farmaceutici S.r.l. at the request of Valenta Pharm Co. in order to design a new delayed-release tizanidine dosage form that would foster high compliance and a stable therapeutic concentration of the active ingredient in blood plasma.
Experimental Part
The clinical trial was conducted as an open randomized study of the comparative pharmacokinetics of a single administration of the four tizanidine dosage forms in four administration sequences and in four periods. Three prototype tizanidine preparations, i.e., delayed-release 6-mg tablets (Doppel Farmaceutici S.r.l., by request of Valenta Pharm Co.) VPH020900, VPH020901, and VP020902, further designated T1, T2, and T3, respectively, and sirdalud preparation 2-mg tablets (Encore Healthcare Pvt. Ltd.), further R, were investigated. A total of 24 healthy male volunteers of ages 18 – 45 years participated in the study. Each volunteer in each of the periods took one of the tested tizanidine prototypes or sirdalud depending on the administration sequence that was determined by the randomization procedure. The wash-out period between administrations was 7 d. A total of 23 volunteers completed the study according to the protocol.
Blood samples were taken in each period using an i.v. catheter in the first 24 h and then venipuncture. Blood was collected in polypropylene tubes as follows: two samples collected before administration of the preparation and one sample each at 0.25, 0.5, 0.75, 1, 1.25, 1.5, 1.75, 2, 2.5, 3, 4, 6, 8, 12, 16, 24, 36, and 48 h after administration. The preservative was K2 EDTA.
Tubes with collected blood samples were placed into an ice bath and then centrifuged at 3,500 rpm for 10 min at 4°C. Then, the blood samples were separated into two aliquots and frozen at –(70 ± 10)°C. The time between collecting the samples and starting the centrifuge was <45 min.
Pharmacokinetic parameters that were calculated by an off-model method, i.e., AUC 0-t, the area under the concentration–time (observed) curve that was calculated by a linear trapezoidal method from 0 to the last measured concentration and C max, the maximum concentration, was used to compare the relative bioavailabilities of the preparations. The quantity AUC 0-∞ was calculated as the sum of the ratio C t/K el and the AUC (observed). The elimination constant (K el) was calculated by a least-squares method using the logarithm of data at the tail end of the pharmacokinetic curve including the last measured concentration. The elimination half-life (T 1/2);T max, the time to reach the maximum concentration; and MRT, the mean residence time were also calculated.
Furthermore, compartmental analysis of the pharmacokinetic parameters of the studied preparations was performed and the population model was determined.
The bioavailability was compared statistically using 90% confidence intervals for the ratios of the geometric averages; a least-squares method for AUC 0-t, AUC 0-∞, and C max; and a procedure analogous to PROC MIXED (SAS 9.2) in the Phoenix WinNonlin 6.3 software and considering a variation model that examined factors such as the preparation, period, and sequence.
An HPLC-MS/MS method using tizanidine D4 [deuterated 5-chloro-N-(4,5-dihydro-1H-imidazol-2-yl-d4)-2,1,3-benzothiazol-4-amine] as an internal standard was developed and validated in order to determine tizanidine in healthy volunteer blood plasma. The method included a liquid-extraction procedure. Chromatography used a Zorbax Eclipse XDB-CN column, 100 × 4.6 mm, 3.5 m at 40°C. The analysis time for each sample was <3.5 min (Table 1). Concentrations were determined by the internal standard method using tizanidine D4 hydrochloride as the standard.
The mobile phase was prepared by mixing MeOH (70 parts) and ammonium formate solution (10 mM, 30 parts) containing formic acid (0.2%). Then, mobile phase was ultrasonicated and stored at room temperature for <3 d after preparation.
The samples were unfrozen. An aliquot (300 μL) of the plasma was placed into a polypropylene tube, treated successively with internal standard solution [50 μL, 15 ng/mL; with the exception of the blank sample, which was treated with MeOH solution (60%, 50 μL)] and NaOH solution (0.2 M, 100 μL), stirred on a vortex mixer, treated with t-BuOMe (2.0 mL), stirred again on the vortex mixer for 5 min at 2,000 rpm, and centrifuged for 5 min at 4,500 rpm and 4°C. Atrace of the supernatant was collected, placed into a separate labeled polypropylene tube, and evaporated under N2 at 40°C for 15 min. The solid was redissolved in mobile phase (200 μL) and analyzed by HPLC (Table 2).
The method for determining tizanidine in blood plasma was validated according to recommendations in Guidance for Industry: Bioanalytical Method Validation, CDER, US FDA, May 2001 and Criteria for Standard Operating Procedures for Bioanalytical Laboratories.
Mass transfer effects were studied by analyzing the sequence, e.g., mobile phase sample, plasma blank sample, plasma sample containing analyte at the lower limit of quantitation (LLOQ), plasma sample containing analyte at the upper limit of quantitation (ULOQ), and plasma blank sample. An LLOQ of 0.100 ng/mL was achieved for this method.
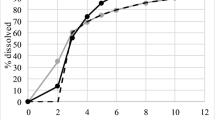
The linearity of the method was determined using a determination coefficient (R 2) for each calibration curve. The values fell in the range 0.9980 – 0.9987. The weighting coefficient was set at 1/x 2 (instead of 1/x) because the determination coefficients were greater if it was used. Figure 1 shows an example of a calibration curve.
The intraseries precision for the LOQ samples varied from 2.11 to 6.00% and from 0.38 to 2.95% for samples of other concentrations. The interseries precision was 6.32% for the LOQ samples and from 1.19 to 2.30% for samples of other concentrations.
The intraseries accuracy varied from –10.78 to –1.96% for the LOQ samples and from –2.46 to 7.29% for samples of other concentrations.
The degree of extraction was determined from the ratio of chromatographic peak areas for the quality-control sample and a standard solution of the same concentration (without extraction). The degree of extraction for tizanidine was (54.64 – 61.03)% (M = 58.03%). The average degree of extraction for tizanidine D4 was 67.62%.
The stability of the samples was determined using five freeze—thaw cycles and storage at room temperature (8 h); of prepared samples, in the autosampler (31 h at 4°C) and stored at room temperature (6 h 20 min); and of the precipitate, after evaporation (28 h 50 min at 2 – 8°C). The maximum deviation was –4.51% for the stability of the precipitate after evaporation. The freeze—thaw stability varied from –2.78 to 1.34%. The stability of prepared samples in the autosampler varied from –0.69 to 0.34%.
Matrix, hemolysis, fatty plasma, and drug-contamination (caffeine, paracetamol, cetirizine, diclofenac, aspirin) effects were also studied and were not found.
The reproducibility following a repeated sample injection after 24 h 15 min showed that the calibration-curve samples deviated from 1.04 to 2.27%; quality-control samples, from 6.15 to 10.42%.
The stability in whole blood was studied during method development (prevalidation). Stability studies determined that tizanidine remained stable in whole blood placed in an ice bath for >1,5 h. Figures 2 and 3 show the chromatograms.
Results and Discussion
Data obtained from 21 volunteers were used for the non-compartmental (off-model) analysis. One volunteer was emoved from the study for personal reasons. Data for two volunteers were not included in the statistical calculation because the preparation concentrations determined during the first visit were below the lower detection limit (both volunteers took prototype T1 on the first visit).
Table 3 presents the calculated pharmacokinetic parameters for the three tizanidine prototypes (delayed-release tablets, 6 mg, Doppel Farmaceutici S.r.l., by request of Valenta Pharm Co.) and reference preparation sirdalud [tablets, 2 mg, 6-mg dose (3 tablets), Encore Healthcare Pvt. Ltd.].
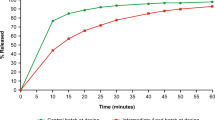
The average concentrations at each sample-collection time point were plotted in order to visualize the pharmacokinetic profile for each preparation (Fig. 4).
The 90% confidence intervals for the ratio of geometric averages of the studied parameters were obtained during dispersion analysis of the logarithms of the data (Table 2).
A mixed model considering the effects of factors such as the preparation, period, and sequence was used for the dispersion analysis.
The variation model for each parameter was written:
where μ is the average; F i , the effect of preparation i; S j , the effect of sequence j; P k (i, j), the effect of period k; Sub l |S j , a random effect of subject l in sequence j; and ε i, j, k, l , the residual variation.
Astatistically significant effect of the sequence on the results of the dispersion analysis was not observed. The preparation factor had a statistically significant effect on C max.However, this factor did not have a statistically significant effect on AUC. The period factor had statistically significant effects on both parameters. Because mass-transfer effects were not observed and compound concentrations at point 0 in all instances were less than the LLOQ, the effect of this factor was not due to insufficient rinsing and could be related to high intraindividual variability of the drug, a change of enzyme systems in the healthy volunteers in response to repeated administration of tizanidine, or a change of GIT activity in healthy volunteers during the study. It is noteworthy that the period factor had practically no effect on the pharmacokinetic parameters of the instant-release preparation. This factor could be studied during future investigations of multiple administrations of the drugs. Table 6 presents the descriptive statistics of AUC and C max for each preparation and period.
The compartmental analysis (model) was selected based on the correlation and determination coefficient of the one-compartment and two-compartment models taking into account the determination of the Lag Time parameter. A three-compartment model was not considered because of its high complexity. A model for 93 profiles from 93 pharmacokinetic profiles of volunteers (100.0%) could be defined for the one-compartment model during the determination of the individual models; parameters for 52 profiles (55.91%), for the two-compartment model. In both instances, the determination coefficient was high at 0.9729 and 0.9855 for the one- and two-compartment models, respectively. The correlation coefficient in both instances was close to unity at 0.9726 and 0.9841 (Figs. 5 and 6). The one-compartment model was used for subsequent calculations because the two-compartment model was defined successfully for only 55.91% of the pharmacokinetic profiles although the determination and correlation coefficients were greater than those for the one-compartment model. Also, the differences in the correlation and determination coefficients were insignificant compared with the fractions of successfully determined individual models. The high correlation coefficient for the two-compartment model could be explained by the fact that a significant part of the model profiles could not be determined.
Models were built using the software module Phoenix WinNonlin 6.3.0.395 PK model: WinNonlin Nonlinear Estimation Program, Nelder—Mead algorithm.
Then, the population one-compartment model taking into account the Lag Time parameter was calculated using the NLME software module of Phoenix WinNonlin (NLME7 built Mar. 19, 2012, 11:59:42). Figure 7 shows a diagram of the model. Figures 8 – 11 show plots of the obtained models. The primary parameters of the pharmacokinetic model are given in Table 7 and can be used for future planning of studies of a tizanidine delayed-release dosage form. This was confirmed by comparing the secondary pharmacokinetic parameters (89.19 – 122.71%) obtained from the modeling and presented in Table 8 with the off-model-method parameters from Table 3. Table 9 presents the comparison3333
Figure 7 shows a diagram of the used model. The preparation flows from the extravascular space (Aa) into a chamber (A1) at an accumulation rate determined by the absorption constant (Ka) and then distributes in the chamber volume (V) and is eliminated from the organism (A0) at a rate determined by the elimination constant (Ke). The concentration dynamics of the preparation in the chamber (CObs) is predicted during the modeling.
The results of the dispersion analysis showed a significant influence of the period factor on the pharmacokinetic parameters of the studied prototypes. Data obtained in the first study period were optimal in this instance, despite the small number of observations.
Thus, all three tizanidine prototypes showed signs of delay based on the MRT parameter (mean retention time), which was (2.217 ± 0.441) h for the instant-release preparation and (6.529 ± 1.990), (5.951 ± 1.295), and (6.384 ± 2.339) h for prototypes T1, T2, and T3, respectively. An analysis of the comparative bioavailability demonstrated a high level of relative exposure for the preparation (AUC): 103.80 (73.69 – 146.20), 124.14 (88.14 – 174.86), and 131.93 (93.66 – 185.82)% for prototypes T1, T2, and T3, respectively, with a significant reduction of the ratio for C max to 35.83, 38.78, and 40.79% for prototypes T1, T2, and T3, respectively (Tables 4 and 5). Each of the prototypes exhibited high bioavailability and could be considered a competitor for further pharmacological development. Differences in the bioavailability were due to the release rate of the active ingredient from the dosage form. Prototype T3 should be singled out because it exhibited the greatest relative exposure (131.93%), which indicated that the ratio of release, accumulation, and elimination rates was optimal. As a result, the preparation had a longer residence time in vivo and maintained the therapeutic concentration level of the active ingredient.
Modeling the pharmacokinetics of the studied preparations produced secondary modeling parameters that were similar in value to those obtained by the off-model method (89.19 – 122.71%). This confirmed that the model was suitable for possible use in planning future clinical trials of these prototypes taking into account the discussed limitations.
References
Instructions for Use of Sirdalud ® , Tablets, 2 mg and 4 mg [in Russian]; http: // www.grls.rosminzdrav.ru.
UK Public Assessment Report. Tizanidine 6mg Tablets; http: // www.mhra.gov.uk / home / groups / par / documents / websiteresources / con014794.pdf
V. G. Kukes, V. P. Fisenko, G. V. Ramenskaya, et al., Assessment of Drug Bioequivalency: Methodical Instructions [in Russian], Moscow (2008).
D. V. Reikhart, G. I. Baram, E. D. Gol?dberg, et al., Farmateka, No. 2 (98), 77 – 78 (2005).
D. V. Reikhart, Farmatsiya, 3, 5 – 8 (2010).
Acknowledgments
We thank Principal Investigator Dr. K. Anil, M. D., and Clinical Investigator Dr. S. Patil, MBBS, Human Pharmacology Unit, Clinigene International Ltd., Clinigene House, Tower I, Semicon Park.
Author information
Authors and Affiliations
Additional information
Translated from Khimiko-Farmatsevticheskii Zhurnal, Vol. 50, No. 6, pp. 26 – 35, June, 2016.
Rights and permissions
About this article
Cite this article
Kukes, V.G., Reikhart, D.V., Artnautov, V.S. et al. Comparative Bioavailability of Tizanidine in Three Dosage Forms (6-MG Delayed-Release Tablets, Sirdalud Preparation, and 2-MG Tablets). Pharm Chem J 50, 394–403 (2016). https://doi.org/10.1007/s11094-016-1458-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11094-016-1458-2