Anew antimigraine drug – Tropoxin (3-(3,4,5-trimethoxybenzoyloxyimino)-8-methyl-8-azabicyclo[1–3]octane hydrochloride) – was developed and was found to prevent or significantly weaken the constrictor reactions of cerebral arteries evoked by serotonin (5-HT) or the 5-HT2B/2C receptor agonist meta-chlorophenylpiperazine (m-CPP) in intact animals and in animals with ischemic brain damage. Tropoxin showed affinity for5-HT2 receptors in the brain and had antiaggregatory actions. It had no marked neurotropic properties and did not alter blood pressure responses to noradrenaline, acetylcholine, or histamine. Pilot clinical trials of Tropoxin provided evidence that it has high efficacy in the interictal treatment of frequent and severe migraine attacks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Migraine is one of the most common chronic neurovascular diseases in the present world, mainly affecting people of peak working age. Around 12% of the population in Russia suffer from migraine, as do about 11% in the USA, 18% in Japan, 26% in Europe, and 30% in South America; the number of patients increases every year [1–6] (Fig. 1).
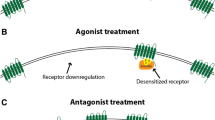
The most widely used drugs for the treatment of migraine are those acting on type 1 (5-HT1A/1B/1D/1F) and type 2 (5-HT2A/2B/2C) serotonin receptors, pointing to the important role of serotonin in the pathogenesis of this disease [7–10]. 5-HT1B/1D/1F receptor agonists are used for the treatment of migraine attacks (sumatriptan, zolmitriptan, naratriptan, and others) [1, 11, 12], while interictal treatment uses 5-HT2B/2C receptor antagonists (methysergide, pizotifen, ciproheptadine, nicergoline), these preventing the vasoconstrictor effect of serotonin [13–16].
The agents identified above, used for the treatment of migraine, do not always have high efficacy, but have marked adverse side effects. This defines the need to seek new drugs for the prophylaxis and treatment of migraine attacks [17].
The present study addressed the pharmacological properties of a new antimigraine drug – Tropoxin (3-(3,4,5-trimethoxybenzoyloxyimino)-8-methyl-8-azabicyclo[1–3]octane hydrochloride) [18, 19].
Experimental Section
Experiments were performed on 153 anesthetized (choral hydrate, 350 – 400 mg/kg, i.p.) and 60 conscious mongrel male rats weighing 250 – 300 g, and 149 conscious mice weighing 18 – 25 g.
Cerebral circulation in animals was evaluated by laser Doppler flowmetry with an ultrasound flow meter from Transonic System Inc. (USA) [20, 21]. Local permanent ischemia was induced by ligation of the left middle cerebral artery in anesthetized rats [22]. Global ischemia in rats was induced by 10-min occlusion of both common carotid arteries with simultaneous reduction of arterial blood pressure to 40 – 50 mmHg by exsanguination followed by reperfusion [20, 21]. Changes in arterial blood pressure in the femoral artery were measured in all experiments. Traces of blood flow measurements and arterial pressure were made on a BIOPAK (USA) polygraph connected to a personal computer.
Cerebral vessel constrictor responses were modeled using 5-HT (20 μg/kg, i.v.; Sigma Aldrich, Germany) or the 5-HT2B/2C receptor agonist m-CPP (0.1 mg/kg, Sigma Aldrich, Germany) [23]. Tropoxin (10 mg/kg) was synthesized at the Experimental-Technical Department, V. V. Zakusov Science Research Institute of Pharmacology. Study compounds were given into the animals’ femoral vein.
Data were analyzed statistically in Biostat and Statistica 8.0 (Statistica Inc., USA). Average results are presented in the text as median and arithmetic mean with its standard error (M ± m). Results were regarded as significant at p ≤ 0.05.
Results and Discussion
Antiserotonin Cerebrovascular Activity of Tropoxin and the Reference Agent
There is no doubt that brain vessels, like serotonin, play a role in the pathogenesis of migraine attacks, so cerebral vascular constrictor reactions were modeled using 5-HT or the 5-HT2B/2C receptor agonist m-CPP.
Experiments performed on anesthetized rats showed that 5-HT (20 μg/kg, i.v.) decreased the volume rate of cerebral blood flow in the internal carotid artery in most cases, by an average of 40% (n = 10) during the first minute after administration. Recovery of the initial level of cerebral blood flow occurred 5 – 7 min after 5-HT injection. In most experiments, decreases in blood flow in the brain in response to serotonin were accompanied by decreases in arterial blood pressure. The series of experiments addressing the influence of 5-HT on the microcirculation of the rat cerebral cortex demonstrated decreases in local cerebral blood flow by a mean of (27.0 ± 3.3)% (n = 10).
Published data indicate that the 5-HT2B/2C receptor agonist m-CPP provokes attacks of headache in migraine patients [24] and induces increases in extravasation of plasma albumin from the meningeal vessels and activation of the sensory fibers of the trigeminovascular system.
The experiments showed that administration of m-CPP (0.1 mg/kg, i.v.) was followed immediately by a 30% decrease in cerebral blood flow in the internal carotid artery (n = 10), with a 33% decrease in the cerebral cortex of the rats (n = 10), with subsequent recovery over a period of 10 min. Repeated doses of both 5-HT and m-CPP given with an interval of 30 min induced analogous changes in cerebral blood flow and arterial blood pressure.
Tropoxin was studied at a dose of 10 mg/kg given i.v. The effective dose was that corresponding to about 10% of the LD50 (78 mg/kg). Studies of the effects of Tropoxin on changes in blood flow in the internal carotid artery in anesthetized rats induced by 5-HT showed that on the background of Tropoxin, administration of 5-HT evoked a decrease in blood flow, by 27.8% and 31.5% at 20 and 40 min respectively (n = 10), which constituted a statistically significant difference from controls (40%, p ≤ 0.05). The duration of the effect was 1 h. The antiserotonin cerebrovascular effect of Tropoxin was also seen in experiments with p.o. administration of drug at a dose of 30 mg/kg (experiment: (28.0 ± 4.6)%; control: (51.0 ± 3.8)%; p ≤ 0.05, n = 8).
In conditions of local ischemic brain damage induced by ligation of the middle cerebral artery in rats, Tropoxin blocked the vasoconstrictor reaction of cortical microvessels induced by 5-HT for 120 min (n = 9) [26].
Before administration of Tropoxin, m-CPP evoked a decrease in cerebral blood flow by a mean of 25%; after Tropoxin, reductions were by 19.2% and 11.3% at 20 and 40 min respectively (p ≤ 0.05, n = 10). This effect was apparent for 1 h. On administration of m-CPP, arterial blood pressure decreased by a mean of 33% and was then restored to levels close to those in controls. Tropoxin had no statistically significant effect on this arterial blood pressure response.
In the series of experiments with administration of m-CPP 20 min after Tropoxin, the decrease in cerebral blood flow in response to agonist was by only 6% at 20 min and 7.5% at 40 min (n = 8). The cerebral vessel constrictor reaction after administration of m-CPP then gradually returned to the response seen in control experiments (27.5%).
Thus, Tropoxin significantly weakened the constrictor effects of both 5-HT and the 5-HT2B/2C receptor agonist on brain vessels.
We then performed a comparative study of the antiserotonin properties of Tropoxin and drugs widely used in neurological practice for the treatment of migraine, particularly the serotonin receptor antagonist methysergide, the α-adrenoblockers dihydroergotamine and nicergoline, and the β-adrenoblocker propranolol. The antiserotonin properties of dihydroergotamine are known, though the literature lacks data on the antiserotonin cerebrovascular properties of both nicergoline and propranolol. We therefore studied the effects of these drugs and the structural analog of Tropoxin, the 5-HT3 receptor antagonist tropisetron, on the constrictor reactions of cerebral vessels in response to administration of 5-HT [27].
This study provided support for published data demonstrating the ability of methysergide and dihydroergotamine to weaken serotonin-induced spasm of the cerebral vessels. In controls, serotonin decreased cerebral blood flow by (47.0 ± 3.5)%; the decrease in influx of blood into brain induced by 5-HT 20 min after administration of methysergide (1 mg/kg, i.v.) was by only (25.0 ± 4.5)% (n = 8, p < 0.01). Dihydroergotamine (1 mg, i.v., n = 8) also produced significant weakening of the decrease in cerebral blood flow seen in response to 5-HT.
Experiments using nicergoline showed that this agent, along with α-adrenoblocking properties, also had anti-serotonin actions in relation to cerebral vessels, as after prior administration of nicergoline (200 μg/kg, i.v.), 5-HT decreased cerebral blood flow by an average of (30.0 ± 5.2)%, compared with (47.0 ± 2.9)% in controls (p < 0.02, n = 10).
The β-adrenoblocker propranolol (1 mg/kg, i.v.) had an antiserotonin effect in 50% of experiments (n = 10), which is evidence for individual sensitivity of animals to this agent.
The structural analog of Tropoxin, the 5-HT3 receptor antagonist tropisetron, did not weaken the reaction of cerebral vessels to 5-HT. Tropisetron produced a small degree of weakening of the arterial blood pressure reaction to 5-HT (n = 7).
Thus, in terms of its antiserotonin cerebrovascular effect, Tropoxin is no less active and in some cases more active than reference agents. The 5-HT3 receptor antagonist tropisetron does not have this action, indicating that these receptors are not involved in mediating the constrictor reactions of cerebral vessels. This explains the observation that tropisetron, which on the basis of experimental data was proposed for the treatment of migraine patients, was not clinically effective [28]; it was introduced into clinical practice as an antiemetic agent.
Cardiovascular, Neuropsychotropic, and Antiaggregatory Properties of Tropoxin
Studies of the cardiovascular effects of Tropoxin established that it produced a small decrease in arterial blood pressure, decreased heart rate, and produced a central suppressive influence on the adrenergic regulation of the circulation, weakening the reflex pressor reaction of arterial blood prespressure and reflex discharges in the sympathetic nerves induced by pain stimulation of afferent fibers in the tibial nerve (n = 15). Tropoxin did not alter the arterial blood pressure reactions to acetylcholine, noradrenaline, or histamine, and induced slight suppression of the vagus reflex (n = 20) [27].
Studies of the neuropsychotropic effects of Tropoxin were performed on 85 mice and 40 rats. These studies showed that it had the ability to produce significant decreases in the duration of sleep induced by hexenal, increases in horizontal activity in an open field, and decreases (1.5-fold) the duration of immobility (“behavioral helplessness”) in the Porsolt swimming test. The agent improved the acquisition/retention of a conditioned passive avoidance reflex in animals with poor learning ability. Tropoxin decreased spontaneous movement activity recorded on an actometer. In addition, it weakened the convulsive actions of thiosemicarbazide and 5-hydroxytryptophan, while high doses increased the action of corasol. Tropoxin had no anxiolytic effect in conditions of a conflict situation and had no antihypoxic or antiamnestic action.
Thus, Tropoxin has a moderate psychostimulatory action. In terms of the spectrum of psychostimulating effects, Tropoxin differs from the actions of typical psychostimulators of the amphetamine type. Data on the ability of Tropoxin to enhance the action of the GABA benzodiazepine complex antagonist corasol and to weaken convulsions evoked by 5-hydroxytryptamine suggest the involvement of the GABA- and serotoninergic neurotransmitter systems in mediating the psychotropic actions of the drug.
Experiments addressing the analgesic activity of Tropoxin using the tail flick and hotplate tests showed that doses of 10 and 50 mg/kg (40 mice and 20 rats) had no effect on pain thresholds in animals in the experiments, so the agent does not have analgesic activity.
Studies using microiontophoresis showed that Tropoxin, like methysergide, suppressed excitatory neuronal responses to 5-HT, i.e., was also an antagonist of 5-HT receptors in the cerebral cortex [29].
Experiments using a radioligand binding method showed that Tropoxin competed with labeled 5-HT2 receptor antagonist spiperone for specific binding sites. Thus, 5-HT2 receptors are the primary target for the antiserotonin activity of Tropoxin [18].
Tropoxin, an antimigraine drug with 5-HT2 receptor antagonist properties, inhibited both ADP- and adrenalin-induced platelet aggregation in vitro at concentrations of 0.01 – 7 mg and ex vivo in rabbit experiments at a dose of 10 mg/kg. The antiaggregatory effect of Tropoxin was comparable with the inhibitory influence of curantyl [30].
The pharmacological effects of Tropoxin are summarized in Table 1.
Results from Clinical Trials of the Antimigraine Actions of Tropoxin
On the basis of the experimental data and in compliance with a resolution of the Pharmacology Committee of the Ministry of Health of the Russian Federation (Protocol No. 6 of 02 July, 1998), a clinical trial of Tropoxin was performed at the Department of Neurology and Neurosurgery, Academician I. P. Pavlov St. Petersburg State Medical University. Results from a pilot-scale blind, placebo-controlled trial of Tropoxin led by Professor V. A. Amelin on the treatment of migraine without aura in 30 patients showed that Tropoxin had high efficacy in the interictal treatment of frequent and severe migraine attacks. A decrease in the frequency of migraine attacks was seen four weeks from the beginning of treatment. There were significant reductions in the intensity and duration of headache and a significant reduction in the quantity of analgesics consumed for amelioration of developing migraine attacks. There was a significant increase in patients’ quality of life. The efficacy of Tropoxin was comparable with that of propranolol, pizotifen, and tricyclic antidepressants. It should be noted that studies of Tropoxin in migraine patients did not note any adverse side effects, in contrast to other drugs used in the treatment of migraine. In the authors’ view, the combination of high efficacy and safety of Tropoxin suggest that it can be regarded as a drug recommended for the interictal treatment of migraine [1].
Thus, these data demonstrating the ability of Tropoxin to counter the constrictor reaction of vessels evoked by 5-HT and m-CPP, with suppression of the excitatory neuronal responses to 5-HT, and an antiaggregatory action, suggest that it can be used as a drug for the interictal treatment of migraine. Experimental data were supported by neurological clinical experience.
It should also be noted that the data reported in [31] show that Tropoxin suppresses the activity of sensory neurons in the trigeminal complex evoked by electrical stimulation of the superior sagittal sinus. This is evidence for the ability of Tropoxin to suppress aseptic “neurogenic” inflammation, which results from the release of vasoactive and algogenic neuropeptides (calcitonin gene-related peptide, substance P) from presynaptic terminals of the trigeminal nerve and is regulated by inhibitory presynaptic heteroreceptors of the 5-HT1B/1D type. The 5-HT1B/1D receptor agonists sumatriptan and zolmitriptan had analogous effects, leading the authors to suggest that Tropoxin may be a partial agonist of presynaptic 5-HT1B/1D receptors. Thus, Tropoxin can be also recommended for studies as an agent for the treatment of migraine attacks.
References
A. V. Amelin, Yu. D. Ignatov, and A. A. Skoromets, Migraine (Pathogenesis, Clinical Aspects, Treatment), St. Petersburg Medical Press, St. Petersburg (2001).
N. N. Yakhno, and D. R. Shtul’man, Diseases of the Nervous System. Handbook for Doctors [in Russian], Meditsina, Moscow (2003).
M. Schurks, R. Y. Zee, J. E. Buring, and T. Kurth, Cephalalgia, 30(4), 447 – 456 (2010); Doi: 10.1111/j.1468 – 2982.2009.
P. M. Rist, J. E. Buring, C. S. Kase, et al., Circulation, 122(24), 2551 – 2557 (2010).
W. Dent, B. Stelzhammer, M. Meindl, et al., Headache, 51(10), 1483 – 1492 (2011); Doi: 10.1111/j.1526 – 4610.2011.
A. Pezzini, E. Del Zotto, A. Giossi, et al., Stroke Res. Treatment, 9(2010); Doi:10.4061/2011/304921.
D. Hoyer and G. Martin, Neuropharmacology, 36, 419 – 428 (1997).
A. Panconesi and R. Sicuteri, Cephalalgia, 17, 3 – 14 (1997).
P. J. Goadsby, Headache: The Journal of Head and Face Pain, 51(4), 650 – 653 (2011).
V. Granados-Soto, C. F. Arguelles, H. I. Rocha-Gonzalez, et al., Neuroscience, 165, 561 – 568 (2010).
S. J. Tepper, A. M. Rapoport, and F. D. Sheftell, Arch. Neurol., 59, 1084 – 1088 (2002).
T. Muller and L. Lohse, Clin. Neuropharmacol., 34(6), 206 – 209 (2011).
E. J. Mylecharane, J. Misbach, J. W. Duckworth, and J. W. Lance, Eur. J. Pharmacol., 48, 1 – 9 (1978).
K. Schmuck, C. Ullmer, H. O. Kalkman, et al., Eur. J. Neurosci., 8(5), 959 – 967 (1996).
G. Casucci, V. Villani, and F. Frediani, Neurol. Sci., 29, 123 – 126 (2008).
J. A. Charles, Headache: The Journal of Head and Face Pain, 51(10), 1550 – 1551 (2011).
A. Raizada, S. S. Vittala, M. Q. Najib, et al., Eur. J. Echocardiogr., 12(11), 880 (2011).
R. S. Mirzoyan, S. B. Seredenin, T. S. Gan’shina, et al., Éksperim. Klin. Farmakol., 61(2), 28 – 31 (1998).
L. M. Kostochka, T. S. Gan’shina, R. S. Mirzoyan, and S. B. Seredenin, Khim.-Farm. Zh., 44, No. 9, 6 – 9 (2010); Pharm. Chem. J., 44(9), 472 – 475 (2010).
R. S. Mirzoyan, T. S. Gan’shina, D. V. Maslennikov, et al., BioMed. Res. Intern., Vol. 2014 (2014), Article ID 586501; http://dx.doi.org/10.1155/2014/586501.
R. C. Mirzoyan, M. B. Plotnikov, T. S. Gan’shina, et al., Handbook for Conducting Preclinical Studies of Drugs [in Russian], Grif i K, Moscow (2012), Part 1, pp. 480 – 487.
A. V. Topchyan, R. S. Mirzoyan, and M. G. Balasanyan, Éksperim. Klin. Farmakol., 59(5), 62 – 64 (1996).
A. A. Gorbunov, T. S. Gan’shina, and R. S. Mirzoyan, Éksperim. Klin. Farmakol., 73(9), 13 – 16 (2010).
A. Panconesi and R. Sicuteri, Cephalalgia, 17(1), 3 – 14 (1997).
A. Yu. Sokolov, O. A. Lyubashina, and S. S. Panteleev, Neirokhimiya, 2, 104 – 112 (2011).
R. S. Mirzoyan, A. V. Topchyan, T. S. Gan’shina, and L. M. Kostochka, Éksperim. Klin. Farmakol., 63(3), 21 – 23 (2000).
T. S. Gan’shina, Éksperim. Klin. Farmakol., 66(3), 17 – 20 (2003).
M. D. Ferrari, M. Wilkinson, D. Hirt, et al., Pain, 45(3), 283 – 291 (1991).
S. N. Kozhechkin, L. M. Kostochka, S. G Bezhanyan, et al., Éksperim. Klin. Farmakol., 68(4), 3 – 6 (2005).
T. M. Vasil’eva, G. N. Petrukhina, N. T. Miftakhova, et al., Éksperim. Klin. Farmakol., 68(3), 30 – 33 (2005).
A. V. Amelin, V. E. Ivanov, Yu. D. Ignatov, et al., Éksperim. Klin. Farmakol., 62(4), 14 – 17 (1999).
Author information
Authors and Affiliations
Additional information
Translated from Khimiko-Farmatsevticheskii Zhurnal, Vol. 50, No. 1, pp. 19 – 23, January, 2016.
Rights and permissions
About this article
Cite this article
Gan’shina, T.S., Gorbunov, A.A., Gnezdilova, A.V. et al. Tropoxin – Drug for the Treatment of Migraine. Pharm Chem J 50, 19–23 (2016). https://doi.org/10.1007/s11094-016-1391-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11094-016-1391-4