Abstract
It is vital to understand the mechanism of epilepsy onset and development. Dysregulated lncRNAs are closely associated with epilepsy. Our work probed the role of lncRNA PVT1/miR-488-3p/FOXD3/SCN2A axis in epilepsy. The mRNA and protein expressions were assessed using qRT-PCR and western blot. MTT assay and TUNEL staining were conducted to assess cell viability and apoptosis, respectively. TNFα, IL-1β and IL-6 levels were analyzed using ELISA. LDH level was tested by Assay Kit. The binding relationship between PVT1, miR-488-3p and FOXD3 were verified using dual luciferase reporter gene assay. The epilepsy model of rats was established by lithium-pilocarpine injection. Nissl staining was performed to evaluate neuronal damage. PVT1 was markedly upregulated in epilepsy model cells. Knockdown of PVT1 increased the viability, while repressed the apoptosis and inflammatory cytokines secretion as well as LDH level in epilepsy cell model. MiR-488-3p alleviated neuronal injury and neuroinflammation in model cells. MiR-488-3p functioned as the direct target of PVT1, and its inhibition neutralized the effects of PVT1 silencing on neuronal cell injury and neuroinflammation in model cells. Furthermore, miR-488-3p inhibited neuronal cell injury and neuroinflammation in model cells by regulating FOXD3/SCN2A pathway. Finally, animal experiments proved that PVT1 promoted epilepsy-induced neuronal cell injury and neuroinflammation by regulating miR-488-3p-mediated FOXD3/SCN2A pathway. PVT1 promoted neuronal cell injury and inflammatory response in epilepsy via inhibiting miR-488-3p and further regulating FOXD3/SCN2A pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy is a chronic neurological disease caused by excessive discharge caused by abnormal excitation of neurons, affecting more than 1% of people worldwide [1,2,3]. Persistent epilepsy results in acute and persistent damage to neurons and its clinical features are recurrent disturbances of consciousness and muscle convulsions [4]. About 30% of patients with epilepsy develop refractory epilepsy, and current anti-epileptic drug treatments fail to control the seizures of these patients [1]. Therefore, it is extremely important to reveal the molecular mechanism of epilepsy pathogenesis, which will help to find novel effective treatment strategies for epilepsy patients.
Long non-coding RNAs (lncRNAs) are non-coding RNAs with transcripts longer than 200 nt [5]. The function of lncRNAs in the pathogenesis of epilepsy has been widely reported [6,7,8,9]. As proof, lncRNA MEG3 overexpression could remarkably suppress neuron apoptosis in hippocampus [10]. In addition, lncRNA NEAT1 silencing was reported to inhibit inflammatory response in epilepsy cell model [7]. LncRNA plasmacytoma variant translocation 1 (PVT1), located on chromosome 8q24, is widely confirmed as an oncogene [11]. It was described that PVT1 silencing could markedly inhibit malignant behaviors of human glioma cells [12]. A recent study emphasized the role of PVT1 in epilepsy, specifically PVT1 knockdown reduced the loss of neurons and inhibited the activation of astrocytes in the hippocampus of epileptic rats [13], suggesting PVT1 was a risk factor affecting epilepsy. Nevertheless, the mechanisms of PVT1 in epilepsy and its correlation with epilepsy inflammation are still unclear.
MicroRNAs (miRNAs) are noncoding RNAs of 20–22 nts in length [14]. As well known, miRNA dysregulation is linked to epilepsy pathogenesis [15]. As proof, Wang et al. displayed that miRNA-137 overexpression in the brains of epileptic mice could suppress seizures and neuronal excitability [16]. MiR-488 has become a research hotspot recently [17, 18]. MiR-488-3p overexpression could remarkably inhibit oxygen glucose deprivation/reoxygenation-induced neuronal cell death [19], revealing that miR-488-3p had protective effects on neurons. Additionally, miR-488 overexpression was reported to suppress the inflammatory response induced by monosodium urate in THP-1 cells [20]. It’s suggested that miR-488-3p functions in regulating neuronal cell damage and inflammation, however its role in epilepsy is largely unclear. It was observed that PVT1 achieved its biological function in many diseases by sponging miR-488-3p [12, 21, 22]. Nevertheless, the regulatory relationship between PVT1 and miR-488-3p in epilepsy is largely unknown, which is worthy of further research.
Forkhead box D3 (FOXD3), as a transcription factor in regulating neural crest cell differentiation, is confirmed to be related to epilepsy progression [23, 24]. As previously reported, FOXD3 was remarkably upregulated in refractory epilepsy cell model, and its silencing relieved magnesium-free-induced neuron damage by elevating sodium voltage-gated channel alpha subunit 2 (SCN2A) expression [24]. We found that FOXD3 was one of the targets of miR-488-3p, thus, we speculated that miR-488-3p could be involved in epilepsy development by regulating the FOXD3/SCN2A pathway.
Herein, we probed the function of lncRNA PVT1 in epilepsy and its underlying molecular mechanisms. We hypothesized that that PVT1 upregulated FOXD3 by sponging miR-488-3p, thereby promoting neuronal cell injury and neuroinflammation in epilepsy. Therefore, PVT1 may become a potential therapeutic target for epilepsy.
Materials and Methods
Cell Culture and Treatment
SH-SY5Y cells were obtained from ATCC. All cells were cultured in DMEM (Gibco) mixed with 10% FBS (Gibco) at 37 °C with 5% CO2. To stimulate SH-SY5Y cells to differentiate into neuron-like cells, cells were subjected to 10 µM retinoic acid (Sigma-Aldrich) for 7 d. Then, cells were cultured in magnesium-free DMEM containing 10 ng/mL BDNF for 3 h to establish refractory epilepsy cell model (Peprotech).
Cell Transfection
The short hairpin of PVT1 (sh-PVT1, 5′-GCGGGTGACCTTGGCACATAC-3′, Cat.No: C02007) was designed according to the sequence of PVT1 transcripts in NCBI. The accepted scramble sequence (GTTCTCCGAACGTGTCACGT) was used as a negative control (sh-NC). To construct the overexpression plasmids of FOXD3 (NM_012183.3), its coding sequence (CDS) were amplified and then inserted into the pcDNA3.1 vector (pcDNA3.1 FOXD3, Cat.No: C05008). MiR-488-3p mimics and inhibitor was employed to overexpress and decrease the level of miR-488-3p, respectively. The sequences were as follows: miR-488-3p mimics (sense: 5′‐UUGAAAGGCUAUUUCUUGGUC‐3′, antisense: 5′‐CCAAGAAAUAGCCUUUCAAUU‐3′, Cat.No: B02001); mimics NC (sense: 5′‐UUCUCCGAACGUGUCACGUTT‐3′, antisense: 5′‐ACGUGACACGUUCGGAGAATT‐3′); miR-488-3p inhibitor (5′‐GACCAAGAAAUAGCCUUUCAA‐3′, Cat.No: B03001); inhibitor NC (5′‐CAGUACUUUUGUGUAGUACAA‐3′). Cells were transfected with a final concentration of 50 nM of the specific sh-RNA PVT1, pcDNA3.1 FOXD3, or 40 nM of miR-488-3p mimics/inhibitor, respectively, using Lipofectamine™ 3000 transfection reagent (Invitrogen) according to the manufacturer’s instructions. Cells were used for follow-up experiments following the detection of transfection efficiency by qRT-PCR. The above plasmids and sequences were all synthesized and constructed by GenePharma.
3-(4, 5-Dimethylthiazolyl2)-2, 5-Diphenyltetrazolium Bromide (MTT) Assay
Cells were seeded in a 96-well plate (2 × 103 cells/well) for 12 h and incubated with 5 mg/mL MTT (Beyotime, Shanghai, China) for 4 h. Then the absorbance at 490 nm was analyzed with a microplate reader after DMSO (Sigma-Aldrich) supplement (Bioteke, Beijing, China).
TdT-Mediated dUTP Nick-End Labeling, (TUNEL) Staining
Cells were fixed and permeabilized. TUNEL staining was conducted using the kit (Roche). The nucleus was stained with DAPI (Sangon). The images were obtained with fluorescence microscope (Olympus).
Dual Luciferase Reporter Gene Assay
WT and MUT reporter plasmids of PVT1/FOXD3 sequences were amplified and cloned into pmiRGLO vector (GenePharma). Then, cells were co-transfected with the recombinant plasmids and miR-488-3p mimics/mimics NC/miR-488-3p inhibitor/inhibitor NC. The Luciferase activity was examined.
Measurement of Lactate Dehydrogenase (LDH) Level
LDH level was assessed by LDH assay Kit (Beyotime). Briefly, SH-SY5Y cells were lysed and the supernatant collected, and the supernatant was incubated with the reaction mixture for 30 min. Finally, the absorbance at 490 nm was analyzed.
Enzyme-Linked Immunosorbent Assay (ELISA)
The secretions of tumor necrosis factor-α (TNF-α), interleukin (IL)-6 and IL-1β were examined by ELISA kits purchased from Beyotime. Cell supernatant and serum were collected for experiment. The experimental operation was performed strictly according to the manual. The data were analyzed in the microboard reader (Bioteke).
Animal Experiments
Male SD rats were purchased from Hunan Star Laboratory Animal Co. LTD (Hunan, China). The rats were randomly divided into following groups: control group, model group, model + sh-NC + inhibitor NC group, model + sh-PVT1 + inhibitor NC group and model + sh-PVT1 + miR-488-3p inhibitor group. Epileptic group rats were injected with 3 μl (0.2 μl/min) of the corresponding lentivirus vector (titer 2 × 108 IFU/ml) into each hippocampus with the use of stereotaxic apparatus, and stepper motorized microsyringe into the hippocampus. Epileptic rat model was constructed using Lithium-pilocarpine as previously described [25]. Briefly, lithium chloride (Sigma-Aldrich) was intraperitoneally injected (127 mg/kg), scopolamine methyl bromide (Sigma-Aldrich, 1 mg/kg) was intraperitoneally injected 24 h later, then 1% pilocarpine (Sigma-Aldrich, 30 mg/kg) was administrated 30 min later. 30 mg/kg pilocarpine (Sigma-Aldrich) was intraperitoneally injected into rats 30 min after 1 mg/kg atropine (Sigma-Aldrich) injection. Epileptic seizures of the rats were evaluated by the modified Racine score as previously reported [26], and the models of grade IV or above were regarded successful. After status epilepticus (SE) for 1 h, 2 mg/kg diazepam (Sigma-Aldrich) was injected for SE termination. The model rats developed spontaneous seizures after 28 d. Then rats were sacrificed, and hippocampus tissues were collected. All animal experimental procedures were reviewed and approved by The Second Xiangya Hospital of Central South University.
Nissl Staining
The hippocampus tissues were fixed in 4% paraformaldehyde and Sections (30 μm in thickness) were prepared. The sections were immersed in a mixed solution of anhydrous ethanol and chloroform overnight. Then sections were dehydrated with different concentrations of ethanol and stained with 0.1% methylphenol (Sigma-Aldrich) for 10 min. The images were obtained with inverted microscope.
Quantitative Real-Time Polymerase Chain Reaction (qRT-PCR)
Total RNA was extracted with TRIzol (Thermo Fisher Scientific). For mRNA and miRNA, the cDNA was synthesized using the Reverse Transcription Kit (Toyobo) and first-strand cDNA synthesis kit (Sangon), respectively. Then, SYBR (Thermo Fisher Scientific) was employed for the qRT-PCR assay. GAPDH and U6 were used as the reference gene for mRNA and miRNA, respectively. The data was analyzed with 2−ΔΔCT method. The primers used in the study were listed as follows (5′-3′):
PVT1 (F): 5′- CTTGCGGAAAGGATGTTGGC -3′
PVT1 (R): 5′- GCCATCTTGAGGGGCATCTT -3′
miR-488-3p (F): 5′- CGGCCGTTGAAAGGCTATTTC -3′.
miR-488-3p (R): 5’-GTCGTATCCAGTGCAGGGTCCGAGGTATTCGCACTGGATACGAC GACCAA -3′.
FOXD3 (F): 5′- CGAGCAAGCCCAAGAAC -3′
FOXD3 (R): 5′- TGCTGATGAACTCGCAGAT -3′
SCN2A (F): 5′- GCTAAGAGACCCAAACAGGAAC -3′
SCN2A (R): 5′- GAATCGAGAGATTGCTTTCCCTT -3′
U6 (F): 5′- CGCTTCGGCAGCACATATAC -3′
U6 (R): 5′- AAATATGGAACGCTTCACGA -3′
GAPDH (F): 5′- TCAAGAAGGTGGTGAAGCAGG -3′
GAPDH (R): 5′- TCAAAGGTGGAGGAGTGGGT -3′
Western Blot
Total proteins were extracted using RIPA (Thermo Fisher Scientific). BCA kit (Beyotime) was used to quantify the concentration. Proteins were separated using the 10% SDS-page gel and further transferred into a PVDF membrane (Millipore). The membranes were subsequently incubated overnight with antibodies against Bax (Abcam, 1:1000, ab32503), Bcl-2 (Abcam, 1:1000, ab196495), cleaved-caspase 3 (Abcam, 1:1000, ab32042), FOXD3 (Abcam, 1:200, ab273019), SCN2A (Cell Signaling Technology, 1:1000, #14,380) and GAPDH antibody (Sigma-Aldrich, 1:10,000, SAB2701826). After being washed with PBS-T, membranes were then incubated with the corresponding secondary antibody (Abcam, 1:5000, ab7090, ab6789) for 60 min. Protein bands were analyzed by an ECL detection kit (Beyotime). Pictures were taken by Gel imaging system (Bio-Rad), then imagJ analized.
Statistical Analysis
All our data were obtained from three independent experiments. Statistical data was analyzed by SPSS 19.0 (IBM) and expressed as means ± standards deviation (SD). The differences among two groups were analyzed by Student’s t-tests. One-way analysis of variance (ANOVA) was performed to assess the differences among multiple groups. The p values less than 0.05 were considered significant.
Results
PVT1 Silencing Inhibited Neuronal Cell Apoptosis and Neuroinflammation in Epilepsy Cell Model
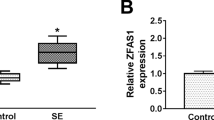
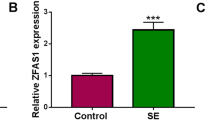
Magnesium-free-induced refractory epilepsy cell model was employed to assess the function of PVT1 in epilepsy. We first found that magnesium-free treatment resulted in increased PVT1 expression in SH-SY5Y cells (Fig. 1A). To probe the function of PVT1 in regulating epilepsy progression, we induced PVT1 knockdown by transfecting sh-PVT1 into SH-SY5Y cells (Fig. 1B). As revealed in Fig. 1C, sh-PVT1 transfection attenuated magnesium-free induced increased PVT1 expression in SH-SY5Y cells. The result of MTT assay subsequently revealed that the cell viability was remarkably suppressed by magnesium-free treatment, which was abrogated by PVT1 knockdown (Fig. 1D). In addition, magnesium-free treatment led to elevated SH-SY5Y cell apoptosis, while it was abolished by PVT1 silencing (Fig. 1E). Similarly, Western blot assay found that sh-PVT1 decreased the level of pro-apoptotic proteins (Bax and cleaved-caspase 3), and increased the anti-apoptotic protein Bcl-2 level in magnesium-free treatment in SH-SY5Y cells (Fig. 1F). Furthermore, leakage of LDH, a well-demonstrated sign of cytotoxicity [27], was remarkably increased in magnesium-free treated SH-SY5Y cells, which was abolished by PVT1 knockdown (Fig. 1G). PVT1 silencing also significantly inhibited the secretion of inflammatory cytokines (TNF-α, IL-1β and IL-6) in epileptic cell models (Fig. 1H). In summary, PVT1 promoted the neuronal cell apoptosis and neuroinflammation in magnesium-free induced SH-SY5Y cells.
PVT1 silencing inhibited neuronal cell injury and neuroinflammation in epilepsy cell model. A PVT1 expression in SH-SY5Y cells after magnesium-free treatment was analyzed by qRT-PCR. B PVT1 expression in SH-SY5Y cells transfected with sh-NC or sh-PVT1 was examined by qRT-PCR. PVT1 knockdown was induced in epilepsy cell model. C qRT-PCR was conducted to assess PVT1 expression. D MTT assay was conducted to assess cell viability. E Cell apoptosis was assessed using TUNEL staining. Scale bar, 100 µm. F Apoptosis-related protein levels were determined using western blot. G LDH level was analyzed by kits. H ELISA was employed to examine inflammatory cytokines secretions. Data were expressed as mean ± SD. All our data were obtained from three independent experiments. *P < 0.05, ** P < 0.01, ***P < 0.001
LncRNA PVT1 Suppressed miR-488-3p Expression by Directly Targeting miR-488-3p
It has been widely described that lncRNA achieves biological functions by sponging miRNA, herein we induced miR-488-3p overexpression/knockdown by transfecting miR-488-3p mimics/inhibitor into cells (Fig. 2A). We found through the starBase database that PVT1 had binding sites to miR-488-3p (Fig. 2B). To confirm the targeting relationship between PVT1 and miR-488-3p, dual luciferase reporter gene assay was subsequently employed. It was revealed that PVT1 directly bound to miR-488-3p (Fig. 2C). Additionally, we noticed that the level of miR-488-3p was significantly reduced by magnesium-free treatment (Fig. 2D). In addition, miR-488-3p in both control cells and model cells was significantly up-regulated by sh-PVT1 transfection (Fig. 2E–F). In total, PVT1 targeted miR-488-3p to negatively regulate miR-488-3p level.
LncRNA PVT1 suppressed miR-488-3p expression by directly targeting miR-488-3p in SH-SY5Y cells. A MiR-488-3p expression in SH-SY5Y cells after miR-488-3p overexpression and miR-488-3p inhibition was assessed by qRT-PCR. B The binding sites between PVT1 and miR-488-3p was analysed by Starbase software. C Dual luciferase reporter gene assay was carried out to verify the binding relationship between PVT1 and miR-488-3p. D MiR-488-3p level in SH-SY5Y cells following magnesium-free treatment was analyzed by qRT-PCR. E PVT1 knockdown was induced in SH-SY5Y cells, and miR-488-3p expression was examined by qRT-PCR. F MiR-488-3p expression in epilepsy model cells following sh-NC or sh-PVT1 transfection was assessed using qRT-PCR. Data were expressed as mean ± SD. All our data were obtained from three independent experiments. *P < 0.05, ** P < 0.01, ***P < 0.001
MiR-488-3p Inhibited Neuronal Cell Apoptosis and Neuroinflammation in Epilepsy Cell Model in SH-SY5Y Cells
To probe the function of miR-488-3p in epilepsy, we induced miR-488-3p overexpression or knockdown in model cells (Fig. 3A). The result of MTT assay subsequently revealed that miR-488-3p overexpression remarkably enhanced cell viability of model cells, while miR-488-3p inhibition presented the opposite effect (Fig. 3B). Additionally, cell apoptosis of epilepsy model cells was obviously suppressed by miR-488-3p overexpression, while the apoptosis was aggravated by miR-488-3p knockdown (Fig. 3C). As expected, Bax and cleaved-caspase 3 levels in epilepsy model cells were obviously downregulated by miR-488-3p overexpression, while Bcl2 level was upregulated, and miR-488-3p inhibition presented the opposite effects (Fig. 3D). Furthermore, the up-regulated miR-488-3p memorably inhibited LDH secretion in model cells, and miR-488-3p inhibition presented the opposite effect (Fig. 3E). It was also found that overexpression of miR-488-3p remarkably reduced inflammatory cytokines TNF-α, IL-1β and IL-6 secretions in model cells, while miR-488-3p inhibition promoted the secretion of these inflammatory cytokines (Fig. 3F). Collectively, miR-488-3p overexpression markedly repressed neuronal cell apoptosis and neuroinflammation in epilepsy cell model, while miR-488-3p inhibition presented the opposite effects, indicating the protective effects of miR-488-3p on epilepsy.
MiR-488-3p inhibited neuronal cell injury and neuroinflammation in epilepsy cell model. A qRT-PCR was employed to analyze miR-488-3p expression. B MTT assay was conducted to assess cell viability. C Cell apoptosis was assessed using TUNEL staining. Scale bar, 100 µm. D Western blot was conducted to assess apoptosis-related protein levels. E LDH level was analyzed by kits. F ELISA was employed to examine inflammatory cytokines secretions. Data were expressed as mean ± SD. All our data were obtained from three independent experiments. *P < 0.05, ** P < 0.01, ***P < 0.001
PVT1 Promoted Neuronal Cell Injury and Neuroinflammation by Targeting miR-488-3p in Epilepsy Cell Model
To evaluate the function of miR-488-3p on PVT1-mediated biological effects on epilepsy in vitro, magnesium-free treated cells were co-transfected with sh-PVT1 and miR-488-3p inhibitor. As revealed in Fig. 4A, miR‐488-3p was markedly up-regulated by sh-PVT1 transfection, which was neutralized by miR-488-3p inhibitor. In addition, miR-488-3p inhibition neutralized the beneficial effect of PVT1 silencing on cell viability of model cells (Fig. 4B). Meanwhile, PVT1 suppression inhibited model cell apoptosis, which was restored by miR-488-3p inhibition as well (Fig. 4C). Besides, miR-488-3p inhibition remarkably eliminated the effects of PVT1 down-regulation on apoptosis-related factors in epilepsy model cells (Fig. 4D). Besides, we also found that miR-488-3p inhibition offset the inhibitory effect of PVT1 silencing on LDH and inflammatory cytokines secretions in magnesium-free induced cells (Fig. 4E–F). In conclusion, miR-488-3p inhibition neutralized the inhibitory effects of PVT1 knockdown on neuronal cell injury and neuroinflammation in epilepsy cell model.
PVT1 promoted neuronal cell injury and neuroinflammation by targeting miR-488-3p in epilepsy cell model. A qRT-PCR was employed to analyze miR-488-3p expression. B MTT assay was conducted to assess cell viability. C Cell apoptosis was assessed using TUNEL staining. Scale bar, 100 µm. D Apoptosis-related protein levels were determined using western blot. E LDH level was analyzed by kits. F Inflammatory cytokines secretions were analyzed by ELISA. Data were expressed as mean ± SD. All our data were obtained from three independent experiments. *P < 0.05, ** P < 0.01, ***P < 0.001
MiR-488-3p Targeted FOXD3 to Negatively Regulate FOXD3 Expression
Herein, it was observed that miR-488-3p had binding sites to FOXD3 predicted by Starbase database (Fig. 5A). Dual luciferase reporter gene assay subsequently displayed that miR‐488-3p directly bound to FOXD3 (Fig. 5B). As revealed in Fig. 5C–D, FOXD3 expression was significantly elevated in epilepsy model cells. In addition, FOXD3 expression in both control cells and magnesium-free treated cells was markedly reduced following miR-488-3p overexpression (Fig. 5E–H). In total, miR-488-3p suppressed FOXD3 expression by directly targeting FOXD3.
MiR-488-3p targeted FOXD3 to negatively regulate FOXD3 expression A Starbase software was applied to predict the binding site between miR-488-3p and FOXD3. B Dual luciferase reporter gene assay was employed to verify the binding relationship between PVT1 and miR-488-3p. C–D FOXD3 expression in SH-SY5Y cells following magnesium-free treatment was examined by qRT-PCR and western blot. E–F FOXD3 expression in SH-SY5Y cells after mimics NC or miR-488-3p mimics transfection was examined by qRT-PCR and western blot. G–H FOXD3 expression in epilepsy model cells after mimics NC or miR-488-3p mimics transfection was analyzed via qRT-PCR and western blot. Data were expressed as mean ± SD. All our data were obtained from three independent experiments. *P < 0.05, ** P < 0.01, ***P < 0.001
MiR-488-3p Suppressed Neuronal cell and Neuroinflammation by Downregulating FOXD3 in Refractory Epilepsy Cell Model
To probe the effect of miR-488-3p/FOXD3 axis on neuronal cell injury and neuroinflammation in epilepsy, we induced miR-488-3p overexpression and FOXD3 overexpression in epilepsy model cells. Firstly, FOXD3 was notably increased by pcDNA 3.1 FOXD3 (Fig. 6A–B). As demonstrated in Fig. 6C, FOXD3 overexpression neutralized the effect of miR-488-3p overexpression on the viability of epilepsy model cells. Additionally, the up-regulated FOXD3 abrogated the inhibitory effect of miR-488-3p overexpression on cell apoptosis in magnesium-free treated cells (Fig. 6D). Consistently, FOXD3 overexpression eliminated the inhibitory effect of miR-488-3p overexpression on Bax and cleaved-caspase 3 levels and the promoting effect on Bcl-2 level (Fig. 6E). It was also found that the inhibitory effect of miR-488-3p overexpression on LDH and inflammatory cytokines secretions in model cells was restored by FOXD3 overexpression (Fig. 6F–G). Furthermore, as FOXD3 could regulate the neuron function by inhibiting SCN2A. Herein, we found that miR-488-3p overexpression reduced FOXD3 expression and elevated SCN2A expression in model cells, while the effects of miR-488-3p overexpression were neutralized by FOXD3 overexpression (Fig. 6H–J). In conclusion, miR-488-3p overexpression inhibited magnesium-free induced neuronal cell injury and neuroinflammation by regulation of FOXD3/SCN2A pathway.
MiR-488-3p suppressed neuronal cell injury and neuroinflammation by downregulating FOXD3 in refractory epilepsy cell model. A–B FOXD3 overexpression was induced in cells, and FOXD3 expression was examined by qRT-PCR and western blot. C MTT assay was conducted to assess cell viability. D Cell apoptosis was assessed using TUNEL staining. Scale bar, 100 µm. E Western blot was conducted to assess apoptosis-related protein levels. F LDH level was analyzed by kits. G ELISA was employed to examine inflammatory cytokines secretions. H–J FOXD3 and SCN2A expressions were assessed by qRT-PCR and western blot. Data were expressed as mean ± SD. All our data were obtained from three independent experiments. *P < 0.05, ** P < 0.01, ***P < 0.001
PVT1 Sponged miR-488-3p to Regulate FOXD3/SCN2A Pathway in Epileptic Rats
To confirm the role of PVT1/miR-488-3p/FOXD3/SCN2A axis in epilepsy, epileptic rats received intrahippocampal injections of miR-488-3p inhibitor and sh-PVT1. It could be seen that sh-PVT1 notably decreased the level of PVT1 in the hippocampus of epileptic rats, and the inhibition of miR-488-3p had no effect on PVT1 expression (Fig. 7A). We observed that PVT1 silencing remarkably up-regulated miR-488-3p expression in the hippocampus of epileptic rats, which was neutralized by miR-488-3p knockdown (Fig. 7B). It was also observed that PVT1 knockdown resulted in reduced FOXD3 expression and increased SCN2A expression in the hippocampus of epileptic rats, while these changes were abolished by miR-488-3p knockdown (Fig. 7C–E). In addition, it turned out that the frequency of epileptic seizures in epilepsy model group was significantly increased, and PVT1 knockdown significantly reduced seizure frequency in epileptic rats, while miR-488-3p inhibition co-transfection reversed the effect of PVT1 knockdown (Fig. 7F). Results from Nissl staining displayed that neuronal damage in hippocampal CA1 and CA3 regions of epileptic rats was obviously improved by PVT1 silencing, which was reversed by miR-488-3p inhibition as well (Fig. 7G). Meanwhile, miR-488-3p inhibition remarkably eliminated the effects of PVT1 silencing on apoptosis-related proteins in hippocampus (Fig. 7H). In addition, miR-488-3p inhibition abrogated the inhibitory effect of PVT1 knockdown on LDH, TNF-α, IL-1β and IL-6 levels in the hippocampus of epileptic rats (Fig. 7I–J). All these results suggested that PVT1 silencing relieved neuronal cell injury and neuroinflammation in epileptic rats by modulating miR-488-3p/FOXD3/SCN2A.
PVT1 sponged miR-488-3p to regulate FOXD3/SCN2A pathway in epileptic rats. A–D qRT-PCR was employed to examine PVT1, miR-488-3p, FOXD3 and SCN2A expressions in hippocampus. E FOXD3 and SCN2A levels in hippocampus were evaluated by western blot. F The average seizure frequency in rats was calculated and presented. G Nissl staining was applied to evaluate neuronal cell damage in hippocampus. Scale bar, 50 µm. H Western blot was conducted to assess apoptosis-related protein levels in hippocampus. I LDH level in hippocampus was analyzed by kits. J Inflammatory cytokines secretions in hippocampus were analyzed by ELISA. Data were expressed as mean ± SD. n = 8. *P < 0.05, ** P < 0.01, ***P < 0.001
Discussion
Epilepsy is a neurological disease caused by abnormal synchronous discharge of brain neurons, and its clinical feature is a transient dysfunction of the central nervous system [28]. Repeated episodes cause brain neuron damage or even necrosis, which leads to neuronal cell proliferation disorders, and then results in the further deterioration of epilepsy [7]. Inflammation is related to susceptibility to epilepsy and increases the frequency of seizures in epilepsy patients [29]. The above-mentioned problems are the root causes that make epilepsy difficult to treat. Our results revealed that PVT1 regulated FOXD3/SCN2A pathway by targeting miR-488-3p, thereby promoting neuronal cell injury and neuroinflammation resulted from epilepsy, which provided a new strategy for epilepsy treatment.
It has been widely reported that various lncRNAs are dysregulated and are closely related to epilepsy progression [30, 31]. It was observed that there were 279 dysregulated lncRNAs in the epilepsy mouse model compared with control mice [30]. Recently, some studies have emphasized the function of PVT1 in regulation of neuronal cell death and inflammatory response. It was previously displayed that PVT1 silencing significantly reduced the cerebral infarct size of stroke model mice [32]. In addition, PVT1 knockdown was reported to attenuate the inflammation in asthma [33]. Herein, we found that PVT1 was markedly upregulated in magnesium-free-induced epilepsy cell model. Our results also proved that PVT1 silencing increased cell viability, repressed the apoptosis and inflammatory response in epilepsy. It’s suggested that PVT1 is a risking factor affecting epilepsy development.
The hypothesis of competing endogenous RNA (ceRNA) provides a new direction for the regulation mechanism of lncRNA [34]. For instance, lncRNA UCA1 was reported to inhibit inflammation in epilepsy via regulation of miR-203 [35]. Nevertheless, whether PVT1 achieves its biological role in epilepsy via functioning as miRNA sponge is largely unknown. As previously reported, miR-488 overexpression repressed the secretion of inflammatory factors in LPS-treated endometrial epithelial cells [36]. It was found that miR-488-3p overexpression could suppress oxygen glucose deprivation/reoxygenation-induced neuronal cell death [19]. We confirmed the binding relationship between PVT1 and miR-488-3p in SH-SY5Y cells. Additionally, our research results showed for the first time that PVT1 promoted the neuronal cell injury and neuroinflammation in epilepsy cell model by targeting miR-488-3p.
As widely reported, dysregulated miRNAs repress genes expressions by binding mRNA target transcripts, thus regulating epilepsy progression [37]. FOXD3, as a transcription factor, has been proved to be indispensable for maintaining the self-renewal and pluripotency of early neural crest-derived progenitor cells [38]. As well, FOXD3 has also been reported to promote the cell viability and suppressed the apoptosis of the hypoxia/reoxygenation-treated neuronal cell cells [39]. More importantly, it was reported that FOXD3 achieved its role in epilepsy by suppressing SCN2A expression [24]. A large part of the sodium current in the central nervous system comes from NaV1.2 sodium channel, which is the post-transcriptional product of SCN2A [40]. SCN2A is linked to refractory epilepsy [41]. Similarly, [24], we demonstrated that FOXD3 was markedly upregulated in epilepsy, while SCN2A expression was decreased. In addition, our results revealed that FOXD3 was a downstream target of miR-488-3p, and we further confirmed that the effects of miR-488-3p on epilepsy cell model were mediated by FOXD3/SCN2A. Moreover, we found that PVT1 deteriorated the neuronal cell apoptosis and neuroinflammation through miR-488-3p/FOXD3/SCN2A axis. Notably, by using the database, it was predicted that miR-488-3p had a potential binding site to IL-1β, suggesting that miR-488-3p may also regulate neuronal inflammatory response and neuronal toxicity in epilepsy by directly inhibiting IL-1β. This possibility needs to be further explored.
Taken together, PVT1 promoted neuronal cell injury and inflammatory response through inhibiting miR-488-3p then further regulating FOXD3/SCN2A pathway in epilepsy. Our research provided a hopeful strategy for epilepsy treatment.
Data Availability
Enquiries about data availability should be directed to the authors.
Abbreviations
- ANOVA:
-
Analysis of variance
- Bax:
-
Bcl-2-associated X,
- Bcl-2:
-
B-cell lymphoma-2
- ceRNA:
-
Competing endogenous RNA
- ELISA:
-
Enzyme linked immunosorbent assay
- FOXD3:
-
Forkhead box D3
- IL:
-
Interleukin
- LDH:
-
Lactate dehydrogenase
- lncRNA:
-
Long non-coding RNA
- miR:
-
MicroRNA
- MTT:
-
3-(4, 5-Dimethylthiazolyl2)-2, 5-diphenyltetrazolium bromide
- PVT1:
-
Plasmacytoma variant translocation 1
- SCN2A:
-
Sodium voltage-gated channel alpha subunit 2
- SD:
-
Standard deviation
- TNF:
-
Tumor necrosis factor
- TUNEL:
-
TdT-mediated dUTP nick-end labeling
- qRT-PCR:
-
Quantitative real-time polymerase chain reaction
References
Stafstrom CE, Carmant L (2015) Seizures and epilepsy: an overview for neuroscientists. Cold Spring Harb Perspect Med 5:a022426
Puri I, Dash D, Padma MV, Tripathi M (2018) Quality of life and its determinants in adult drug refractory epilepsy patients who were not candidates for epilepsy surgery: a correlational study. J Epilepsy Res 8:81–86
Yang N, Guan QW, Chen FH, Xia QX, Yin XX, Zhou HH, Mao XY (2020) Antioxidants targeting mitochondrial oxidative stress: promising neuroprotectants for epilepsy. Oxid Med Cell Longev 2020:6687185
Wang HK, Yan H, Wang K, Wang J (2017) Dynamic regulation effect of long non-coding RNA-UCA1 on NF-kB in hippocampus of epilepsy rats. Eur Rev Med Pharmacol Sci 21:3113–3119
Li J, Li Z, Zheng W, Li X, Wang Z, Cui Y, Jiang X (2017) LncRNA-ATB: an indispensable cancer-related long noncoding RNA. Cell Prolif 50:e12381
Cai X, Long L, Zeng C, Ni G, Meng Y, Guo Q, Chen Z, Li Z (2020) LncRNA ILF3-AS1 mediated the occurrence of epilepsy through suppressing hippocampal miR-212 expression. Aging (Albany NY) 12:8413–8422
Wan Y, Yang ZQ (2020) LncRNA NEAT1 affects inflammatory response by targeting miR-129-5p and regulating Notch signaling pathway in epilepsy. Cell Cycle 19:419–431
Zhao MW, Qiu WJ, Yang P (2020) SP1 activated-lncRNA SNHG1 mediates the development of epilepsy via miR-154-5p/TLR5 axis. Epilepsy Res 168:106476
Zhang M, Yang H, Chen Z, Hu X, Wu T, Liu W (2021) Long noncoding RNA X-inactive-specific transcript promotes the secretion of inflammatory cytokines in LPS stimulated astrocyte cell via sponging miR-29c-3p and regulating nuclear factor of activated T cell 5 expression. Front Endocrinol 12:573143
Zhang H, Tao J, Zhang S, Lv X (2020) LncRNA MEG3 reduces hippocampal neuron apoptosis via the PI3K/AKT/mTOR pathway in a rat model of temporal lobe epilepsy. Neuropsychiatr Dis Treat 16:2519–2528
Colombo T, Farina L, Macino G, Paci P (2015) PVT1: a rising star among oncogenic long noncoding RNAs. Biomed Res Int 2015:304208
Xue W, Chen J, Liu X, Gong W, Zheng J, Guo X, Liu Y, Liu L, Ma J, Wang P, Li Z, Xue Y (2018) PVT1 regulates the malignant behaviors of human glioma cells by targeting miR-190a-5p and miR-488-3p. Biochim Biophys Acta Mol Basis Dis 1864:1783–1794
Zhao T, Ding Y, Li M, Zhou C, Lin W (2019) Silencing lncRNA PVT1 inhibits activation of astrocytes and increases BDNF expression in hippocampus tissues of rats with epilepsy by downregulating the Wnt signaling pathway. J Cell Physiol 234(9):16054–16067
Bartel DP (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116:281–297
Henshall DC, Hamer HM, Pasterkamp RJ, Goldstein DB, Kjems J, Prehn JHM, Schorge S, Lamottke K, Rosenow F (2016) MicroRNAs in epilepsy: pathophysiology and clinical utility. Lancet Neurol 15:1368–1376
Wang W, Guo Y, He L, Chen C, Luo J, Ma Y, Li J, Yang Y, Yang Q, Du C, Zhang Y, Li Z, Xu X, Tian X, Wang X (2018) Overexpression of miRNA-137 in the brain suppresses seizure activity and neuronal excitability: a new potential therapeutic strategy for epilepsy. Neuropharmacology 138:170–181
Hao Y, Zhang D, Guo Y, Fu Z, Yu D, Guan G (2020) miR-488-3p sponged by circ-0000495 and mediated upregulation of TROP2 in head and neck squamous cell carcinoma development. J Cancer 11:3375–3386
Wen Z, Shen Q, Zhang H, Su Y, Zhu Z, Chen G, Peng L, Li H, Du C, Xie H, Xu X, Tang W (2019) Circular RNA CCDC66 targets DCX to regulate cell proliferation and migration by sponging miR-488-3p in Hirschsprung’s disease. J Cell Physiol 234:10576–10587
Zhou L, Yang W, Yao E, Li H, Wang J, Wang K, Zhong X, Peng Z, Huang X (2021) MicroRNA-488-3p regulates neuronal cell death in cerebral ischemic stroke through vacuolar protein sorting 4B (VPS4B). Neuropsychiatr Dis Treat 17:41–55
Zhou W, Wang Y, Wu R, He Y, Su Q, Shi G (2017) MicroRNA-488 and -920 regulate the production of proinflammatory cytokines in acute gouty arthritis. Arthritis Res Ther 19:203
Wu XZ, Cui HP, Lv HJ, Feng L (2019) Knockdown of lncRNA PVT1 inhibits retinoblastoma progression by sponging miR-488-3p. Biomed Pharmacother 112:108627
Li Y, Li S, Luo Y, Liu Y, Yu N (2017) LncRNA PVT1 regulates chondrocyte apoptosis in osteoarthritis by acting as a sponge for miR-488-3p. DNA Cell Biol 36:571–580
Krishnakumar R, Chen AF, Pantovich MG, Danial M, Parchem RJ, Labosky PA, Blelloch R (2016) FOXD3 regulates pluripotent stem cell potential by simultaneously initiating and repressing enhancer activity. Cell Stem Cell 18:104–117
Xiang J, Wen F, Zhang L, Zhou Y (2018) FOXD3 inhibits SCN2A gene transcription in intractable epilepsy cell models. Exp Neurol 302:14–21
Shen Y, Peng W, Chen Q, Hammock BD, Liu J, Li D, Yang J, Ding J, Wang X (2019) Anti-inflammatory treatment with a soluble epoxide hydrolase inhibitor attenuates seizures and epilepsy-associated depression in the LiCl-pilocarpine post-status epilepticus rat model. Brain Behav Immun 81:535–544
Ihara Y, Tomonoh Y, Deshimaru M, Zhang B, Uchida T, Ishii A, Hirose S (2016) Retigabine, a Kv7.2/Kv7.3-channel opener, attenuates drug-induced seizures in knock-in mice harboring Kcnq2 mutations. PLoS ONE 11:e0150095
Mohamed NV, Plouffe V, Rémillard-Labrosse G, Planel E, Leclerc N (2014) Starvation and inhibition of lysosomal function increased tau secretion by primary cortical neurons. Sci Rep 4:5715
McCormick DA, Contreras D (2001) On the cellular and network bases of epileptic seizures. Annu Rev Physiol 63:815–846
Scheid R, Teich N (2007) Neurologic manifestations of ulcerative colitis. Eur J Neurol 14:483–493
Jang Y, Moon J, Lee ST, Jun JS, Kim TJ, Lim JA, Park BS, Yu JS, Park DK, Yang AR, Park KI, Jung KY, Kim M, Jung KH, Jeon D, Chu K, Lee SK (2018) Dysregulated long non-coding RNAs in the temporal lobe epilepsy mouse model. Seizure 58:110–119
Luo ZH, Walid AA, Xie Y, Long H, Xiao W, Xu L, Fu Y, Feng L, Xiao B (2019) Construction and analysis of a dysregulated lncRNA-associated ceRNA network in a rat model of temporal lobe epilepsy. Seizure 69:105–114
Lu J, Xu F, Lu H (2020) LncRNA PVT1 regulates ferroptosis through miR-214-mediated TFR1 and p53. Life Sci 260:118305
Ma L, Zhang Q, Hao J, Wang J, Wang C (2020) LncRNA PVT1 exacerbates the inflammation and cell-barrier injury during asthma by regulating miR-149. J Biochem Mol Toxicol 34:e22563
Peng WX, Koirala P, Mo YY (2017) LncRNA-mediated regulation of cell signaling in cancer. Oncogene 36:5661–5667
Yu Q, Zhao MW, Yang P (2020) LncRNA UCA1 suppresses the inflammation via modulating miR-203-mediated regulation of MEF2C/NF-κB signaling pathway in epilepsy. Neurochem Res 45:783–795
Liu J, Guo S, Jiang K, Zhang T, Zhiming W, Yaping Y, Jing Y, Shaukat A, Deng G (2020) miR-488 mediates negative regulation of the AKT/NF-κB pathway by targeting Rac1 in LPS-induced inflammation. J Cell Physiol 235:4766–4777
Liu AH, Wu YT, Wang YP (2017) MicroRNA-129-5p inhibits the development of autoimmune encephalomyelitis-related epilepsy by targeting HMGB1 through the TLR4/NF-kB signaling pathway. Brain Res Bull 132:139–149
Mundell NA, Plank JL, LeGrone AW, Frist AY, Zhu L, Shin MK, Southard-Smith EM, Labosky PA (2012) Enteric nervous system specific deletion of Foxd3 disrupts glial cell differentiation and activates compensatory enteric progenitors. Dev Biol 363:373–387
Li R, Zhao K, Ruan Q, Meng C, Yin F (2020) The transcription factor Foxd3 induces spinal cord ischemia-reperfusion injury by potentiating microRNA-214-dependent inhibition of Kcnk2. Exp Mol Med 52:118–129
Meisler MH, O’Brien JE, Sharkey LM (2010) Sodium channel gene family: epilepsy mutations, gene interactions and modifier effects. J Physiol 588:1841–1848
Fukuma G, Oguni H, Shirasaka Y, Watanabe K, Miyajima T, Yasumoto S, Ohfu M, Inoue T, Watanachai A, Kira R, Matsuo M, Muranaka H, Sofue F, Zhang B, Kaneko S, Mitsudome A, Hirose S (2004) Mutations of neuronal voltage-gated Na+ channel alpha 1 subunit gene SCN1A in core severe myoclonic epilepsy in infancy (SMEI) and in borderline SMEI (SMEB). Epilepsia 45:140–148
Acknowledgements
We would like to give our sincere gratitude to the reviewers for their constructive comments.
Funding
This work was supported by the Natural Science Foundation of Hunan Province (Grant No. 2021JJ30961).
Author information
Authors and Affiliations
Contributions
FW and JX: wrote the main manuscript text and ZT, DH and YJ: prepared figures. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors agree with the presented findings, have contributed to the work, and declare no conflict of interest.
Ethical approval
All animal experimental procedures were reviewed and approved by The Second Xiangya Hospital of Central South University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wen, F., Tan, Z., Huang, D. et al. LncRNA PVT1 Promotes Neuronal Cell Apoptosis and Neuroinflammation by Regulating miR-488-3p/FOXD3/SCN2A Axis in Epilepsy. Neurochem Res 48, 895–908 (2023). https://doi.org/10.1007/s11064-022-03801-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-022-03801-y