Abstract
Dehydrocorybulbine (DHCB), an alkaloid from Corydalis yanhusuo. W.T, has been identified as a dopamine receptor antagonist. We extended our assessment of its pharmacological profile and found that DHCB exhibits high to moderate binding affinities to sigma 1 and 2 receptors, serotonin 5-HT7 receptor, and histamine H2 receptors. This led us to evaluate DHCB properties in pharmacological (apomorphine and MK-801) animal models of schizophrenia in mice. The pharmacological profile of DHCB was screened through radioligand receptor binding assays. Single dose of DHCB reversed the locomotor hyperactivity, stereotypy, and prepulse inhibition deficits induced by the dopaminergic agonist apomorphine. DHCB also reversed the depressive-like behavior and memory deficit induced by the glutamatergic antagonist MK-801 in the forced swim and the novel object recognition assays, respectively. These results indicate that DHCB effectively improves schizophrenia-like behavioral deficits that are induced by the disruption of dopaminergic and glutamatergic systems. The effectiveness of DHCB in reversing responses that mimic negative and cognitive deficits of schizophrenia might suggest that its anti-schizophrenia effects are mediated through modulating the activities of several receptor particularly sigma 1, sigma 2, 5-HT7 and dopamine receptors. Our study casts DHCB as a promising lead for therapeutic treatment of schizophrenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia is a mental disorder that affects 1% of the world population and is characterized by a breakdown of the thought processes and by poor emotional responsiveness [1]. Patients suffer from three major classes of symptoms: positive symptoms (delusions, hallucinations, bizarre speech and thought); negative symptoms (anhedonia, affective flattening, socially withdrawal) and cognitive deficits (impairments in attention, learning, and memory) [2].
Although a significant progress has been made, the etiology and pathophysiology of schizophrenia remain largely unknown, and there are no diagnostic tests, or biological markers, to assist in defining the onset and follow illness progression. The dopamine hypothesis first emerged in relation to pharmacological evidence—specifically the ability of dopamine antagonists to reverse psychotic symptoms [3]. The glutamate hypothesis then emerged, which relies on the hypofunction of glutamatergic signaling via N-methyl-d-aspartate (NMDA) receptors in schizophrenia [4]. It was based on the observation that blockade of NMDA receptors by non-competitive antagonist such as phencyclidine (PCP) or ketamine closely mimics the complete spectrum of schizophrenic symptoms in particular with negative and cognitive deficits [5, 6]. Beyond the dopamine and glutamate hypotheses, several non-exclusive hypotheses have been proposed based on epidemiological, genetic, brain imaging, postmortem or pharmacological studies in human or animal models.
Current drugs are classified into typical and atypical antipsychotics. The typical antipsychotics were the first to be developed and are mostly dopamine D2 receptor antagonists. They are still the first line of defense but show limited success in treating negative or cognitive symptoms and are often plagued with extrapyramidal dysfunction. The atypical antipsychotics are newer and are more effective at treating negative symptoms. They have affinities for a broad range of receptors often involving serotonin, muscarinic, histamine and α adrenergic antagonisms although they may also interact with the D2 receptor. The most efficient antipsychotic may be the atypical clozapine which has a broad range of activities in particular at the D4 and 5-HT2 receptors but is also plagued by deleterious side effects.
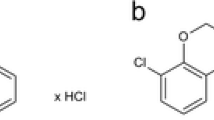
Our previous study identified the alkaloid dehydrocorybulbine (DHCB) (Fig. 1), isolated from Corydalis yanhusuo. W.T, as an analgesic compound acting at least in part as a dopamine receptor antagonist [7]. Dopamine receptor antagonists are used as the target of antipsychotics [8, 9]. We extended our analysis of DHCB pharmacological profile and found that it carries binding activities at 5-HT7 and sigma receptors. Therefore, we evaluated DHCB in vivo antipsychotic efficacy in apomorphine, a dopamine receptor agonist, as well as MK-801, a NMDA receptor antagonist, induced deficits that reflect schizophrenic symptoms in mice.
Experimental Procedures
Receptor Profiling
The detailed experimental protocols for the radioligand receptor binding assays are available on the National Institute of Mental Health (NIMH) Psychoactive Drug Screening Program (PDSP) website at http://pdsp.med.unc.edu/UNC-CH%20Protocol%20Book.pdf [10].
Animals
Male Swiss Webster mice (age 8–12 weeks, Charles River, Wilmington, MA) were used in the experiments. Mice were group-housed and maintained on a 12-h light/dark cycle (light on at 7:00 am) with food and water available ad libitum. All experimental procedures were approved by the Institutional Animal Care and Use Committee of University of California, Irvine and were performed in compliance with national and institutional guidelines for the care and use of laboratory animals.
Drug Administrations
DHCB was synthesized as previously described [7]. DHCB was dissolved in saline. Apomorphine and MK-801 (Sigma-Aldrich) were dissolved in saline. DHCB (5, 10, 40 mg/kg, i.p., 5 ml/kg), apomorphine (5 mg/kg, i.p., 5 ml/kg) and MK-801 (0.2 mg/kg, i.p., 5 ml/kg) were administered with different periods of time before the assay depending on the assays.
Behavioral Testing
Apomorphine-Induced Hyperactivity
The locomotor activity was assessed as previously described [11]. Briefly, mice were placed into the open field test chamber (40 × 40 cm, Med Associates, inc.), and allowed 45 min of acclimation before the test. For DHCB (5, 10, 40 mg/kg) dose response experiment, the habituation step was skipped because of the known effect of DHCB decreasing spontaneous locomotor activity [7]. DHCB (10 mg/kg) and apomorphine (5 mg/kg) were administered 30 min and 15 min before the test, respectively. Saline was administered as control. Mice horizontal and stereotypic activities for 60 min were recorded and analyzed by Activity Monitor 5 software (Med Associates, Inc.).
Apomorphine Induced Enhanced Stereotypy
The stereotypy assay was carried out as described before [12]. Mice were individually placed in a new cage without bedding and were allowed to acclimate for 45 min before the test. DHCB (10 mg/kg) and apomorphine (5 mg/kg) were administered 30 min and 15 min before the test, respectively. Saline was administered as control. Stereotypic behaviors were observed and recorded for 10 s every minute for 30 min. Stereotypy rating scale is 0 = inactivity, 1 = grooming, 2 = locomotion, 3 = sniffing directed upward, 4 = sniffing with head down, 5 = intense sniffing in a small circumscribed area, 6 = intense sniffing with bursts of lick, 7 = constant licking or gnawing box, 8 = self-licking or biting. Rating scores for 30 min were collapsed and shown as a total stereotypy counts.
Apomorphine Induced Prepulse Inhibition (PPI) Deficit
PPI was performed as previously described [13]. Mice were tested in a startle chamber consists of a nonrestrictive Plexiglas cylinder resting on a platform inside of a ventilated and sound attenuated box. A high frequency loudspeaker inside each chamber produced background noise of 65 dB as well as the various acoustic stimuli. Vibrations of the Plexiglas cylinder caused by the body startle response of the animal are converted into analog signals by a piezoelectric accelerometer attached to the platform. A total of 65 readings are recorded at 1 ms intervals beginning at the stimulus onset. Average amplitude over this time is used as the measure of startle. Calibration was performed before every use to ensure the accuracy of the sound levels and startle measurements.
During the test, mice were placed in the startle chambers for 5 min acclimation with 65 dB background noise. The PPI session consisted of five different trials: no-stimulus trials, 3 prepulse trials and startle trials. No-stimulus trials consist of background noise only (65 dB). Startle trials consist of a 40 ms duration startle stimulus at 120 dB (p120). Prepulse trials consist of a 20 ms duration prepulse at 68 dB (pp3), 71 dB (pp6), or 77 dB (pp12), a 100 ms interstimulus interval, followed by a 40 ms duration startle stimulus at 120 dB. Test sessions began with 5 presentations of the p120 trial, followed by 10 presentations of the no-stimulus trial, p120 trials, pp3, pp6, and pp12 prepulse trials given in a pseudorandom order with an intertrial interval of 8–23 s (mean 15 s) and ending with 5 presentations of the p120 trial. DHCB (10 mg/kg) and apomorphine (5 mg/kg) were administered 55 min and 10 min before the test, respectively. Saline was administered as control. The amount of PPI is calculated as a percentage score for each acoustic prepulse intensity: % PPI = 100-([(startle response for prepulse + pulse trials)/(startle response for pulse-alone trials)] × 100). The magnitude of the response was calculated as the average response to all of the startle or prepulse trials.
MK-801 Induced Immobility
The forced swim assay was performed with slight modification as previously described [14, 15]. In brief, MK-801(0.2 mg/kg) was administered once daily for consecutive 14 days. Saline was administered as control. On day 16 (48 h after the last injection), DHCB (10 mg/kg) or saline were administered 60 min prior to the test. Mice were then placed individually in a transparent glass cylinder containing water (24 cm high, 14.5 cm diameter, 14 cm water depth) at 23–25 °C and forced to swim. Mice were videotaped for 6 min, and the immobility time (time spent passively floating) is recorded for the last 4 min, after discarding activity in the first 2 min during which an animal tries to escape. ANY-MAZE software was used to record and analyze immobility (Stoelting Co.).
MK-801 Induced Novel Object Recognition (NOR) Deficit
The novel objects recognition task was assessed as described previously [15, 16]. This task consists of a training phase and a testing phase. Before training, all mice were handled 1–2 min a day for 3 days and were habituated to the experimental apparatus 10 min a day for 3 consecutive days without objects. The experimental apparatus is a rectangular open field (20 × 40 × 20 cm, manufactured by carpentry facility, University of California, Irvine). During the training phase, DHCB (10 mg/kg) and MK-801 (0.2 mg/kg) were administered50 min and 30 min before the training session, respectively. Saline was administered as control. Mice were then placed in the experimental apparatus with two identical objects(PVC male pipe adapter, white, 1.5 inch × 2.2 inch; PVC female hose mender, green, 1.4 inch × 2.2 inch) and allowed to explore for 10 min. Exploration was defined as occurring when an animal faced an object by one inch or less or when any part of the animal body touched the object, except for the tail. The objects were thoroughly cleaned with 10% ethanol and then dried between trials to make sure no olfactory cues were present. Ninety minutes later, mice were given with the retention phase. During these retention sessions, mice were allowed to explore the experimental apparatus for 5 min in the presence of one familiar and one novel object. The location of the novel object was counterbalanced between trials. Duration and the number of times that the mice explored familiar or novel object were recorded individually. The relative exploration time was recorded and expressed by a discrimination index: [D.I. = (Tnovel − Tfamiliar)/(Tnovel+ Tfamiliar) × 100%]. Tests were video recorded and analyzed by ANY-MAZE software (Stoelting Co.).
Data Analysis
Graphpad Prism (GraphPad Software, Inc.) was used for statistical analysis. Data are presented as mean ± S.E.M. Results of locomotor activity, stereotypic behavior, forced swim test, and startle reactivity were analyzed by one way ANOVA followed by Dunnett’s post hoc tests. Results of PPI and novel object recognition were analyzed by two way ANOVA followed by Bonferroni post hoc test, and P < 0.05 was considered statistically significant.
Results
DHCB Receptor Profiling
Our previous study has shown that DHCB displays dopamine receptors antagonistic activities. D2 receptor is partially involved in the antinociceptive effects but not in the sedative effects of DHCB at low doses [7]. That suggests to us that DHCB might bind to multiple pharmacological targets. To further explore the DHCB’s pharmacological profile, DHCB was screened against a large panel of receptors, transporters and ion channels through the NIMH PDSP. The results show that DHCB has no affinity to the receptors, channels or transporters summarized in Table 1. On the other hand, DHCB is found to bind to dopamine receptors (D1-D5), α1D, α2A, α2B and α2C adrenergic receptors with low affinity (Ki > 1 μM), while exhibiting moderate affinity to the serotonin-7 receptor, sigma 1 and 2 receptors and histamine-2 receptors (100 nM < Ki < 1 μM, Table 2). DHCB showed relatively low binding affinity the dopamine receptors when compared to its high activity at these receptors [7], probably due to assay differences. DHCB pharmacological profile as a whole suggested to us that it may antipsychotic effects.
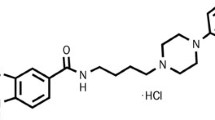
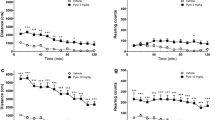
Effect of DHCB on Schizophrenia-Like Symptoms Induced by Apomorphine
We first assessed the effect of DHCB on hyperactivity and enhanced stereotypies induced by the dopamine receptor agonist apomorphine. DHCB 10 mg/kg was selected as a sub-effective dose, as determined by DHCB dose responses in the locomotor and stereotypic activities (P > 0.05, Fig. 2a, b). We previously reported that DHCB at 40 mg/kg has sedative effects [7]. Acute administration of apomorphine at 5 mg/kg induced hyper-locomotor activity in mice, as indicated by a significant increase of total distance travelled and stereotypical counts (P < 0.01, Fig. 2c, d). An acute administration of DHCB at 10 mg/kg reverses apomorphine-induced locomotor hyperactivity and stereotyped behavior (P < 0.01, Fig. 2c, d). The reversal effect of DHCB (10 mg/kg) on apomorphine (5 mg/kg) induced stereotypies was further confirmed via manual scoring (P < 0.05, Fig. 2e). These data indicate that DHCB attenuates apomorphine induced responses that reflect schizophrenia-like positive symptoms.
Effect of DHCB on apomorphine-induced responses. a Dose responses of DHCB (5, 10, 40 mg/kg) in the locomotor activity assay (n = 7–8). One way ANOVA revealed a significant drug effect (F3,26 = 11.31, P < 0.0001). Dunnett’s post hoc tests: drug vs saline, ***P < 0.001. b Dose responses of DHCB (5, 10, 40 mg/kg) in the stereotyped behaviors assay (n = 7–8). One way ANOVA revealed a significant drug effect (F3,26 = 21.74, P < 0.0001). Dunnett’s post hoc tests: drug vs saline, ***P < 0.001. c Effect of DHCB (10 mg/kg) in acute apomorphine (APO, 5 mg/kg) induced hyperactivity in the locomotor activity assay (n = 14–20). One way ANOVA revealed a significant drug effect (F3,62 = 10.94, P < 0.0001). Bonferroni post hoc test: drug vs saline, ***P < 0.001, N.S. not significant; APO + DHCB vs APO, ##P < 0.01. d Effect of DHCB (10 mg/kg) in acute apomorphine (APO, 5 mg/kg) induced increased stereotypic behavior with automatic counting (n = 14–20). One way ANOVA revealed a significant drug effect (F3,62 = 11.36, P < 0.0001). Bonferroni post hoc test: drug vs saline, **P < 0.01, N.S. not significant; APO + DHCB vs APO, ##P < 0.01. e Effect of DHCB (10 mg/kg) in acute apomorphine (APO, 5 mg/kg) induced increased stereotypic behavior with manual counting (n = 7–8). One way ANOVA revealed a significant drug effect (F3,26 = 23.26, P < 0.0001). Bonferroni post hoc test: drug vs saline, ***P < 0.001, N.S. not significant; APO + DHCB vs APO, #P < 0.05
Effect of DHCB on Schizophrenia-Like Symptoms Induced by MK-801
The NMDA receptor antagonist MK-801 is known to increase immobility in the forced swim assay. DHCB alone (10 mg/kg) displayed no significant effect on the immobility time (P > 0.05, Fig. 3a). Repeated administration of MK-801 at 0.2 mg/kg for 14 days significantly increased mice immobility time (P < 0.01, Fig. 3b). This effect is reversed by an acute administration of DHCB at 10 mg/kg (P < 0.01, Fig. 3b), which indicates that DHCB attenuates MK-801 induced responses that reflect schizophrenia-like negative symptoms.
Effect of DHCB on MK-801 induced responses. a Dose responses of DHCB (5, 10, 40 mg/kg) in the forced swim assay (n = 7–8). One way ANOVA revealed a significant drug effect (F3,25 = 8.494, P = 0.0005). Dunnett’s post hoc tests:drug vs saline, ***P < 0.001. b Effect of DHCB (10 mg/kg) in sub-chronic MK-801 (0.2 mg/kg) induced increased immobility in the forced swim assay (n = 10). One way ANOVA revealed a significant drug effect (F2,27 = 6.560, P = 0.0048). Bonferroni post hoc test: drug vs saline, ** P < 0.01, N.S. not significant; MK-801 + DHCB vs MK-801, ##P < 0.01
Effect of DHCB on Sensorimotor Gating Deficits Induced by Apomorphine
We then explored the effect of DHCB on PPI deficit induced by apomorphine. DHCB alone (10 mg/kg) was found to have no significant effect on startle reactivity (P > 0.05, Fig. 4a) nor on PPI ratio (P > 0.05, Fig. 4b). As shown in Fig. 4c, acute administration of apomorphine (5 mg/kg) significantly decreased the PPI ratio (P < 0.05, Fig. 4c). DHCB (10 mg/kg) is able to reverse the PPI deficit induced by apomorphine (P < 0.05, Fig. 4c).
Effect of DHCB on apomorphine-induced sensorimotor gating deficit. a Dose responses of DHCB (5, 10, 40 mg/kg) in the startle reactivity assessed in the prepulse inhibition (PPI) assay (n = 16). One way ANOVA revealed a significant drug effect (F3,60 = 2.962, P = 0.0392). Dunnett’s post hoc tests: drug vs saline, *P < 0.05. b Dose responses of DHCB (5, 10, 40 mg/kg) in the prepulse inhibition ratio assessed in the PPI assay (n = 15–17). Two way ANOVA revealed no significant drug effect (F3,177 = 1.351, P = 0.2595). c Effect of DHCB (10 mg/kg) in acute apomorphine (APO, 5 mg/kg) induced prepulse inhibition deficit in the PPI assay (n = 15–17). Two way ANOVA revealed a significant drug effect (F2,135 = 22.44, P < 0.001). Bonferroni post hoc test: drug vs saline, *P < 0.05, ***P < 0.001, N.S. not significant; APO + DHCB vs APO: #P < 0.05, ##P < 0.01
Effect of DHCB on MK-801 Induced Cognitive Deficits
We also investigated the effect of DHCB on object recognition deficit induced by MK-801. DHCB (10 mg/kg) did not affect object exploration during the training session nor object recognition during the retention session, when compared to saline group (P > 0.05, Fig. 5a–c). MK-801administration (0.2 mg/kg) before the training session did not affect object exploration (P > 0.05, Fig. 5d). However, MK-801 treated mice did not discriminate between novel and old objects during the retention session (P > 0.05, Fig. 5e; P < 0.001, Fig. 5f). An acute administration of DHCB (10 mg/kg) before the training session reverses the novel object recognition deficit induced by MK-801 (P < 0.05, Fig. 5e, f). Taken together, our data suggest that DHCB attenuates apomorphine and MK-801responses reflecting schizophrenia-like cognitive symptoms.
Effect of DHCB on cognitive deficit. a Dose responses of DHCB (5, 10, 40 mg/kg) in the exploration time on identical objects during training session assessed in the novel object recognition (NOR) assay (n = 6–8). Two way ANOVA revealed no significant object effect (F1,48 = 0.17, P = 0.6819). b Dose responses of DHCB (5, 10, 40 mg/kg) in the exploration time on both new and old objects during training session assessed in the NOR assay (n = 6–8). Two way ANOVA revealed a significant drug effect (F3,48 = 13.42, P < 0.001) and object effect (F1,48 = 47.20, P < 0.001).Bonferroni post hoc test: new object vs old object, *** P < 0.001, N.S. not significant. c Dose responses of DHCB (5, 10, 40 mg/kg) in the discrimination index assessed in the NOR assay (n = 6–8). One way ANOVA revealed a significant drug effect (F3,24 = 3.769, P = 0.0239). Dunnett’s post hoc tests: drug vs saline, * P < 0.05. d Effect of DHCB (10 mg/kg) during training session in MK-801 induced object recognition deficit assessed in the NOR assay (n = 8). Two way ANOVA revealed no significant object effect (F1,42 = 2.033, P = 0.1613). e Effect of DHCB (10 mg/kg) during training session MK-801 induced object recognition deficit assessed in the NOR assay (n = 8). Two way ANOVA revealed a significant drug effect (F2,42 = 3.435, P = 0.0415) and object effect (F1,42 = 11.15, P = 0.018). Bonferroni post hoc test: new object vs old object, *P < 0.05, N.S. not significant. f Effect of DHCB (10 mg/kg) in the discrimination index in MK-801 induced object recognition deficit assessed in the NOR assay (n = 7–8). One way ANOVA revealed a significant drug effect (F2,20 = 8.874, P = 0.017). Bonferroni post hoc test: drug vs saline, **P < 0.01, N.S. not significant; MK-801 + DHCB vs MK-801, N.S. not significant
Discussion
The alkaloid dehydrocorybulbine (DHCB) is known to have analgesic effect that is mediated, at least in part, through its dopamine receptor (in particular D2) blockade [7]. In this study we expanded our search for its mode of action and profiled it against a battery or receptors. In radioligand binding assays, DHCB exhibits in addition to its known antagonism at the dopamine receptors, a high binding affinity to serotonin receptor (5-HT7), sigma 1 and 2 receptors, moderate binding affinity to histamine-2 (H2) receptors and to a less extent to α1D, α2A, α2B and α2C adrenergic receptors (Table 2).
DHCB affinities to the dopamine receptors show differences when measured by binding (as in this study) or by receptor reactivity. These differences result from the assays used in this comparison. In the binding assays DHCB displaces specific antagonists while in the activity assay it displaces an agonist. It is also possible that DHCB acts as a non-competitive dopamine receptor antagonist which can be tested in a future study.
DHCB binding to the 5-HT7 receptor is of interest since a number of atypical antipsychotics including clozapine, amisulpride, lurasidone and risperidone have high affinities for 5-HT7 receptors [17,18,19,20]. These atypical antipsychotics have been shown to be effective in reversing pharmacological induced schizophrenia-like negative and cognitive symptoms. Clozapine and risperidone are known to attenuate ketamine or MK-801 induced enhanced immobility in the forced swim assay [14, 21]. Lurasidone as well as the selective 5-HT7 receptor antagonists SB-269970 and SB-656104-A have been shown to attenuate ketamine or MK-801 induced cognitive deficits in the novel object recognition, the Morris water maze, the five-choice serial reaction time task and the inhibitory avoidance assays [22,23,24,25]. The effect of lurasidone is completely blocked by 5-HT7 receptor agonist AS19, which indicating the importance of 5-HT7 receptor antagonistic activity of lurasidone against MK-801 induced deficits [24].
DHCB binding at the sigma-1 receptor suggested also an antipsychotic role for DHCB. The sigma-1 receptor (σ-1R) is known to enhance the function of NMDARs via multiple pathways such as increasing the expression, trafficking, and surface levels of NMDA receptors [26]. Sigma-1 receptor agonist fluvoxamine, donepezil and selective sigma-1 receptor agonist neurosteroid dehydroepiandrosterone-sulfate (DHEA-S) and SA4503 have been shown to improve PCP-induced novel object recognition deficit [27,28,29]. These effects are blocked by the selective sigma-1 receptor antagonist NE-100 [30]. Clinical studies have revealed that fluvoxamine improves the antipsychotics treatment against the negative and cognitive symptoms of schizophrenic patients [31, 32].
Finally, histamine 2 receptor and α2-adrenoceptors antagonists have also been shown to be involved in the treatment of schizophrenia [33, 34]. DHCB displays binding activities at these receptors. Taken together, DHCB extended receptor pharmacological profile suggested to us that it may carry antipsychotic activity and set up to test in a variety of pharmacological assays known to reflect in mice the different aspects of schizophrenia.
Systemic administrations of dopamine agonists such as apomorphine induce hyperactivity in locomotion and also stereotyped behaviors such as constant sniffing, licking and gnawing. These responses are inhibited by typical antipsychotics, which exhibit dopamine receptor antagonistic properties, such as haloperidol [35, 36] and are widely used to evaluate the effect of compounds in attenuating the positive symptoms of schizophrenia [37,38,39,40]. Therefore the attenuating effects of DHCB of apomorphine-induced hyperactivity in locomotion and stereotyped behaviors is not surprising given that DHCB blocks D1-D2 receptors [7].
Prepulse inhibition (PPI) is observed from human to rodents and has been used for measuring sensorimotor gating behavior [41, 42]. PPI deficits have been observed in schizophrenic patients. Dopamine receptor agonists are used to disrupt PPI in rodents and thus allow for evaluating the predictive validity of compounds [43]. We show that DHCB effectively attenuates apomorphine-induced PPI deficits (Fig. 4), suggesting that DHCB may have beneficial effects against schizophrenia sensory motor gating deficit.
Enhanced immobility in the forced swim test reflects affective flattening in rodents [44]. Immobility induced by repeated MK-801 treatment has been used as a promising model to assess negative symptoms of schizophrenia [14]. Object recognition deficit has been observed in schizophrenic patients [45]. Acute treatment of MK-801 induces object recognition deficit which is used for evaluating effects of compounds on cognitive deficits in schizophrenia [46]. The atypical antipsychotics such as clozapine, risperidone have been shown to attenuate NMDA receptor antagonist PCP or MK-801 induced enhanced immobility in the forced swim assay [14, 47] as well as object recognition deficit in the novel object recognition assay [48, 49]. Classical antipsychotics such as haloperidol were shown less effective in reversing negative and cognitive symptoms of schizophrenia [21, 50]. DHCB effectively attenuates MK-801-induced immobility in the forced swim assay (Fig. 3) and object recognition deficit (Fig. 5). These data indicate that DHCB can affect responses that reflect schizophrenia-like negative and cognitive symptoms and suggest that its mode of action is different from those of the classical antipsychotics.
In summary, our study reports DHCB effectiveness to ameliorate apomorphine- and MK-801 induced responses that reflect the positive, negative and cognitive schizophrenia symptoms in mice. It also shows that DHCB mode of action may be complex relying on a variety of receptors. Therefore, DHCB might be a natural compound that serves as candidate for therapeutic treatment of schizophrenia.
References
Jones CA, Watson DJ, Fone KC (2011) Animal models of schizophrenia. Br J Pharmacol 164:1162–1194
Andreasen NC (1995) Symptoms, signs, and diagnosis of schizophrenia. Lancet 346:477–481
Mueser KT, McGurk SR (2004) Schizophrenia. Lancet 363:2063–2072
Coyle JT (1996) The glutamatergic dysfunction hypothesis for schizophrenia. Harv Rev Psychiatry 3:241–253
Becker A, Peters B, Schroeder H, Mann T, Huether G, Grecksch G (2003) Ketamine-induced changes in rat behaviour: a possible animal model of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 27:687–700
Javitt DC, Zukin SR (1991) Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry 148:1301–1308
Zhang Y, Wang C, Wang L, Parks GS, Zhang X, Guo Z, Ke Y, Li KW, Kim MK, Vo B, Borrelli E, Ge G, Yang L, Wang Z, Garcia-Fuster MJ, Luo ZD, Liang X, Civelli O (2014) A novel analgesic isolated from a traditional Chinese medicine. Curr Biol 24:117–123
Seeman P (2010) Dopamine D2 receptors as treatment targets in schizophrenia. Clin Schizophr Relat Psychoses 4:56–73
Sanyal S, Van Tol HH (1997) Review the role of dopamine D4 receptors in schizophrenia and antipsychotic action. J Psychiatr Res 31:219–232
Besnard J, Ruda GF, Setola V, Abecassis K, Rodriguiz RM, Huang XP, Norval S, Sassano MF, Shin AI, Webster LA, Simeons FR, Stojanovski L, Prat A, Seidah NG, Constam DB, Bickerton GR, Read KD, Wetsel WC, Gilbert IH, Roth BL, Hopkins AL (2012) Automated design of ligands to polypharmacological profiles. Nature 492:215–220
Wang L, Alachkar A, Sanathara N, Belluzzi JD, Wang Z, Civelli O (2015) A methionine-induced animal model of schizophrenia: face and predictive validity. Int J Neuropsychopharmacol 18:pyv054
LaHoste GJ, Marshall JF (1992) Dopamine supersensitivity and D1/D2 synergism are unrelated to changes in striatal receptor density. Synapse 12:14–26
Ralph-Williams RJ, Lehmann-Masten V, Otero-Corchon V, Low MJ, Geyer MA (2002) Differential effects of direct and indirect dopamine agonists on prepulse inhibition: a study in D1 and D2 receptor knock-out mice. J Neurosci 22:9604–9611
Langen B, Dost R, Egerland U, Stange H, Hoefgen N (2012) Effect of PDE10A inhibitors on MK-801-induced immobility in the forced swim test. Psychopharmacology 221:249–259
Alachkar A, Wang L, Yoshimura R, Hamzeh AR, Wang Z, Sanathara N, Lee SM, Xu X, Abbott GW, Civelli O (2018) Prenatal one-carbon metabolism dysregulation programs schizophrenia-like deficits. Mol Psychiatry 23:282–294
Nilsson M, Hansson S, Carlsson A, Carlsson ML (2007) Differential effects of the N-methyl-d-aspartate receptor antagonist MK-801 on different stages of object recognition memory in mice. Neuroscience 149:123–130
Ishibashi T, Horisawa T, Tokuda K, Ishiyama T, Ogasa M, Tagashira R, Matsumoto K, Nishikawa H, Ueda Y, Toma S, Oki H, Tanno N, Saji I, Ito A, Ohno Y, Nakamura M (2010) Pharmacological profile of lurasidone, a novel antipsychotic agent with potent 5-hydroxytryptamine 7 (5-HT7) and 5-HT1A receptor activity. J Pharmacol Exp Ther 334:171–181
Abbas AI, Hedlund PB, Huang XP, Tran TB, Meltzer HY, Roth BL (2009) Amisulpride is a potent 5-HT7 antagonist: relevance for antidepressant actions in vivo. Psychopharmacology 205:119–128
Meltzer HY, Huang M (2008) In vivo actions of atypical antipsychotic drug on serotonergic and dopaminergic systems. Prog Brain Res 172:177–197
Roth BL, Craigo SC, Choudhary MS, Uluer A, Monsma FJ Jr, Shen Y, Meltzer HY, Sibley DR (1994) Binding of typical and atypical antipsychotic agents to 5-hydroxytryptamine-6 and 5-hydroxytryptamine-7 receptors. J Pharmacol Exp Ther 268:1403–1410
Chindo BA, Adzu B, Yahaya TA, Gamaniel KS (2012) Ketamine-enhanced immobility in forced swim test: a possible animal model for the negative symptoms of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 38:310–316
Nikiforuk A, Holuj M, Potasiewicz A, Popik P (2015) Effects of the selective 5-HT7 receptor antagonist SB-269970 on premature responding in the five-choice serial reaction time test in rats. Behav Brain Res 289:149–156
Nikiforuk A, Kos T, Fijal K, Holuj M, Rafa D, Popik P (2013) Effects of the selective 5-HT7 receptor antagonist SB-269970 and amisulpride on ketamine-induced schizophrenia-like deficits in rats. PLoS ONE 8:e66695
Horisawa T, Nishikawa H, Toma S, Ikeda A, Horiguchi M, Ono M, Ishiyama T, Taiji M (2013) The role of 5-HT7 receptor antagonism in the amelioration of MK-801-induced learning and memory deficits by the novel atypical antipsychotic drug lurasidone. Behav Brain Res 244:66–69
Horisawa T, Ishibashi T, Nishikawa H, Enomoto T, Toma S, Ishiyama T, Taiji M (2011) The effects of selective antagonists of serotonin 5-HT7 and 5-HT1A receptors on MK-801-induced impairment of learning and memory in the passive avoidance and Morris water maze tests in rats: mechanistic implications for the beneficial effects of the novel atypical antipsychotic lurasidone. Behav Brain Res 220:83–90
Pabba M, Sibille E (2015) Sigma-1 and N-methyl-d-aspartate receptors: a partnership with beneficial outcome. Mol Neruopsychiatry 1:47–51
Kunitachi S, Fujita Y, Ishima T, Kohno M, Horio M, Tanibuchi Y, Shirayama Y, Iyo M, Hashimoto K (2009) Phencyclidine-induced cognitive deficits in mice are ameliorated by subsequent subchronic administration of donepezil: role of sigma-1 receptors. Brain Res 1279:189–196
Ishima T, Fujita Y, Kohno M, Kunitachi S, Horio M, Takatsu Y, Minase T, Tanibuchi Y, Hagiwara H, Iyo M, Hashimoto K (2009) Improvement of Phencyclidine-induced cognitive deficits in mice by subsequent subchronic administration of fluvoxamine, but not sertraline. Open Clin Chem J 2:7–11
Hashimoto K, Fujita Y, Iyo M (2007) Phencyclidine-induced cognitive deficits in mice are improved by subsequent subchronic administration of fluvoxamine: role of sigma-1 receptors. Neuropsychopharmacology 32:514–521
Okuyama S, Nakazato A (1996) NE-100: a novel sigma receptor antagonist. CNS Drug Rev 2:226–237
Silver H, Aharon N, Kaplan A (2003) Add-on fluvoxamine improves primary negative symptoms: evidence for specificity from response analysis of individual symptoms. Schizophr Bull 29:541–546
Silver H, Barash I, Aharon N, Kaplan A, Poyurovsky M (2000) Fluvoxamine augmentation of antipsychotics improves negative symptoms in psychotic chronic schizophrenic patients: a placebo-controlled study. Int Clin Psychopharmacol 15:257–261
Langer SZ (2015) alpha2-adrenoceptors in the treatment of major neuropsychiatric disorders. Trends Pharmacol Sci 36:196–202
Meskanen K, Ekelund H, Laitinen J, Neuvonen PJ, Haukka J, Panula P, Ekelund J (2013) A randomized clinical trial of histamine 2 receptor antagonism in treatment-resistant schizophrenia. J Clin Psychopharmacol 33:472–478
Dias FR, de Matos LW, Sampaio Mde F, Carey RJ, Carrera MP (2012) Opposite effects of low versus high dose haloperidol treatments on spontaneous and apomorphine induced motor behavior: evidence that at a very low dose haloperidol acts as an indirect dopamine agonist. Behav Brain Res 229:153–159
Seeger TF, Seymour PA, Schmidt AW, Zorn SH, Schulz DW, Lebel LA, McLean S, Guanowsky V, Howard HR, Lowe JA 3rd et al (1995) Ziprasidone (CP-88,059): a new antipsychotic with combined dopamine and serotonin receptor antagonist activity. J Pharmacol Exp Ther 275:101–113
Ruthrich HL, Grecksch G, Matthies H (1993) Influence of beta-casomorphins on apomorphine-induced hyperlocomotion. Pharmacol Biochem Behav 44:227–231
Randrup A, Munkvad I (1967) Stereotyped activities produced by amphetamine in several animal species and man. Psychopharmacologia 11:300–310
Liu YF, Civelli O, Grandy DK, Albert PR (1992) Differential sensitivity of the short and long human dopamine D2 receptor subtypes to protein kinase C. J Neurochem 59:2311–2317
Zhou QY, Li C, Civelli O (1992) Characterization of gene organization and promoter region of the rat dopamine D1 receptor gene. J Neurochem 59:1875–1883
Swerdlow NR, Geyer MA, Braff DL (2001) Neural circuit regulation of prepulse inhibition of startle in the rat: current knowledge and future challenges. Psychopharmacology 156:194–215
Braff DL, Geyer MA, Swerdlow NR (2001) Human studies of prepulse inhibition of startle: normal subjects, patient groups, and pharmacological studies. Psychopharmacology 156:234–258
Auclair AL, Kleven MS, Besnard J, Depoortere R, Newman-Tancredi A (2006) Actions of novel antipsychotic agents on apomorphine-induced PPI disruption: influence of combined serotonin 5-HT1A receptor activation and dopamine D2 receptor blockade. Neuropsychopharmacology 31:1900–1909
Porsolt RD, Le Pichon M, Jalfre M (1977) Depression: a new animal model sensitive to antidepressant treatments. Nature 266:730–732
Gabrovska VS, Laws KR, Sinclair J, McKenna PJ (2003) Visual object processing in schizophrenia: evidence for an associative agnosic deficit. Schizophr Res 59:277–286
van der Staay FJ, Rutten K, Erb C, Blokland A (2011) Effects of the cognition impairer MK-801 on learning and memory in mice and rats. Behav Brain Res 220:215–229
Noda Y, Kamei H, Mamiya T, Furukawa H, Nabeshima T (2000) Repeated phencyclidine treatment induces negative symptom-like behavior in forced swimming test in mice: imbalance of prefrontal serotonergic and dopaminergic functions. Neuropsychopharmacology 23:375–387
Karasawa J, Hashimoto K, Chaki S (2008) D-Serine and a glycine transporter inhibitor improve MK-801-induced cognitive deficits in a novel object recognition test in rats. Behav Brain Res 186:78–83
Grayson B, Idris NF, Neill JC (2007) Atypical antipsychotics attenuate a sub-chronic PCP-induced cognitive deficit in the novel object recognition task in the rat. Behav Brain Res 184:31–38
Hashimoto K, Fujita Y, Shimizu E, Iyo M (2005) Phencyclidine-induced cognitive deficits in mice are improved by subsequent subchronic administration of clozapine, but not haloperidol. Eur J Pharmacol 519:114–117
Acknowledgement
This work was supported by Eric L. and Lila D. Nelson Chair in Neuropharmacology.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, L., Zhang, Y., Wang, C. et al. A Natural Product with High Affinity to Sigma and 5-HT7 Receptors as Novel Therapeutic Drug for Negative and Cognitive Symptoms of Schizophrenia. Neurochem Res 44, 2536–2545 (2019). https://doi.org/10.1007/s11064-019-02873-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-019-02873-7