Abstract
Mdivi-1 is a selective inhibitor of mitochondrial fission protein, Drp1, and can penetrate the blood–brain barrier. Previous studies have shown that Mdivi-1 improves neurological outcomes after ischemia, seizures and trauma but it remains unclear whether Mdivi-1 can attenuate early brain injury after subarachnoid hemorrhage (SAH). We thus investigated the therapeutic effect of Mdivi-1 on early brain injury following SAH. Rats were randomly divided into four groups: sham; SAH; SAH + vehicle; and SAH + Mdivi-1. The SAH model was induced by standard intravascular perforation and all of the rats were subsequently sacrificed 24 h after SAH. Mdivi-1 (1.2 mg/kg) was administered to rats 30 min after SAH. We found that Mdivi-1 markedly improved neurologic deficits, alleviated brain edema and BBB permeability, and attenuated apoptotic cell death. Mdivi-1 also significantly reduced the expression of cleaved caspase-3, Drp1 and p-Drp1(Ser616), attenuated the release of Cytochrome C from mitochondria, inhibited excessive mitochondrial fission, and restored the ultra-structure of mitochondria. Furthermore, Mdivi-1 reduced levels of MDA, 3-NT, and 8-OHdG, and improved SOD activity. Taken together, our data suggest that Mdivi-1 exerts neuroprotective effects against cell death induced by SAH and the underlying mechanism may be inhibition of Drp1-activated mitochondrial fission and oxidative stress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subarachnoid hemorrhage (SAH) is a devastating event with high morbidity and mortality. Recent studies have shown that early brain injury (EBI), which occurs within the first 72 h after SAH, may be the primary determinant of poor outcomes in SAH, and effective treatment against EBI has become a key goal in SAH patient care [1–4]. The pathophysiologic process by which SAH leads to EBI is complicated. It has been reported that neuronal cell apoptosis and oxidative stress after SAH may be critical to the development of EBI and might explain its serious impact on short- as well as long-term outcomes [5–7]; however, the molecular mechanisms and relationship between neuron apoptosis and oxidative stress in EBI after SAH are not entirely clear.
Mitochondria are key organelles that participate in many important cellular processes, including energy metabolism, production of ROS, and apoptosis. Mitochondrial dysfunction has been shown to not only be in the pathological process of SAH models, but also SAH patients [6, 8]. A new development in the understanding of mitochondrial dysfunction was the discovery of drastic morphological changes in the organelles. Mounting evidences have confirmed that mitochondria are highly dynamic organelles that continuously divide and fuse to form new individual units and interconnected networks within the cell [9]. A balance between mitochondrial fission and fusion is important for mitochondrial function and morphology [9]. Excessive mitochondrial fission causes mitochondrial fragmentation, leading to apoptosis in a number of pathological processes, including cardiomyocyte death [10], ischemia–reperfusion injury [11] and neuronal injury [12, 13]; however, a recent study also showed that aberrant mitochondrial morphology can cause oxidative stress [14]. Therefore, regulation of mitochondrial morphology via mitochondrial fission and fusion may be a new option for SAH treatment. Mitochondrial dynamics are mediated by membrane-remodeling dynamin family proteins. In mammals, dynamin-like protein 1 (DLP1, also known as dynamin-related protein 1, Drp1) is the main protein that regulates mitochondrial fission, and also acts as an intrinsic factor in several mitochondria-dependent apoptosis pathways [15].
The quinazolinone derivative, Mdivi-1, is a selective inhibitor of the mitochondrial fission protein and inhibits Drp1 self-assembly, guanosine triphosphate (GTP) hydrolysis, and mitochondrial fission. Compared with other drugs, one of the main distinguishing characteristics of Mdivi-1 is that it can penetrate the blood–brain barrier, which is very important for central nervous system diseases [16]. Recent studies have shown that pretreatment with mdivi-1 provides neuroprotection in many diseases, including ischemic-reperfusion injury [11], epilepsy [13, 17] and traumatic brain injury [18]; however, it not known whether or not Mdivi-1 affects brain mitochondria-mediated apoptosis and oxidative stress after SAH.
In this study, we have, therefore, investigated whether Mdivi-1 can attenuate neuronal damage in the early stage after SAH. Additionally, we also examined the effect of mitochondrial fission inhibition in regulating mitochondria-mediated apoptosis and on oxidative stress to reveal the potential protective mechanism.
Materials and Methods
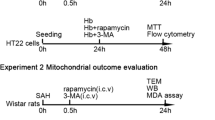
Animal Preparation and Study Design
Male Wistar rats (6–8 weeks old, 270–330 g) were purchased from the laboratory animal center of the Second Affiliated Hospital of Harbin Medical University (Harbin, China). All procedures were approved by the Institutional Animal Care and Use Committees at the First Affiliated Hospital of Harbin Medical University and were conducted in compliance with the National Institutes of Health guidelines for the care and use of laboratory animals. The rats were randomly divided into four groups: (1) the sham-operated group underwent sham surgery; (2) the SAH group was subjected to SAH; (3) the SAH + vehicle group was subjected to SAH and treated with vehicle; (4) the SAH + Mdivi-1 group was treated with intravenous Mdivi-1 (1.2 mg/kg) according to previous study [11]. The Mdivi-1 or vehicle was administered intravenously 30 min after SAH. Animals that died during or after surgery were replaced until the final group size achieved the expected number in each group.
Rat SAH Model
Male Wistar rats were anesthetized using pentobarbital (40 mg/kg, i.p.) and subjected to endovascular perforation, as previously described [19]. Briefly, the left carotid artery, left external carotid artery (ECA) and left internal carotid artery (ICA) were separated from the tissue. A blunt 4–0 nylon suture was placed in the ECA, advanced through the ICA for about 2 cm and held motionless for 10 s to perforate the artery and create the SAH. For sham-operated rats, the filaments were advanced into the ICA, but no arterial perforation was performed. The inferior basal temporal lobes adjacent to clotted blood were obtained for analysis in our study (Fig. 1).
Drug Administration
A stock solution (50 mmol/L) of Mdivi-1 (Selleck Chemicals, Houston, TX, USA) in DMSO was diluted with sterile saline to 1 mmol/L and injected intravenously 30 min after induction of SAH. The dose of Mdivi-1 was selected as previously described [11]. Normal saline containing DMSO at the same concentration as that used in the Mdivi-1 group was adopted as the vehicle control.
Mortality and SAH Grade
The mortality of the rats was recorded during and after the SAH procedure. The severity of the SAH, based on a previously described grading system [19], was measured by two blinded observers at the time of sacrifice. The grade scores were based on the volume of clots in six segments of the basal cistern. Each segment was scored 0–3 as follows [19]: 0, no subarachnoid blood; 1, minimal subarachnoid blood; 2, moderate blood clot with recognizable arteries; and 3, blood clot obliterating all arteries within the segment. The rats received a total score, which ranged from 0 to 18.
The Neurological Examination
Neurological functions were evaluated before sacrifice, on the basis of the previously described Garcia Scale [20]. Briefly, neurological deficit scores were the sum of the scores in six individual tests: spontaneous activity, spontaneous movement of four limbs, forepaw outstretching, climbing, body proprioception and response to whisker stimulation. The minimum neurological score is 3 and the maximum is 18. All tests were evaluated by two blinded observers.
Brain Water Content Measurement
The rats (n = 6 per group) were sacrificed 24 h post-SAH. Brains were removed immediately and divided into four parts: left hemisphere; right hemisphere; cerebellum; and brain stem. Each part was weighed to obtain the wet weight (WW), and then dried at 106 °C to obtain the dry weight (DW). The percentage of brain water content was calculated as [(WW–DW) / WW] × 100%.
Blood–Brain Barrier Permeability
BBB permeability was assessed 24 h after SAH as described previously [21]. Evan’s blue dye (2%, 5 ml/kg, Sigma) was injected over 2 min into the right femoral vein and circulated for 1 h. Then the rat was sacrificed following perfusion with PBS. The brain samples were weighed and homogenized in 50% trichloroacetic acid and centrifuged at 15,000×g for 30 min. After centrifugation, the supernatant was collected and mixed with ethanol and trichloracetic acid. The samples were then incubated overnight at 4 °C and centrifuged again. The resultant supernatant was determined by spectrofluorophotometer. Measurements were conducted at excitation wavelength 620 nm, emission wavelength 680 nm, and bandwidth 10 nm.
TUNEL and Immunohistological Staining
Rats (n = 6 per group) were sacrificed and perfused with PBS until the perfusate ran clear and then with 4% paraformaldehyde. For TUNEL staining, the ipsilateral temporal lobe cortices were removed and immersed in 4% paraformaldehyde at 4 °C for 6–8 h and then in 30% sucrose solution until the tissue sank (2 days). The brains were frozen in liquid nitrogen, and 7-µm sections were mounted on glass slides. TUNEL staining, to detect DNA double-strand damage, was carried out according to the kit manufacturer’s protocol (Roche, Basel, Switzerland), and sections were examined using an LSM-710 laser scanning confocal microscope (Carl Zeiss, Thornwood, NY, USA). The total number of DAPI- and TUNEL-positive cells were counted by a blinded investigator in four separate fields in four different slices of each brain. For immunohistochemical staining, the brain samples were fixing with the 4% paraformaldehyde and embedded in paraffin, as previously described [22]. Seven micrometer sections were used for immunohistochemical staining. The sections were deparaffinized and incubated with 3% hydrogen peroxide for 10 min, then washed in PBS. Rabbit antibody against cleaved caspase-3 (1:250 dilution; Beyotime Biotechnology, Haimen, China) was administered, followed by a horseradish peroxidase-conjugated secondary goat anti-rabbit IgG. Diaminobenzidine (DAB) was used as a chromogen. The immunoreactivity of cleaved caspase-3 in the brain was also determined by two blinded investigators.
Western Blot and Isolation of Mitochondria
Rats (n = 6 per group) were euthanized 24 h after SAH. The ipsilateral basal cortical samples that faced the clots were isolated and immediately frozen in liquid nitrogen as previously described [23]. Mitochondrial fractions were isolated using a Mitochondrial Extraction Kit (Solarbio Life Sciences, Beijing, China), according to the manufacturer’s instructions. The final supernatants were stored as cytosol fractions. Western blots were performed as previously described [22], using the following primary antibodies: anti-Cytochrome C, anti-cleaved caspase-3 and anti-β-actin (1:1000 dilution, Beyotime Biotechnology, Haimen, China), anti-COX IV (Cytochrome C oxidase IV) and p-Drp1(Ser616) (1:1000 dilution, Cell Signaling Technology, Boston, MA, USA) and Drp1 (1:1000 dilution, Abcam, Cambridge, UK). The images were analyzed in a blinded pattern using Image J software. COX IV and β-actin were used as internal standards.
Transmission Electron Microscopy
Rats (n = 6 each group) were sacrificed, perfused with saline, and fixed using 4% paraformaldehyde. Then, the ipsilateral temporal lobe cortices were minced into small (<1 mm3) fragments, fixed with 2.5% buffered glutaraldehyde for 4 h at 4 °C, post-fixed with 2% osmic acid in the same buffer for 90 min, dehydrated using a series of ethanol solutions and embedded in araldite overnight at 60 °C. The araldite-embedded specimens were cut into 60 nm sections using an EM UC7 ultramicrotome (Leica, Wetzlar, Germany). The sections were then fixed to nickel grids, stained with uranyl acetate and lead citrate and observed and photographed using a transmission electron microscope (Carl Zeiss Thornwood, NY, USA).
Measurement of MDA Levels and SOD Activities
Left basal cortical samples were harvested and immediately frozen in liquid nitrogen until use. The malondialdehyde (MDA) level and superoxide dismutase (SOD) activity were measured according to manufacturer instructions (Beyotime Biotechnology). All standards and samples were run in duplicate. The tissue protein was determined using a BCA Protein Assay Kit (Beyotime Biotechnology).
Evaluation of 3-NT and 8-OHdG Levels
The concentration of 3-NT and 8-OHdG was measured with a commercial enzyme-linked immunosorbent assay kit (Oxiselect™ nitrotyrosine, oxidative DNA damage ELISA kit for 3-NT or 8-OHdG; Cell Biolabs, Inc., San Diego, USA). Briefly, samples, standards, and primary antibodies were added to the wells of a well plate, which was then incubated at 4 °C for 12 h. A standardized preparation of HRP-conjugated antibody was added to each well to bind the immobilized 3-NT and 8-OHdG for 1 h at room temperature. The HRP and substrate were allowed to react, terminated by addition of the substrate fluid acid, and the OD value (λ = 450 nm) was measured. The standard curve was used to determine the levels of 3-NT and 8-OHdG in the samples.
Statistical Analysis
All data are presented as mean ± SD. Differences in mortality among groups were tested using the Fisher exact test. Other data were analyzed by one-way analysis of variance (ANOVA), followed by Tukey’s test for multiple comparisons. Differences were considered to be statistically significant at a value of P < 0.05. SPSS 19.0 statistics software (IBM, Armonk, NY, USA) were used for data analysis.
Results
Mortality and SAH Grade
None of the sham-operated rats died. The moralities of the SAH, SAH + vehicle, and SAH + Mdivi-1 group were 22.2% (8 of 44 rats), 19.4% (7 of 43 rats), and 13.9% (5 of 41 rats), respectively. The SAH + Mdivi-1 group had decreased mortality compared with the SAH group, but the differences were not statistically significant. The mean SAH grading scores were 0 in the sham-operated group, and the differences between the scores of the other three groups were of not statistically significant (Fig. 2a).
Effect of Mdivi-1 treatment on brain injury 24 h after induction of SAH. a Quantification of SAH severity, n = 36. b Quantification of neurological scores, n = 36. c Quantification of brain water content, n = 6. d Quantification of Evans blue extravasation, n = 6. Data are presented as mean ± S.D. Versus sham group, Asterisk denotes P < 0.01; versus SAH and SAH + vehicle group, hash denotes P < 0.01. P values were analyzed using one-way ANOVA
Mdivi-1 Improved Neurobehavioral Function and Alleviated Brain Edema and BBB Disruption
The neurologic scores of each group were measured 24 h after SAH. Brain water content in both hemispheres, the cerebellum, and the brain stem were tested separately at the same time points. The neurologic scores and water content were significantly worse after SAH (vs. the sham group, P < 0.01; Fig. 2b, c). Mdivi-1 administration significantly improved the neurologic scores following SAH injury and decreased brain water content in both hemispheres (vs. the SAH + vehicle group, P < 0.01; Fig. 2b, c). BBB permeability was examined by Evans blue assay 24 h following SAH. SAH caused a significantly increased extravasation of Evans blue in the globe brain, which implied BBB leakage. Treatment with Mdivi-1 markedly reduced BBB leakage compared to the SAH and SAH + vehicle groups (P < 0.01, Fig. 2d).
Mdivi-1 Attenuated Apoptotic Cell Death
We quantified cellular death using TUNEL staining. Following treatment with Mdivi-1, apoptotic cell death was determined 24 h after induction of SAH. Very few TUNEL-positive cells were observed in temporal lobe cortices in the sham group and the number of positive cells was markedly increased after SAH. Mdivi-1 treatment dramatically decreased the number of TUNEL-positive cells (P < 0.01, Fig. 3).
Cortical cellular apoptosis in different groups. a Representative TUNEL/DAPI photomicrographs of ipsilateral cortex in different groups (scale bar = 100 μm). b Quantification of TUNEL-positive neurons in each group. Data are presented as mean ± S.D. (n = 6). Versus sham group, Asterisk denotes P < 0.01; versus SAH and SAH + vehicle group, hash denotes P < 0.01. P values were analyzed using one-way ANOVA
Mdivi-1 Inhibited Mitochondria-Mediated Apoptosis After SAH
Whether or not the apoptosis mitochondrial signal transduction pathway was involved in the early brain injury stage after SAH and the role of Mdivi-1 was validated. Western blotting was used to the detect the level of Cytochrome C and cleaved caspase-3 expression. Immunohistochemistry staining was used to further verify the reliability of the activation level of cleaved caspase-3. Twenty-four hours after SAH, the release of Cytochrome C from mitochondria into the cytosol and the expression level of cleaved caspase-3 were significantly up-regulated in the basal cortex after SAH (vs. the sham group, P < 0.01), and this was blocked by treatment with Mdivi-1 (vs. the SAH + vehicle group, P < 0.01; Fig. 4a–d). Immunohistochemistry staining also showed that the number of cleaved caspase-3-positive cells, which were increased by SAH injury, were decreased in the SAH + Mdivi-1 group (vs. the SAH + vehicle group, P < 0.01; Fig. 4e, f).
Effect of treatment with Mdivi-1 on cleaved caspase-3 and Cytochrome C expression 24 h after induction of SAH. a Representative western blots showing levels of cleaved caspase-3 and Cytochrome C in ipsilateral cortex. b Relative band densities of mitochondrial Cytochrome C. c Relative band densities of cytosolic Cytochrome C. d Relative band densities of cleaved caspase-3. The densities of the protein bands were analyzed and normalized to β-actin or COX IV. (n = 6). e Immunohistochemical study of cleaved caspase-3 on the ipsilateral cortex, the representative photomicrographs in each group (scale bar = 100 μm). f Quantification of positive cells in each group (n = 6). Data are presented as mean ± S.D. Versus sham group, Asterisk denotes P < 0.01; versus SAH and SAH + vehicle group, hash denotes P < 0.01. P values were analyzed using one-way ANOVA
Mdivi-1 Inhibited Mitochondrial Fission After SAH
To verify whether or not mitochondrial fission was involved in cell injury, transmission electron microscopy and western blotting were used. The transmission electron microscopy images showed that the mitochondrial fission was increased. Furthermore, the cristae of mitochondria were disrupted and had an ambiguous appearance (Fig. 5b, c) following SAH, which were different from the sham group (Fig. 5a). These changes were reversed in the SAH + Mdivi-1 group (Fig. 5d). The expression levels of both Drp1 and p-Drp1(Ser616) markedly increased after SAH (vs. the sham group), and these up-regulation were clearly inhibited by Mdivi-1 (vs. the SAH + vehicle group, P < 0.01; Fig. 5e–g).
Mdivi-1 effects on mitochondrial fission in the rat cortex. a–d The representative electron microscopy images of mitochondrial morphology; a sham group; b SAH group; c SAH + vehicle group; d SAH + Mdivi-1 group. The asterisks indicate normal mitochondria. Arrows indicate mitochondria under fission. Arrow-heads indicate mitochondria swelling and cristae vague. Scale bar indicates 1 μm (n = 6). e–g Levels of Drp1 and p-Drp1(Ser616) proteins which mediated mitochondrial fission in ipsilateral cortex. e Representative western blots showing levels of Drp1 and p-Drp1(Ser616). f Quantification of relative band densities of Drp1. g Quantification of relative band densities of p-Drp1(Ser616). Data are presented as mean ± S.D. (n = 6). Versus sham group, Asterisk denotes P < 0.01; versus SAH and SAH + vehicle group, hash denotes P < 0.01. P values were analyzed using one-way ANOVA
Mdivi-1 Attenuated Oxidative Stress After SAH
The above results showed that Mdivi-1 alleviates mitochondria-mediated apoptosis by inhibiting Drp1-related excessive mitochondrial fission. In addition, mitochondria injury contributed to oxidative stress that induced neuronal death in SAH was demonstrated. Thus, we determined whether or not Mdivi-1 inhibited oxidative stress following SAH. MDA, 3-NT, and 8-OHdG are oxidative damage markers of lipid, protein, and DNA damage, respectively. Our data indicated that the levels of MDA, 3-NT, and 8-OHdG increased significantly after SAH (vs. the sham group, P < 0.05), and were reduced by Mdivi-1 treatment (vs. the SAH + vehicle group, P < 0.05; Fig. 6a, c, d). The SOD activity was statistically lower after SAH (vs. the sham group, P < 0.05; Fig. 6b), and was reserved by Mdivi-1 administration (vs. the SAH + vehicle group. P < 0.05; Fig. 6b).
Effects of Mdivi-1 treatment on oxidative stress 24 h after SAH induction. a The level of MDA in each group (n = 6). b The activity of SOD in each group (n = 6). c The concentration of 3-NT in each group (n = 6). d The concentration of 8-OHdG in each group (n = 6). Data are presented as the mean ± S.D. (n = 6). Versus sham group, Asterisk denotes P < 0.05; versus SAH and SAH + vehicle group, hash denotes P < 0.05. P values were analyzed using one-way ANOVA
Discussion
The present study provides the first direct evidence that the selective Drp1 inhibitor, Mdivi-1, exerts protective effects against EBI after SAH. First, Mdivi-1 improves neurological deficits, alleviates brain edema and BBB permeability, and reduces the number of TUNEL-positive cells. Second, our findings also show that inhibition of mitochondria-mediated apoptosis may contribute to the protection provided by mdivi-1. Mdivi-1 inhibited the release of Cytochrome C from the inner membrane space to the cytosol and subsequent activation of the caspase-9 and -3 cascades. Third, our data showed that excessive mitochondrial fission was involved in the EBI stage following SAH, and could be blocked by Mdivi-1. The transmission electron microscopy results showed that mitochondrial fragmentation and disruption of the mitochondrial structure occurred after SAH, and were improved by Mdivi-1. This was further confirmed by the significant increases in Drp1 and p-Drp1(Ser616) protein levels, which were also decreased by Mdivi-1 treatment. Fourth, we found Mdivi-1 treatment alleviated oxidative stress following SAH, which was confirmed by the reduction in MDA, 3-NT, and 8-OHdG levels and the elevation in SOD activity. In the present study, we advanced the hypothesis that Mdivi-1 could alleviate apoptosis in the early brain injury stage after SAH by inhibiting Drp1-activated mitochondrial fission and oxidative stress.
Previous studies suggested that mitochondria were dynamic organelles that underwent cycles of fusion and fission to maintain their morphology and function. Under stress, such as ischemia, seizures and trauma, excessive fission has been shown to contribute to apoptosis through a series of pathological processes [11, 17, 24–26]. Drp1, the mitochondrial fission regulatory protein, has been suggested to play a pivotal role in regulating mitochondrial fission and mitochondria-dependent apoptosis pathways [11, 27]. The precise mechanism by which Drp1 regulates neuronal apoptosis is, however, still unclear. Previous studies assumed that, under physiological conditions, Drp1 was present mainly in an unassembled form in the cell cytosol but that, in response to increased internal or external stimuli, it was recruited to the mitochondrial outer membrane and assembled into fission foci. These foci were thought to induce mitochondrial fragmentation prior to caspase activation by the release of Cytochrome C [9]. Many studies have shown that expression levels of Drp1 were increased by different stimuli, perhaps leading to excessive mitochondrial fission [11, 18, 27, 28]. Grohm et al. found that Drp1 siRNA and small molecule inhibitors of Drp1 could prevented mitochondrial fission and loss of mitochondrial membrane potential [29]. Wu et al. [18] reported that up-regulation of Drp1 expression started 1 h post-traumatic brain injury and peaked at 24 h, and inhibition Drp1 could reverse the morphologic change in the mitochondria. These results were in line with our finding that Drp1 was overexpressed after SAH. It has also been suggested that regulation of Drp1 by post-translocation modifications, such as phosphorylation and S-nitrosylation, is important for Drp1 cycling between the cytosol and mitochondria [9]. Taguchi et al. reported that human Drp1 could be activated by Cdk1/cyclin B-mediated phosphorylation of Ser616 in the variable domain, promoting Drp1-dependent mitochondrial fission [30]. In the present study, we also found that expression of p-Drp1(Ser616) increased after SAH, and we reported this for the first time in neurovascular disease.
As we know, the blood–brain barrier is the main impediment influencing drug effects in central nervous system diseases. The advantage of Mdivi-1 is that it can penetrate the blood–brain barrier due to its lipophilic nature. As a highly efficacious small molecule, it has been shown to proven cytoprotective benefits in several cell types involved in a wide array of injury models [16]. The protective mechanisms of Mdivi-1 are complex; a previous study reported that Mdivi-1 inhibited mitochondrial fission by blocking Drp1-self-assembly and GTP hydrolysis and blocked apoptotic cell death by inhibiting mitochondrial outer membrane permeabilization, which led to Cytochrome C release during apoptosis [31]; however, in our study we showed that treatment with Mdivi-1 decreased expression levels of Drp1 and p-Drp1(Ser616). This phenomenon was partially verified by other experiments. Zhang et al. [11] reported that Mdivi-1 alleviates cerebral ischemia/reperfusion injury via down-regulating expression of Drp1. Giedt et al. [32] reported that Mdivi-1 reduces endothelial cell injury after simulated ischemia/reperfusion by inhibiting the phosphorylation of Drp1. Likewise, the present results showed that treatment with Mdivi-1 also decreased the level of cleaved-caspase-3 and Cytochrome C expression in the cytoplasm, which were characteristics of apoptosis. Furthermore, our transmission electron microscopy results also confirmed that Mdivi-1 inhibited mitochondrial fission and restored mitochondrial structure after SAH. Taken together, these data suggest that Mdivi-1 reduced mitochondria-mediated cell apoptosis by inhibiting the expression and phosphorylation of Drp1, which are key proteins for regulating mitochondrial fission in the EBI stage after SAH.
Oxidative stress has also been proven to be a fundamental pathway leading to neuronal death after SAH. Because mitochondria are the original source for oxygen-free radicals and are at the most sensitive position for reactive oxygen species. A previous study showed that aberrant mitochondrial morphology can product excessive ROS in epilepsy [32]. In the present study, we observed that Mdivi-1 alleviates oxidative stress, as shown by the decreased levels of MDA, lower concentration of 3-NT and 8-OHdG, and increased SOD activity in the SAH models. These protective effects may be relevant to its’ role in inhibition of excessive mitochondrial fission. Similar results were also reported in epilepsy and hyperglycemia models [17, 33], in which Drp1-mediated mitochondrial fission was an upstream regulator of oxidative stress. The mechanisms of ROS overproduction from excessive mitochondrial fission remain fully described. It has been suggested that excessive mitochondrial fission may lead to the loss of mitochondrial membrane potential, the rearrangement of mitochondrial electron transport chain components, and defective mitochondrial oxidative phosphorylation [25]. Based on our findings, we speculate that excessive mitochondrial fission may be associated with the release of Cytochrome C from the mitochondria to the cytoplasm, which is an indispensable part of the oxidation respiratory chain. Mdivi-1 can inhibit mitochondrial fission, reduce the release of Cytochrome C, and restore the function of the electron transport chain.
In the present study, we have demonstrated a protective effect of Mdivi-1 on EBI after SAH and have suggested potential mechanisms underlying this effect. There are, however, several limitations in this study. Firstly, we have only evaluated the neuroprotective effect of administered Mdivi-1 24 h after SAH. Future studies should assess the pharmacokinetics and long-term effects of Mdivi-1. Secondly, the pathways that regulate Drp1 expression and phosphorylation warrant further investigation. Third, we also need to investigate the physiologic effect of the active metabolites of Mdivi-1 to ensure there are no undesirable biological effects. This is necessary for advancing Mdivi-1 closer to clinical application.
Conclusions
In summary, our findings suggest that the Drp1 inhibitor, Mdivi-1, exerts therapeutic effects in EBI after SAH. The underlying mechanism is attributable to suppressing apoptosis by inhibiting Drp1-activated mitochondrial fission and oxidative stress.
Abbreviations
- SAH:
-
Subarachnoid hemorrhage
- Drp1:
-
Dynamin-like protein 1
- EBI:
-
Early brain injury
- ECA:
-
External carotid artery
- ICA:
-
Internal carotid artery
References
Fujii M, Yan J, Rolland WB, Soejima Y, Caner B, Zhang JH (2013) Early brain injury, an evolving frontier in subarachnoid hemorrhage research. Transl Stroke Res 4(4):432–446. doi:10.1007/s12975-013-0257-2
Sehba FA, Hou J, Pluta RM, Zhang JH (2012) The importance of early brain injury after subarachnoid hemorrhage. Prog Neurobiol 97(1):14–37. doi:10.1016/j.pneurobio.2012.02.003
Serrone JC, Maekawa H, Tjahjadi M, Hernesniemi J (2015) Aneurysmal subarachnoid hemorrhage: pathobiology, current treatment and future directions. Expert Rev Neurother 15(4):367–380. doi:10.1586/14737175.2015.1018892
Conzen C, Schubert GA (2016) About the importance of the acute phase of subarachnoid hemorrhage and the chances for successful translation. J Neurol Sci. doi:10.1016/j.jns.2016.09.031
Yuksel S, Tosun YB, Cahill J, Solaroglu I (2012) Early brain injury following aneurysmal subarachnoid hemorrhage: emphasis on cellular apoptosis. Turk Neurosurg 22(5):529–533. doi:10.5137/1019-5149.JTN.5731-12.1
Cai J, Cao S, Chen J, Yan F, Chen G, Dai Y (2015) Progesterone alleviates acute brain injury via reducing apoptosis and oxidative stress in a rat experimental subarachnoid hemorrhage model. Neurosci Lett 600:238–243. doi:10.1016/j.neulet.2015.06.023
Zhang ZY, Sun BL, Liu JK, Yang MF, Li DW, Fang J, Zhang S, Yuan QL, Huang SL (2015) Activation of mGluR5 attenuates microglial activation and neuronal apoptosis in early brain injury after experimental subarachnoid hemorrhage in rats. Neurochem Res 40(6):1121–1132. doi:10.1007/s11064-015-1572-7
Jacobsen A, Nielsen TH, Nilsson O, Schalen W, Nordstrom CH (2014) Bedside diagnosis of mitochondrial dysfunction in aneurysmal subarachnoid hemorrhage. Acta Neurol Scand 130(3):156–163. doi:10.1111/ane.12258
Otera H, Ishihara N, Mihara K (2013) New insights into the function and regulation of mitochondrial fission. Biochim Biophys Acta 1833(5):1256–1268. doi:10.1016/j.bbamcr.2013.02.002
Zaja I, Bai X, Liu Y, Kikuchi C, Dosenovic S, Yan Y, Canfield SG, Bosnjak ZJ (2014) Cdk1, PKCdelta and calcineurin-mediated Drp1 pathway contributes to mitochondrial fission-induced cardiomyocyte death. Biochem Biophys Res Commun 453(4):710–721. doi:10.1016/j.bbrc.2014.09.144
Zhang N, Wang S, Li Y, Che L, Zhao Q (2013) A selective inhibitor of Drp1, mdivi-1, acts against cerebral ischemia/reperfusion injury via an anti-apoptotic pathway in rats. Neurosci Lett 535:104–109. doi:10.1016/j.neulet.2012.12.049
Cherubini M, Gines S (2016) Mitochondrial fragmentation in neuronal degeneration: Toward an understanding of HD striatal susceptibility. Biochem Biophys Res Commun. doi:10.1016/j.bbrc.2016.08.042
Xie N, Wang C, Lian Y, Zhang H, Wu C, Zhang Q (2013) A selective inhibitor of Drp1, mdivi-1, protects against cell death of hippocampal neurons in pilocarpine-induced seizures in rats. Neurosci Lett 545:64–68. doi:10.1016/j.neulet.2013.04.026
Pletjushkina OY, Lyamzaev KG, Popova EN, Nepryakhina OK, Ivanova OY, Domnina LV, Chernyak BV, Skulachev VP (2006) Effect of oxidative stress on dynamics of mitochondrial reticulum. Biochim Biophys Acta 1757(5–6):518–524. doi:10.1016/j.bbabio.2006.03.018
Frank S, Gaume B, Bergmann-Leitner ES, Leitner WW, Robert EG, Catez F, Smith CL, Youle RJ (2001) The role of dynamin-related protein 1, a mediator of mitochondrial fission, in apoptosis. Dev Cell 1(4):515–525
Rosdah AA, J KH, Delbridge LM, Dusting GJ, Lim SY (2016) Mitochondrial fission - a drug target for cytoprotection or cytodestruction? Pharmacol Res Perspect 4 (3):e00235. doi:10.1002/prp2.235
Xie N, Wang C, Wu C, Cheng X, Gao Y, Zhang H, Zhang Y, Lian Y (2016) Mdivi-1 protects epileptic hippocampal neurons from apoptosis via inhibiting oxidative stress and endoplasmic reticulum stress in vitro. Neurochem Res 41(6):1335–1342. doi:10.1007/s11064-016-1835-y
Wu Q, Xia SX, Li QQ, Gao Y, Shen X, Ma L, Zhang MY, Wang T, Li YS, Wang ZF, Luo CL, Tao LY (2016) Mitochondrial division inhibitor 1 (Mdivi-1) offers neuroprotection through diminishing cell death and improving functional outcome in a mouse model of traumatic brain injury. Brain Res 1630:134–143. doi:10.1016/j.brainres.2015.11.016
Sugawara T, Ayer R, Jadhav V, Zhang JH (2008) A new grading system evaluating bleeding scale in filament perforation subarachnoid hemorrhage rat model. J Neurosci Methods 167(2):327–334. doi:10.1016/j.jneumeth.2007.08.004
Garcia JH, Wagner S, Liu KF, Hu XJ (1995) Neurological deficit and extent of neuronal necrosis attributable to middle cerebral artery occlusion in rats. Statistical validation. Stroke 26 (4):627–634; discussion 635
Zhao H, Ji Z, Tang D, Yan C, Zhao W, Gao C (2013) Role of autophagy in early brain injury after subarachnoid hemorrhage in rats. Mol Biol Rep 40(2):819–827. doi:10.1007/s11033-012-2120-z
Zheng B, Zheng T, Wang L, Chen X, Shi C, Zhao S (2010) Aminoguanidine inhibition of iNOS activity ameliorates cerebral vasospasm after subarachnoid hemorrhage in rabbits via restoration of dysfunctional endothelial cells. J Neurol Sci 295(1–2):97–103. doi:10.1016/j.jns.2010.04.012
Cheng G, Chunlei W, Pei W, Zhen L, Xiangzhen L (2010) Simvastatin activates Akt/glycogen synthase kinase-3beta signal and inhibits caspase-3 activation after experimental subarachnoid hemorrhage. Vasc Pharmacol 52(1–2):77–83. doi:10.1016/j.vph.2009.12.001
Fischer TD, Hylin MJ, Zhao J, Moore AN, Waxham MN, Dash PK (2016) Altered mitochondrial dynamics and TBI pathophysiology. Front Syst Neurosci 10:29. doi:10.3389/fnsys.2016.00029
Qiu X, Cao L, Yang X, Zhao X, Liu X, Han Y, Xue Y, Jiang H, Chi Z (2013) Role of mitochondrial fission in neuronal injury in pilocarpine-induced epileptic rats. Neuroscience 245:157–165. doi:10.1016/j.neuroscience.2013.04.019
Li G, Jia Z, Cao Y, Wang Y, Li H, Zhang Z, Bi J, Lv G, Fan Z (2015) Mitochondrial division inhibitor 1 ameliorates mitochondrial injury, apoptosis, and motor dysfunction after acute spinal cord injury in rats. Neurochem Res 40(7):1379–1392. doi:10.1007/s11064-015-1604-3
Kim H, Lee JY, Park KJ, Kim WH, Roh GS (2016) A mitochondrial division inhibitor, Mdivi-1, inhibits mitochondrial fragmentation and attenuates kainic acid-induced hippocampal cell death. BMC Neurosci 17(1):33. doi:10.1186/s12868-016-0270-y
Liang N, Wang P, Wang S, Li S, Li Y, Wang J, Wang M (2014) Role of mitochondrial calcium uniporter in regulating mitochondrial fission in the cerebral cortexes of living rats. J Neural Transm 121(6):593–600. doi:10.1007/s00702-014-1166-6
Grohm J, Kim SW, Mamrak U, Tobaben S, Cassidy-Stone A, Nunnari J, Plesnila N, Culmsee C (2012) Inhibition of Drp1 provides neuroprotection in vitro and in vivo. Cell Death Differ 19(9):1446–1458. doi:10.1038/cdd.2012.18
Taguchi N, Ishihara N, Jofuku A, Oka T, Mihara K (2007) Mitotic phosphorylation of dynamin-related GTPase Drp1 participates in mitochondrial fission. J Biol Chem 282(15):11521–11529. doi:10.1074/jbc.M607279200
Cassidy-Stone A, Chipuk JE, Ingerman E, Song C, Yoo C, Kuwana T, Kurth MJ, Shaw JT, Hinshaw JE, Green DR, Nunnari J (2008) Chemical inhibition of the mitochondrial division dynamin reveals its role in Bax/Bak-dependent mitochondrial outer membrane permeabilization. Dev Cell 14(2):193–204. doi:10.1016/j.devcel.2007.11.019
Puttachary S, Sharma S, Stark S, Thippeswamy T (2015) Seizure-induced oxidative stress in temporal lobe epilepsy. BioMed Res Int 2015:745613. doi:10.1155/2015/745613
Yu T, Jhun BS, Yoon Y (2011) High-glucose stimulation increases reactive oxygen species production through the calcium and mitogen-activated protein kinase-mediated activation of mitochondrial fission. Antioxid Redox Signal 14(3):425–437. doi:10.1089/ars.2010.3284
Acknowledgements
This research was supported in part by the Innovative Science Research Foundation of Harbin Medical University [Grant Number 2016LCZX59], the National Natural Science Foundation of China [Grant Number 81401009], and the Natural Science Foundation of Heilongjiang Province [grant number QC2013C088]. We thank Professor Zhang for help in designing experiments and advice about the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, P., Li, Y., Zhu, S. et al. Mdivi-1 Alleviates Early Brain Injury After Experimental Subarachnoid Hemorrhage in Rats, Possibly via Inhibition of Drp1-Activated Mitochondrial Fission and Oxidative Stress. Neurochem Res 42, 1449–1458 (2017). https://doi.org/10.1007/s11064-017-2201-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-017-2201-4