Abstract
Paeoniflorin (PF) is the main active component extracted from the roots of Paeonialactiflora, a traditional Chinese medicine used for the treatment of neurodegenerative disorders, especially Parkinson’s disease (PD). The degeneration of dopaminergic (DA-) neurons in PD may be caused by pathological activation of acid-sensing ion channels (ASICs). Thus, we designed a series of experiments to evaluate the therapeutic effects of PF and to test whether its effects are related to its inhibitory effect on ASIC1a. We found that systemic administration of PF or ASICs blockers (psalmotoxin-1 and amiloride) improved behavioral symptoms, delayed DA-neuronal loss and attenuated the reduction of dopamine (DA) and its metabolites in a rat model of 6-hydroxydopamine (6-OHDA)-induced PD. In addition, our data showed that PF, like ASICs blockers, regulated the expression of ASIC1a, decreased the level of α-synuclein (α-SYN), and improved autophagic dysfunction. Further experiments showed that ASIC1a knockdown down-regulated the α-SYN level and alleviated the autophagic injury in the 6-OHDA-treated ASIC1a-silenced PC12 cells. In summary, these findings indicate that PF enhanced the autophagic degradation of α-SYN and, thus, protected DA-neurons against the neurotoxicity caused by 6-OHDA. These findings also provide experimental evidence that PF may be a neuroprotectant for PD by acting on ASIC1a and that ASIC1a may be involved in the pathogenesis of PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is the second most common age-related neurodegenerative disorder. Progressive loss of dopaminergic (DA-) neurons in the substantia nigra (SN) pars compacta (SNc) and the formation of Lewy bodies are pathological features of PD. Although the etiology of PD remains unclear, mounting evidence indicates that multiple factors lead to this disease, including oxidative stress, mitochondrial dysfunction, proteasome dysfunction, inflammatory or immune response, disturbances of calcium homeostasis, excitotoxicity, and apoptosis [1–3]. In recent years, we have focused on studying the mechanism of α-synuclein (α-SYN), which is the main component of Lewy bodies [4, 5]. α-SYN, a characteristic marker of various types of PD, is degraded by the ubiquitin–proteasome system (UPS) and the autophagy-lysosome pathway (ALP) [5, 6]. Mounting evidence suggests that autophagic impairment induced by pathological factors, such as oxidative stress, results in excessive accumulation of misfolded proteins, which contributes to the onset and progression of PD [7, 8].
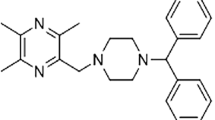
Acidosis is a common cause of tissue impairment. Recent studies have shown that significant reduction of extracellular pH can activate the special voltage-independent, proton-gated cation-selective channels called acid-sensing ion channels (ASICs), which are widely distributed in the central and peripheral sensory nervous system [9, 10]. So far, at least seven subtypes of ASICs (ASIC1a, lb, 2a, 2b, 3a, 3b and 4) encoded by four different genes have been identified [11]. Of all the ASICs, homomeric ASIC1a and heteromeric ASIC1a/2b channels have permeability to Ca2+ [12, 13]. A number of studies have demonstrated that acidosis within the brain is involved in various nervous system degenerative diseases, including acute brain injury and PD, and that ASIC1a is found to be expressed in the vulnerable DA-neurons in the SN [14, 15]. In addition, amiloride, a non-selective ASICs blocker, protects DA-neurons against 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced degeneration in mice. Psalmotoxin-1 (PcTx1), a subtype-selective ASIC1a blocker has also been reported to weaken the affinity of dopamine (DA) for dopamine transporter (DAT) [14, 16]. All these data suggest that ASICs are related to the damage of DA-neurons. Therefore we hypothesize that the degeneration of DA-neurons may be caused by chronic and pathological activation of ASICs, and that selective inhibition of some subunits of ASICs may delay the progression of PD.
To date, no direct evidence demonstrating a relationship between ASICs and autophagy has been found. Our previous experimental data revealed that amiloride protects PC12 cells against 1-methyl-4-phenylpyridinium (MPP+) and acidic damage, and that this protective effect is closely related to the changes of autophagy-specific proteins LC3-II and LAMP2a [17, 18]. These findings led us to presume that enhancement of α-SYN autophagic degradation, via its action on ASICs, may protect DA-neurons.
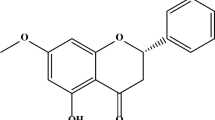
Paeoniflorin (PF), a monoterpene glycoside, is the main biologically active component extracted from the roots of Paeonia lactiflora and is used in traditional Chinese medicine. Previous studies have demonstrated that PF has a variety of pharmacological effects, including anti-oxidant and anti-inflammatory effects and inhibition of intracellular Ca2+ overload [19, 20]. Recent studies also suggest that PF has neuroprotective properties and can be used in clinic to treat cerebral ischemia, epilepsy, and neurodegenerative disorders, especially PD [21]. However, its mechanism of neuroprotection remains unclear. Our previous work has shown that PF protects PC12 cells against MPP+ and acidic damage through regulating autophagy, just like amiloride does [17, 18]. In this study, the 6-hydroxydopamine (6-OHDA)-induced PD rat model was used to evaluate the protective effects of PF on DA-neurons and to further investigate PF’s molecular mechanisms. We expect to provide evidence that PF is a new neuroprotectant for PD and to determine whether ACIS1a is a potential therapeutic target in PD.
Material and Methods
Drugs and Chemicals
PF (monomer, purity >98 %) was purchased from the National Institute for the Control of Pharmaceutical and Biological Products of China (Beijing). Psalmotoxin-1 (PcTx1) was obtained from Alomone Labs (Jerusalem, ISR). 6-OHDA and amiloride were purchased from Sigma–Aldrich (St Louis, MO, USA). Apomorphine (APO) was obtained from Enzolife Science in Japan. The sources of the primary antibodies used in these experiments are as follows: mouse anti-tyrosine hydroxylase (TH) antibody (Sigma, USA), rabbit anti-LC3 (Abcam, Cambridge, UK), mouse anti-α-SYN (Abcam), rabbit anti-p62 (Enzo, Japan), and rabbit anti-ASIC1a (Alomone Labs). The small interfering RNA (siRNA) sequences targeting rat ASIC1a were as follows: siRNA-1, 5′-CACUGUGCAAUCUCAAUGATT-3′ and 5′-UCAUUGAGAUUGCACAGUGTT-3′; siRNA-2, 5′-GACUCGGAUUUCUUCGACUTT-3′ and 5′-AGUCGAAGAAAUCCGAGUCTT-3′; and siRNA-3, 5′-CCUACGAGGUCAUUAAGCATT-3′ and 5′-UGCUUAAUGACCUCGUAGGTT-3′. Negative control siRNA was purchased from GenePharma (Shanghai, China).
Animals and Experimental Procedure
All 140 male Sprague–Dawley (SD) rats (180–220 g, 2–3 month old) were purchased from the Center for Experimental Animals (Soochow University, China). Animals were housed under specific conditions: quiet environment, day-night rhythm (12 h light–dark cycles), and free access to food and water. The experimental procedures were agreed to by the Institutional Animal Care and Use Committee of Soochow University (Suzhou, China).
6-OHDA-Induced PD Model and the Behavioral Test
The rats were anesthetized with 3.6 % chloral hydrate [0.18 g/kg, intraperitoneal (i.p.)] and were fixed on a stereotaxic apparatus (David Kopf Instruments, CA, USA). According to the stereotaxic brain atlas of rat [22], 6-OHDA (10 µg 6-OHDA hydrochloride in 5 µL of saline solution, 5 µg 6-OHDA at each point), or sterile saline (2.5 µL at each point) were injected at two points in the right striatum (Bregma coordinates for two injection points—first point: AP, +1.0 mm; ML, +3.0 mm; DV, −4.5 mm; and second point: AP, −0.2 mm; ML, +3.0 mm; DV, −6.0 mm) at the rate of 0.5 µL/min by 10-µL Hamilton syringe. After the injection, the needle was retained in the striatum for 3 min. Then the needle was withdrawn at the rate of 1 mm/min. After surgery, the rats were returned to the same environment they were in prior to surgery.
Three weeks after the operation, the rats’ contralateral rotations induced by APO [0.5 mg/kg, subcutaneous (s.c.)] were measured and recorded with a video camera once a week for two consecutive weeks. The duration of each recording time was 30 min. Rats with a rotating frequency of over 7 turns/min were included in the PD model. These selected model rats were divided into the following six groups: vehicle treatment group (sterile saline, i.p.), PF 15 mg/kg, i.p. treatment group, PF 30 mg/kg, i.p. treatment group, PF 60 mg/kg, i.p. treatment group, PcTx1 0.7 µg/kg, intranasal (i.n.) treatment group, and amiloride 10 mg/kg, i.p. treatment group. At the same time, sham-operated rats received vehicle or PF (60 mg/kg) treatment. All these rats were treated with vehicle or PF or amiloride or PcTx1 once a day for 21 days. And the changes in the contralateral rotational behavior caused by APO (0.5 mg/kg, s.c.) were tested once a week for 3 weeks after the rats received treatment.
High-Performance Liquid Chromatography (HPLC) Determination of DA, Serotonin, and Their Metabolites in the Striatum
The levels of DA, 3,4-dihydroxyphenylacetic acid (DOPAC), 4-hydroxy-3-methoxyphenylacetic acid (HVA), serotonin (5-HT) and 5-hydroxyindole-3-acetic acid (5-HIAA) in the striatum were measured by HPLC. A Waters 2695 Separation Module HPLC system (Waters Company, Milford, MA, USA) equipped with a Waters 2475 Fluorescence detector (Waters Company) was used. A C18 chromatographic column (250 × 4.6 mm, 5 µm, Akzonobel, AMS, NL) was used to qualitatively and quantitatively analyze the neurotransmitters, and the column temperature was maintained at 30 °C. Data acquisition and integration were controlled by Applied Biosystems Analyst Software (Applied Biosystems/MDS SCIEX, version 1.4.2). The rats were sacrificed and the striatum was dissected from brain. Then the tissue was homogenized and sonicated in 200 µL saline on ice for 10 s, three times; then, the same volume of 200 µL perchloric acid (4 °C, 0.4 mol/L) was added. The mixture was centrifuged at 10,000 rpm for 15 min at 4 °C; then, the supernatant mixed with 200 µL perchloric acid (4 °C, 0.4 mol/L) was centrifuged at 10,000 rpm for 10 min at 4 °C again. Next, the supernatant was diluted in perchloric acid (4 °C, 0.4 mol/L); and the total volume was 1 mL. The supernatant was then filtered (0.45 µm, Millipore, Boston, MA, USA), and 10 µL of sample was injected into the HPLC system for analysis. The mobile phase included 0.1 M sodium acetate, methanol (99.9 %) (9:1, v/v) and was adjusted to pH 5.1. The flow rate of the sample and mobile phase was set at 1 mL/min. The excitation wavelength was set at 290 nm and emission wavelength was set at 330 nm. The levels of monoamine neurotransmitters were expressed as µg/g wet tissue.
Western Blot Analysis
Midbrain tissue of rats was dissected and homogenized in radioimmunoprecipitation assay tissue lysis buffer (1:10, w/v, Beyotime Institute of Biotechnolog, Shanghai, China), to which protease inhibitor cocktail was added. The lysate was placed on ice for 30 min and centrifuged at 132,000 rpm for 15 min at 4 °C. Then the supernatant was collected; and protein concentration was measured by bicichoninic acid protein assay kit (Beyotime). The samples (20 µL) were separated with 12 % sodium dodecyl sulfate–polyacrylamide gels and transferred onto polyvinylidine fluoride membranes. After blocking with 2 % bovine serum albumin (BSA) in phosphate buffered saline (PBS) with Tween-20 (3.2 mM Na2HPO4, 0.5 mM KH2PO4, 0.1 % Tween-20, pH 7.4) at 37 °C for 1 h, membranes were incubated with primary antibodies, including anti-LC3 (1:1000), mouse anti-α-SYN (1:500), anti-p62 (1:1000), and anti-ASIC1a (1:200) at 4 °C overnight. Next, the membranes were incubated with corresponding secondary antibodies (1:5000) at room temperature for another hour. The special protein bands were detected by ECL chemiluminescence kit (GE Healthcare, Buckinghamshire, UK), and the density of protein bands was analyzed by using Image J software (National Institute of Health, Bethesda, MD, USA).
Immunohistochemistry
The rats were deeply anesthetized with 3.6 % chloral hydrate and perfused with 4 % paraformaldehyde (PFA). The intact brain tissues were collected and then fixed in 4 % PFA at 4 °C for 24 h. The tissues were immersed in 15 % sucrose/PBS solution (0.1 M) and 30 % sucrose/PBS solution (0.1 M) sequentially at 4 °C until they sunk to the bottom of the tube. After being stored at −80 °C for 30 min, frozen sections containing SN were cut at a thickness of 12 µm and mounted on gelatin-coated glass slides. Briefly, fresh sections were treated in 3 % H2O2 for 15 min to get rid of endogenous peroxidase, blocked with 5 % goat serum in Triton X-100-PBS for 30 min, and then incubated with primary antibody (anti-TH, 1:1,000, Sigma–Aldrich; anti-ASIC1a, 1:50, Alomone Labs) overnight at 4 °C. Next, slides were incubated with horseradish peroxidase (HRP)-marked polymers (Gene Tech Company Limited, Shanghai, China) or corresponding Alexa Fluor secondary antibodies (Life Technologies, Carlsbad, CA, USA) for 30 min at room temperature. HRP sections were treated with diaminobenzidine solution to visualize immunostaining; then, the sections were observed and photographed with a Zeiss microscope (AXIOSCOPE A1, Zeiss Corp, Jena, Germany). After Hoechst 33342 (1 µg/mL, Sigma–Aldrich) was added to stain the nuclei, Alexa Fluor sections were observed and photographed under confocal microscope (LSM700, Zeiss Corp). The numbers of TH-positive (TH+) neurons in the SN were counted with the aid of a superimposed grid to estimate the loss of DA-neurons. Five sections from each rat in the same atlas levels were analyzed by two researchers blind to the treatment group.
Cell Culture and siRNA Transfection
PC12 cell lines, provided by the Chinese Academy of Sciences (Shanghai, China), were incubated in Dulbecco’s modified Eagle’s medium containing 10 % fetal bovine serum and 1 % penicillin/streptomycin at 37 °C in a 5 % humidified CO2 atmosphere. Cells were plated onto a 24-well plate (1 × 105 cells/well) and allowed to grow for 24 h prior to further experimentation. Then, these cells were cultured with serum-free medium without antibiotics for 4 h, followed by transfection with negative siRNA or ASIC1a siRNAs using Lipofectamine 2000 (Life Technologies). After 24 h, the cells were collected, total protein was extracted from PC12 cells, and ASIC1a-protein expression was examined by western blot to monitor the gene-silencing effect. Next, the ASIC1a siRNA transfected cells and negative siRNA transfected cells were further treated with 6-OHDA (50 µM) or vehicle for 12 h. The levels of ASIC1a, α-SYN, and autophagic markers (LC3-II, p62) were then measured by western blot.
Statistical Analysis
All data were expressed as the mean ± standard error of the mean (SEM). Results were assessed by SPSS Version 6.1 software (SPSS, Chicago, IL, USA) using one-way analysis of variance followed by a post hoc (Turkey) analysis for multiple comparisons among groups. Differences were considered significant when the P value was less than 0.05.
Results
PF and ASICs Blockers Affected the Behavioral Symptoms in 6-OHDA-Lesioned Rats
To evaluate the curative effects of PF and ASICs blockers (PcTx1, amiloride), the successful PD model rats were selected in the 4th week following unilateral injection of 6-OHDA into the right striatum and then treated with vehicle (saline) or PF (15 or 30 or 60 mg/kg) or ASICs blockers (PcTx1 0.7 µg/kg, amiloride 10 mg/kg) for 21 continuous days. No rotational behavior was observed throughout the test in sham-operated and sham-operated plus PF (60 mg/kg) treatment rats (Fig. 1). The number of contralateral rotations in vehicle-treated 6-OHDA lesioned rats increased gradually from the 4th to 7th weeks after surgery (## P < 0.01), but this phenomenon did not occur in the 6-OHDA-lesioned rats treated with PF or ASICs blockers (PcTx1, amiloride) (*P < 0.01, **P < 0.05) (Fig. 2). These data show the remarkable neurotoxicity induced by 6-OHDA. The data also suggest that PF and ASICs blockers (PcTx1, amiloride) slowed down the progress of rotational behavior induced by APO in 6-OHDA-lesioned rats in a time-dependent manner.
Behavioral test in 6-OHDA-lesioned rats. The contralateral rotations induced by APO developed in the 6-OHDA-lesioned rats in a time-dependent manner, but occurrence of contralateral rotational behavior could not be observed in the sham-operated and sham-operated plus PF (60 mg/kg) treatment groups. Mean ± SEM. n = 10 in sham group, n = 10 in sham plus PF group, n = 12 in 6-OHDA-lesioned group, ## P < 0.01 versus week 4
Administration with PF and ASICs-blocker (PcTx1, amiloride) improved the contralateral rotational behavior in unilaterally 6-OHDA-lesioned rats. PF (15 or 30 or 60 mg/kg) or PcTx1 (0.7 µg/kg) or amiloride (Ami, 10 mg/kg) was given daily from the 4th to 6th weeks after unilateral injection of 6-OHDA. Mean ± SEM. n = 12 in each group, ## P < 0.01 versus week 4, *P < 0.05, **P < 0.01 versus vehicle control group at same time point. Ami amiloride
PF and ASICs Blockers Prevented Progression of the DA-Neuronal Loss in the SN of 6-OHDA-Lesioned Rats
To further investigate the effects of PF and ASICs blockers (PcTx1, amiloride) on neuronal degeneration, immunohistochemistry was used to detect the number of TH+ neurons in the SNc in unilaterally 6-OHDA-lesioned rats. The number of TH+ neurons in the intact side of 6-OHDA-lesioned and in sham-operated rats had no apparent reduction, but remarkable loss of TH+ neurons in the 6-OHDA-lesioned side was observed. In the rats, treated with PF (30 mg/kg) or ASICs blockers (PcTx1 0.7 µg/kg, amiloride 10 mg/kg) once daily for 21days, the loss of TH+ neurons was prevented (Fig. 3a). This was further confirmed by counting the number of TH+ neurons in the SN (Fig. 3b). Compared with sham rats, the number of TH+ neurons in 6-OHDA-lesioned side treated with saline was reduced by 56.3 % (**P < 0.01). The number of TH+ neurons was significantly higher in the 6-OHDA-lesioned side treated with PF and ASICs blockers (PcTx1, amiloride) than that in saline-treated rats (## P < 0.01). These findings suggest the possible neuroprotective effects of PF and ASICs blockers (PcTx1, amiloride) on DA-neuronal degeneration induced by 6-OHDA.
Effects of PF and ASICs-blocker (PcTx1, amiloride) treatment on 6-OHDA-induced TH+ neuronal degeneration. a Representative pictures of immunohistochemistry showing PF (30 mg/kg) or PcTx1 (0.7 µg/kg) or Ami (10 mg/kg) treatment alleviated TH+ neuronal loss in SNc of 6-OHDA-lesioned rats. b The number of TH+ neurons in the right side of the SNc was counted at 7 weeks after surgery; then the mean value of the TH+ neuron number calculated from four rats was regarded as the data for each group. A total of five sections were counted and analyzed in each rat. Data are expressed as the mean ± SEM, n = 4, **P < 0.01 versus sham group; ## P < 0.01 versus saline-treated 6-OHDA group. Total neurons in the SNc were observed by increased cell size. Photos were taken at ×50 magnification (Scale bar 200 µm) (a)
PF and ASICs Blockers Treatment Reduced the Levels of DA and its Metabolites in the Striatum
Next, the levels of neurotransmitters (DA and its metabolites, 5-HT and its metabolites) in the striatum were examined with HPLC. On the whole, we found no apparent difference in the levels of DA and its metabolites between the intact sides of PD rats and the striatum of sham-group rats. Compared with those in sham-operated rats, the levels of DA and DOPAC, as well as HVA in 6-OHDA-lesioned striatum treated with saline were markedly reduced by approximately 72.1, 50.3, and 52.2 %, respectively (**P < 0.01), whereas the ratio of DA metabolites to DA was raised by about 46.8 % (Fig. 4a–d). These data suggest that 6-OHDA induced significant DA-neuronal loss in the striatum and confirmed that a successful PD rat model was established. We also observed that the levels of DA and its metabolites were significantly higher and that the ratio of DA metabolites to DA was significantly lower in the injured striatum of PD rats treated with PF (15 or 30 or 60 mg/kg) or ASICs blockers (PcTx1 0.7 µg/kg, amiloride 10 mg/kg) than the ratio in saline-treated rats (# P < 0.05, ## P < 0.01) (Fig. 4a–d). However, we did not observe a marked difference in the levels of 5-HT and its metabolites between the rats in the sham group and those in the PD group (Fig. 4e, f). These results suggest that the lesion of the DA- terminals is relatively selective and demonstrate once again that PF and ASICs blockers (PcTx1, amiloride) protected DA-neurons against 6-OHDA-induced damage.
Effects of PF and ASICs-blocker (PcTx1, amiloride) treatment on DA and its metabolites reduction in the striatum. The levels of DA and its metabolite DOPAC and HVA (a–d) and the levels of 5-HT and its metabolite 5-HIAA (e, f) in the striatum of 6-OHDA-lesioned rats were determined by HPLC. Left (intact side), indicated as a hollow column; right (injured side), indicated as black column. The results are expressed as µg/g tissue. Data are expressed as the mean ± SEM, n = 8, **P < 0.01 versus the sham group; # P < 0.05, ## P < 0.01 versus the injured striatum in saline-treated 6-OHDA group
PF and ASICs Blockers Treatment Suppressed the Up-Regulation of ASIC1a Expression in the SN
Our previous experiment revealed that PF protected PC12 cells against MPP+ or acidic damage. Thus, we designed a series of studies to investigate more deeply the relationship between the PF’s neuroprotection and ASIC1a in an invivo model. We observed that expression of ASIC1a was remarkably higher in 6-OHDA-lesioned SN treated with saline compared to expression in the SN of sham rats (**P < 0.01) (Fig. 5a), and the increased expression of ASIC1a in lesioned SN of PD rats co-localized with TH (Fig. 5b, c). These findings indicate that the activation of ASIC1a was caused by 6-OHDA toxicity which may have induced the changes of pH. PF (30 mg/kg) and ASICs blockers (PcTx1 0.7 µg/kg, amiloride 10 mg/kg) each significantly inhibited the increase of ASIC1a expression in the lesioned SN to different degrees compared with ASIC1a expression in the saline-treated group (## P < 0.01) (Fig. 5a). These data suggest that, like ASICs blockers (PcTx1, amiloride), PF inhibited the activation of ASIC1a induced by 6-OHDA.
Effects of PF and ASICs-blocker (PcTx1, amiloride) treatment on up-regulation of ASIC1a expression in the SN. a Treatment with PF (30 mg/kg), PcTx1 (0.7 µg/kg) and Ami (10 mg/kg) for 3 weeks inhibited the increase of ASIC1a expression in 6-OHDA-lesioned SN, n = 5. b, c Seven weeks after 6-OHDA injection, this toxin induced significant increase of ASIC1a expression in the lesioned SN. Data are expressed as the mean ± SEM, n = 4. **P < 0.01 versus the sham group; ## P < 0.01 versus the injured SN in saline-treated 6-OHDA group. Pictures were observed and taken with a confocal microscope. Photos were taken at ×200 magnification (Scale bar 50 µm) (b) and ×630 magnification (Scale bar 20 µm) (c)
PF and ASICs Blockers Inhibited the α-SYN Accumulation in the SN Induced by 6-OHDA
α-SYN aggregation likely contributes to PD pathogenesis, and the ALP is a critical route for this protein degradation [4, 5, 23–25]. A previous study in our lab demonstrated that PF protects PC12 cells by increasing the autophagic degradation of α-SYN [18]. Thus, in the present study, we continued to investigate whether PF could also reduce the level of α-SYN in vivo. We found that α-SYN expression in the 6-OHDA-lesioned side treated with saline was higher than that in sham rats (**P < 0.01) (Fig. 6a). As expected, both PF (30 mg/kg) and ASICs blockers (PcTx1 0.7 µg/kg, amiloride 10 mg/kg) dramatically reduced the α-SYN level in 6-OHDA-lesioned SN to different degrees (## P < 0.01) (Fig. 6a). These data suggest that 6-OHDA neurotoxicity can cause abnormal α-SYN accumulation, as previous studies reported [26]. Numerous studies have investigated the correlation between α-SYN overexpression and cell death. A previous report showed that overexpression of human α-SYN causes human DA neuronal death [27]. Other studies also showed that knockdown of endogenous α-SYN levels could attenuate some neurotoxicity in vitro [28, 29]. Thus, we infer that PF and ASICs blockers (PcTx1, amiloride) might protect DA neurons in vivo by alleviation of the α-SYN accumulation.
Effects of PF and ASICs-blocker (PcTx1, amiloride) treatment on α-SYN, LC3-II and p62 up-regulated expression in the SN after 6-OHDA lesion. The protein expression was tested by western blotting analysis. aTreatment with PF (30 mg/kg), PcTx1 (0.7 µg/kg) and Ami (10 mg/kg) for 3 weeks attenuated 6-OHDA-induceded increase of α-SYN expression in the SN. b, c Treatment with PF, PcTx1 and Ami for 3 weeks decreased expression of LC3-II and p62. Data are expressed as the mean ± SEM, n = 4. **P < 0.01 versus the sham group; ## P < 0.01 versus the injured SN in the saline-treated 6-OHDA group
Our previous data showed that the MPP+-induced autophagic impairment potentially leads to α-SYN aggregation in PC12 cells. Thus, we further tested the expression of LC3-II and p62, which are autophagic markers to evaluate the autophagic activity in vivo. Western blotting showed that LC3-II and p62 levels in lesioned SN of PD rats treated with saline were markedly higher than those in sham rats (**P < 0.01) (Fig. 6b, c). However, both PF (30 mg/kg) and ASICs blockers (PcTx1 0.7 µg/kg, amiloride 10 mg/kg) significantly decreased the levels of LC3-II and p62 (## P < 0.01) (Fig. 6b, c). These results imply that, despite autophagic activation, the autophagic process in DA-neurons was incomplete, and also suggest that PF and ASICs blockers (PcTx1, amiloride) enhanced α-SYN degradation by ameliorating autophagic impairment.
ASIC1a Knockdown Alleviated the α-SYN Accumulation in PC12 Cells Induced by 6-OHDA
Because our results indicated that ASICs blockers (PcTx1, amiloride) could enhance the clearance of α-SYN, we directly examined the involvement of ASIC1a in 6-OHDA-induced α-SYN accumulation by evaluating the α-SYN expression in ASIC1a deficient cells using an RNA–interfering technique. Western blotting showed that, compared with the control siRNA cells, the transfection of ASIC1a siRNA-3 led to a significant downregulation of ASIC1a-protein expression in PC12 cells (**P < 0.01) (Fig. 7a). Thus, the siRNA-3 was used in the following experiment. After knockdown of ASIC1a, PC12 cells were incubated in the presence or absence of 6-OHDA (50 µM), and then we evaluated the ASIC1a and α-SYN expression by western blotting. In the control siRNA cells, we observed an increase in ASIC1a and α-SYN expression in 6-OHDA treated cells (*P < 0.05). However, knockdown of ASIC1a inhibited the increase of ASIC1a and a-SYN levels in 6-OHDA-induced PC12 cells (# P < 0.05, ## P < 0.01) (Fig. 7b, c). These results indicate that the α-SYN clearance was enhanced when the activation of ASIC1a was suppressed.
Down-regulated expression of α-SYN, LC3-II and p62 in PC12 cells after knockdown of ASIC1a. a PC12 cells were transfected with ASIC1a siRNA-1, siRNA-2, siRNA-3, or negative siRNA as a control. ASIC1a siRNA-3 effectively inhibited the ASIC1a protein level and was used in the following study. b, c After knockdown of ASIC1a, the increased levels of ASIC1a and α-SYN were inhibited in 6-OHDA-induced PC12 cells. d Due to knockdown of ASIC1a, levels of LC3-II and p62 significantly decreased in ASIC1a siRNA PC12 cells even with 6-OHDA (50 µM) compared with levels in 6-OHDA-treated control siRNA cells. Data are expressed as the mean ± SEM, n = 3. *P < 0.05, **P < 0.01 versus the control or control siRNA; # P < 0.05, ## P < 0.01 versus the 6-OHDA-treated control siRNA
As the ALP is critical for clearing misfolded α-SYN [30], we examined the autophagic activity by measuring the levels of autophagic markers (LC3II and p62) after ASIC1a knockdown. Western blotting also showed the upregulation of LC3-II and p62 in the 6-OHDA-induced control siRNA cells, just like the result in the rat model (*P < 0.05). However, the levels of LC3-II and p62 decreased partly in 6-OHDA treated- PC12 cells in response to ASIC1a-gene knockdown (# P < 0.05) (Fig. 7d).
Discussion
PF can cross the blood–brain barrier and has extensive pharmacological effects in the nervous system [19, 31]. Recently, the effect of PF on DA-neuronal degeneration in PD has attracted increasing attention. Accumulating evidence suggests that PF modulates the autophagic activity, which is a main pathway to clear misfolded or aggregated proteins such as α-SYN, a possible toxic mediator of pathology in PD [24, 32, 33]. Our previous work found that both PF and amiloride could protect PC12 cells against MPP+ and acidic injury by enhancing autophagic degradation of α-SYN and that PF’s protective effects may be closely associated with its action on ASICs. All these findings encouraged us to further evaluate the therapeutic value of PF and test whether its therapeutic effect is connected with its inhibitory effect on ASIC1a in an in vivo model.
6-OHDA, has been used to induce death of DA-neurons in PD models for over 30 years [34]. Because of the similarity to DA and high affinity to DAT, 6-OHDA is often mistakenly taken up by DA-neurons [35]. The neuronal damage and eventual death induced by 6-OHDA is mainly attributable to the massive oxidative stress caused by the toxin. In this study, a model based on the unilateral striatal injection of 6-OHDA was chosen because the process of neuronal degeneration caused by 6-OHDA is similar to the clinical progression of PD [36]. As the loss of TH+ neurons in the SNc after intrastriatal 6-OHDA infusion reaches its maximum value at week 4, the onset of experimental intervention at this time point was designed to test the neuroprotective effect of PF [37].
In recent years, numerous studies have investigated ASICs. ASICs, a type of H+-gated cation channel, are characterized by acid sensitivity and can be activated by changes in pH [9, 10]. Most nervous system diseases such as cerebral ischemia, seizures and PD, are accompanied by brain tissue acidosis; given the sensitivity of ASICs to pH, the activation of ASICs may play an important role in the pathogenesis of these diseases [38–41]. Amiloride has been used as a diuretic since 1967 for the inhibition of the epithelial sodium channels (ENaCs) in the renal tubules [14]. Amiloride also blocks ASICs, members of the ENaC/Degenerin family. PcTx1 is a toxin that is extracted as a minor component (<1 % of protein content) from the venom of the South American tarantula, Psalmopoeus cambridgei [42]. Amiloride and PcTx1 have neuroprotective effects in rodent models of PD, Huntington’s disease, multiple sclerosis, and cerebral ischemia [14, 43–45]. Thus, we chose amiloride and PcTx1 as positive controls in this study. We found that PF and these ASICs blockers, amiloride and PcTx1, markedly ameliorated APO-induced rotational behavior in unilaterally 6-OHDA-lesioned rats. Meanwhile, the immunohistochemistry and HPLC data further showed that PF and the ASICs blockers (amiloride, PcTX1) alleviated the loss of DA-neurons in the SNc and decreased the levels of DA and its metabolites in the striatum of PD model rats. Though the above-mentioned data show that PF and the ASICs blockers only got the effect of partial restoration due to irreversible changes occurring before treatment initiation, we believe this limitation is consistent with the clinical condition being investigated. These results reveal that PF and the ASICs blockers could indeed protect DA-neurons in the SN against 6-OHDA-induced damage. These results, together with those from previous reports, demonstrate that PF may be a potential therapeutic drug for PD [31, 46]. These findings further suggest a possible relationship between the protective effects of PF and its action on ASICs.
Until now, no direct evidence had confirmed a decrease of pH in DA-neurons that were subjected to 6-OHDA toxin. However, the accumulated toxin in the cytoplasm results in acceleration of oxidation and inhibition of mitochondrial oxidative respiratory chain complexes I and IV, so that glycolysis becomes active and lactic acid accumulates, which may ultimately lead the pathological activation of ASICs [47]. Of course, 6-OHDA can also cause cell toxicity via other pathways [26]. In our study, western blotting showed the enhancement of ASIC1a levels in the lesioned side of model rats, and immunofluorescence also showed significantly increased expression of ASIC1a, which was co-localized with TH, in the SN with 6-OHDA-induced damage. Similar results were found in 6-OHDA-induced PC12 cells. These findings indicate pathological activation of ASIC1a induced by 6-OHDA and further suggest that ASIC1a may be related to the pathogenesis of PD, consistent with previous reports and our previous results [14, 17, 18].
Previous reports did not provide direct evidence of the relationship between the protective effects of PF and its inhibitory effects on ASICs. But our previous research revealed that PF could protect PC12 cells against acidic damage. Additionally, whole-cell patch recording configuration revealed that PF could block the acid-induced current in PC12 cells in a dose-dependent manner just as amiloride or PcTx1 did [17, 18]. In the present study, western blotting results further showed that PF reduced the ASIC1a levels significantly, just like ASICs blockers (PcTx1, amiloride). These results clearly indicate the action of PF on ASIC1s. Thus, we infer that PF may protect DA-neurons by inhibiting the activation of ASICs, especially ASIC1a.
α-SYN is one of the pathological hallmarks of PD [5]. Aggregation of abnormal proteins such as α-SYN, is toxic and may result in damage or even death of neurons [48]. Therefore, inhibition of the abnormal accumulation of α-SYN is becoming a promising therapeutic strategy for PD. In PD, intraneuronal α-SYN is maintained at normal levels via the UPS and ALP. ALP plays an especially important role in the onset and progression of PD [23–25]. To a certain extent, autophagy can protect cells against a variety of damage, but excessive activation of autophagy or autophagic dysfunction will result in the pathogenesis of some neurodegenerative diseases such as PD [49]. The level of LC-3 II reflects autophagic activity and is closely related to the quantity of autophagosomes [50]. p62/SQSTM1, one of the substrates and a ubiquitin-conjugated protein, is degraded through autophagy when bound to the LC3 and ubiquitinated protein [51, 52]. Although 6-OHDA does not produce α-SYN oligomers in the nigrostriatal pathway, several previous studies showed that 6-OHDA-induced neurotoxicity not only triggered an oxidative burst and dysregulation autophagy, but also caused α-SYN accumulation in vitro and in vivo [26, 53, 54]. We also found that the levels of α-SYN, LC-3 II, and p62 were higher in rates with 6-OHDA-induced injury than those in rats from the sham group with no exception. These data suggest that autophagic activation may be a neuroprotective mechanism to degrade aberrant protein elicited by 6-OHDA toxicity, but the disruption of autophagic flux, which is reflected by increased p62 levels will lead to the accumulation of α-SYN.
Thusfar, we know that ASICs are closely linked to the UPS [43], a protein degradation pathway, but there is no adequate evidence to verify the direct connection between ASICs and ALP activity. Our earlier studies have shown that acidosis induces α-SYN accumulation, enhancement of α-SYN autophagic degradation via blocking ASICs may contribute to protecting PC12 against MPP+ or acidic damage. An interesting discovery in this study is that PF partly reversed the effect of 6-OHDA toxin on α-SYN accumulation and disruption of autophagic flux, and ASICs blockers (PcTx1, amiloride) exhibited similar effects. Thus, these data suggest that the activation of ASIC1a may be involved in the dysfunction of the α-SYN autophagic degradation pathways.
To prove a direct relationship between ASIC1a and 6-OHDA-induced abnormal α-SYN accumulation, we first used specific ASIC1a siRNA to evaluate the expression of α-SYN, LC-3 II, and p62 in ASIC1a -suppressed PC12 cells. In agreement with our results in vivo, we found increased levels of α-SYN, LC-3 II, and p62 in 6-OHDA-induced control siRNA cells. Knockdown of ASIC1a resulted in the enhancement of α-SYN clearance and partial restoration of autophagic injury in siRNA transfected cells treated with 6-OHDA. These findings imply that activation of ASIC1a is probably linked to the impairment of α-SYN clearance, and ASIC1a may be a vital upstream regulator in the autophagic degradation process.
ASIC1a is permeable to Ca2+, so the activation of these channels can induce calcium influx in neurons [55]. A recent study found that an intracellular Ca2+ increase activates a variety of kinases and proteases associated with an autophagic signal [56]. Hcyer-Hansen et al. also demonstrated that the activation of autophagy was mediated by Ca2+/calmodulin-dependent kinase kinase-beta and adenosine monophosphate-activated protein kinase [57]. In addition, Ca2+ could regulate autophagy by the Ca2+- calpain -Gsa non-mTOR pathway [58]. Both our previous data and the present study provide evidence that PF can suppress the activation of ASICs. Thus, we believe PF’s neuroprotective effects result from its inhibition of ASIC1a activity, which in turn ameliorates autophagic dysfunction induced by calcium influx.
In conclusion, our present data clearly demonstrate that systemic administration of PF or ASICs blockers improved behavioral symptoms, delayed DA neuronal loss and attenuated the reduction in levels of DA and its metabolites in PD model. PF may be a neuroprotectant by its effect on ASIC1a; and, thus, ASIC1a may be a potential target for treatment of PD because of the close relationship between ASIC1a and autophagic degradation.
References
Pan T, Kondo S, Le W, Jankovic J (2008) The role of autophagy-lysosome pathway in neurodegeneration associated with Parkinson’s disease. Brain 131:1969–1978
Tofaris GK (2012) Lysosome-dependent pathways as a unifying theme in Parkinson’s disease. Mov Disord 27:1364–1369
Hirsch EC, Jenner P, Przedborski S (2013) Pathogenesis of Parkinson’s disease. Mov Disord 28:24–30
Fujiwara H, Hasegawa M, Dohmae N, Kawashima A, Masliah E, Goldberg MS, Shen J, Takio K, Iwatsubo T (2002) Alpha-synuclein is phosphorylated in synucleinopathy lesions. Nat Cell Biol 4:160–164
Spillantini MG, Schmidt ML, Lee VM, Trojanowski JQ, Jakes R, Goedert M (1997) Alpha-synuclein in Lewy bodies. Nature 388:839–840
Kaushik S, Cuervo AM (2012) Chaperone-mediated autophagy: a unique way to enter the lysosome world. Trends Cell Biol 22:407–417
Hara T, Nakamura K, Matsui M, Yamamoto A, Nakahara Y, Suzuki-Migishima R, Yokoyama M, Mishima K, Saito I, Okano H, Mizushima N (2006) Suppression of basal autophagy in neural cells causes neurodegenerative disease in mice. Nature 441:885–889
Komatsu M, Waguri S, Chiba T, Murata S, Iwata J, Tanida I, Ueno T, Koike M, Uchiyama Y, Kominami E, Tanaka K (2006) Loss of autophagy in the central nervous system causes neurodegeneration in mice. Nature 441:880–884
Yu Y, Chen Z, Li WG, Cao H, Feng EG, Yu F, Liu H, Jiang H, Xu TL (2010) A nonproton ligand sensor in the acid-sensing ion channel. Neuron 68:61–72
Alvarez de la Rosa D, Canessa CM, Fyfe GK, Zhang P (2000) Structure and regulation of amiloride-sensitive sodium channels. Annu Rev Physiol 62:573–594
Waldmann R, Champigny G, Bassilana F, Heurteaux C, Lazdunski M (1997) A proton-gated cation channel involved in acid-sensing. Nature 386:173–177
Xiong ZG, Zhu XM, Chu XP, Minami M, Hey J, Wei WL, MacDonald JF, Wemmie JA, Price MP, Welsh MJ, Simon RP (2004) Neuroprotection in ischemia: blocking calcium-permeable acid-sensing ion channels. Cell 118:687–698
Sherwood TW, Lee KG, Gormley MG, Askwith CC (2011) Heteromeric acid-sensing ion channels (ASICs) composed of ASIC2b and ASIC1a display novel channel properties and contribute to acidosis-induced neuronal death. J Neurosci 31:9723–9734
Arias RL, Sung ML, Vasylyev D, Zhang MY, Albinson K, Kubek K, Kagan N, Beyer C, Lin Q, Dwyer JM, Zaleska MM, Bowlby MR, Dunlop J, Monaghan M (2008) Amiloride is neuroprotective in an MPTP model of Parkinson’s disease. Neurobiol Dis 31:334–341
Pidoplichko VI, Dani JA (2006) Acid-sensitive ionic channels in midbrain dopamine neurons are sensitive to ammonium, which may contribute to hyperammonemia damage. Proc Natl Acad Sci USA 103:11376–11380
Chu XP, Miesch J, Johnson M, Root L, Zhu XM, Chen D, Simon RP, Xiong ZG (2002) Proton-gated channels in PC12 cells. J Neurophysiol 87:2555–2561
Cao BY, Yang YP, Luo WF, Mao CJ, Han R, Sun X, Cheng J, Liu CF (2010) Paeoniflorin, a potent natural compound, protects PC12 cells from MPP+ and acidic damage via autophagic pathway. J Ethnopharmacol 131:122–129
Sun X, Cao YB, Hu LF, Yang YP, Li J, Wang F, Liu CF (2011) ASICs mediate the modulatory effect by paeoniflorin on alpha-synuclein autophagic degradation. Brain Res 1396:77–87
Hu ZY, Xu L, Yan R, Huang Y, Liu G, Zhou WX, Zhang YX (2013) Advance in studies on effect of paeoniflorin on nervous system. Zhongguo Zhong yao za zhi 38:297–301
Zhang W, Dai SM (2012) Mechanisms involved in the therapeutic effects of Paeonia lactiflora pallas in rheumatoid arthritis. Int Immunopharmacol 14:27–31
Huang KS, Lin JG, Lee HC, Tsai FJ, Bau DT, Huang CY, Yao CH, Chen YS (2011) Paeoniae alba radix promotes peripheral nerve regeneration. Evid Based Complement Alternat Med 2011:109809
Paxinos G, Watson C (1986) The rat brain in stereotaxic coordinates. Academic, New York
Martinez-Vicente M, Cuervo AM (2007) Autophagy and neurodegeneration: when the cleaning crew goes on strike. Lancet Neurol 6:352–361
Levine B, Kroemer G (2008) Autophagy in the pathogenesis of disease. Cell 132:27–42
Mizushima N, Levine B, Cuervo AM, Klionsky DJ (2008) Autophagy fights disease through cellular self-digestion. Nature 451:1069–1075
Wei X, He S, Wang Z, Wu J, Zhang J, Cheng Y, Yang J, Xu X, Chen Z, Ye J, Chen L, Lin L, Xiao J (2014) Fibroblast growth factor 1attenuates 6-hydroxydopamine-induced neurotoxicity: an in vitro and in vivo investigation in experimental models of Parkinson’s disease. Am J Transl Res 6:664–677
Zhou W, Schaack J, Zawada WM, Freed CR (2002) Overexpression of human alpha-synuclein causes dopamine neuron death in primary human mesencephalic culture. Brain Res 926:42–50
Chen L, Huang E, Wang H, Qiu P, Liu C (2013) RNA interference targeting alpha-synuclein attenuates methamphetamine-induced neurotoxicity in SH-SY5Y cells. Brain Res 1521:59–67
Saberzadeh J, Arabsolghar R, Takhshid MA (2016) Alpha synuclein protein is involved in aluminum-induced cell death and oxidative stress in PC12 cells. Brain Res 1635:153–160
Crews L, Spencer B, Desplats P, Patrick C, Paulino A, Rockenstein E, Hansen L, Adame A, Galasko D, Masliah E (2010) Selective molecular alterations in the autophagy pathway in patients with Lewy body disease and in models of alpha-synucleinopathy. PloS One 5:e9313
Dong H, Li R, Yu C, Xu T, Zhang X, Dong M (2015) Paeoniflorin inhibition of 6-hydroxydopamine-induced apoptosis in PC12 cells via suppressing reactive oxygen species-mediated PKCdelta/NF-kappaB pathway. Neuroscience 285:70–80
Wu H, Li W, Wang T, Shu Y, Liu P (2008) Paeoniflorin suppress NF-kappaB activation through modulation of I kappaB alpha and enhances 5-fluorouracil-induced apoptosis in human gastric carcinoma cells. Biomed Pharmacother 62:659–666
Winslow AR, Rubinsztein DC (2011) The Parkinson disease protein alpha-synuclein inhibits autophagy. Autophagy 7:429–431
Ungerstedt U (1968) 6-Hydroxy-dopamine induced degeneration of central monoamine neurons. Eur J Pharmacol 5:107–110
Blandini F, Armentero MT (2012) Animal models of Parkinson’s disease. FEBS J 279:1156–1166
Schwarting RK, Huston JP (1996) The unilateral 6-hydroxydopamine lesion model in behavioral brain research. Analysis of functional deficits, recovery and treatments. Prog Neurobiol 50:275–331
Blandini F, Armentero MT, Martignoni E (2008) The 6-hydroxydopamine model: news from the past. Parkinsonism Relat Disord 14 Suppl 2:S124–129
Noel J, Salinas M, Baron A, Diochot S, Deval E, Lingueglia E (2010) Current perspectives on acid-sensing ion channels: new advances and therapeutic implications. Expert Rev Clin Pharmacol 3:331–346
Sluka KA, Winter OC, Wemmie JA (2009) Acid-sensing ion channels: a new target for pain and CNS diseases. Curr Opin Drug Discov Dev 12:693–704
Chu XP, Xiong ZG (2012) Physiological and pathological functions of acid-sensing ion channels in the central nervous system. Curr Drug Targets 13:263–271
Grunder S, Chen X (2010) Structure, function, and pharmacology of acid-sensing ion channels (ASICs): focus on ASIC1a. Int J Physiol Pathophysiol Pharmacol 2:73–94
Baron A, Diochot S, Salinas M, Deval E, Noel J, Lingueglia E (2013) Venom toxins in the exploration of molecular, physiological and pathophysiological functions of acid-sensing ion channels. Toxicon 75:187–204
Wong HK, Bauer PO, Kurosawa M, Goswami A, Washizu C, Machida Y, Tosaki A, Yamada M, Knopfel T, Nakamura T, Nukina N (2008) Blocking acid-sensing ion channel 1 alleviates Huntington’s disease pathology via an ubiquitin–proteasome system-dependent mechanism. Hum Mol Genet 17:3223–3235
Friese MA, Craner MJ, Etzensperger R, Vergo S, Wemmie JA, Welsh MJ, Vincent A, Fugger L (2007) Acid-sensing ion channel-1 contributes to axonal degeneration in autoimmune inflammation of the central nervous system. Nat Med 13:1483–1489
Turner RJ, Van den Heuvel C, Vink R (2004) Amiloride increases neuronal damage after traumatic brain injury in rats. J Am Coll Nutr 23:534S–537S
Liu DZ, Zhu J, Jin DZ, Zhang LM, Ji XQ, Ye Y, Tang CP, Zhu XZ (2007) Behavioral recovery following sub-chronic paeoniflorin administration in the striatal 6-OHDA lesion rodent model of Parkinson’s disease. J Ethnopharmacol 112:327–332
Duty S, Jenner P (2011) Animal models of Parkinson’s disease: a source of novel treatments and clues to the cause of the disease. Br J Pharmacol 164:1357–1391
Greenbaum EA, Graves CL, Mishizen-Eberz AJ, Lupoli MA, Lynch DR, Englander SW, Axelsen PH, Giasson BI (2005) The E46K mutation in alpha-synuclein increases amyloid fibril formation. J Biol Chem 280:7800–7807
Cherra SJ 3rd, Chu CT (2008) Autophagy in neuroprotection and neurodegeneration: a question of balance. Future Neurol 3:309–323
Jiang M, Fernandez S, Jerome WG, He Y, Yu X, Cai H, Boone B, Yi Y, Magnuson MA, Roy-Burman P, Matusik RJ, Shappell SB, Hayward SW (2010) Disruption of PPARgamma signaling results in mouse prostatic intraepithelial neoplasia involving active autophagy. Cell Death Differ 17:469–481
Pankiv S, Clausen TH, Lamark T, Brech A, Bruun JA, Outzen H, Overvatn A, Bjorkoy G, Johansen T (2007) p62/SQSTM1 binds directly to Atg8/LC3 to facilitate degradation of ubiquitinated protein aggregates by autophagy. J Biol Chem 282:24131–24145
Bjorkoy G, Lamark T, Brech A, Outzen H, Perander M, Overvatn A, Stenmark H, Johansen T (2005) p62/SQSTM1 forms protein aggregates degraded by autophagy and has a protective effect on huntingtin-induced cell death. J Cell Biol 171:603–614
Fouillet A, Levet C, Virgone A, Robin M, Dourlen P, Rieusset J, Belaidi E, Ovize M, Touret M, Nataf S, Mollereau B (2012) ER stress inhibits neuronal death by promoting autophagy. Autophagy 8:915–926
Dagda RK, Das Banerjee T, Janda E (2013) How Parkinsonian toxins dysregulate the autophagy machinery. Int J Mol Sci 14:22163–22189
Mari Y, Katnik C, Cuevas J (2010) ASIC1a channels are activated by endogenous protons during ischemia and contribute to synergistic potentiation of intracellular Ca(2+) overload during ischemia and acidosis. Cell Calcium 48:70–82
East DA, Campanella M (2013) Ca2+ in quality control: an unresolved riddle critical to autophagy and mitophagy. Autophagy 9:1710–1719
Hoyer-Hansen M, Bastholm L, Szyniarowski P, Campanella M, Szabadkai G, Farkas T, Bianchi K, Fehrenbacher N, Elling F, Rizzuto R, Mathiasen IS, Jaattela M (2007) Control of macroautophagy by calcium, calmodulin-dependent kinase kinase-beta, and Bcl-2. Mol Cell 25:193–205
Polymeropoulos MH, Higgins JJ, Golbe LI, Johnson WG, Ide SE, Di Iorio G, Sanges G, Stenroos ES, Pho LT, Schaffer AA, Lazzarini AM, Nussbaum RL, Duvoisin RC (1996) Mapping of a gene for Parkinson’s disease to chromosome 4q21-q23. Science 274:1197–1199
Acknowledgments
This work was supported by the National Natural Science Foundation of China (81471299, 81301090), the Research Fund for the Doctoral Program of Higher Education of China (RFDP, 20123201110015), the Jiangsu Provincial Special Program of Medical Science (BL2014042), the Suzhou Clinical Research Center of Neurological Disease (Szzx201503), and the Science and Technology Project of Nantong (MS 22015082). This work was also partially supported by the Priority Academic Program Development of Jiangsu Higher Education Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there are no conflicts of interest.
Additional information
Xiao-Su Gu and Fen Wang have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Gu, XS., Wang, F., Zhang, CY. et al. Neuroprotective Effects of Paeoniflorin on 6-OHDA-Lesioned Rat Model of Parkinson’s Disease. Neurochem Res 41, 2923–2936 (2016). https://doi.org/10.1007/s11064-016-2011-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-016-2011-0