Abstract
Purpose
To report preliminary outcomes of high dose image-guided intensity modulated radiotherapy (IG-IMRT) in the treatment of chordomas of the sacrum, mobile spine and skull base.
Methods
Retrospective analysis of chordoma patients treated with surgery and/or radiotherapy (RT) in a single tertiary cancer center. Initial treatment was categorized as (A) Adjuvant or definitive high-dose RT (78 Gy/39fx or 24 Gy/1fx) vs (B) surgery-only or low dose RT. The primary endpoint was the cumulative incidence of local failure.
Results
A total of 31 patients were treated from 2010 through 2020. Median age was 55 years, tumor location was 64% sacrum, 13% lumbar, 16% cervical and 6% clivus. Median tumor volume was 148 cc (8.3 cm in largest diameter), 42% of patients received curative-intent surgery and 65% received primary RT (adjuvant or definitive). 5-year cumulative incidence of local failure was 48% in group A vs 83% in group B (p = 0.041). Tumor size > 330 cc was associated with local failure (SHR 2.2, 95% CI 1.12 to 7.45; p = 0.028). Eight patients developed distant metastases, with a median metastases-free survival of 56.1 months. 5-year survival for patients that received high dose RT was 72% vs 76% in patients that received no or low dose RT (p = 0.63).
Conclusion
Our study suggests high-dose photon IG-IMRT improves local control in the initial management of chordomas. Health systems should promote reference centers with clinical expertise and technical capabilities to improve outcomes for this complex disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chordomas are rare neoplasms arising from persistent notochordal elements. Incidence is approximately 0.8 per 100.000 inhabitants [1]. Sites of origin are sacrum (50%), skull base (30%), and mobile spine (20%). Chordomas are generally indolent, but locally invasive and destructive. Overall, disease morbidity is more a function of its local aggressiveness than its potential to metastasize [2].
Surgery plus particle therapy has historically been considered the gold standard treatment for chordomas [2,3,4,5,6]. Nevertheless, worldwide, there are access barriers to particle therapy. Ninety-one percent of the centers are located in high income countries [7], whereas 84% of the world population lives in Low and Middle Income Countries [8]. There are no centers in Latin America, Africa or Oceania [7].
Preliminary data suggests highly conformal high dose image-guided intensity modulated photon radiotherapy (IG-IMRT) is an alternative to treat chordoma patients [9, 10]. However, due to poor outcomes of low-dose photon radiation [11], surgeons in regions without access to particle therapy have historically been reluctant to refer patients to radiotherapy.
In 2014, we started a Multidisciplinary High Dose Photon IG-IMRT program to treat patients with Chordoma. The aim of this study is to report preliminary outcomes with high dose IG-IMRT and compare it with patients receiving none or low-dose radiotherapy.
Methods
This is a retrospective cohort of patients treated for chordoma at Instituto do Cancer do Estado de São Paulo (ICESP), an academic tertiary cancer center in in São Paulo, Brazil. We included all patients with histologically proven chordomas treated with surgery and/or radiotherapy (RT) between June 2010 and October 2020. Patients that received biopsy-only with no further treatment were excluded. All patients had pathology reviewed at our center and were histologically classified into conventional, atypical, poorly differentiated and dedifferentiated chordomas [12]. There were no age criteria in the study, though generally adult patients are referred to our center.
Surgery
We included patients who were operated on at this institution and those who received previous surgery at other institutions and were referred for adjuvant or salvage treatment. Surgery was rated as palliative if the intention of the procedure was to alleviate pain or improve function without significant tumor removal; curative intent if the surgeon planned a complete removal of the tumor, regardless of the margin. Tumor removal was further classified into en bloc or piecemeal.
Radiotherapy planning and delivery
For high dose IG-IMRT, patients with base of skull and cervical lesions were immobilized with thermoplastic mask. Patients with mobile-spine and sacral lesions were immobilized with body-fix. Simulation CT with 2-mm slice thickness was obtained and co-registered with Magnetic Resonance Imaging (MRI) for delineation. In cases with spinal instrumentation, CT myelography was performed as needed for additional spinal cord conspicuity.
Clinical Target Volume (CTV) included Gross Tumor Volume (GTV) and areas at-risk for local relapse, established by pre- and post- op images and, when available, surgeon’s input from intra-operative findings. GTV to High-risk CTV [2] margins depended on tumor site, surgical procedure and nearby critical organs at risk (OAR). As a general guideline, high-risk CTV included the entire bone compartment, 1–5 mm margin around soft tissue invasion in cervical and clivus chordomas and 5–10 mm in sacral and lumbar chordomas. An additional margin could be applied for possible soft tissue oedema throughout treatment. CTV editing was performed to remove overlap with uninvolved critical OAR. High-risk CTV was treated to 78 Gy in 39 fractions (2 Gy/fx).
Intermediate-risk CTV margins were highly variable and evolved over time. In the beginning of our experience volumes were tighter. Currently, for small intact chordomas, we still consider omitting intermediate risk CTV or treating only the biopsy path. Conversely, for post-op cases, wider margins are applied to treat the surgical bed and respective anatomical compartments. Our general policy is to cover the entire surgical access to the skin, especially in atypical chordomas. Intermediate-risk CTV was treated to 60–70 Gy in 39 fractions (simultaneous integrated boost). No bolus was added to skin scars.
The spinal cord was delineated on T2-weighed MRI or CT myelography. PRV spinal cord was the true cord plus 1.5 mm margin. PRV spinal cord maximum (0.03 cc) dose started at 64 Gy in the beginning of our series and is now at 67 Gy for cervical and 63 Gy for lumbar or thoracic spine. Earlier, uninvolved nerve roots and cauda equina received ≤ 66 Gy and nerve roots encompassed by the tumor received prescription dose with “no hot spot”. Currently, in mobile spine chordoma, it´s our policy to discuss the potential implications of any given nerve or plexus injury with the patient and, upon written consent, cover the GTV with at least 74 Gy. This approach applies to all OAR except the spinal cord and brainstem. A full list of dose constraints is available on the supplementary appendix (online only).
Planning Target Volume (PTV) margin was 1–3 mm without expansion into the spinal canal. A 1 mm margin was used when tumor abutted critical OAR. Planning was performed using Volumetric Modulated Arc Therapy (a form of rotational IMRT) using 6 MV photons. Efforts were made to avoid circumferential irradiation of the esophagus, bowel and rectum. For CTV/PTV volumes bound by the skin, a 1 to 2 cm auto flash margin was added to allow for possible soft tissue oedema during treatment. Image guidance was performed with Daily Cone-Beam CT and online 6-degree correction. All patients consented for treatment and potential related morbidity according to tumor location. Figure 1 shows an example of a C2-C3 cervical chordoma.
Based on multidisciplinary team (MDT) discussion, an alternative RT schedule of Stereotactic Radiosurgery (SRS) 24 Gy single fraction (24 Gy/1fx)[13] was used in selected sacral chordoma cases. The indications were: small bowel abutting the tumor (bowel displacement procedure plus SRS), intermediate or poor prognosis concomitant cancer or symptomatic metastatic chordoma. High-dose CTV delineation followed the same general principles. PTV margin was 1–2 mm depending on OAR proximity.
Endpoints
Our primary endpoint was local control defined as absence of tumor progression on surgical bed or within PTV. After treatment, MRI was typically performed every 6 months. All images were reviewed by a dedicated musculoskeletal radiologist. We categorized patients into two groups: (A) High dose RT, defined as patients who received ≥ 74 Gy fractionated RT or 24 Gy single fraction as part of their initial treatment (either definitive or adjuvant) and (B) None or Low-dose RT, defined as patients who received surgery-only with no adjuvant RT or with dose < 74 Gy. This cut-point was based on the consensus that at least 74 Gy should be delivered to chordomas using standard fractionation [2].
Secondary endpoints were regional failure-free survival, distant metastases-free survival, overall survival and toxicity. Treatment-related toxicity was scored using Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. Time-to-event endpoints were measured from the date of the start of first treatment (surgery or radiation).
Statistical considerations
Baseline characteristics were reported using descriptive statistics. Local control was estimated using the cumulative incidence function treating death as competing event and compared using Fine and Gray model [14]. Survival curves were generated using the Kaplan–Meier method and compared using the log-rank test. Categorical variables were compared using chi-square test or Fisher´s exact test. A p-value of < 0.05 was considered significant. Statistical analyses were performed using Stata 14, College Station, TX: StataCorp LP.
This study was approved by the Institutional Review Board, Local Ethics Committee and was conducted in accordance with the Ethical Principles of the Declaration of Helsinki.
Results
From June 2010 through October 2020, 33 patients were identified. Two patients refused further treatment following biopsy and were excluded; thus, 31 patients were analyzed. Median follow-up for patients alive was 51 months (group A and B were, respectively, 45 months (range 7 to 68 months) and 60 months (19 to 123 months). Baseline characteristics of patients are summarized in Table 1. Median age was 55 years (range 32 to 75 years). Most patients had sacral chordomas (64%), followed by cervical (16%) and lumbar (13%).
Surgery
Thirteen (42%) patients received curative-intent surgery as their first treatment. Seven (23%) had a piecemeal resection; 5 (16%) had an intended en-bloc resection, of which 4 were completed. One patient with a L5-S1 chordoma had an intra-operative acute thrombosis of the right external iliac artery. The thrombus was resected, but due to cardiovascular instability, tumor removal was not completed; patient had myocardial infarction in the fifth post-op and died the following day.
Four (13%) patients received palliative surgery: three had decompression and fusion and one had decompression. Temporary organ displacement [15] was performed in 2 patients (see below).
Initial radiotherapy
Twenty (65%) patients received primary RT (15 definitive and 5 adjuvant). Three patients received initial RT at other institutions. The remaining 17 (55%) patients received RT as part of their initial treatment at ICESP. In group A, all the 13 fractionated RT patients received 78 Gy/39fx. Median fractionated RT dose in Group B was 60 Gy in 1.8-2 Gy/fx (range 45 Gy to 72 Gy); two (6%) patients with sacral chordomas received 24 Gy/1fx: one patient had concurrent stage IV rectal cancer; one patient had bowel abutting the tumor and had temporary organ displacement before SRS [15].
In patients that received initial high dose fractionated RT, median GTV, high-risk CTV and high-risk PTV volumes were, respectively, 154 cc, 197 cc and 294 cc. Median dose to 99% of GTV (D99%) was 74.2 Gy (IQR 67.4–77.5 Gy). Median D99% of high-risk CTV was 74.5 Gy (IQR 70.3–76.6 Gy). Median D95% of high-dose PTV was 77.4 Gy (IQR 75.2–78.2 Gy). A detailed description of target volumes coverage (table S1) and organ at risk doses (table S2) can be found at the online appendix.
Local control
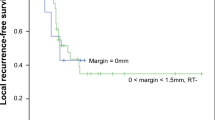
The 3- and 5-year cumulative incidence of local failure were, respectively, 29% and 48% in group A versus 60% and 83% in group B (p = 0.041), suggesting high dose RT as part of the initial treatment significantly increased local control (Fig. 2).
Tumor size > 330 cc was associated with local failure (SHR 2.2, 95% CI 1.12 to 7.45; p = 0.028) while histology was not (SHR 1.85, 95% CI 0.47 to 6.99; p = 0.38).
Figure 3 shows an example of a large sacral chordoma treated to 78 Gy in 39 fractions that slowly regressed during follow-up.
A 56-year-old male patient with a large sacral chordoma displacing the rectum; a Pretreatment T2-weighted images; b Volumetric Modulated Arc Therapy isodoses, prescription was 78 Gy in 39 fractions c 18 months posttreatment T2-weighted fat saturated images depicting reduction of the presacral component
Regional failure-free survival
High initial RT dose had no impact on regional failure-free survival (p = 0.75), whereas patients that received primary surgery were at higher risk for regional relapse (p = 0.01). Median regional relapse-free survival for patients with initial surgery (with or without adjuvant RT) was 31 months versus 54.1 months in patients who received primary treatment without surgery (HR 5.2; 95% CI 1.12 to 25).
Distant metastases-free survival
A total of 8 patients developed distant metastasis. Median metastases-free survival was 56.1 months, with no difference between patients from group A or B (p = 0.8). Histologic subtype significantly influenced the occurrence of metastases. Median metastases-free survival was 56.1 months in patients with conventional vs 39.1 months in patients with atypical chordoma.
Survival
5-year survival for patients that received high dose RT was 72% versus 76% in patients that received no or low dose RT. As our high-dose program started in 2014, these patients had a comparatively shorter follow-up. Median survival was not reached in patients treated with high-dose RT versus 98.9 months in patients treated with none or low-dose RT (p = 0.63) (Fig. 4).
Nine patients died during follow-up. In the high-dose RT group, two patients died without evidence of disease progression: one patient with a C2-C3 chordoma treated with 78 Gy died at 19 months of follow-up during a myocardial revascularization surgery. One patient was initially seen at an outside hospital due to acute intestinal obstruction in 2016. He underwent exploratory laparotomy, in which a pT3pNx (KRAS mutated) rectosigmoid adenocarcinoma was resected through an anterior approach. He was then referred to our center, where staging revealed multiple lung and liver metastases and a “S3–S5 10.8 cm sacral mass”. He received 1st line FLOX chemo with partial response in the lung and liver, but stability of the sacral lesion. Biopsy revealed a conventional chordoma. After MDT discussion in 2017, we treated the sacral chordoma with 24 Gy/1fx. During follow-up, patient experienced liver, lung and bone progression with CEA elevation. Clinical course was compatible with metastatic colorectal cancer and no biopsy was felt necessary. Patient received further systemic treatments alternating between response, stability and progression. In 2019, patient developed CNS metastasis and eventually died of progressive colorectal cancer. Throughout 29.8 months of follow-up, there was no progression of the sacral chordoma.
A 63-year-old female patient with a 6.3 cm S3–S5 atypical chordoma was treated with temporary bowel displacement and 24 Gy/1fx. At 11 months, MRI showed a small volume increase that was initially believed to be pseudoprogression. At 17 months, repeat MRI confirmed a true progression that was retrospectively declared at 11 months. Patient underwent salvage en bloc resection with complete removal of the tumor. Postoperatively, she developed multiple infections with prolonged ICU stay due to sepsis and renal failure. She died 30 days after surgery at 20.8 months of follow-up.
Salvage radiotherapy
Six (19%) patients received salvage radiotherapy. Due to the small number of patients, we provide descriptive details with no formal statistical analysis.
Four patients received high-dose salvage RT. One patient with sacral chordoma previously had surgery and adjuvant RT 45 Gy/25fx. She presented to us with a 5.1 cm local relapse at the level of S2. We performed bowel displacement with saline infusion and treated the lesion with SRS 24 Gy/1fx. The patient developed local progression 43 months after retreatment. One patient received SRS for a 4 cm sciatic nerve metastasis. The lesion remained controlled until death due to systemic disease at 11 months. Two other patients received fractionated high dose salvage RT. One patient previously had multiple surgical procedures for a sacral chordoma. She presented to us with an 8.1 cm S1 lesion and was treated with 78 Gy/39fx. The patient subsequently developed a regional relapse at L3-L5 that was salvaged with SBRT 40 Gy/5fx. During follow-up, she developed distant metastases before failing locally at the salvage RT site after 35.8 months. One patient received 74.2 Gy/35fx to a 7.2 cm S2 lesion and failed locally at 11 months after salvage RT.
Two other patients received low-dose RT as salvage treatment. One patient with a L3 chordoma received 54 Gy/27fx and progressed locally 42 months after treatment. One patient with a L1 chordoma received 50 Gy/25fx and progressed locally 21 months after treatment.
Complications
Fifteen patients had data on surgical complications from the initial treatment. Of these, eleven patients (73%) had severe surgical complications that were classified as grade 3 in 3 patients, grade 4 in 6 patients and grade 5 in 2 (13%) patients. Grade 5 complications occurred during total en bloc sacrectomies; one was a massive blood loss due to iliac vein injury and the other a myocardial infarction.
Of the 23 patients that received RT, the most common late toxicity was spinal fracture, which developed in 4 (19%) patients [Grade 1 in 1 (78 Gy); grade 2 in 2 (78 Gy and 45 Gy + SRS 24 Gy); grade 3 in 1 (70 Gy)]. These patients had high sacral chordomas and developed S1 vertical fracture. Median time-to-fracture was 9.2 months (range 5.6 to 23.9 months).
Nine (60%) patients that received initial high dose RT developed other late treatment related complications, of which were Grade 1 in 4 (27%) and grade 2 in 5 (33%) patients. Two patients developed grade 2 skin induration; four patients developed grade 1 skin hyperpigmentation. One patient developed skin telangiectasia. One patient (surgery plus adjuvant RT for clivus chordoma) developed grade 1 glaucoma.
One patient with a previous traumatic (non-tumor related) paraparesis developed grade 2 fecal incontinence 3 months after receiving 78 Gy. No patient developed other late rectal toxicity. There were no grade 4 or 5 complications that could be attributed to RT.
Discussion
The present cohort comprises 10 years of a local paradigm shift, namely, the shift from radiotherapy in palliative scenarios toward high dose IG-IMRT as part of initial treatment. As in many parts of the world, Brazil has no particle therapy available for clinical use. Because of historical inefficiency of low dose photon radiotherapy in treating chordomas [11], surgeons were unenthusiastic about referring patients to radiotherapy even after piece-meal resection.
Our preliminary experience suggests that high dose photon radiotherapy significantly improves local control rates, reducing 5-year local failure from 83 to 48%. Our results are within the range of other high dose chordoma series [3, 4, 9, 10, 16,17,18,19,20]. Sahgal et al. [9] reported on a cohort of 24 base of skull chordoma patients treated with high dose photon IG-IMRT to a median dose of 76 Gy. With a median GTV volume of 14.5 cc, they achieved 5-year local control of 65%.
We report on a broader primary tumor location and included chordomas of the sacrum, mobile spine and base of skull. As expected, we had larger tumors, with median GTV in patients receiving initial RT of 149 cc or 8.1 cm. Other groups have reported tumor size as an adverse prognostic factor on local control [4, 20] or survival [1, 21]. In our study, patients with tumor > 330 cc were at increased risk for local failure (SHR 2.2; p = 0.028). Interestingly, Imai et al. [5] report on a series of 95 sacral chordomas treated with carbon ions to a median dose of 70.4 GyE in 16 fractions. With a median CTV of 370 cc, they report a 5-year local control of 88%. One can only speculate how much of this remarkable local control is a function of particle quality versus dose. We suggest this dose fractionation be further explored in studies of high-dose IG-IMRT in the treatment of sizeable sacral chordoma.
A relevant finding in our study is that patients that received initial surgery were more likely to experience regional failure (HR 5.2; p = 0.01). This could be explained by the fact that en bloc intent resection was performed in only 16% of surgical patients. Locally advanced disease at the time of diagnosis was common, limiting surgical options with reasonable morbidity. Rotondo et al., in a series of 126 spine chordomas treated with surgery and high dose combined photons and protons, report improved locoregional control in patients treated with en-bloc resection compared with intralesional resection (70% vs 53%) [22]. Interestingly, Chen et al. report on 24 spine chordomas from the same institution treated with definitive RT, achieving 5-year local progression-free survival of 80% [21]. When en bloc resection is not possible, limited spinal cord decompression followed by definitive RT could be an option. This approach is well established in the treatment of metastatic spinal cord tumors [23] and should be further evaluated in the management of chordomas.
During our follow-up, there were no grade 4 or 5 complications attributable to RT. The most common late toxicity was spinal insufficiency fracture, which developed in 4 (19%) patients with sacral chordoma. Median time-to-fracture was 9.4 months. Not minimizing the potential implications of these events, we consider them acceptable in light of the inherent morbidity of high sacrectomies. There were no late rectal toxicities, likely due to small PTV margins and avoidance of circumferential organ irradiation. Nevertheless, we heed attention to the fact that in recent years, as our experience matured both in terms of local control and failure, we have adopted a more aggressive approach favoring GTV coverage in lieu of OAR (except spinal cord and brainstem). This should render more complications in the future.
A small number of our patients (two) received salvage high dose RT. Although we did not perform a formal statistical comparison, these patients eventually relapsed locally during follow up. As others groups have demonstrated, local control and survival of RT given at initial treatment is superior to salvage therapy [4, 16, 19]. This suggests high-dose RT at relapse cannot compensate for suboptimal initial treatment and patients should be routinely considered for high dose RT (adjuvant or definitive) at the time of primary presentation [9].
We also highlight that our survival data needs to be interpreted carefully. Of the 3 deaths in the high RT dose group, 2 were not disease-related and one was a grade 5 complication following salvage en bloc sacrectomy. Although a difference in 5-year survival could not be demonstrated, due to the slow growth rate of most chordomas, we believe 10-year survival should ideally be used to compare different treatment strategies.
Our study has several limitations. First, it’s a retrospective cohort of patients with its inherent shortcomings. Secondly, the initial management of some cases was suboptimal. Due to the rarity of the disease, we chose not to exclude these patients, but to report real-world data. Thirdly, in an effort to harmonize with recently updated data on 24 Gy/1fx[13], we categorized it as high dose RT. Due to the small number of patients treated with SRS (2 initial, 2 salvage RT) and heterogeneous prognosis, our data can´t contribute to the debate of fractionated treatment versus SRS. At this time our standard approach is still fractionated high dose IG-IMRT.
The strength of our study is that it reports on a modest sized cohort treated with high dose photon RT at a reference center with experience in chordomas [2]. Our results are especially relevant to parts of the world without access to particle therapy.
In conclusion, our study suggests high-dose photon IG-IMRT improves local control in the initial management of chordomas. Health systems should promote reference centers with clinical expertise and technical capabilities of treating chordomas, thus improving outcomes for this complex disease.
Data availability
De-identified data will be available upon request on a case-by-case basis to researchers who provide a methodologically sound proposal. Requests should be made to the corresponding author and will then be evaluated by the participating study institutions.
References
Bakker SH, Jacobs WCH, Pondaag W et al (2018) Chordoma: a systematic review of the epidemiology and clinical prognostic factors predicting progression-free and overall survival. Eur Spine J 27:3043–3058. https://doi.org/10.1007/s00586-018-5764-0
Stacchiotti S, Sommer J (2015) Building a global consensus approach to chordoma: a position paper from the medical and patient community. Lancet Oncol 16:e71–e83. https://doi.org/10.1016/S1470-2045(14)71190-8
Munzenrider JE, Liebsch NJ (1999) Proton therapy for tumors of the skull base. Strahlenther Onkol 175(Suppl):57–63. https://doi.org/10.1007/BF03038890
Uhl M, Mattke M, Welzel T et al (2014) Highly effective treatment of skull base chordoma with carbon ion irradiation using a raster scan technique in 155 patients: first long-term results. Cancer 120:3410–3417. https://doi.org/10.1002/cncr.28877
Imai R, Kamada T, Sugahara S et al (2011) Carbon ion radiotherapy for sacral chordoma. Br J Radiol 84:48–53. https://doi.org/10.1259/bjr/13783281
Boriani S, Bandiera S, Biagini R et al (2006) Chordoma of the mobile spine: fifty years of experience. Spine (Phila Pa 1976) 31:493–503. https://doi.org/10.1097/01.brs.0000200038.30869.27
Particle therapy facilities in clinical operation. https://www.ptcog.ch/index.php/facilities-in-operation. Accessed 14 Apr 2021
(2020) The world bank population data. https://data.worldbank.org/indicator/SP.POP.TOTL. Accessed 15 Sept 2021
Sahgal A, Chan MW, Atenafu EG et al (2015) Image-guided, intensity-modulated radiation therapy (IG-IMRT) for skull base chordoma and chondrosarcoma: preliminary outcomes. Neuro Oncol 17:889–894. https://doi.org/10.1093/neuonc/nou347
Yamada Y, Laufer I, Cox BW et al (2013) Preliminary results of high-dose single-fraction radiotherapy for the management of chordomas of the spine and sacrum. Neurosurgery 73:673–680. https://doi.org/10.1227/NEU.0000000000000083
Catton C, O’Sullivan B, Bell R et al (1996) Chordoma: long-term follow-up after radical photon irradiation. Radiother Oncol 41:67–72. https://doi.org/10.1016/S0167-8140(96)91805-8
Ridenour RV, Ahrens WA, Folpe AL, Miller DV (2010) Clinical and histopathologic features of chordomas in children and young adults. Pediatr Dev Pathol 13:9–17. https://doi.org/10.2350/09-01-0584.1
Jin CJ, Berry-Candelario J, Reiner AS et al (2020) Long-term outcomes of high-dose single-fraction radiosurgery for chordomas of the spine and sacrum. J Neurosurg Spine 32:79–88. https://doi.org/10.3171/2019.7.SPINE19515
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509. https://doi.org/10.1080/01621459.1999.10474144
Katsoulakis E, Solomon SB, Maybody M et al (2013) Temporary organ displacement coupled with image-guided, intensity-modulated radiotherapy for paraspinal tumors. Radiat Oncol 8:150. https://doi.org/10.1186/1748-717X-8-150
Park L, DeLaney TF, Liebsch NJ et al (2006) Sacral chordomas: impact of high-dose proton/photon-beam radiation therapy combined with or without surgery for primary versus recurrent tumor. Int J Radiat Oncol Biol Phys 65:1514–1521. https://doi.org/10.1016/j.ijrobp.2006.02.059
DeLaney TF, Liebsch NJ, Pedlow FX et al (2009) Phase II study of high-dose photon/proton radiotherapy in the management of spine sarcomas. Int J Radiat Oncol Biol Phys 74:732–739. https://doi.org/10.1016/j.ijrobp.2008.08.058
Indelicato DJ, Rotondo RL, Begosh-Mayne D et al (2016) A Prospective outcomes study of proton therapy for chordomas and chondrosarcomas of the spine. Int J Radiat Oncol Biol Phys 95:297–303. https://doi.org/10.1016/j.ijrobp.2016.01.057
Holliday EB, Mitra HS, Somerson JS et al (2015) Postoperative proton therapy for chordomas and chondrosarcomas of the spine: adjuvant versus salvage radiation therapy. Spine (Phila Pa 1976) 40:544–549. https://doi.org/10.1097/BRS.0000000000000804
Snider JW, Schneider RA, Poelma-Tap D et al (2018) Long-term outcomes and prognostic factors after pencil-beam scanning proton radiation therapy for spinal chordomas: a large, single-institution cohort. Int J Radiat Oncol Biol Phys 101:226–233. https://doi.org/10.1016/j.ijrobp.2018.01.060
Chen YL, Liebsch N, Kobayashi W et al (2013) Definitive high-dose photon/proton radiotherapy for unresected mobile spine and sacral chordomas. Spine (Phila Pa 1976) 38:930–936. https://doi.org/10.1097/BRS.0b013e318296e7d7
Rotondo RL, Folkert W, Liebsch NJ et al (2015) High-dose proton-based radiation therapy in the management of spine chordomas: outcomes and clinicopathological prognostic factors. J Neurosurg Spine 23:788–797. https://doi.org/10.3171/2015.3.SPINE14716
Laufer I, Iorgulescu JB, Chapman T et al (2013) Local disease control for spinal metastases following “separation surgery” and adjuvant hypofractionated or high-dose single-fraction stereotactic radiosurgery: outcome analysis in 186 patients. J Neurosurg Spine 18:207–214. https://doi.org/10.3171/2012.11.SPINE12111
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Study conception: ATCC; WJGT. Data Collection: ATCC; CBCH; ARS; VR; LGCAL; BGMMC; WJGT. Statistical Analysis: ATCC. Initial Draft: ATCC. Interpretation of results and approval of final manuscript: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest.
Ethical approval
This study was approved by the Institutional Review Board, Local Ethics Committee and was conducted in accordance with the Ethical Principles of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, A.T.C., Hong, C.B.C., Narazaki, D.K. et al. High dose image-guided, intensity modulated radiation therapy (IG-IMRT) for chordomas of the sacrum, mobile spine and skull base: preliminary outcomes. J Neurooncol 158, 23–31 (2022). https://doi.org/10.1007/s11060-022-04003-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04003-w