Abstract
Introduction
Despite optimal surgical resection, meningiomas may recur, with increasing grade and the degree of resection being predictive of risk. We hypothesize that an increasing Ki67 correlates with a higher risk of recurrence of resected WHO grade I meningiomas.
Methods
The study population consisted of patients with resected WHO grade 1 meningiomas in locations outside of the base of skull. Digitally scanned slides stained for Ki67 were analyzed using automatic image analysis software in a standardized fashion.
Results
Recurrence was observed in 53 (17.7%) of cases with a median follow up time of 25.8 months. Ki67 ranged from 0 to 30%. Median Ki67 was 5.1% for patients with recurrence and 3.5% for patients without recurrence. In unadjusted analyses, high Ki-67 (≥ 5 vs. < 5) vs. ≥ 5) was associated with over a twofold increased risk of recurrence (13.1% vs. 27% respectively; HR 2.1731; 95% CI [1.2534, 3.764]; p = 0.006). After Adjusting for patient or tumor characteristics, elevated Ki-67 remained significantly correlated with recurrence. Grade 4 Simpson resection was noted in 71 (23.7%) of patients and it was associated with a significantly increased risk of recurrence (HR 2.56; 95% CI [1.41, 4.6364]; p = 0.002).
Conclusions
WHO grade 1 meningiomas exhibit a significant rate of recurrence following resection. While Ki-67 is not part of the WHO grading criteria of meningiomas, a value greater than 5% is an independent predictor for increased risk of local recurrence following surgical resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meningiomas are the most common primary intracranial neoplasm, accounting for 34% of all primary CNS tumors in the United States [1]. The majority, over 75%, of resected meningioma cases are classified as a WHO grade I meningioma. For patients with evidence of disease progression or with symptomatic lesions, surgical resection is the standard of care when the meningioma is located in an accessible location. The extent of resection is graded according to the Simpson grading system, which classifies meningioma resections into five grades; grades I–III are considered complete tumor removal with different degrees of dura resection/coagulation. However, a grade IV is a subtotal resection and grade V is a simple decompression [2]. Despite optimal surgical resection, meningiomas frequently recur. One factor associated with increased recurrence is the extent of resection, with significantly lower rates of recurrence in patients with complete resections [3,4,5]. Another factor strongly associated with recurrence is histologic grade, with increasing grade correlating with higher rates of recurrence [6]. Unlike with atypical (WHO grade II) and anaplastic (WHO grade III) meningiomas, where the indications for post-operative radiotherapy (RT) are less controversial, for patients with WHO grade I meningiomas, indications for the use of post-operative radiotherapy are not clearly defined. While considered a benign entity, they have a long natural history and recurrence rates are as high as 30% at 15 years following resection have been reported [5].
The Ki67 protein is a nuclear protein associated with ribosomal RNA transcription. It is a cellular marker of proliferation, and the Ki67 labeling index is widely used across several malignancies as a proxy of rapid growth and therefore aggressiveness of a tumor. In meningiomas, increasing Ki67 values have been correlated with tumor grade, with reported labeling indices ranges of 1–16% (average 3%) for grade I meningiomas, 2–20% (average 8%) for grade II meningiomas, and 7–32% (average 17%) for grade III meningiomas [7]. In addition, high Ki67 is correlated with higher rates of recurrence [8, 9]. However, the studies examining the relationship between Ki67 and recurrence frequently use visual estimation by the pathologist, which is more likely to have poor inter- and intra-observer concordance [10]. In our study, we aimed to demonstrate that an increasing Ki67 labeling index, as detected by a reliable, validated, and automated method [11, 12], correlates with a higher risk of recurrence in patients with resected WHO grade 1 meningiomas.
Methods and materials
Patient selection
This is a retrospective study performed with institutional IRB approval (IRB#13D.551). We identified 535 consecutive patients with WHO grade 1 meningiomas who underwent resection from 2005 to 2013 by querying the institutional tumor registry. The WHO grade I meningiomas analyzed in this study meet the criteria for classification and grading as meningioma, WHO grade I by the 2016 Classification of Tumors of the Central Nervous system [13]. The study sample consisted of 314 specimens that were located outside the base of skull. Meningiomas arising from the base of skull were excluded due to institutional preference to treat with radiation alone and these rarely underwent resection. An additional 15 patients were excluded due to unavailable tissue blocks or operative reports making 299 meningioma specimens were eligible for the final analysis. Initial patient and tumor characteristics as well as follow up data were obtained from medical records. Recurrence was defined as tumor growth on follow up MRI imaging of the brain using MacDonalds criteria [14]. The imaging frequency was as follows: 3 months after surgery of RT, then every 6 months for 2 years, then annually. As this was a retrospective study, patient consent was not required.Tissue analysis
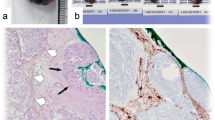
Deparaffinized tissue sections were stained with Ventana CONFIRM anti-Ki-67 (30-9) Rabbit Monoclonal Primary Antibody and hematoxylin counter stain utilizing the U ultraView DAB method on the VENTANA BenchMark ULTRA IHC/ISH Staining Module. Stained sections were then scanned at 20 × on the Aperio Scan Scope XT (Leica Biosystems Lab Solutions, Buffalo Grove, IL)). A representative area of meningioma was selected for quantification of Ki67 staining and was quantified with the Aperio IHC-nuclear detection algorithm to detect the number of positively stained nuclei and calculate the percentage of positively stained nuclei. The average area analyzed was 68 mm2 and the average number of nuclei analyzed per each case was 234,996. All slides (including those with a previously reported Ki67 value in the pathology report) were analyzed in such fashion at the time of the study by a neuropathologist to ensure consistency and reproducibility of Ki67 scoring.
Treatment delivery
Simpson grading of resection extent was determined by a single neurosurgeon (A.C.) based on operative reports and imaging performed within 48 h of surgery. RT was performed on a dedicated stereotactic linear accelerator with 6 MV photon energy. Those receiving RT were treated with stereotactic fractionated RT (FSRT) to a total dose of 5400 cGy for immediate postoperative RT (n = 13), or to a total salvage dose of 5400 cGy (n = 10), with 9 salvage patients receiving doses ranging from 4650 to 6000 cGy, all in 180 cGy-200 cGy daily fractions. A smaller patient group received a single fraction radiosurgery (SRS) of 1500 cGy (20 pts salvage SRS; 4 pts postoperative SRS) or 1800 cGy (3 salvage). Patients were immobilized with a customized rigid aquaplast mask and underwent daily image guidance (IGRT) with a commercial two-dimensional system (ExacTrac, BrainLab, Munich, Germany). Post-operative radiation therapy was defined as therapy directed at the resection bed and starting within 6 months from surgery. The need for post-operative RT was made on a case-by-case basis by the treating physician. Conversely, salvage RT was defined as starting more than 6 months after the initial resection.
Statistical analysis
Sample characteristics were summarized using frequencies and percentages. Ki67 was monotonically, but not linearly associated with increased risk of recurrence. To account for this and suggest a reasonable risk threshold from these data, Ki67 values were dichotomized as ≥ 5% vs. < 5% which corresponds to the median Ki67 among patients that experienced recurrence. Time to recurrence was calculated as time from surgery to first recurrence (defined as the date of the imaging study showing recurrence) and censored at date of last contact or death. Log-rank tests were used to test the association between explanatory factors and recurrence. Cox proportional hazards models were used to test the relationship between Ki67 level and risk of recurrence both univariably and while controlling for other study variables including gender, age, Simpson grade of resection extent, post-operative RT use and tumor location (as mixed site vs. single site). The significance level for all test was set at 0.05. Analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
Baseline patient, tumor and treatment characteristics
Records and specimens of 299 patients with meningiomas were analyzed. The median follow up time was 31.5 months (range 0–123.7 months). The baseline characteristics are shown in Table 1. Women constituted 69% of the analyzable sample. Mean patient age was 59.5 years (SD 13.9). The majority of patients had a Simpson grade I resection (46.2%). Median Ki-67 value was 3.5 (mean 4.9; range 0–30).
Only a fraction (n=64; 21.4%) of patients had RT at any time after surgery, and the majority received RT as salvage for recurrence rather than post-operatively (n= 46 [15.4%] vs. n=18 [6%]).
Factors affecting recurrence
Recurrence of the meningioma was observed in 53 (17.7%) of cases examined, occurring at the median time of 20.3 months. Median Ki67 was 5.1% for patients with recurrence and 3.5% for patients without recurrence. In unadjusted analyses, high Ki-67 (≥ 5 vs. < 5) was associated with over a 2-fold increased risk of recurrence (13.1% vs. 27.0% respectively; HR 2.31; 95% CI [1.34, 4.00]; p = 0.003) (Fig. 1 and Table 2).
Adjusting for patient demographics or tumor characteristics (including Simpson Grade) did not significantly impact the risk relationship between Ki-67 and recurrence. Grade 4 Simpson resection, which is a partial removal of tumor, was noted in 71 (23.7%) of patients and it was associated with a significantly increased risk of recurrence (HR 2.56 95% CI [1.41, 4.64]; p = 0.002) compared to patients with Simpson Grade 1-3 resection, which are all considered to achieve macroscopically complete removal of tumor (Table 2). However, there was no significant difference in the distribution of Ki-67 values between patients with Simpson resection Grades 1, 2, 3 or 4 (Fig. 2 and Table 3).
Impact of radiation
RT was given to 64 patients; in 18 patients, post-operatively based on physician judgment and in 46, as salvage after recurrence. Whereas post-operative RT appeared to reduce the risk of recurrence (HR 0.53 95% CI [0.16, 1.74]; p = 0.298), the number of patients who received immediate post-operative RT (n=18) was too small to show a statistically significant benefit.
Discussion
Despite the reported propensity of WHO grade I meningiomas to recur with increasing observation time after resection, there are no clear guidelines regarding the appropriate use of or timing of post-operative radiotherapy. While Ki-67 assessment is not part of the WHO grading criteria of meningiomas, in our study a value greater than 5% strongly correlated with an increased risk of local recurrence following surgical resection (HR 2.17), independent of the extent of resection, which also correlates with recurrence. We therefore propose Ki-67 scoring as a standard component of meningioma pathology reports, as measured by the digital pathology with quantitative image analysis of Ki-67 staining.
Previously published series have shown RT to be an effective primary treatment for benign meningiomas, with 10 year local control rates of 90% or higher [15, 16] and high rates of symptom improvement for those patients that present with symptomatic disease [12]. The completeness of resection has been customarily graded according to the Simpson Grade (1–4), with Grades 1–3 considered a “gross total” resection, and Grade 4 considered a “subtotal” resection [2, 17], depending on the complete removal of the tumor, dural attachments and involved bone. The recurrence rate after the subtotal resection is high and increases with observation period, with 5-year and 10-year rates of 37–62% and 52–100%, respectively [16]. Post-operative radiation therapy following a subtotal resection of benign meningiomas reduces the rates of subsequent recurrence. In the MDACC series of 92 patients with WHO grade I meningiomas, 5 year PFS was 91% for patients treated with post-operative RT, compared to 32% for patients treated with STR alone [18]. No Ki-67 information was available in this study.
The multi-institutional prospective trial, RTOG 0539, was a Phase II clinical study that aimed to tailor postoperative radiation therapy for patients with meningiomas based on their risk stratification, taking into account the extent of resection, histology and evidence of recurrence [19]. While this trial was an important attempt to add to the body of available data and to clarify guidelines for post-operative treatment of meningiomas, patients with newly diagnosed WHO grade I meningiomas were considered low risk, regardless of extent of resection, and therefore did not receive any radiation. Patients with low risk meningiomas (newly diagnosed WHO grade I meningiomas, regardless of extent of resection) had a 5 year progression-free survival (PFS) of 86.1% and a 5 year local failure (LF) rate of 12.5%, whereas intermediate risk patients (recurrent WHO grade I meningiomas or newly diagnosed WHO grade II meningiomas with gross total resection) had a 5 year PFS of 83.7% and a 5 year LF of 14.2%19. Therefore, the indications for postoperative RT for WHO grade I meningiomas (if any), continue to remain unclear.
Several previous studies have demonstrated that higher Ki-67 confers a higher rate of recurrence, but various scoring techniques with variable accuracies were employed [20,21,22]. To our knowledge, ours is the first study in meningioma, where Ki-67 was rigorously analyzed using an automated image analysis software that allows for reliable determination of Ki-67 values, minimizing the inter-observer variability [11, 12]. A similar analysis was recently reported in breast cancer [23], where the computer assisted image analysis allowed determination of a threshold Ki-67 value ≥ 14% predicting in a multivariate analysis an increased likelihood of recurrence and shorter overall survival in 440 patients.
In our study, a small subset of patients who received post-operative RT did indeed have lower rates of meningioma recurrence. Given the strong correlation of Ki-67 with subsequent recurrence, its role as a prognostic factor deserves further investigation in a prospective fashion. We propose a prospective, clinical trial that utilizes Ki-67 to risk-stratify patients with WHO grade I resected meningiomas, randomizing patients deemed high risk based on Ki-67 above 5 to immediate post-operative RT vs. active surveillance, and employing observation only for low risk patients. Such a trial would represent an important step in validating Ki-67 as a prognostic tool as well as further dissecting the role of post-operative radiation for high risk low grade meningiomas. An important question whether adjuvant radiation is as effective as salvage radiotherapy remains unanswered for Grade 1 meningiomas, although there is accumulating evidence that patients with atypical meningiomas have a higher second recurrence risk when receiving salvage vs. immediate postoperative radiation [24]. This topic is currently investigated in the NRG Oncology BN003 Phase III trial of observation versus irradiation for a gross totally resected Grade 2 meningioma [NCT03180268].
There are several important limitations of our retrospective study, which should be considered when interpreting the data for individual patients. Our patient population included both irradiated and non-irradiated patients in adjuvant and salvage settings. Our follow-up of a median of 2.5 years may not capture all late recurrences, although the primary endpoint for RTOG 0539 was PFS at 3 years [19].
While the decision regarding the use of post-operative RT remains a highly individualized decision based on several patient factors, our study indicates that Ki-67 may be an additional important factor to help tailor personalized treatment decisions. It is important to weigh the risks and benefits of close observation with serial MRI imaging and use of adjuvant radiotherapy with the patient to make treatment decisions. Recurrent meningiomas may be salvaged based on RTOG 0539 data but recurrent tumors may require further surgery, changing quality of life. These risks should be balanced by earlier initiation of radiation, which may lead to toxicity or (rarely) second cancers. Using molecular characteristics of tumor to better define subgroups of patients at high risk of recurrence may best help balance the competing risks between recurrence and radiation treatment. Our data provides additional information to aid shared decision making with the patient until future prospective trials can better define high-risk patients. Future studies may also further define sub groups at risk for recurrence analyzing p53, MIB-1 and angiogenic markers.
Conclusions
A proportion of low grade, WHO grade I meningiomas will exhibit a high rate of recurrence following resection. Finding personalized markers that may help to differentiate between low vs. high-risk WHO grade 1 meningiomas is important. While Ki-67 is not part of the WHO grading criteria of meningiomas, a value greater than 5% strongly correlates with an increased risk of local recurrence following surgical resection. Post-operative RT for patients with high Ki-67 levels should be further investigated in prospective studies.
References
Wiemels J, Wrensch M, Claus EB (2010) Epidemiology and etiology of meningioma. J Neurooncol 99(3):307–14
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 20(1):22–39
Otero-Rodriguez A, Tabernero MD, Monoz-Martin MC et al (2016) Re-evaluating Simpson grade I, II and III resections in neurosurgical treatment of World Health Organization Grade I meningiomas. World Neurosurg. 96:483–488
Nanda A, Bir SC, Maiti TK et al (2016) Relevance of Simpson grading system and recurrence-free survival after surgery for World Health Organization grade I meningioma. J Neurosurg 8:1–11
Winther TL, Torp SH (2016) The significance of the extent of resection in modern neurosurgical practice of WHO grade I meningiomas. World Neurosurg S1878–8750(16):31182–2
Riemenschneider MJ, Perry A, Reifenberger G (2006) Histological classification and molecular genetics of meningiomas. Lancet Neurol. 5(12):1045–54
Abry E, Thomassen IØ, Salvesen OØ et al (2010) The significance of Ki67/MIB-1 labeling index in human meningiomas: a literature study. Pathol Res Pract 206(12):810–5
Oya S, Kawai K, Nakatomi H et al (2012) Significance of Simpson grading system in modern meningioma surgery: integration of the grade with MIB-1 labeling index as a key to predict the recurrence of WHO grade I meningiomas. J Neurosurg 117(1):121–8
Vankalakunti M, Vasishta RK, Radotra BD et al (2007) MIB-1 immunolabeling: a valuable marker in prediction of benign recurring meningiomas. Neuropathology 27(5):407–12
Papathomas TG, Pucci E, Giordano TJ (2016) An international Ki67 reproducibility study in adrenal cortical carcinoma. Ann J Surg Pathol 40(4):569–76
Laurinavicius A, Plancoulaine B, Laurinaviciene A et al (2014) A methodology to ensure and improve accuracy of Ki67 labelling index estimation by automated digital image analysis in breast cancer tissue. Breast Cancer Res. 16(2):R35
Stalhammar G, Fuentes Martinez N, Lippert M et al (2016) Digital image analysis outperforms manual biomarker assessment in breast cancer. Mod Pathol 2:1–12
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131(6):808–20
Macdonald D, Cascino T, Schold SJ et al (1990) Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8(7):1277–1280
Combs SE, Adeberg S, Dittmar JO et al (2013) Skull base meningiomas: long term results and patient self-reported outcome in 507 patients treated with fractionated stereotactic radiotherapy (FSRT) or intensity modulated radiotherapy (IMRT). Radiother Oncol 106(2):186–91
Day SE, Halasz LM (2017) Radiation therapy for WHO grade I meningioma. Chinese Clin Oncol. 6(1):S4
Gallagher MJ, Jenkinson MD, Brodbelt AR et al (2016) WHO grade 1 meningioma recurrence: are location and Simpson grade still relevant? Clin Neurol Neurosurg 141:117–21
Soyuer S, Chang EL, Selek U et al (2004) Radiotherapy after surgery for benign cerebral meningioma. Radiother Oncol 71(1):85–90
Rogers L, Zhang P, Vogelbaum MA et al (2018) Intermediate-risk meningioma: initial outcomes from NRG Oncology RTOG 0539. J Neurosurg 129(1):35–47
Abry E, Thomassen IO, Salvesen OO et al (2016) (2010) The significance of Ki-67/MIB-1 labeling index in human meningiomas: a literature study. Pathol Res Pract 12:810–5
Pavelin S, Becic K, Forempoher G et al (2013) Expression of Ki-67 and p53 in meningiomas. Neoplasma 60(5):480–5
Roser F, Samii M, Ostertag H et al (2004) The Ki-67 proliferation antigen in meningiomas. Experience in 600 cases. Acta Neurochir (Wien) 146(1):37–44
Tay TKY, Thike AA, Pathmanathan N et al (2018) Using computer assisted image analysis to determine the optimal Ki67 threshold for predicting outcome of invasive breast cancer. Oncotarget 9(14):11619–11630
Pant S, Tonse R, Kannan S et al (2018) Impact of timing of radiotherapy on outcomes in atypical meningioma: a clinical audit. Pract Radiat Oncol S1879–8500(18):30049–3
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
Institutional IRB approval was obtained for the retrospective review of patient charts.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Kamila Nowak Choi and Joshua D. Palmer contributed equally to the published work.
Rights and permissions
About this article
Cite this article
Nowak-Choi, K., Palmer, J.D., Casey, J. et al. Resected WHO grade I meningioma and predictors of local control. J Neurooncol 152, 145–151 (2021). https://doi.org/10.1007/s11060-020-03688-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03688-1