Abstract
Purpose
Brain tumor-related epilepsy (TRE) is often resistant to currently available antiepileptic medications (AEDs). Clobazam was initially approved as adjunctive AED for patients with Lennox Gastaut syndrome but has been used in TRE, despite limited evidence in this context. This observational study aims to examine the effect of clobazam on seizure frequency on patients who have a primary CNS tumor and continued seizures despite their current AEDs.
Methods
A retrospective review of patients with histologically-confirmed primary brain tumors seen in the neuro-oncology interdisciplinary clinic from April 2016–2019 was completed, and patients on clobazam were identified. Response to clobazam was defined as a greater than 50% reduction in seizure frequency. Additional data including patient and tumor characteristics, treatment course, tolerability, AEDs used prior to addition of clobazam, and AEDs concomitantly used with clobazam were collected.
Results
A total of 35 patients with TRE on clobazam were identified, with 2 patients unable to tolerate the medication due to side effects. Of the 33 remaining patients, a total of 31 (93.9%) of patients were deemed responders. Ten patients (30.3%) were seizure free within 6 months of clobazam initiation and 21 (63.6%) reported a significant reduction in seizure frequency. This reduction also allowed several patients to modify concurrent AEDs.
Conclusions
Clobazam is an effective agent to use as add-on AED in TRE, with 94% of patients showing a significant response within 6 months. Furthermore, the addition of clobazam may yield a reduction in polypharmacy, as concomitant AEDs can be reduced and potentially withdrawn.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy is common in patients with brain tumors and has a major impact on quality of life for patients. About 30–50% of patients with primary brain tumors are diagnosed with seizures on initial presentation, and 10–30% of patients will develop seizures later in the disease course [1,2,3]. Seizures are more common among lower grade and slow-growing tumors, in particular in the presence of an IDH mutation [4]; whereas they are somewhat less frequently seen in higher grade tumors. Postoperative seizure freedom rates also vary depending on the type of tumor (70–90% with glioneuronal tumors, 65–80% with low grade gliomas) [2, 3]. Post-operative tumor-related epilepsy refractory to two or more medications is seen in 15–35% of low grade glioma cases and 15% in glioblastoma [3, 5].
Overall, of all tumor types, after standard neuro-oncological interventions (i.e., resection, chemotherapy), an estimated 12–50% do not respond to antiepileptic treatments which significantly impacts quality of life for patients with tumors [3]. Antiepileptics used in tumoral epilepsy are chosen carefully as these can interact with chemotherapy agents used for treatment of tumors; however, there is little information on the efficacy and tolerability of one AED over another in this population [6].
Clobazam is a unique antiepileptic medication that has not been formally studied in patients with tumor-related epilepsy. The drug falls under the class of benzodiazepines and works by potentiation of GABA-A receptors [7]. Clobazam has been marketed in Europe as an anxiolytic and add-on antiepileptic drug since the late 1970s. In the United States, it was only in 2011 that clobazam received FDA approval as an adjunct treatment in Lennox–Gastaut syndrome [8]. In practice, it is used as adjunct therapy in medically refractory focal epilepsy. Limited studies are available, although within these limitations, a reported 52–57% of patients with refractory epilepsy have been reported to achieve a >50% reduction in seizure frequency, and one study reported 19% of patients achieving seizure freedom over a 3-month course [8]. Clobazam is generally well tolerated with mild sedation, dizziness, and occasional ataxia as rare side effects [9]. Here we describe the first large series of patients with tumor-related epilepsy treated with clobazam as an add-on AED to conventional antiepileptic medications.
Methods
This is an observational study designed as a single-center retrospective review of brain tumor patients prescribed clobazam in a specialized interdisciplinary brain tumor outpatient clinic at Northwestern Memorial Hospital. Patients were identified based on analysis of electronic medical records seen between April of 2016 and April of 2019. Through the Northwestern University Enterprise Data Warehouse database (EDW), all patients with a diagnosis of a brain tumor (i.e., malignant neoplasm of the brain, benign neoplasm of brain and other parts of central nervous system) were identified (n = 1494). Patient records of those patients treated with clobazam and followed in the outpatient setting for a minimum of 6 months were reviewed (n = 39). Only those with primary glial tumors were included in the study leaving a total of 35 patients over the age of 18 years old taking clobazam in the context of a pathology-confirmed glial tumor.
Data including patient demographics, clinical notes, specific health information relating to seizures (e.g., seizure diaries), medical history, laboratory tests, antiepileptic medication and doses, concomitant medications, brain imaging reports, tumor pathology, and genetics were reviewed. Data was stored in the Northwestern University Tumor Related Epilepsy REDCap database (Grant Number UL1TR001422).
Data was collected from neuro-oncology clinic visits at 6, 12, 18-, and 24-month intervals. For patients who passed away or did not return to clinic prior to the follow-up visit, data was abstracted from the last neuro-oncology clinic note and the patient was grouped with the nearest appropriate interval.
Results
Patient characteristics and tumor characteristics
Between April 2016 and April 2019, a total of 35 patients on clobazam whom had previously undergone a biopsy and/or resection of their brain tumor were identified. Patient characteristics are displayed in Table 1. There was a predominance of males (74.2%) in this cohort. Median age was 43.5 years (range: 21.8–76.8 years old). All patients had a pathologically-confirmed primary brain tumor, the majority of whom harbored an IDH mutation. Histologic classification was determined using the histological classification of brain tumors approved by the World Health Organization [10].
All patients had gliomas, including grade II diffuse astrocytomas, grade II oligodendrogliomas, anaplastic astrocytomas, anaplastic oligodendrogliomas, and glioblastoma (GBM). GBM was the most common tumor type in this cohort with 42.9% of patients diagnosed with GBM. 20% had anaplastic astrocytomas, 20% with grade II oligodendroglioma, 11.4% with grade III anaplastic oligodendroglioma, and 5.7% with grade II astrocytomas. The majority of tumors were in the frontal lobe (45.7%) followed by temporal lobe with the remainder in other locations (Table 1).
The number of patients alive at each interval during follow up was 22, 16, 11, and 7 at 6-, 12-, 18-, and 24-months respectively. Mean duration of follow up after the initiation of clobazam was 16.0 months.
Tumor molecular genetics
Of the 31 patients with reported IDH status, 87.5% of low-grade gliomas had an IDH mutation. Similarly, 90% of patients with WHO grade III tumors harbored an IDH mutation. Among the 14 GBMs, 14.3% had an IDH mutation (Table 2).
Treatment at time of addition of clobazam
All of the patients underwent maximal safe tumor resection prior to starting clobazam. At the start of clobazam, the status of oncologic treatment was variable among patients. Some were undergoing initial treatment, some were undergoing treatment for tumor recurrence, and some had no ongoing oncologic treatment at initiation of clobazam Among those on initial tumor treatment, seven patients had completed the planned course of radiation therapy (RT) and were continuing chemotherapy with temozolomide (TMZ) at the time of starting clobazam. Eight patients had completed the planned course of RT and TMZ. Three patients were stable from an oncologic perspective, post TMZ or post RT, or were stable not having started RT or TMZ. Fourteen patients were being treated for tumor reoccurrence, undergoing repeat TMZ or on varying chemotherapy regimens (Table 3).
Efficacy of clobazam and seizure frequency
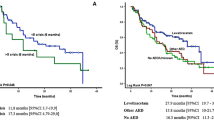
Seizure frequency was reported at the start of clobazam and then at subsequent neuro-oncology visits in intervals of 6, 12, 18, and 24 months. Categories of seizure frequency status were based on the 30–60 days prior to the last neuro-oncology clinic note, epilepsy clinic note, or inpatient note. The following categories were utilized: status epilepticus, one or more seizures daily, 2–6 seizures per week, 1–2 seizures per week, 2–3 seizures per month, 1 seizure per month, less than 1 seizure per month, and no seizures (Fig. 1). The majority of patients started on clobazam were seen by an epileptologist at some point during their clinical course (29/35).
Of 35 patients, 28 (80%) started clobazam due to refractory seizures, and seven (20%) started clobazam due to experiencing side effects of other AEDs. Two of thirty-five patients were unable to tolerate clobazam due to lethargy and increased somnolence. One of these two patients did report seizure freedom on clobazam.
Ten of thirty-three (30.3%) patients were seizure free within 6 months after addition of clobazam. Of the remaining 23 patients, 21 (63.6%) reported a greater than 50% reduction in seizure frequency (Fig. 1). Two patients continued to have at least 2 seizures per week despite the use of clobazam. In these two patients, progression of the tumor and other medical comorbidities, respectively could, in part, have contributed to their continued seizures. The mean effective daily dose of clobazam was 20.4 mg. The median daily effective dose was 20 ± 30 mg. The mean duration of follow up after addition of clobazam was 11.7 months. Median duration of follow up was 5.5 ± 59 months.
As seen in Fig. 1, at start of addition of clobazam, a majority (30.3%) of these patients reported 2–3 seizures/month, 18.2% reported having 1–2 seizures/week, 15.2% reported multiple seizures a day, 15.2% reported 2–6 seizures/week, 15.2% reported less than one seizure per month, and the rest were in status, alluding to the fact that these patients had refractory tumoral epilepsy (Fig. 1).
At 6-month follow up or earlier if the patients died, 14 patients reported less than one seizure/month, 10 patients reported seizure freedom, and 7 patients reported 2–3 seizures/month. One patient had 2–6 seizures/week, and one patient reported episodes of status epilepticus (Fig. 1).
At 12 months, 17 patients had died. However, of those alive and on clobazam (n = 16), at 12 months, six were seizure free, six reported seizure frequency of less than one per month, and three had 2–3 seizures/month. Only one patient reported seizures one to two times per week. At 18 months, 11 patients in this cohort were alive. Of these, four were seizure free, four reported seizure frequency of less than once per month, and three had 2–3 seizures/month. No patients reported daily or weekly seizures. At 2 year follow up, out of seven patients alive, four were seizure free, and three (n = 3) reported seizure frequency of less than one a month (Fig. 1). Thus, a significant reduction in seizure frequency in TRE was seen at these follow up intervals. The most common side effect reported in patients that discontinued clobazam was increased sedation; however, these side effects were seen in the immediate setting when clobazam was first started. In addition, sedation was reported in the setting of admission for status epileptics with concomitant antiepileptics used or in the setting of concurrent tumor progression with use of chemotherapy and RT.
Seizure response in relation to anti-tumor treatment and clobazam
At the start of clobazam, 21 patients were undergoing ongoing anti-tumor therapy including initial course of TMZ, repeat TMZ, lomustine (CCNU), procarbazine or investigational treatment within a clinical trial (Table 3). Fifteen of these patients had at least a 50% reduction in seizure frequency within 6 months, although were not completely seizure free. Of note, 5 patients became seizure free within 7 days after starting clobazam. For comparison, 12 patients were not on tumor-treatment at the time of start of clobazam. Of those, 6 patients had at least a 50% reduction in seizure frequency within 6 months. Five patients not on anti-tumor therapy were seizure free after starting clobazam, amounting to 91.7% of patient responders among those patients not receiving ongoing tumor treatment.
Clobazam and other antiepileptics
The most common concomitant antiepileptics used in this cohort of patients prior to addition of clobazam for refractory seizures in this cohort were levetiracetam (n = 20) and lacosamide (n = 16). A number of patients were able to wean concurrent antiepileptics after addition of clobazam given improved seizure frequency as seen per last available clinic note. Prior to addition of clobazam, 2 patients were on one antiepileptic (AED), 21 were on two AEDs, 8 were on three AEDs, 2 on four AEDs. After the addition of clobazam, the antiepileptic medications in addition to clobazam at the last neuro-oncologic clinic visit were documented. Of these, 11 patients were on one AED in addition to clobazam, 19 were on two AEDs in addition to clobazam, and 2 were on three AEDs in addition to clobazam.
Discussion
Management of brain tumor related epilepsy is complex and in the absence of prospective clinical trial highly individualized and dependent on the prescribing physicians experience and preference. Antiepileptic medications must be carefully chosen to avoid significant interactions with chemotherapy agents. In particular, older drugs like phenytoin, carbamazepine, and derivatives lead to strong induction of metabolic hepatic enzymes that subsequently increases metabolism and excretion of many chemotherapy agents. Antiepileptics must also have a good side effect profile for adequate tolerability given the myriad of side effects of chemotherapy, radiation therapy, and tumor resections [11]. There are no standard guidelines on the choice of agents used in TRE and which agent should be considered first-, second-, third- or fourth-line agents. Furthermore, given the refractory nature of TRE in the literature published with other antiepileptic agents, the investigation to identify more effective agents is warranted.
As clobazam is used and has been found to be effective in non-tumor refractory epilepsy, the epileptologist within the Northwestern Brain Tumor Institute (JT) had initially noted effectiveness in the patients with TRE refractory to other antiepileptic medications. Based on this observation, while not previously formally investigated until this study, the medication was increasingly used by neuro-oncologists and critical care neurologist in this population at our institution.
In our study, clobazam was shown to be an effective agent as an add-on therapy in this population with a total of 94% (31/33) of patients responding within 6 months, with either complete seizure freedom (10/31, 30.3%) or a > 50% reduction in seizure frequency (21/33, 63.6%). A total responder rate of 94% was noted in this study. This response was seen regardless of age, gender, or tumor characteristics. In addition, this response was also seen independent of the timing in their treatment course. The status of tumor, progression versus stability, was also variable in this cohort of patients (Tables 2 and 3).
Some studies have shown evidence for antiepileptics considered effective in TRE. However, there is no data on the efficacy of clobazam as an effective agent in TRE even though it is often used in these cohort of patients. This is the first retrospective cohort study studying the efficacy of clobazam in TRE [9].
Several agents considered safe to use in tumoral epilepsy include levetiracetam, lacosamide, lamotrigine, clonazepam, lorazepam, diazepam, clobazam, zonisamide, gabapentin, topiramate, and pregabalin. However, none of these medications have reported the same proportion of responder rates in this population. Lacosamide is considered an effective drug as add-on therapy in TRE and has shown a reduction in seizure frequency of >50% in 35.7% of patients and seizure freedom in 42.9% of patients as published by Maschio et al. [12, 13]. Topiramate has also been studied and shown seizure freedom in 55.6% of patients and greater than 50% reduction of seizure frequency in 20% of patients when used as a first line agent in TRE with a total responder rate of 75.6% [14]. Levetiracetam as monotherapy as well as an add-on agent in TRE has shown seizure freedom in 47.3% and greater than 50% reduction in seizure frequency in 26% of patients [15]. Novy et al. similarly published results of pregabalin as monotherapy and as an add-on showing seizure freedom in 66.7% of patients and > 50% reduction in frequency in 33.3% of patients; however, the total sample size was small, only 9 patients [16]. Zonisamide has been associated with a responder rate of 53.8% [17]. Clobazam as add-on therapy has shown to be effective in 43% of patients with epilepsy; however, it has not been studied in the context of TRE [7].
The mean effective daily dose of clobazam in this cohort of patients was 20.4 mg. Concomitant antiepileptics were used in these cohort of patients prior to addition of clobazam due to refractory nature of TRE. Often, clobazam replaced an AED and in some cases, the total number of AEDs could be reduced. Patients who were started on clobazam who were also on multiple antiepileptics prior to the start of clobazam were often able to reduce the burden of multiple antiepileptics to some extent in addition to having significant reduction in seizure frequency.
What could explain the responsiveness of patients with AED resistant TRE to clobazam? The pathogenesis of tumoral epilepsy is not well understood; however, several changes in the peritumoral tissue contribute to seizure activity like neurotransmitter changes, including upregulation of glutamate receptors and downregulation of GABA-A receptors, ion concentration, pH, and oxygen levels [1]. One potential benefit of clobazam is due to its prolonged effect on the GABA receptors, owing to its long elimination half-life, offering the added advantage of continuous suppression.
While there are no definitive molecular markers that have been inextricably linked to seizures in the context of gliomas, there is a clear relationship between the presence of IDH 1/2 (isocitrate dehydrogenase) mutations and seizures that is currently being investigated in this population [4, 18]. Both IDH1 and IDH2 mutations result in an accumulation of 2-hydroxyglutarate (2HG), which has a similar structure to glutamate, an excitatory neurotransmitter. This mutation is noted in 70–80% of patients with WHO grade II gliomas and secondary glioblastomas and is rare in primary glioblastomas (3–21%) [19, 20]. Beyond just the presence of the mutation, increased expression of the mutation has been present in patients with epilepsy compared to those without epilepsy in the context of tumors with an IDH1 mutation [19, 20].
TRE, when adequately managed, can have a significant effect on the quality of life of patients [1]. Medical management of brain tumors with aggressive chemotherapy, radiation, and surgery along with the psychologic stress of carrying a grave diagnosis often takes a significant toll on the quality of life of these patients. Tumoral epilepsy can not only add to this distress, but also significantly affects the quality of life of these patients. However, if adequately managed, tumoral epilepsy can significantly reduce the morbidity associated with BT and help improve the quality of life of these patients.
The small sample size and data from only one institution is a limitation of our study and does not allow data readily to be generalized. Furthermore, given the inherent challenges with studying patients with brain tumors, the heterogeneous nature of the disease and variable locations and treatments, response to an AED does not occur in isolation and other factors may have played a role in leading to improved seizure control. This is a retrospective study, patients were seen by different providers, and the seizure assessment and AED management was not standardized. Despite these limitations, clobazam appears to be an effective and well-tolerated medication in this population.
Conclusion
This study supports the use of clobazam in patients with TRE. In the cohort of patients studied, clobazam was effective at reduction of seizure frequency with a responder rate of 93.9%. Addition of clobazam not only allowed improved seizure frequency significantly, it also helped reduce the burden of multiple AED combinations used for seizure control in this population. It allowed to simplify treatment regimens in a patient population that often has to take numerous other medications as cancer treatment or for co-morbidities. Further studies should include a prospective study with the use of clobazam as a first-line agent as well as a comparative studies between clobazam and other AEDs as adjunct therapy in this population.
References
Erturk Cetin O, Isler C, Uzan M, Ozkara C (2017) Epilepsy-related brain tumors. Seizure 44:93–97. https://doi.org/10.1016/j.seizure.2016.12.012
Englot DJ, Chang EF, Vecht CJ (2016) Epilepsy and brain tumors. Handb Clin Neurol 134:267–285. https://doi.org/10.1016/B978-0-12-802997-8.00016-5
Van Breemen MSM, Wilms EB, Vecht CJ (2007) Epilepsy in patients with brain tumours: epidemiology, mechanisms, and management. Lancet Neurol 6(5):421–430. https://doi.org/10.1016/s1474-4422(07)70103-5
Chen H, Judkins J, Thomas C, Wu M, Khoury L, Benjamin CG, Pacione D, Golfinos JG, Kumthekar P, Ghamsari F, Chen L, Lein P, Chetkovich DM, Snuderl M, Horbinski C (2017) Mutant IDH1 and seizures in patients with glioma. Neurology 88(19):1805–1813
Kerkhof M, Vecht CJ (2013) Seizure characteristics and prognostic factors of gliomas. Epilepsia 54(Suppl 9):12–17. https://doi.org/10.1111/epi.12437
de Groot M, Reijneveld JC, Aronica E, Heimans JJ (2012) Epilepsy in patients with a brain tumour: focal epilepsy requires focused treatment. Brain 135(Pt 4):1002–1016. https://doi.org/10.1093/brain/awr310
Vecht C, Royer-Perron L, Houillier C, Huberfeld G (2017) Seizures and anticonvulsants in brain tumours: frequency, mechanisms and anti-epileptic management. Curr Pharm Des 23(42):6464–6487
Gauthier AC, Mattson RH (2015) Clobazam: a safe, efficacious, and newly rediscovered therapeutic for epilepsy. CNS Neurosci Ther 21(7):543–548
Bresnahan R, Martin-McGill KJ, Williamson J, Michael BD, Marson AG (2019) Clobazam add-on therapy for drug-resistant epilepsy. Cochrane Database Syst Rev 10:CD004154. https://doi.org/10.1002/14651858.CD004154.pub5
Gupta A, Dwivedi T (2017) A simplified overview of World Health Organization classification update of central nervous system tumors 2016. J Neurosci Rural Pract 8(4):629–641. https://doi.org/10.4103/jnrp.jnrp_168_17
Maschio M, Dinapoli L, Vidiri A et al (2009) The role side effects play in the choice of antiepileptic therapy in brain tumor- related epilepsy: a comparative study on traditional antiepileptic drugs versus oxcarbazepine. J Exp Clin Cancer Res 28:60
Maschio M, Dinapoli L, Mingoia M et al (2011) Lacosamide as add-on in brain tumor-related epilepsy: preliminary report on efficacy and tolerability. J Neurol 258(11):2100–2104
Newton HB, Connelly J, Lima J, Cunningham H, Pearl D, Malkin M (2010) Lacosamide in brain tumour patients with refractory seizures: efficacy and tolerability. J Neurol 25(Suppl 1):S1–S246 P476
Maschio M, Dinapoli L, Zarabla A et al (2008) Outcome and tolerability of topiramate in brain tumor associated epilepsy. J Neuro-Oncol 86:61–70
Maschio M, Albani F, Baruzzi A et al (2006) Levetiracetam therapy in patients with brain tumour and epilepsy. J Neuro-Oncol 80:97–100
Novy J, Stupp R, Rossetti AO (2009) Pregabalin in patients with primary brain tumors and seizures: a preliminary observation. Clin Neurol Neurosurg 111:171–173
Maschio M, Dinapoli L, Saveriano F et al (2009) Efficacy and tolerability of zonisamide as add-on in brain tumor-related epilepsy: preliminary report. Acta Neurol Scand 120:210–212
Yang Y, Mao Q, Wang X, Liu Y, Mao Y, Zhou Q, Luo J (2016) An analysis of 170 glioma patients and systematic review to investigate the association between IDH-1 mutations and preoperative glioma-related epilepsy. J Clin Neurosci 31:56–62. https://doi.org/10.1016/j.jocn.2015.11.030
Liubinas SV, D’Abaco GM, Moffat BM, Gonzales M, Feleppa F, Nowell CJ et al (2014) IDH1 mutation is associated with seizures and protoplasmic subtype in patients with low-grade gliomas. Epilepsia 55(9):1438–1443. https://doi.org/10.1111/epi.12662
Liubinas SV, O’Brien TJ, Moffat BM, Drummond KJ, Morokoff AP, Kaye AH (2014) Tumour associated epilepsy and glutamate excitotoxicity in patients with gliomas. J Clin Neurosci 21(6):899–908. https://doi.org/10.1016/j.jocn.2014.02.012
Acknowledgements
REDCap is supported at FSM by the Northwestern University Clinical and Translational Science (NUCATS) Institute, Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number UL1TR001422. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brahmbhatt, N., Stupp, R., Bushara, O. et al. Efficacy of clobazam as add-on therapy in brain tumor-related epilepsy. J Neurooncol 151, 287–293 (2021). https://doi.org/10.1007/s11060-020-03664-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03664-9