Abstract
Purpose
Several studies describe sleep–wake disturbances in pediatric craniopharyngioma, but none have determined the prevalence or associated predictors of excessive sleepiness in this group after diagnosis and prior to post-operative observation or adjuvant radiotherapy. In this study, we report sleep–wake disturbances in children and adolescents with craniopharyngioma and associated clinical and treatment variables.
Methods
After surgery and prior to radiotherapy or observation, pediatric patients (n = 110) with craniopharyngioma ≥ 3 years old completed a baseline sleep clinic evaluation by a pediatric sleep specialist, polysomnography (PSG) and next-day multiple sleep latency test (MSLT). MSLT was limited to those ≥ 6 years old. Logistic regression models were used to determine the relationship between patient characteristics and the presence and type of hypersomnia.
Results
Amongst patients completing PSG and MSLT, 80% had polygraphic evidence of excessive daytime sleepiness. Hypersomnia due to medical condition was diagnosed in 45% and narcolepsy in 35%. Overweight or obese patients were more likely to be diagnosed with hypersomnia (P = 0.012) or narcolepsy (P = 0.009). Grade 2 hypothalamic involvement (HI) at diagnosis was associated with the diagnosis of narcolepsy (P = 0.0008).
Conclusions
This study describes the prevalence and associated predictors of hypersomnia for patients with craniopharyngioma after surgical resection. HI was predictive of narcolepsy diagnosis, and a higher body mass index z-score was associated with hypersomnia due to medical condition and narcolepsy. We recommend that sleep assessment and intervention begin after surgical resection, especially in overweight or obese patients and those with extensive tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Craniopharyngioma is a low-grade intracranial tumor of the sellar/parasellar region of the brain [1]. The invaded region of the brain may include the hypothalamus, pituitary gland, and optic nerves. Although rare, 30–50% of craniopharyngiomas are diagnosed in children and adolescents [1, 2]. The primary goal of treatment is to preserve function and reduce treatment-related complications. Patients treated with surgery alone or limited surgery and radiotherapy have comparable 5- and 10-year progression-free survivals; however, visual field disruption, endocrine deficiencies, hypothalamic obesity, sleep–wake disturbance, and neurocognitive impairment remain common regardless of treatment [3, 4]. These impairments secondary to the location and treatment of craniopharyngioma negatively impact the health-related quality of life (HRQoL) of children and adolescents.
Sleep–wake disturbances are common in patients with craniopharyngioma due to location of the tumor. One mechanism is dysfunction of the hypothalamic circadian pacemaker within the suprachiasmatic nucleus, which regulates melatonin secretion and timing of sleep propensity [5]. Damage to the hypothalamus can also induce central disorders of hypersomnolence [6,7,8,9], which collectively represent both narcolepsy and hypersomnia due to a medical disorder when using the International Classification of Sleep Disorders, 3rd edition [ICSD-3]. The general term, hypersomnia, is defined as “daily periods of irrepressible need to sleep or daytime lapses into sleep” (International Classification of Sleep Disorders [ICSD-3]). Narcolepsy is characterized by hypersomnia and the presence of ≥ 2 periods of sleep-onset rapid eye movement (REM) periods during the multiple sleep latency test (MSLT) with cataplexy (narcolepsy type 1), or without cataplexy (narcolepsy type 2) [ICSD-3]. Hypersomnia due to a medical disorder is defined by the ICSD-3 as chronic hypersomnia which occurs due to an underlying medical or neurological disorder, with fewer than two sleep-onset REM periods on the MSLT [ICSD-3]. In both disorders, the hypersomnia and MSLT findings are not better explained by other causes such as insufficient sleep, obstructive sleep apnea, a circadian rhythm sleep/wake disorder, or the effects of medications or substances, or their withdrawal [ICSD-3].
Hypersomnia, whether due to narcolepsy or hypersomnia due to a medical disorder, can negatively impact neurocognitive functioning and school performance in pediatric patients with craniopharyngioma [2, 6, 10], indicating the need for early assessment and intervention to improve long-term outcomes in these patients. Despite the high prevalence of central disorders of hypersomnolence in children and adolescents with craniopharyngioma, sleep–wake disturbances and long-term outcomes in survivors have been reported only in case studies and small cohorts, with variability in the timing of sleep diagnosis after tumor diagnosis. Our earlier study found a mean time of 6.9 years from tumor diagnosis to sleep referral, indicating a need for earlier sleep intervention [8]. Research to date has not characterized the prevalence of sleep disturbances after surgical resection and prior to radiotherapy or observation or the associated predictors of hypersomnia. Therefore, the aim of this study is to describe and characterize hypersomnia in this patient population and the associated patient-, disease-, and treatment variables. Investigating these variables may help identify patients at greatest risk for sleep-related disorders early in treatment.
Materials and methods
Participants
From August 2011 to May 2016, polysomnography (PSG) and next-day MSLT were performed in children and adolescents (n = 110) diagnosed with craniopharyngioma based on neuroimaging, intraoperative findings (cyst fluid) or histopathology. For the latter, all cases were confirmed adamantinomatous craniopharyngioma. All patients were seen and evaluated by a pediatric sleep medicine specialist in a sleep clinic. The PSG and MSLT was obtained prior to radiotherapy or observation after treatment with surgery alone. PSG was completed for those age ≥ 3 years and PSG and MSLT for those age ≥ 6 years.
Study design
This single institution cross-sectional study enrolled all eligible patients after surgical resection and prior to radiation therapy. This study was approved by the institutional review board. Consent was obtained from all patients aged 18 years and older or parents of patients less than 18 years. Assent was obtained from children according to institutional guidelines. Demographic and clinical characteristics and questionnaires were collected at the time of testing. Patient self-reported and parent-proxy reported HRQoL and fatigue questionnaires were collected.
Clinical variables were defined by the study team for consistency in reporting. The extent of preoperative hypothalamic involvement (HI) in neuroimaging was categorized as grade 0 (no HI), grade 1 (anterior HI), or grade 2 (anterior and posterior HI, including the mammillary bodies) [1, 2]. Surgery was categorized as no surgery, resection, or catheter placement. Cerebrospinal fluid diversion was categorized as ventriculoperitoneal shunt or endoscopic third ventriculostomy. Diabetes insipidus was categorized as present or not, based on prescribed desmopressin. Visual field status was categorized as intact bilaterally or having unilateral or bilateral field defect. Visual acuity was classified as having unilateral or bilateral reduced vision, with no functional impairments.
Measures
Polysomnography
Comprehensive, attended nocturnal PSG was performed at an American Academy of Sleep Medicine (AASM) accredited sleep center. PSG was initiated within 1 h of the patient's usual bedtime. The following physiologic parameters were recorded during PSG: electroencephalograms (at least four channels); electro‐oculogram (two channels); submental electromyogram (one channel); electrocardiogram; respiratory effort measured at the chest and abdomen; air flow measured using oronasal thermisters and nasal pressure transducers; continuous oximetry; positional sensors; electromyogram or accelerometry of the anterior tibialis to assess limb movements; audio recordings to detect snoring and other obstructive sounds; and videotape recordings to document movements and behaviors during sleep.
Sleep–wake scoring was performed by using standardized techniques and AASM scoring criteria [11]. Obstructive apneas were scored when air‐flow registration decreased by 90% to 100% with continued respiratory effort, with at least two respiratory cycles for patients younger than 18 years and at least 10 s for patients 18 years of age and older. Hypopneas were scored when air‐flow registration was decreased by at least 30% from baseline, either in association with a 3% drop in oxygen saturation values or in association with an arousal. Duration criteria used were the same as those to diagnose obstructive apnea. Arousals were scored by using the AASM scoring criteria.
Multiple sleep latency test
The MSLT is an objective, in‐laboratory assessment of a patient's tendency to fall asleep under standardized conditions and was performed after nocturnal PSG in subjects 6 years and older. The MSLT was performed according to AASM guidelines [12]. Patients were given four or five nap opportunities at 2‐h intervals throughout the day and were observed and not allowed to sleep between nap opportunities. If sleep onset occurred during a nap trial, patients were allowed to sleep for 15 minutes (min) and then awakened by the technologist. If no sleep occurred after 20 min, the nap opportunity ended, and sleep latency was recorded as 20 min. The mean sleep latency (MSL) was calculated as the arithmetic mean of all nap opportunities. The number of naps and the corresponding sleep stages were recorded. Criteria for identification of hypersomnia on the MSLT were according to Tanner staging (prepubescent versus pubescent) and defined as an MSL of ≤ 15 min in prepubescent children with Tanner stage 1 and of ≤ 10 min in pubescent youth with Tanner stage 2 or greaterFootnote 1 [13]. Tanner staging was documented by study endocrinologist. Criteria for narcolepsy included an MSL of ≤ 15 min in prepubescent children with Tanner stage 1 and of ≤ 10 min in pubescent youth with Tanner stage 2 or higher,Footnote 2 and presence of two or more sleep‐onset REM periods. Subjects who showed evidence of hypersomnia and fewer than two sleep-onset REM periods were considered to have hypersomnia due to a medical condition.
Health-related quality of life and sleep assessment
HRQoL was assessed in children and adolescents by using the Pediatric Quality of Life Inventory (PedsQL V.4), a 23-item Likert-type scale measuring physical, emotional, social, and school functions. The instrument has parallel forms for the patient and parent reports. The instrument for both patients and parents is internally consistent (Cronbach alpha coefficients of 0.91 and 0.92, respectively) and clinically valid [14]. The instrument’s scores are transformed to a 0–100-point scale, with higher scores reflecting a higher HRQoL. The Pediatric Quality of Life Inventory brain tumor module is a 24-item Likert-type scale assessing HRQoL in children and adolescents receiving treatment or are survivors of pediatric brain tumors. The module contains six scales and addresses cognitive function, pain and hurt, movement and balance, procedural anxiety, nausea, and worry. The instrument is scored by the PedsQL V.4, with higher scores reflecting a higher HRQoL. The PedsQL brain tumor module was completed by the parent proxy and by children and adolescents aged ≥ 5 years. The brain tumor module is internally consistent [15]. The Peds QL multidimensional fatigue scale evaluates physical, cognitive, and sleep-related fatigue. The scale was completed by the parent proxy and by children and adolescents aged ≥ 5 years. The 18-item Likert-type scale is internally consistent and clinically valid in children with cancer and chronic illness, with higher scores representing decreased symptoms of fatigue [14].
Data analyses
Baseline patient demographic, clinical, sleep, and HRQoL-related characteristics were summarized using descriptive statistics. Logistic regression (using exact methods) or the Fisher’s exact test was used to determine whether patient demographic, clinical, sleep, and QoL related characteristics were associated with a diagnosis of a sleep/wake disturbance (obstructive sleep apnea [OSA], hypersomnia, or narcolepsy) at baseline. The odds ratios for associations between sleep and patient/disease characteristics were calculated with and without the adjustment for the potential confounding characteristic of preoperative hypothalamic involvement. Statistical analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC). A two-sided significance level of P < 0.05 was used for all statistical tests.
Results
Of 110 patients in the study, 98 (89%) completed a baseline PSG and 86 (88%) completed both the PSG and next-day MSLT. Table 1 describes baseline demographics (age, tanner stage, gender, race and BMI) and disease characteristics (preoperative HI, number of surgeries and surgical extent, CSF diversion, diabetes insipidus and visual fields) of patients who completed a PSG and those who completed a PSG and next-day MSLT. Table 2 gives the mean or median PSG and MSLT sleep characteristics and the mean patient self-reported and parent-proxy HRQoL.
Of the 98 patients completing a baseline PSG, five met the criteria for borderline to mild OSA (apnea–hypopnea index ≥ 2). Of patients completing the PSG and MSLT, 39 (45%) were diagnosed with hypersomnia due to medical disorder and 30 (35%) with narcolepsy. The remaining 17 patients (20%) did not have objectively documented hypersomnia.
We then explored baseline demographic and disease characteristics collected form patients with craniopharyngioma.
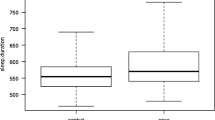
We found that the adjusted and unadjusted odds ratios of sleeping diagnosis with patient and disease characteristics lead to identical conclusions of significance, regardless of the inclusion or exclusion of the adjustment for preoperative hypothalamic involvement. Table 3 gives the unadjusted results of the logistic regression models exploring the relationship between patient demographic, disease characteristics and hypersomnia at baseline and compared to patients without sleep or wake disturbance. Between the two groups, there were no differences in age, tanner stage, gender or race. Nor were there differences in extent of surgery and number of surgeries, CSF diversion, diabetes insipidus, visual fields or acuity, HRQoL or fatigue. The association between categorized body mass index (BMI) z-score and hypersomnia due to a medical condition at baseline could not be computed reliably within the logistic regression model. Therefore, the Fisher’s exact test was used to test this association. The baseline categorized BMI z-score was significantly associated with hypersomnia due to a medical condition at baseline; a greater proportion of overweight or obese patients were diagnosed with hypersomnia due to a medical condition at baseline than were patients who were not overweight or obese (100% vs. 63%, P = 0.012).
Table 4 shows the unadjusted results of logistic regression models exploring the association between patient demographic, disease characteristics and narcolepsy at baseline and compared to patients without sleep or wake disturbance. Between the two groups, there were no differences in age, tanner stage, gender or race. Nor were there differences in extent of surgery and number of surgeries, CSF diversion, diabetes insipidus, visual fields or acuity, HRQoL or fatigue. The association between categorized BMI z-score and a diagnosis of narcolepsy at baseline could not be computed reliably within the logistic regression model. Therefore, the Fisher’s exact test was used to test this association. Baseline categorized BMI z-score was significantly associated with a diagnosis of narcolepsy at baseline; a greater proportion of overweight or obese patients were diagnosed with narcolepsy than were patients who were not overweight or obese (100% vs. 56%, P = 0.009). Patients with grade 2 HI at diagnosis had higher odds of being diagnosed with narcolepsy at baseline than were patients with grade 0–1 preoperative HI [OR (95% CI): 6.3 (1.5–30.99), P = 0.008].
Discussion
This study describes the prevalence of excessive daytime sleepiness after surgical resection and before radiotherapy in a cohort of pediatric patients with newly diagnosed craniopharyngioma, as well as the associated predictors of excessive daytime sleepiness. Children with craniopharyngioma are known to have sleep–wake regulatory disturbances, suffer from obesity and associated obstructive sleep apnea, and have an increased occurrence of secondary hypersomnia [9]. Sleep–wake disturbances such as these may result in decreased psychosocial and academic QoL [6, 10]. We examined associated patient-, disease-, and treatment variables to determine whether they might predict patients at greatest risk of hypersomnia early in treatment, thereby increasing opportunities for early assessment and intervention and improving their HRQoL. Surprisingly self-reported HRQoL, symptoms and fatigue were not associated with sleepiness. While mean scores indicated poorer HRQoL and higher reported fatigue among those with hypersomnia/narcolepsy, there was no significant difference between those with sleepiness and those with no sleep–wake disturbance. This may reflect acclimation to excessive sleepiness prior to craniopharyngioma diagnosis.
Almost 50% of patients with craniopharyngioma met criteria for hypersomnia due to a medical disorder and 35% for narcolepsy, highlighting that 80% of the sample experienced excessive daytime sleepiness after diagnosis and prior to radiotherapy or observation after surgery alone. Although our study is the first to describe the prevalence of sleepiness after surgery, findings are consistent with previous studies indicating that children and adolescents with craniopharyngioma experience fatigue and sleep–wake disruption, which persists in 65–80% of patients after treatment [6, 7, 9]. Although narcolepsy and hypersomnia due to a medical condition are highly prevalent in this population, many patients have a delay in sleep referral [8], indicating a need to establish guidelines for earlier sleep intervention.
While all patients with craniopharyngioma are at risk for disorders of hypersomnolence, patients who are overweight or obese at presentation are at greatest risk. Our study found that a higher BMI z-score was predictive of both hypersomnia due to a medical condition and narcolepsy diagnosis at baseline, with findings consistent with prior research indicating that hypersomnia severity is higher in obese craniopharyngioma patients [16]. Secondary narcolepsy is also a contributing factor to weight control in already obese craniopharyngioma patients [9], with narcolepsy onset associated with abrupt weight gain [17].
In addition to patients who are overweight and obese, newly diagnosed patients with imaging showing grade 2 HI before surgery should be screened for disorders of hypersomnolence, more specifically narcolepsy. This finding is consistent with studies describing higher grade of hypothalamic tumor involvement and clinically significant daytime sleepiness and narcolepsy [6,7,8, 18]. Additionally, research shows that higher grade HI predicts worse performance on measures of attention, processing speed, memory, executive function, and adaptive skills [2, 19]. More recently, Fournier-Goodnight et al. [4] evaluated neurocognitive function in pediatric craniopharyngioma patients after surgery and prior to radiotherapy. Poorer performance was predicted by higher-grade presurgical HI, and patients showed weaker neurocognitive performance than did the normative group.
Limitations of our study include the use of cross-sectional data and small sample size across sleep diagnosis. We plan to perform follow-up studies to examine the trajectory of hypersomnia and other sleep–wake disturbances in this population over multiple timepoints. Additionally, Subjective measurements may not be sensitive in identifying patients at risk for sleepiness. We have reported that the modified Epworth Sleepiness Scale (M-ESS) was not a valid measure in the pediatric craniopharyngioma patient population. Our sample demonstrated poor sensitivity, missing 35% of those with significant objective sleepiness even when the cut score for detection of significant sleepiness was reduced from the established cut score of 10 to 6 [20]. Therefore, subjective sleep measured by the M-ESS was removed as a potential predictor in this study. Finally, the validity of mean sleep latency measurements on the MSLT can be influenced by a variety of factors and care must be taken in the interpretation of results. For example, children who are anxious in the sleep laboratory environment or in pain are more likely to be “hyperalert” and thus, findings might not be representative of the child’s usual degree of sleepiness.
Conclusions
Sleep disorders are commonly described among patients with craniopharyngioma. This study demonstrates the early onset of significant sleepiness due to a medical disorder after surgical resection and prior to adjuvant radiotherapy or observation. Therefore, clinicians should consider early diagnosis and intervention for hypersomnolence based on predictors of obesity and hypothalamic grade, as well as clinical history. Interventions should include education on hypersomnia/narcolepsy, good sleep hygiene practices, and consideration of wake-promoting medications as early as possible in the child’s course. The patient and parent should be given suggestions for managing sleepiness during the school day, with instructions for the child’s educators and recommended academic accommodations potentially improving social interaction, academic performance, and HRQoL.
Notes
The MSLT is considered the “gold standard” for objective characterization of daytime sleepiness, but normative data from typically developing children and uniformly accepted cut-off values for pathological sleepiness in children are lacking. We chose a cut-off value for mean sleep latency of < 15 min in prepubescent children and < 10 min in pubescent youth. This is a deviation from the ICSD-3 recommendation (cut-off value of < 8 min), which refers to adults.
Refer Footnote 1.
References
Muller HL, Gebhardt U, Teske C, Faldum A, Zwiener I, Warmuth-Metz M, Pietsch T, Pohl F, Sorensen N, Calaminus G, Study Committee of K (2011) Post-operative hypothalamic lesions and obesity in childhood craniopharyngioma: results of the multinational prospective trial KRANIOPHARYNGEOM 2000 after 3-year follow-up. Eur J Endocrinol 165(1):17–24. https://doi.org/10.1530/EJE-11-0158
Ozyurt J, Thiel CM, Lorenzen A, Gebhardt U, Calaminus G, Warmuth-Metz M, Muller HL (2014) Neuropsychological outcome in patients with childhood craniopharyngioma and hypothalamic involvement. J Pediatr 164(4):876–881. https://doi.org/10.1016/j.jpeds.2013.12.010
Muller HL (2016) Preoperative staging in childhood craniopharyngioma: standardization as a first step towards improved outcome. Endocrine 51(1):1–3. https://doi.org/10.1007/s12020-015-0800-x
Fournier-Goodnight AS, Ashford JM, Merchant TE, Boop FA, Indelicato DJ, Wang L, Zhang H, Conklin HM (2017) Neurocognitive functioning in pediatric craniopharyngioma: performance before treatment with proton therapy. J Neurooncol 134(1):97–105. https://doi.org/10.1007/s11060-017-2492-y
Brzezinski A (1997) Melatonin in humans. N Engl J Med 336(3):186–195. https://doi.org/10.1056/NEJM199701163360306
Jacola LM, Conklin HM, Scoggins MA et al (2016) Investigating the role of hypothalamic tumor involvement in sleep and cognitive outcomes among children treated for craniopharyngioma. J Pediatr Psychol 41:610
Khan RB, Merchant TE, Sadighi ZS, Bello MS, Lu Z, Sykes A, Wise MS, Crabtree VM, Zabrowski J, Simmons A, Clark ME, Mandrell BN (2018) Prevalence, risk factors, and response to treatment for hypersomnia of central origin in survivors of childhood brain tumors. J Neurooncol 136(2):379–384. https://doi.org/10.1007/s11060-017-2662-y
Mandrell BN, Wise M, Schoumacher RA, Pritchard M, West N, Ness KK, Crabtree VM, Merchant TE, Morris B (2012) Excessive daytime sleepiness and sleep-disordered breathing disturbances in survivors of childhood central nervous system tumors. Pediatr Blood Cancer 58(5):746–751. https://doi.org/10.1002/pbc.23311
Muller HL (2010) Increased daytime sleepiness in patients with childhood craniopharyngioma and hypothalamic tumor involvement: review of the literature and perspectives. Int J Endocrinol 2010:519607. https://doi.org/10.1155/2010/519607
Cohen M, Guger S, Hamilton J (2011) Long term sequelae of pediatric craniopharyngioma—literature review and 20 years of experience. Front Endocrinol (Lausanne) 2:81. https://doi.org/10.3389/fendo.2011.00081
Berry RB, Gamaldo CE, Harding SM, Brooks R, Lloyd RM, Vaughn BV, Marcus CL (2015) AASM scoring manual version 2.2 updates: new chapters for scoring infant sleep staging and home sleep apnea testing. J Clin Sleep Med 11(11):1253–1254. https://doi.org/10.5664/jcsm.5176
Littner MR, Kushida C, Wise M, Davila DG, Morgenthaler T, Lee-Chiong T, Hirshkowitz M, Daniel LL, Bailey D, Berry RB, Kapen S, Kramer M, Standards of Practice Committee of the American Academy of Sleep M (2005) Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep 28(1):113–121. https://doi.org/10.1093/sleep/28.1.113
Gozal D, Wang M, Pope DW Jr (2001) Objective sleepiness measures in pediatric obstructive sleep apnea. Pediatrics 108(3):693–697. https://doi.org/10.1542/peds.108.3.693
Varni JW, Burwinkle TM, Katz ER, Meeske K, Dickinson P (2002) The PedsQL in pediatric cancer: reliability and validity of the pediatric quality of life inventory generic core scales, multidimensional fatigue scale, and cancer module. Cancer 94(7):2090–2106. https://doi.org/10.1002/cncr.10428
Palmer SN, Meeske KA, Katz ER, Burwinkle TM, Varni JW (2007) The PedsQL brain tumor module: initial reliability and validity. Pediatr Blood Cancer 49(3):287–293. https://doi.org/10.1002/pbc.21026
Muller HL, Muller-Stover S, Gebhardt U, Kolb R, Sorensen N, Handwerker G (2006) Secondary narcolepsy may be a causative factor of increased daytime sleepiness in obese childhood craniopharyngioma patients. J Pediatr Endocrinol Metab 19(Suppl 1):423–429. https://doi.org/10.1055/s-2006-974095
Postiglione E, Antelmi E, Pizza F, Lecendreux M, Dauvilliers Y, Plazzi G (2018) The clinical spectrum of childhood narcolepsy. Sleep Med Rev 38:70–85. https://doi.org/10.1016/j.smrv.2017.04.003
Weil AG, Muir K, Hukin J, Desautels A, Martel V, Perreault S (2018) Narcolepsy and hypothalamic region tumors: presentation and evolution. Pediatr Neurol 84:27–31. https://doi.org/10.1016/j.pediatrneurol.2017.12.016
Fjalldal S, Holmer H, Rylander L, Elfving M, Ekman B, Osterberg K, Erfurth EM (2013) Hypothalamic involvement predicts cognitive performance and psychosocial health in long-term survivors of childhood craniopharyngioma. J Clin Endocrinol Metab 98(8):3253–3262. https://doi.org/10.1210/jc.2013-2000
Crabtree VM, Klages KL, Sykes A, Wise MS, Lu Z, Indelicato D, Merchant TE, Avent Y, Mandrell BN (2019) Sensitivity and specificity of the modified epworth sleepiness scale in children with craniopharyngioma. J Clin Sleep Med 15(10):1487–1493. https://doi.org/10.5664/jcsm.7982
Acknowledgements
The authors thank the patients and their families who participated in this study. This work was supported by Cancer Center Support Grant (CA21765) from the National Cancer Institute and the ALSAC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest that are directly or indirectly related to the research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mandrell, B.N., LaRosa, K., Hancock, D. et al. Predictors of narcolepsy and hypersomnia due to medical disorder in pediatric craniopharyngioma. J Neurooncol 148, 307–316 (2020). https://doi.org/10.1007/s11060-020-03519-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03519-3