Abstract
Purpose
To investigate the frequency, magnitude and possible causes of frame-shifts that may occur between treatment planning and treatment delivery when performing Gamma Knife radiosurgery with rigid frame-based immobilization.
Methods
Differences between computed tomography (CT) framed fiducial stereotactic coordinate reference and cone beam computed tomography stereotactic coordinates after image registration were recorded for 49 frame-based GK radiosurgery cases performed using the Gamma Knife Icon. Parameters recorded include rotational shifts, translational shifts, and the GK-computed Maximum Shot Displacement (MSD) between the two stereotactic coordinate spaces. Other patient-specific parameters were collected and linear regression analysis was performed to evaluate predictors of increased displacement.
Results
The median values of rotational shifts were: pitch 0.14°, yaw 0.17°, and roll 0.13°. The median absolute values of translational shifts were: left–right 0.39 mm, anteroposterior 0.14 mm, and superior-inferior 0. 22 mm. The median value of MSD was 0.71 mm. Twelve cases (24.5%) had a MSD of greater than 1.0 mm. Male gender was associated with increased MSD (p = 0.013) and translational shifts (root-mean-squared value, p = 0.017). Cases with large differences between right and left sided pin lengths were also associated with increased MSD (p = 0.011).
Conclusions
The use of CBCT image guidance in frame-based GK radiosurgery allows unintended frame shifts to be identified and corrected. A significant fraction (24.5%) of patients had large enough shifts to result in a MSD of greater than 1.0 mm. Male gender and eccentrically placed frames were associated with increased MSD, and particular care should be taken in these cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radiosurgery has revolutionized the treatment of neurological disorders. The existing radiosurgery platforms, including Gamma Knife (GK, Elekta AB, Stockholm, Sweden), Cyberknife (Accuray, Sunnyvale, CA), and LINAC-based units, all allow for highly targeted delivery of radiation. To achieve this precise treatment while minimizing damage to adjacent normal tissues, target volumes must be well-defined and immobilized during planning and treatment delivery [1, 2]. This is commonly achieved through the use of a stereotactic head frame which immobilizes the patient during treatment and provides a 3-dimensional stereotactic coordinate system for tumor localization [1,2,3]. As the technique relies on millimeter range accuracy, subtle movements in the stereotactic head frame relative to the target can lead to improper radiation dosing of the target or organs at risk, especially when treatment is given over a single fraction.
The typical workflow of a frame-based GK system involves the use of a stereotactic head frame to immobilize the patient, followed by a MRI or CT scan for defining the stereotactic space and treatment planning. The head frame has fiducials which appear on the scans and allow for registration of the treatment planning images to the stereotactic coordinate system. Following alignment of the images with the coordinate system, a treatment plan is created. This coordinate system is then used for appropriate positioning to allow for targeted delivery of radiation and creates a stereotactic reference. As the rigid attachment of a head frame to the patient is believed to be the most reliable form of immobilization, the idea that unintended frame shifts could cause inaccuracies in radiation delivery is rarely considered a possibility [2, 4].
Until recently there were limited methods to study the extent of frame shifts. The relatively recent introduction of the Gamma Knife Icon system has now provided an innovative method of investigating this issue. The Gamma Knife Icon system has an integrated cone beam CT (CBCT) that is able to obtain images immediately prior to delivery of treatment, allowing for a second check of patient alignment immediately preceding radiosurgery. Although the primary purpose of this system is to ensure appropriate targeting of radiation during frameless Gamma Knife treatments, the integration of CBCT imaging to frame-based Gamma Knife treatment protocols has provided an independent method of assessing accuracy of patient position immediately prior to treatment delivery [5]. The purpose of this study was to investigate the causes and dependencies of frame shifts that may occur between the time of radiosurgery planning and time of treatment delivery and to assess the role of imaging following frame placement to reduce treatment errors. Furthermore, although there are several publications addressing the issue of frame shifts during GK delivery, these publications are from a limited number of centers, and a broader understanding of the frequency of frame shifts during GK is warranted. This work illustrates the extent of frame shifts and the issues encountered during GK delivery at our center. In the current study, frame shifts were determined by measuring the differences between the reference coordinates from the initial planning CT and the pretreatment CBCT coordinates, after rigid CT-CT image co-registration. Patient specific and treatment associated factors were then correlated to the positional data to determine predictors of increased shifts. Through this investigation, we aimed to evaluate the magnitude of frame shifts and identify factors associated with increased discrepancies, in order to help improve the accuracy and the safety of future GK treatments.
Materials and methods
Institutional review board approval for patient data collection was obtained. Data collection involved 49 adult patients who underwent frame-based GK treatments during 2018 at our institution. All patients were treated with a single fraction of radiation. Prior to the date of radiosurgery, an MRI of the brain was obtained. Our radiosurgical workflow has been previously published [6]. In brief, on the day of radiosurgery a head frame was placed on the patient for immobilization, which was secured to the skull with four pins. Each frame placement was performed by a Gamma Knife trained and board certified neurosurgeon. A fiducial indicator box was fixed to the stereotactic frame and a diagnostic CT scan (which served as the stereotactic reference image set) was done and transferred to the treatment planning software. The MRI images obtained of the day prior were registered to the CT images using anatomic landmarks and a plan was finalized. The patient was then taken to the treatment suite and the frame was affixed to the treatment couch. A CBCT was obtained and co-registered to the diagnostic CT, which provided an independent method of evaluating the stereotactic coordinate system. Any rotations and/or translations from the original plan coordinates were computed by the treatment planning software. Set up error was determined by comparing the initial CT to the pretreatment CBCT. The resolution of the CBCT was 0.5 × 0.5 × 0.5mm3 with 0.5 mm slice thickness. The field of view was 224 mm × 224 mm × 224 mm. Image registrations was performed by the physics staff using the automated matching function within the Normalized Mutual Information algorithm, then verified by the treating neurosurgeon and radiation oncologist. Registration was achieved using the entire skull as the region of interest.
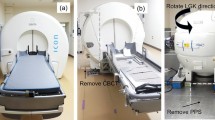
A typical illustration of positional and dose distribution differences between the original planned treatment and the delivered treatment for a frame-based GK treatment is shown in Fig. 1a–c. In cases where a clinically meaningful shift was identified, the neurosurgeon and radiation oncologist physically verified frame fixation, and then re-planned as necessary to allow for accurate treatment (sometimes using the CBCT as the stereotactic reference image set). It is important to note that although set up error can be detected via the use of a pretreatment CBCT, GK Icon only allows for pre-treatment position adjustments for mask based treatments, and does not allow for application of positional corrections when performing framed treatments.
This figure demonstrates set-up error defined as the difference between the planned treatment (based on CT simulation stereotactic reference coordinates) and the delivered treatment (based on CBCT stereotactic coordinates) for a patient undergoing framed based gamma knife treatment on the GK Icon. a Demonstrates a visual representation of set up error where the dashed lined indicates the original plan and the solid line demonstrates the delivered plan. b Demonstrates the magnitude of the shifts in X, Y, and Z directions. c Demonstrates volume of tumor receiving over 12 Gy in the original plan vs. delivered treatment. Note that although minimal differences are detected between the planned and the delivered treatments, corrections cannot applied for frame based treatments
At the time of frame placement, the length of the pins used were physically measured with the use of a ruler and were were recorded. During data analysis, the differences in length between the anterior right vs. anterior left pins, as well as the posterior right vs. posterior left pins, were determined for each patient. For instance, consider a case with anterior right and left pin lengths of 29 mm and 28 mm respectively, and posterior right and left pin lengths of 31 mm and 27 mm respectively. The difference in pin lengths between the anterior right and left is 1 mm, while the difference in pin lengths between the posterior right and left pin lengths is 4 mm. Therefore, the posterior position pin length difference of 4 mm will be documented as the maximum eccentricity between right vs. left pin lengths for this particular case. This type of calculation was performed for all cases and the maximum eccentricity between right vs. left pins was documented and compared between different patients.
Differences between the CT stereotactic reference coordinates and the CBCT stereotactic coordinates were recorded for 49 consecutive frame-based GK radiosurgery cases. Parameters recorded include rotational shifts, translational shifts, and the GK-computed Maximum Shot Displacement (MSD) between the two stereotactic coordinate spaces. Decisions regarding replanning vs. treating were made on a case by case basis and were at the discretion of the treating radiation oncologist and the neurosurgeon based on the magnitude of shift and resultant dosimetry. Other patient-specific parameters were collected and linear regression analyses were performed to evaluate predictors for increased shifts and shot displacements.
Results
Clinical characteristics
Treatment and clinical data were reviewed for the first 49 patients who underwent frame-based Elekta Gamma Knife Icon (GK) treatments in 2018 at our institution. The median age of our patients was 65 years with a minimum age of 30 years and a maximum age of 86 years. Of the analyzed patients, 17 (35%) were male and 32 (65%) were female. KPS was 100 in 14 cases (28.5%), 90 in 19 cases (38.8%), 80 in 7 cases (14.3%), and ≤ 70 in 9 cases (18.4%). Clinical characteristics of the patient cohort are documented in Table 1.
Treatment characteristics
The procedure of frame attachment to the cranium via pin placement was performed by one of four neurosurgeons shown as neurosurgeon 1–4 in Table 1. Neurosurgeon #1 performed 9 procedures (18.4%), #2 performed 5 procedures (10.2%), #3 performed 12 procedures (24.4%) and #4 performed 23 procedures (47.0%). Pins were placed at four locations: anterior right, anterior left, posterior right and posterior left. The median anterior right pin length was 26.2 mm (range 13.3–35.5 mm), median anterior left pin length was 25.9 mm (range 17.3–37.0 mm), median posterior right pin length was 25.8 mm (range 10.8–47.3 mm), and median posterior left pin length was 26.6 mm (range 10.8–44.3 mm) [4]. Sum of pin lengths and maximum pin length were determined for each GK treatment case. The median of the sum of all 4 pin lengths was 104.4 mm and the median of the maximum pin lengths was 29.9 mm. The differences in length between the anterior right vs. anterior left pins, as well as the posterior right vs. posterior left pins, were determined for each patient as described in the methods section. The median value was found to be 5. 2 mm.
Due to unacceptable rotational or translational discrepancies between original plan coordinates and treatment coordinates, 11/49 cases (22.5%) were ultimately re-planned, these findings are shown in Table 1.
Measured shifts
Rotational and translational shifts at the time of treatment were determined by the CBCT obtained immediately prior to treatment. The descriptive statistics of measured shifts are displayed in Table 2. The median values of rotational shifts were: pitch 0.14° [range 0.00°–2.93°, standard deviation (SD) 0.58°]; yaw 0.17° (range 0.01° to 4.60°, SD 0.73°); and roll 0.13° (range 0.00°–0.75°, SD 0.13°). With regard to RMS rotational shifts, 41 cases (83.7%) had shifts between 0 and 0.5°, 3 cases (6.1%) had shifts between 0.5 and 1.0° and 5 cases (10.2%) had shifts greater than 1.0°. The absolute mean RMS rotation was 0.57 mm (range 0.06–5.24, SD 0.91 mm).
The median absolute values of translational shifts were: left–right 0.39 mm (range 0.02–5.89 mm, SD 0.85 mm); anteroposterior 0.14 mm (range 0.00–3.30 mm, SD 0.55 mm); and superior-inferior 0.22 mm (range 0.01–3.74 mm, SD 0.63 mm). With regard to RMS translational shifts, 21 cases (42.9%) had shifts between 0 and 0.5 mm, 20 cases (40.8%) had shifts between 0.5 and 1.0 mm, and 8 cases (16.3%) had shifts greater than 1 mm. The absolute mean RMS translation was 0.85 mm (range 0.16–7.24 mm, SD 1.13 mm).
Maximum shot displacement was determined and, 14 (28.6%) were found to have displacements between 0 and 0.5 mm, 23 cases (47.0%) had displacements between 0.5 and 1.0 mm, and 12 cases (24.5%) had displacements greater than 1.0 mm. The median value of MSD was 0.71 mm (range 0.13–6.75 mm, SD 0.71 mm).
Analysis of patient and treatment characteristics associated with frame shifts
Simple linear regression analysis was performed to determine factors associated with increased frame shifts. Table 3 summarizes the results of these tests. Age, KPS, neurosurgeon, anterior/posterior right pin lengths, anterior/posterior left pin lengths, sum of pin distance and maximum pin length were not associated with increased MSD or RMS rotational/translational shifts ( p > 0.05). Male gender was associated with increased MSD (p = 0.013) and increase RMS rotational (p = 0.028) and RMS translational shifts (p = 0.017) (Fig. 2a). Cases with a large difference between anterior (or posterior) pin lengths were also associated with increased MSD (p = 0.011) (Fig. 2b). Other parameters measured, including patient age, performance status, and pin length, did not show correlation with larger measured shifts or MSD (p < 0.05).
Simple linear regression analysis was performed to determine factors associated with increased frame shifts. a Demonstrates that male gender was associated with increased MSD, increased RMS rotational and RMS translational shifts. b Demonstrates that maximum eccentricity between right vs. left pin lengths significantly associated with greater MSD
Greater posterior right/left pin lengths increasing sum of pin distances, and increasing maximum pin lengths were associated with greater pitch (posterior right p = 0.018; posterior left p = 0.038; sum of pin distances p = 0.039; maximum pin length p = 0.019). Greater anterior left pin length was associated with increased yaw (p = 0.025). Male gender, increasing posterior left pin lengths, and increasing maximum eccentricity between right vs. left pin lengths was associated with greater translational shifts in the superior-inferior direction (male gender p = 0.004; posterior left pin length p = 0.027; maximum eccentricity between right vs. left pin lengths p = 0.014).
Notably, no factors were found to associate with increased roll or increased translational shifts in the left–right or anteroposterior directions.
Discussion
There are currently limited studies regarding the extent and the possible causes of frame shifts during rigid frame-based GK treatments. Peach et al. presented a case study during which planning CT coordinates and treatment CBCT coordinates were compared for patients undergoing frame-based GK. They concluded that subtle frameshifts occur following rigid immobilization and that the use of CBCTs to verify reliability of frame placement can reduce the transmission of clinically significant errors during radiation delivery [7]. Dutta et al. examined 150 cases of Gamma Knife treatments during which CBCT was performed prior to treatment delivery and found that discrepancies in coordinates were less than 1 mm in most instances. The study noted that large differences were associated with low Karnofsky performance scale and longer pin lengths [4]. Li et al. assessed setup and intrafraction positional changes and noted that mean set up errors and intrafraction errors were approximately 0.2 and 0.03 mm, respectively [8]. Carminucci and colleagues performed a study comparing intrafraction error in mask based vs. frame-based GK treatments and found that both forms of treatment demonstrated small setup, translational, and rotational errors [9]. These studies confirm that despite the presumed rigidity of frame-based GK treatments, measurable displacements can still occur during patient setup and treatment delivery.
Our study contributes to this limited body of work by demonstrating that frame-based GK treatments involve small, unintended shifts in a significant portion of the patients treated with this modality. We found that approximately 25% (12/49) of patients had large enough shifts to result in MSDs greater than 1.0 mm, suggesting that frame immobilization may not be as rigid as previously described. We noted that male gender and eccentrically placed frames with larger pin length variations were associated with increased MSD. An early systematic error analysis by Maciunas et al. revealed that the accuracy of frame placement is significantly impacted by factors such as the weight encountered by the frame and quality of imaging [10]. We hypothesize that factors such as incomplete contact with the periosteum, cross-threading of pins, improper angling of pins, over torqueing of the frame during placement, and increased flexion associated with using pins of varying lengths, may all lead to subtle shifts. Patient associated factors that may contribute to frame instability include frame motion during patient positioning, mechanical stress associated with larger weight bearing loads (larger head masses, for instance) and the laxity of bone flaps associated with prior craniotomies that may make secure pin placement difficult. Interestingly, our findings regarding the impact of pin length dissimilarities were independently corroborated by Renier and Nicolas in a prior study regarding the targeting inaccuracies caused by mechanical distortion of stereotactic frames. In this study, the authors noted that although length differences between the two opposite pairs of pins were often very limited, even small increases in the heterogeneity between pin lengths significantly increased the amount of frame distortion. They also found that the level of torque used for frame fixation impacted frame distortion and deviation from the intended stereotactic target [11]. Additionally, although image co-registration is performed by an experienced physicist, it is possible that the quality of image resolution and small offsets in image co-registration could have also contributed to detectable differences between simulation CT coordinates and the CBCT coordinates.
One notable finding of our study is the value of image guidance even when delivering frame-based radiosurgery. In a typical framed based GK workflow, pretreatment imaging immediately prior to radiosurgery is not obtained. Based on the findings of our study, we believe that image guidance using CBCT is a powerful tool to assess motion error. Therefore we routinely obtain pretreatment CBCTs to ensure radiosurgical accuracy. It is however important to consider that a highly experienced SRS center may observe frame shifts at a lower rate in comparison to a newly established program and may opt to not utilize CBCTs on a regular basis. Although our neurosurgeons were very experienced in performing frame placements for Linac based radiosurgery, our center was relatively new at performing frame placements for GK treatments at the time of data gathering. The novelty of this procedure may have contributed to the degree of observed frame shifts at our institution.
To our knowledge, the association of male gender with greater shifts was a novel finding in our study. We hypothesize that this phenomenon may in part be due to the generally large head mass of male patients, although the exact etiology has yet to be studied independently. Regardless, the association of gender with increased shifts is hypothesis generating, and further studies should be performed to evaluate the causes and potential remedies.
A question that often arises when discussing frame displacement is whether a margin should be added to the planning target volumes to ensure adequate target coverage. Although margins are utilized in LINAC-based SRS, given that the aim of GK is to ensure target coverage while achieving maximum sparing of normal brain, margins beyond the GTV are not typically added. Ma et al. used mathematical models to assess the impact of adding 0.5–3.0 mm margins in GK based SRS. The authors found that the addition of a 2 mm margin led to an increase of approximately 55% of the prescription dose volume and a predicted symptomatic necrosis rate of 6–25% [12]. As the GK Icon platform allows for detection and correction of any major shifts prior to treatment, we do not propose the addition of margins to GK treatments when they are performed with the GK Icon. We believe that addition of margins in this situation is likely to increase radiation toxicity to the normal brain without a clear clinical benefit. However, given that we detected shifts in a considerable number of cases, at institutions with GK but without the ability to obtain CBCT imaging prior to treatment (i.e. those without a GK Icon), the addition of margins may reduce the possibility of a target miss depending on the clinical scenario and resultant risks.
There are several limitations of our study that are worth mentioning. First, our study is a single institution retrospective study with a limited sample size. Additionally, the frequency of shifts (25% patients with MSD > 1 mm) detected in our study is somewhat higher than what was observed in other similar studies. It must be noted that the data for this study was collected early in our GK program and we believe that the novelty of our program may have significantly contributed to the observed rate of detection and correction of frame shifts. Therefore, our findings are particularly relevant among new GK Icon programs. We hypothesize that the observed shifts will reduce over time as we continue to refine our process to maximize the safety of this procedure.
Our study also did not assess the influence of other confounding variables on set up error, such as medical comorbidities, pain, and patient anatomic characteristics, such as head size and neck length. Furthermore, our study did not examine the extent and factors associated with intrafraction motion or shifts occurring during other steps in the process of GK delivery. We plan to address these factors in future studies to better characterize the causes of frame shifts during GK delivery.
Conclusions
The purpose of our study was to evaluate the magnitude and the factors that contribute to frameshifts during GK radiosurgery. Our study identified that detectable frameshifts occur during GK radiosurgery. However, given that we have limited follow up data, it is difficult to determine whether subtle frame shifts lead to any clinically relevant consequences and further studies are needed to evaluate the long term impact of frame shifts with regard to disease control and radiation toxicity. We hypothesized that a number of factors related to mechanical stress on the frame and the uncertainty of image co-registration likely contribute to frame shifts. Factors such as large head size, time from frame placement to treatment delivery, and functional status of the patient that were not explored in our study also likely play some role in the observed shifts. The results of our study shed light into the technical uncertainties of GK radiosurgery and we believe that further exploration of this topic will lead to improvements in the safety and the efficacy of radiosurgery delivery in the future.
References
Leksell L, Jernberg B (1980) Stereotaxis and tomography. A technical note Acta Neurochir 52(1–2):1–7. https://doi.org/10.1007/bf01400939
Lunsford LD, Flickinger J, Lindner G, Maitz A (1989) Stereotactic radiosurgery of the brain using the first United States 201 cobalt-60 source gamma knife. Neurosurgery 24(2):151–159. https://doi.org/10.1227/00006123-198902000-00001
Wu A (1992) Physics and dosimetry of the gamma knife. Neurosurg Clin N Am 3(1):35–50
Dutta SW, Kowalchuk RO, Trifiletti DM, Peach MS, Sheehan JP, Larner JM, Schlesinger D (2018) Stereotactic shifts during frame-based image-guided stereotactic radiosurgery: clinical measurements. Int J Radiat Oncol Biol Phys 102(4):895–902. https://doi.org/10.1016/j.ijrobp.2018.05.042
Duggar WN, Morris B, Fatemi A, Bonds J, He R, Kanakamedala M, Rey-Dios R, Vijayakumar S, Yang C (2019) Gamma Knife((R)) icon CBCT offers improved localization workflow for frame-based treatment. J Appl Clin Med Phys 20(11):95–103. https://doi.org/10.1002/acm2.12745
Trifiletti DM, Dutta SW, Lee CC, Sheehan JP (2019) Pituitary tumor radiosurgery. Prog Neurol Surg 34:149–158. https://doi.org/10.1159/000493059
Peach MS, Trifiletti DM, Dutta SW, Larner JM, Schlesinger DJ, Sheehan JP (2018) Spatial shifts in frame-based Gamma Knife radiosurgery: a case for cone beam CT imaging as quality assurance using the Gamma Knife(R) Icon. J Radiosurg SBRT 5(4):315–322
Li W, Cho YB, Ansell S, Laperriere N, Menard C, Millar BA, Zadeh G, Kongkham P, Bernstein M, Jaffray DA, Chung C (2016) The use of cone beam computed tomography for image guided gamma knife stereotactic radiosurgery: initial clinical evaluation. Int J Radiat Oncol Biol Phys 96(1):214–220. https://doi.org/10.1016/j.ijrobp.2016.04.011
Carminucci A, Nie K, Weiner J, Hargreaves E, Danish SF (2018) Assessment of motion error for frame-based and noninvasive mask-based fixation using the Leksell Gamma Knife Icon radiosurgery system. J Neurosurg 129(Suppl1):133–139. https://doi.org/10.3171/2018.7.GKS181516
Maciunas RJ, Galloway RL Jr, Latimer JW (1994) The application accuracy of stereotactic frames. Neurosurgery 35(4):682–694. https://doi.org/10.1227/00006123-199410000-00015 (discussion 694-685)
Renier C, Massager N (2019) Targeting inaccuracy caused by mechanical distortion of the Leksell stereotactic frame during fixation. J Appl Clin Med Phys 20(5):27–36. https://doi.org/10.1002/acm2.12576
Ma L, Sahgal A, Larson DA, Pinnaduwage D, Fogh S, Barani I, Nakamura J, McDermott M, Sneed P (2014) Impact of millimeter-level margins on peripheral normal brain sparing for gamma knife radiosurgery. Int J Radiat Oncol Biol Phys 89(1):206–213. https://doi.org/10.1016/j.ijrobp.2014.01.011
Funding
No funding was required.
Author information
Authors and Affiliations
Contributions
DSS, JLP, ARH, TDM, RR, SMH, BM, SK, DMT, LAV: Conception and design. DSS, ARH, JLP, TDM, DMT, LAV: Data collection. DSS, ARH, DMT, LAV: Data analysis and interpretation. DSS, TDM, DMT, LAV: Manuscript writing. DSS, JLP, TDM, RR, SMH, BM, SK, ARH, DMT, LAV: Final approval of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Trifiletti receives unrelated clinical trial research funding from Novocure and publishing fees from Springer. The remaining authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seneviratne, D.S., Hadley, A.R., Peterson, J.L. et al. Assessment of unintended shifts during frame-based stereotactic radiosurgery using cone beam computed tomography image guidance. J Neurooncol 148, 273–279 (2020). https://doi.org/10.1007/s11060-020-03463-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03463-2