Abstract
Bevacizumab (BV), a neutralizing monoclonal antibody against the vascular endothelial growth factor ligand, is recognized as a potent anti-angiogenic agent with antitumor activity. The aim of this single-center, retrospective, longitudinal study was to investigate the possible predictive value of baseline demographic, clinical and laboratory parameters for early 3-month response to BV therapy in patients with recurrent glioma. Forty-nine patients with recurrent glioma received BV at 10 mg/kg intravenously every 3 weeks alone or in association with chemotherapy were included in this study. Blood samples were collected from all patients before the first (baseline), the second and the third administration of BV. After 3 months of BV therapy, patients with partial response were defined as responders whereas patients with stable or progressive disease were defined as non-responders. The median overall follow-up was 8 months (range 1–73), the median overall survival (OS) was 8 months (95% CI 6–10) and the median progression free survival (PFS) was 4 months (95% CI 3–5). Thirty-five % of patients were responders and showed significantly lower von Willebrand factor (VWF) levels than non-responders at all sample times (p < .02 for all). Also, on multivariate analysis the baseline VWF value was the only predictor for an early response to BV therapy. Furthermore, D-dimer and prothrombin fragment 1+2 were predictive factors for OS while Karnofsky performance status resulted predictive for PFS. VWF antigen value is a possible predictive biomarker for an early 3-month response to BV therapy in recurrent glioma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gliomas are tumors of glial cell origin that represent 77% of primary malignant brain neoplasms [1]. Glioblastoma (GBM) is the most common and aggressive form of gliomas, categorized as World Health Organization (WHO) grade IV. It is associated with very poor prognosis since a 2-year relative survival rate varies from 29.8% at 20–44 years to only 1.4% in patients over 75 years of age [1]. Furthermore, GBM is one of the most vascularized human tumours and express high levels of pro-angiogenic factors, including vascular endothelial growth factor (VEGF) [2]. VEGF is a major regulator of tumour angiogenesis promoting endothelial cell proliferation, survival and migration [3]. Bevacizumab (BV), a neutralizing monoclonal antibody against the VEGF ligand functioning as a chimeric VEGF receptor, is recognized as a potent anti-angiogenic agent with antitumor activity [4].
The effects of BV in the treatment of glioma were demonstrated to be transient since almost all patients progress after a median time of 3–5 months [4]. In two phase III trials, the median progression free survival (PFS) was 3–4 months longer in patients with GBM on BV plus standard therapy compared to those on only standard treatment [5]. These data resulted in line with a previous Cochrane Database Systemic Review showing that only PFS and not overall survival (OS) may benefit by use of BV in GBM [6]. Besides, the clinical outcomes suggest that a substantial proportion of GBM are either initially resistant or quickly develop resistance to VEGF blockade because of adaptive upregulation of alternative angiogenic pathways [4]. Thus, it is important to identify patients’ subpopulation that could benefit from BV therapy in order to define specific criteria for starting, discontinuing or restarting BV.
However, the predictive biomarkers remained elusive despite almost over a decade of clinical development for anti-VEGF therapies. Previous studies assessed the prognostic value of fluorodeoxyglucose-PET uptake in recurrent high-grade glioma (HGG) under BV and irinotecan therapy, which resulted the most powerful predictor of either PFS, OS or response to BV-based therapy among all variables: histological grade, Karnofsky performance status (KPS), steroid intake, and number of previous treatments [7]. Similarly, an increase in (18)F-fluorodopa- or (18)F-fluorothymidine-PET uptake after BV treatment may be a useful biomarker for predicting PFS and OS in recurrent gliomas treated with BV [8]. Also pretreatment relative cerebral blood volume at magnetic resonance imaging (MRI) was identified as a potential predictive imaging biomarker in BV-treated recurrent GB [9] as well as perfusion MRI may be helpful for evaluating the anti-angiogenic effect of a BV treatment [10]. However, the acquisition and analysis methodology of these techniques need to be better standardized.
In addition to prognostic values of pretreatment MRI also some molecular markers (EGFR status and MGMT methylation) in patient with recurrent glioma were demonstrated to be predictive for either better response to BV, a longer PFS or OS [11]. In a more recent trial the histo-molecular subtypes of glioma did not resulted predictive of BV response rates [12]. Studies on predictive value of blood biomarkers for monitoring BV therapy have been conducted in other neoplasms suggesting a possible predictive role of hypertension and VEGF polymorphisms but with their limited use in the clinical practice [13]. In a more recent study, the patients with a non-small cell lung cancer and increased plasma levels of VEGF, E-selectin, and S-ICAM seemed to benefit more from BV therapy [14]. However, there are not validated biomarkers for the response to BV in glioma.
In our analysis we have selected baseline laboratory parameters both closely influenced by BV pharmacological action and representative of hypercoagulable cancer status. Indeed, VEGF influences not only tumoral angiogenesis but also coagulation as well as vascular homeostasis by mediating the repair of damaged endothelial surfaces [3]. In fact, VEGF blockade increases both thrombotic and haemorrhagic events besides GBM patients show a pre-existing predisposition to develop venous thromboembolism with a slightly higher risk than other cancer patients for this complication [15].
Cancer patients have a hypercoagulable state expressed by increase of tissue factor (TF), prothrombin fragment 1+2 (F1+2), thrombin–antithrombin complexes (TAT), and D-dimer indicating the presence of in vivo thrombin generation and fıbrin formation and fıbrinolysis [16]. Activation of the coagulation system may have a role in the progression of GBM likely because intratumoral vaso-occlusive thrombosis contributes to hypoxia, necrosis and angiogenesis [17].
In addition to their hemostatic function, TF and thrombin promote angiogenesis through the endothelial cells (EC) activation with exocytosis of Weibel–Palade bodies (WPB), which store regulators of angiogenesis and inflammation, including angiopoietin 2 (Ang-2) and von Willebrand factor (VWF) [18]. VWF mediates platelet adhesion to both the subendothelial matrix and endothelial surfaces as well as carries coagulation factor VIII (FVIII), pro-coagulant anti-hemophilic factor, in the circulation [19]. Also some degradation products of fibrin have been previously shown to hold angiogenic properties [20].
The aim of our study was to investigate the possible predictive value of baseline demographic (sex, age), clinical (brain tumour type, its methylation, KPS, concomitant chemotherapy, steroid dose) and laboratory (angiogenic factors, markers of coagulation and fibrinolysis activation, complete blood count) parameters for early 3-month response to BV therapy in patients with recurrent glioma. Furthermore, we assessed the prognostic value of an early response to BV therapy as well as of the same baseline parameters for patient’s PSF and OS.
Methods
Study design
This single-center, retrospective, longitudinal study was an ancillary sub-study of a prospective, single-center, open-label trial, concluded in 2013 and aimed to evaluate early predictive biomarkers from dynamic contrast-enhanced MRI for the response to BV in HGG as well as was a part of Institutional biobank. The study was approved by the Institutional Ethics Committee and a written informed consent was received from each patient.
We enrolled 49 patients with recurrent glioma treated with BV at 10 mg/kg intravenously every 3 weeks alone or in association with chemotherapy between July 2008 and September 2013.
All patients received at baseline (i.e. before the first BV administration) a neurological evaluation, KPS score assessment [21] and steroid therapy dose recording as reported in the database of Neuro-oncology Unit. Blood samples were routinely collected from all patients before the first (T0 or baseline), the second (T1) and the third (T2) administration of BV. Samples stored in the Institutional biobank were analysed for an additional testing by laboratory biologists blinded to clinical response and outcome.
All patients underwent brain MRI at baseline and every 3 months up to progression. Both Fluid Attenuated Inversion Recovery and contrast-enhanced weighted sequences were considered for evaluating the tumor volume as well as assessing the response to treatment, according to the Response Assessment Neuro-Oncology criteria (RANO criteria) [22]. According to RANO criteria, we considered: complete response (CR) as requiring all of the following: complete disappearance of all enhancing measurable and non-measurable disease sustained for at least 4 weeks; no new lesions; stable or improved T2/FLAIR lesions; and no corticosteroids or on physiological replacement doses only, and stable or improved clinical condition. In the absence of a confirming scan 4 weeks later, this response was considered only stable disease (SD). Partial response (PR) required all of the following: ≥ 50% decrease, compared with baseline, in the sum of products of perpendicular diameters of all measurable enhancing lesions sustained for at least 4 weeks; no progression of non-measurable disease; no new lesions; stable or improved T2/FLAIR lesions on same or lower dose of corticosteroids compared with baseline scan; and on a corticosteroid dose not greater than the dose at time of baseline scan and is stable or improved clinically. In the absence of a confirming scan 4 weeks later, this response was considered only SD. SD occurred if the patient did not qualify for CR, PR, or disease progression and required the following: stable T2/FLAIR lesions on same or lower dose of corticosteroids compared with baseline scan and clinically stable status. In the event that the corticosteroid dose was increased for new symptoms and signs without confirmation of disease progression on neuroimaging, and subsequent follow-up imaging showed that this increase in corticosteroids was required because of disease progression, the last scan considered to show SD was that obtained when the corticosteroid dose was equivalent to the baseline dose. Progression was defined by any of the following: ≥ 25% increase in sum of the products of perpendicular diameters of enhancing lesions (compared with baseline if no decrease) on stable or increasing doses of corticosteroids; a significant increase in T2/FLAIR lesions on stable or increasing doses of corticosteroids compared with baseline scan or best response after initiation of therapy, not due to comorbid events; the appearance of any new lesions; clear progression of non-measurable lesions; or definite clinical deterioration not attributable to other causes apart from the tumour, or to decrease in corticosteroid dose. Failure to return for evaluation as a result of death or deteriorating condition was also considered as progression.
Despite SD is usually considered as a response to therapy, we considered patients with SD at first MRI (after 3 months of BV therapy) as early non-responders since BV usually reduces an initial tumor volume even in patients who will progress after only a few months [4]. Thus, we defined as early responders the patients with PR whereas non-responders the patients with SD or PD.
In September 2017 the data of PSF and OS of all patients were assessed.
Blood collection and laboratory assays
Blood samples were collected in EDTA tubes, 3.2% sodium citrate tubes and tubes without anticoagulant (Vacutainer, Becton–Dickinson, Franklin Lakes, NJ, USA). Complete blood cell counts were obtained on EDTA anticoagulated whole blood using the hematology analyzer (UniCel® DxH 800; Beckman Coulter, Miami, FL, USA). With and without citrate anticoagulant tubes were centrifuged within 1 h at 2500 g for 20 min, to obtain platelet-poor plasma and serum. The plasma aliquots were either immediately processed for coagulation assays or stored at − 80 °C for subsequent testing. All coagulation parameters (D-dimer, FVIII, VWF antigen) were assayed by clotting, chromogenic and immunological methods on fully-automated ACLTOP analyzer using HemosIL® commercial kits (Instrumentation Laboratory Company, Bedford, MA, USA). Abnormal values were defined by the clinical laboratory or manufacturer’s assay. Plasma levels of TAT and F1+2 were measured by enzyme-linked immunosorbent assay Enzygnost® TAT micro and Enzygnost® F1+2 mono kits, respectively (Siemens Healthcare Diagnostics Inc, NY, USA), according to the manufacturer’s instructions. Both assays employ the quantitative sandwich enzyme immunoassay technique. All samples showing values above the standard curve were re-tested with appropriate dilutions. Plasma levels of plasminogen-activator inhibitor type 1 (PAI-1) were determined by Asserachrom® kit (DiagnosticaStago, Asnieres, France), according to the manufacturer’s instructions, employing the quantitative sandwich enzyme immunoassay technique. Serum levels of VEGF were measured using Quantikine Human VEGF Immunoassay (R&D Systems, Minneapolis, MN, USA), according to the manufacturer’s instructions. All samples were run in duplicate, and the analysis was repeated if the median coefficient of variance for all the analyses was > 25% for a given sample.
Statistical analysis
Descriptive statistics were used to describe the patients’ characteristics. The association between variables was tested by the Pearson Chi-Square test or the Fisher’s Exact test. The comparison of measures obtained at different time points in the same patients was performed by Wilcoxon or Friedman non parametric test. The comparison between groups was performed by Mann–Whitney U test or Kruskal–Wallis non parametric test, when appropriate. The Spearman non-parametric rank test was used to correlate the data. Bonferroni correction for multiple comparisons was applied, when appropriate.
The Kaplan–Meier method was used to estimate PFS and OS, calculated from BV initiation. The log-rank test will be used to assess differences between subgroups. The level of significance was set at p ≤ .05.
The receiver operating characteristic and the maximally selected Log-Rank statistics analysis were applied to the continuous variable in order to estimate the most appropriate cut-off values able to split patients into groups with different outcome probabilities [23].
The odds ratio (OR), hazard ratio (HR) and the 95% confidence intervals (95% CI) were estimated for each variable. On univariate analysis baseline demographic and clinical characteristics such as sex, age, brain tumour type and its methylation, KPS, concomitant chemotherapy as well as laboratory parameters including platelet count, mean volume and distribution width, neutrophil and lymphocyte counts, neutrophil/lymphocyte ratio, hemoglobin, circulating levels of VEGF, VWF, FVIII, TAT, F1+2, PAI-1and D-dimer were evaluated.
Variables testing significant on univariate analysis were entered into multivariate analysis. Multivariate logistic regression model and Cox regression model were developed using stepwise regression (forward selection) to compare the predictive power of different factors. Enter limit and remove limit were p = .10 and p = .15, respectively.
The SPSS (21.0), R (2.6.1), and MedCalc (14.2.1) licensed statistical programs were used for all analyses.
Results
Patient’s demographic and clinical characteristics
The patient’s demographic and clinical characteristics are shown in Table 1. The median period between the last chemotherapy and BV initiation was 2 months (range 1–54) while the median period between a more recent surgery and BV onset was 13 months (2–220). Baseline dexamethasone dose was 8 mg (0–24). The median number of BV administrations was 4 (1–32). The median follow-up was 8 months (range 1–73). The median PFS was 4 months (95% CI 3–5) and the median OS was 8 months (95% CI 6–10). 1-year OS was 26.5% and 2-year OS was 14.3%.
Biomarkers analyzed
Correlations between patient’s baseline demographic, clinical and laboratory variables
-
(a)
males compared to females had a significantly lower both FVIII (152 vs. 232%, p = .01) and platelet count (137 vs. 199 × 109/L, p = .02) but a higher Hb (14.4 vs. 12.3 g/dL, p = .04);
-
(b)
patients older than 44 years compared to others had a higher either VWF (201 vs. 159%, p = .01), neutrophil count (5.7 vs. 3.8 × 109/L, p = .04) or neutrophil/lymphocyte ratio (6.2 vs. 2.8, p = .007);
-
(c)
patients with KPS lower than 80 compared to others had a higher either D-dimer (402 vs. 127 ng/mL, p = .002), FVIII (228 vs. 145%, p = .001), TAT (7.8 vs. 4.4 µg/L, p = .02), VEGF (319 vs. 197 pg/mL, p = .03), VWF (191 vs. 164%, p = .04) or neutrophil count (7.6 vs. 4.1 × 109/L, p = .01);
-
(d)
patients treated with both BV and concomitant chemotherapy compared to those treated only with BV had a lower VEGF (197 vs. 336 pg/mL, p = .04) and a higher Hb (14.7 vs. 12.3 g/dL, p = .003);
-
(e)
there were significant Spearman correlations between FVIII and either VWF (r = 0.8, p < .0001), D-dimer (r = 0.6, p < .0001), TAT (r = 0.5, p < .0001) or PAI-1 (r = 0.43, p = .002); between D-dimer and VWF (r = 0.55, p < .0001); between F1+2 and TAT (r = 0.6, p < .0001); between platelet count and either neutrophil (r = 0.42, p = .008) and lymphocyte counts(r = 0.55, p < .0001), hemoglobin (r = 0.45, p = .001) or PAI-1 (r = 0.51, p < .0001); between lymphocyte count and hemoglobin (r = 0.6, p < .0001) (Table 2).
Patient response to BV therapy
Patient response to BV therapy was defined by RANO criteria (see “Methods” section) and a first MRI was performed after 3 months from BV initiation. This was defined as a point time for an early patient response to BV therapy.
At this phase, 17 patients (35%) showed a PR, 8 patients (16%) had a SD and 24 patients (49%) had a PD, thus 35% of patients were early responders and 65% of patients were non-responders.
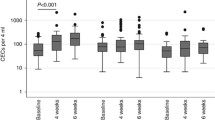
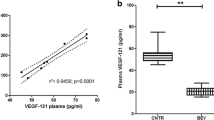
Among all laboratory parameters only serum VEGF levels markedly decreased in all patients after the onset of treatment (p < .0001) whereas VWF antigen significantly increased compared with baseline (p = .001) (Table 3).
The patients treated with both BV and concomitant chemotherapy compared to those treated only with BV had at T1 a higher both D-dimer (272 vs. 134 ng/mL, p = .024) and Hb (14.4 vs. 13.6 g/dL, p = .05) while at T2 they had a higher both D-dimer (318 vs. 124 ng/mL, p = 02) and PAI-1 (44 vs. 21 ng/mL, p = 02).
Biomarkers predictive of response to BV therapy
There were not significant differences for all baseline variables among PR, SD and PD patients, however, at T2 a VWF value became significantly different among three groups (PR 155 vs. SD 188 vs. PD 197%, p = .02). Responders (PR) showed significantly lower VWF levels than non-responders (SD and PD) either at baseline, at T1 or at T2 (p = .02 for all).
There was a low correlation between baseline VWF and steroid dose (p = .001, R = 0.48), but no correlation between baseline VWF and time frame from both the previous chemotherapy and a more recent surgery to BV onset.
Similarly, there was a trend (p = .07) for lower baseline levels of plasma FVIII in responders (median 151, range 88–240) than in non-responders (median 199 range 96–342), which have become significantly lower at T2 [p = .045, median 136 (92–260) vs. 193 (107–350), respectively]. There were no significant differences between responders and non-responders in other laboratory parameters at baseline and during the treatment (data not shown).
On univariate analysis, both lower baseline VWF (p = .02) and FVIII (p = .046) were associated with an early response to BV therapy while on multivariate analysis the only significant predictor remained a VWF value (OR 0.988, 95% CI 0.978–0.998, p = .02) (Table 4).
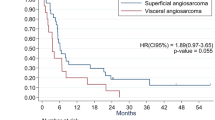
Biomarkers predictive of PFS and of OS
On univariate analysis a lower baseline either D-dimer (p = .002, Fig. 1a), F1+2 (p = .02, Fig. 1b) or TAT (p = .03) as well as a higher KPS (p = .02) or an early response to BV therapy (p = .05, Fig. 1c), were associated with improved OS, while on multivariate analysis only both lower D-dimer (HR 2.336, 95% CI 1.215–4.493, p = .01) and F1+2 (HR 2.934, 95% CI 1.0–8.651, p = .05) were predictive factors for improved OS (Table 4). On univariate analysis both lower FVIII (p = .03) and higher KPS (p = .046) were associated with improved PFS whereas on multivariate analysis only a higher KPS (HR 2.03, 95% CI 1.01–4.07, p = .046) resulted predictive (Table 4).
Discussion
The results of our study show a possible predictive role of VWF antigen as biomarker for an early 3-month response to BV therapy in patients with recurrent glioma. Our data should be considered preliminary because of some shortcomings of this study like single-center and retrospective design, small sample size and heterogenous population for both tumour type and BV therapy (concomitant or alone). A lower VWF level was found in responders compared to non-responders not only at baseline but also in course of two first BV administrations albeit there was its gradual increase. However, it may be considered only as an early biomarker for response to BV since it was not associated with a better PFS and OS. While the reduction in VEGF value during the BV therapy is certainly treatment-related, it is still not clear whether the increase in circulating levels of VWF is directly dependent from therapy or from host’s compensative response to this drug related to VWF–VEGF negative modulation. Moreover, since a VWF level has been previously demonstrated to be influenced by a high (1.0 mg/kg) but not a low (0.04 mg/kg) dose of dexamethasone in healthy people [24], we evaluated the relationships between baseline steroid dose and VWF value in our patients. We found a low correlation between these parameters probably because none of the patients was treated with a high steroid dose.
Some previous papers showed an increase in VWF and FVIII in testicular cancer patients especially in course of vascular events during bleomycin, etoposide and cisplatin chemotherapy [25], as well as an increase of VWF antigen in advanced colorectal cancer during oxaliplatin-based chemotherapy but only in patients that were not treated concomitantly with bevacizumab [26]. Our patients treated with both BV and concomitant chemotherapy were not different from those treated with only BV for all baseline parameters and their VWF was not different even at T1 and T2. Moreover, a baseline value of laboratory parameters in our population was unlikely influenced by previous chemotherapies because there was a wash-out interval from their suspension and an onset of BV either with or without concomitant chemotherapy.
VWF plays two major functions in primary and secondary hemostasis both by promoting platelet adhesion and aggregation to the subendothelium at sites of vascular injury and by participating indirectly in the coagulation process as non-covalently binding factor VIII protecting it from proteolytic degradation [27].
Furthermore, it has recently become evident that VWF is involved in several pathologic processes beyond hemostasis such as cell proliferation, vascular inflammation, apoptosis and tumour metastasis [28]. In particular, Starke et al. demonstrated that the lack of VWF promotes angiogenic processes as was illustrated by markedly increased endothelial cell proliferation in the absence of VWF in vitro and an increased vessel density of the vasculature in the ears of VWF-deficient mice [29]. The molecular basis of this VWF-dependent effect is still not completely clear. Experimental data point to VWF as a negative modulator of VEGF-dependent angiogenesis via multiple intracellular and extracellular pathways involving Vitronectin and Ang-2, both ligands for VWF [29]. Unfortunately, we did not evaluate the circulating Ang-2 level in our patients, thus we cannot verify this hypothesis basing on the circulating levels of both VWF and Ang-2.
In accordance with these experimental data, there was also found an increase of circulating EC and cytokines concerning angiogenesis in patients with genetic deficit of VWF [30]. We could hypothesize that the patients with a lower circulating VWF value in our study are those with increased angiogenesis and thus more susceptible to the effect of the anti-angiogenic agents.
We also found a trend for lower plasma FVIII levels in responders compared to non-responders, as could be expected due to VWF binding, which has become statistically significant after two treatment cycles. This finding could mean that responders have a less procoagulant status than no responders.
Furthermore, on univariate analysis PFS was associated with both FVIII level (inversely) and KPS (directly) albeit on multivariate analysis only KPS resulted predictive for PFS. However, a PFS of responders, differently from their FVIII, was not different from that of non-responders. In a large randomized, double-blind, placebo-trial in newly diagnosed GBM, first-line BV therapy in addition to standard radiotherapy–chemotherapy prolonged PFS of 3–4 months but did not improve their OS [31]. In the recurrent GBM, the evaluation of literature data using weighted median estimate supported the prolongation of both PFS and OS during BV therapy alone or in combination with chemotherapy [5]. However, we had no placebo-control group and our patient’s sample was relatively small as well as their median PFS was of only 4 months.
Despite on univariate analysis an early response to BV therapy resulted associated with improved OS in our patients, on multivariate analysis only lower D-dimer and F1+2 values were independently predictive for improved OS confirming the results of Vienna Cancer and Thrombosis study on the association of higher D-dimer with poor prognosis in a large cancer patient population [32]. Our results are also in line with the findings of a longitudinal study conducted by Reitter et al. in 112 cancer patients in which significantly higher levels of FVIII, P-selectin and D-dimer were associated with shorter survival [33].
Today, it is recognized that there is a complex, reciprocal relationship between cancer and thrombosis [16]. Indeed, tumor cells have the capacity to activate the hemostatic system and this leads to an increased thrombotic risk in cancer patients [34]. Tumor cells are able to activate the coagulation system both directly by the release of procoagulants factors and indirectly by the activation of EC, leukocytes and platelets as well as by the production of VEGF, mucinous glycoproteins, and circulating TF–bearing microparticles [35]. On the other hand, the thrombin generation and fibrin formation have been implicated in angiogenesis, tumor cell invasion and metastatic spread. Therefore, our findings further support a relation between an activation of hemostasis, reflected by increased plasma levels of D-dimer and F1+2, and a more aggressive tumor biology leading to poor clinical outcomes.
In conclusion, our preliminary data suggest that a baseline VWF antigen level might help to predict an early response to BV therapy in recurrent glioma patients. However, the role of angiogenic factors as predictors of response to angiogenic treatment requires further exploration. A more extensive analysis of carefully selected circulating biomarkers with a mechanistic link to the VEGF pathway is required to predict benefits from anti-angiogenetic treatments including BV, to monitor treatment response and to assess whether and when to discontinue treatment.
References
Schwartzbaum JA, Fisher JL, Aldape KD, Wrensch M (2006) Epidemiology and molecular pathology of glioma. Nat Clin Pract Neurol 2(9):494–503
Kargiotis O, Rao JS, Kyritsis AP (2006) Mechanisms of angiogenesis in gliomas. J Neurooncol 78(3):281–293
Jain RK (2002) Tumor angiogenesis and accessibility: role of vascular endothelial growth factor. Semin Oncol 29(6 Suppl 16):3–9
Yi Li S, Ali J, Clarke, Cha S (2017) Bevacizumab in recurrent glioma: patterns of treatment failure and implications. Brain Tumor Res Treat 5(1):1–9
Diaz RJ, Ali S, Qadir MG, De La Fuente MI, Ivan ME, Komotar RJ (2017) The role of bevacizumab in the treatment of glioblastoma. J Neurooncol 133(3):455–467
Khasraw M, Ameratunga MS, Grant R, Wheeler H, Pavlakis N (2014) Antiangiogenic therapy for high-grade glioma. Cochrane Database Syst Rev 22(9):CD008218. https://doi.org/10.1002/14651858.CD008218.pub3
Colavolpe C, Chinot O, Metellus P, Mancini J, Barrie M, Bequet-Boucard C, Tabouret E, Mundler O, Figarella-Branger D, Guedj E (2012) FDG-PET predicts survival in recurrent high-grade gliomas treated with bevacizumab and irinotecan. Neuro Oncology 14(5):649–657. https://doi.org/10.1093/neuonc/nos012
Harris RJ, Cloughesy TF, Pope WB, Nghiemphu PL, Lai A, Zaw T, Czernin J, Phelps ME, Chen W, Ellingson BM (2012) 18F-FDOPA and 18F-FLT positron emission tomography parametric response maps predict response in recurrent malignant gliomas treated with bevacizumab. Neuro Oncology 14(8):1079–1089. https://doi.org/10.1093/neuonc/nos141
Kickingereder P, Wiestler B, Burth S, Wick A, Nowosielski M, Heiland S, Schlemmer HP, Wick W, Bendszus M, Radbruch A (2015) Relative cerebral blood volume is a potential predictive imaging biomarker of bevacizumab efficacy in recurrent glioblastoma. Neuro Oncology 17(8):1139–1147. https://doi.org/10.1093/neuonc/nov028
Choi SH, Jung SC, Kim KW, Lee JY, Choi Y, Park SH, Kim HS (2016) Perfusion MRI as the predictive/prognostic and pharmacodynamic biomarkers in recurrent malignant glioma treated with bevacizumab: a systematic review and a time-to-event meta-analysis. J Neurooncol 128(2):185–194. https://doi.org/10.1007/s11060-016-2102-4
Chen C, Huang R, MacLean A, Muzikansky A, Mukundan S, Wen PY, Norden AD (2013) Recurrent high-grade glioma treated with bevacizumab: prognostic value of MGMT methylation, EGFR status and pretreatment MRI in determining response and survival. J Neurooncol 115(2):267–276. https://doi.org/10.1007/s11060-013-1225-0
Toft A, Urup T, Christensen IJ, Michaelsen SR, Lukram B, Grunnet K, Kosteljanetz M, Larsen VA, Lassen U, Broholm H, Poulsen HS (2018) Biomarkers in recurrent grade III glioma patients treated with bevacizumab and irinotecan. Cancer Invest 2:1–10. https://doi.org/10.1080/07357907.2018.1430818
Jubb AM, Harris AL (2010) Biomarkers to predict the clinical efficacy of bevacizumab in cancer. Lancet Oncol 11:1172–1183. https://doi.org/10.1016/S1470-2045(10)70232-1
Rodríguez Garzotto A, Díaz-García CV, Agudo-López A, Prieto García E, Ponce S, López-Martín JA, Paz-Ares L, Iglesias L, Agulló-Ortuño MT (2016) Blood-based biomarkers for monitoring antiangiogenic therapy in non-small cell lung cancer. Med Oncol 33(10):105. https://doi.org/10.1007/s12032-016-0824-y
Brandes AA, Bartolotti M, Tosoni A, Poggi R, Franceschi E (2015) Practical management of bevacizumab-related toxicities in glioblastoma. Oncologist 20(2):166–175
Rickles FR, Falanga A (2001) Molecular basis for the relationship between thrombosis and cancer. Thromb Res 102:V215-224
Magnus N, D’Asti E, Garnier D, Meehan B, Rak J (2013) Brain neoplasms and coagulation. Semin Thromb Hemost 39(8):881–895
Belting M, Dorrell MI, Sandgren S, Aguilar E, Ahamed J, Dorfleutner A, Carmeliet P, Mueller BM, Friedlander M, Ruf W (2004) Regulation of angiogenesis by tissue factor cytoplasmic domain signaling. Nat Med 10(5):502–509
Franchini M, Frattini F, Crestani S, Bonfanti C, Lippi G (2013) von Willebrand factor and cancer: a renewed interest. Thromb Res 131(4):290–292
Thompson WD, Smith EB, Stirk CM, Marshall FI, Stout AJ, Kocchar A (1992) Angiogenic activity of fibrin degradation products is located in fibrin fragment E. J Pathol 168(1):47–53
Schag CC, Heinrich RL, Ganz PA (1984) Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncology 2(3):187–193
Wen PY, Macdonald DR, Reardon DA et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neurooncology working group. J Clin Oncol 28:1963–1972
Horton TLB (2003) On the exact distribution of maximally selected rank statistics. Comput Statist Data Anal 43:121–137
Jilma B, Cvitko T, Winter-Fabry A, Petroczi K, Quehenberger P, Blann AD (2005) High dose dexamethasone increases circulating P-selectin and von Willebrand factor levels in healthy men. Thromb Haemost 94(4):797–801
Lubberts S, Boer H, Altena R, Meijer C, van Roon AM, Zwart N, Oosting SF, Kamphuisen PW, Nuver J, Smit AJ, Mulder AB, Lefrandt JD, Gietema JA (2016) Vascular fingerprint and vascular damage markers associated with vascular events in testicular cancer patients during and after chemotherapy. Eur J Cancer 63:180–188. https://doi.org/10.1016/j.ejca.2016.05.022
Nishigori N, Matsumoto M, Koyama F, Hayakawa M, Hatakeyayama K, Ko S, Fujimura Y, Nakajima Y (2015) von Willebrand factor-rich platelet thrombi in the liver cause sinusoidal obstruction syndrome following oxaliplatin-based chemotherapy. PLoS ONE 10(11):e0143136. https://doi.org/10.1371/journal.pone.0143136
Terraube V, O’Donnell JS, Jenkins PV (2010) Factor VIII and von Willebrand factor interaction: biological, clinical and therapeutic importance. Haemophilia 16(1):3–13
Lenting PJ, Casari C, Christophe OD, Denis CV (2012) von Willebrand factor: the old, the new and the unknown. J Thromb Haemost 10(12):2428–2437
Starke RD, Ferraro F, Paschalaki KE, Dryden NH, McKinnon TA, Sutton RE, Payne EM, Haskard DO, Hughes AD, Cutler DF, Laffan MA, Randi AM (2011) Endothelial von Willebrand factor regulates angiogenesis. Blood 117(3):1071–1080
Gritti G, Cortelezzi A, Bucciarelli P, Rezzonico F, Lonati S, LaMarca S et al (2011) Circulating and progenitor endothelial cells are abnormal in patients with different types of von Willebrand disease and correlate with markers of angiogenesis. Am J Hematol 86(3):650–656
Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, Colman H, Chakravarti A, Pugh S, Won M, Jeraj R, Brown PD, Jaeckle KA, Schiff D, Stieber VW, Brachman DG, Werner-Wasik M, Tremont-Lukats IW, Sulman EP, Aldape KD, Curran WJ Jr, Mehta MP (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370(8):699–708
Ay C, Dunkler D, Pirker R, Thaler J, Quehenberger P, Wagner O, Zielinski C, Pabinger I (2012) HighD-dimer levels are associated with poor prognosis in cancer patients. Haematologica 97(8):1158–1164
Reitter EM, Kaider A, Ay C, Quehenberger P, Marosi C, Zielinski C, Pabinger I (2016) Longitudinal analysis of hemostasis biomarkers in cancer patients during antitumor treatment. J Thromb Haemost 14(2):294–305
Falanga A, Panova-Noeva M, Russo L (2009) Procoagulant mechanisms in tumour cells. Best Pract Res Clin Haematol 22:49–60
Lyman GH, Khorana AA (2009) Cancer, clots and consensus: new understanding of an old problem. J Clin Oncol 27(29):4821–4826
Funding
Associazione Italiana Tumori Cerebrali (AITC) supported this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Pace, A., Mandoj, C., Antenucci, A. et al. A predictive value of von Willebrand factor for early response to Bevacizumab therapy in recurrent glioma. J Neurooncol 138, 527–535 (2018). https://doi.org/10.1007/s11060-018-2820-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-2820-x