Abstract
Central nervous system (CNS) tumors are a leading cause of death in pediatric oncology. New drugs are desperately needed to improve survival. We evaluated the outcome of children and adolescents with CNS tumors participating in phase I trials within the Innovative Therapies for Children with Cancer (ITCC) consortium. Patients with solid tumors aged < 18 years at enrollment in their first dose-finding trial between 2000 and 2014 at eight ITCC centers were included retrospectively. Survival was evaluated using univariate/multivariate analyses. Overall, 114 patients were included (109 evaluable for efficacy). Median age was 10.2 years (range 1.0–17.9). Main diagnoses included: medulloblastoma/primitive neuroectodermal tumors (32.5%) and high-grade gliomas (23.7%). Complete/partial responses (CR/PR) were reported in 7.3% patients and stable disease (SD) in 23.9%. Performance status of 90–100%, school/work attendance, normal ALT/AST and CR/PR/SD correlated with better overall survival (OS) in the univariate analysis. No variables assessable at screening/enrollment were associated with OS in the multivariate analysis. Five patients (4.5%) were discontinued from study due to toxicity. No toxic deaths occurred. Median OS was 11.9 months with CR/PR, 14.5 months with SD and 3.7 months with progressive disease (p < 0.001). The enrollment of children and adolescents with CNS tumors in phase I trials is feasible, safe and offers potential benefit for the patients. Sustained disease stabilization has a promising role as a marker of anti-tumor activity in children with CNS tumors participating in phase I trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 16–20% of the cancers diagnosed in children aged 0–14 years in Europe are central nervous system (CNS) tumors [1]. CNS tumors constitute a leading cause of cancer-related death in children in Europe, the United States and Canada, with 5-year survival rates of 57–72% [1, 2]. Hence, there is an unmet need for novel strategies to improve survival outcomes. Dose-finding trials (phase I and seamless phase I/II trials) are crucial in the evaluation of novel anti-cancer agents for children, since these studies determine the Recommended Phase II Dose for a given drug. However, patients with CNS tumors are sometimes excluded from these trials due to doubts about drug penetration across the blood–brain barrier and/or concerns raised by a history of seizures, corticosteroid requirements and risk of certain neurologic complications, such as raised intracranial pressure, CNS bleeding or spinal cord compression [3]. Nonetheless, dose-finding trials are increasingly being incorporated at earlier time points of treatment-failure for children with advanced solid tumors [4] and there are initiatives to identify prospectively pediatric and adult patients with CNS tumors who might be future candidates for future phase I and phase II studies (NCT00009035). A better understanding of the current landscape of pediatric patients with CNS tumors treated in phase I trials across Europe will contribute to optimizing recruitment and maximizing the efficiency of future phase I trials.
Our main objective was to evaluate the survival outcomes of children and adolescents with CNS tumors enrolled in phase I trials within the Innovative Therapies for Children with Cancer (ITCC) European consortium. In addition, we assessed potential prognostic factors of overall survival (OS) at study entry and tested two predictive scores previously validated in adult cancer patients: the Royal Marsden Hospital (RMH) score and the MD Anderson Cancer Center (MDACC) score [5,6,7].
Patients and methods
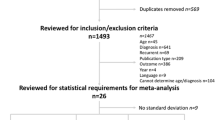
The present study is a post-hoc analysis of the patients with CNS tumors included in the recently published larger ITCC study evaluating prognostic factors of OS in children and adolescents aged < 18 years at enrollment in their first dose-finding trial [8]. Patients were enrolled between 1st January 2000 and 31st December 2014 across eight European centers. All phase I trials had been approved by local institutional review boards. Informed consent by parents/legal guardians and patients had been obtained for participation to the corresponding trial.
Only patients who had completed trial screening and had received at least one dose of the study drug were included in the analysis. All diagnoses of refractory or recurrent CNS tumors were eligible, except for low grade gliomas. Relevant clinical data at baseline and efficacy outcomes were collected accordingly. Lansky and Karnofsky performance status scales were converted to Eastern Cooperative Oncology Group (ECOG) scale for calculation of the MDACC score as follows: Lansky/Karnofsky of 90–100, 70–80, 50–60 or 30–40% were equivalent to an ECOG of 0, 1, 2 or 3, respectively.
Outcome data were collected as follows: best response was defined according to protocol-specific response assessment criteria from day 1 of cycle 1 (C1D1) until best radiological response (including disease stabilization) at any timepoint or disease progression, whichever occurred earlier; event-free survival (EFS) was defined from C1D1 until disease progression on trial, death or study discontinuation, whichever occurred earlier; OS was measured from C1D1 until death or last follow-up. Patients who were still participating in the trial at the time of data collection were censored at last follow-up for calculation of the EFS and OS. Early mortality rates were also calculated at 30 and 90 days from C1D1. If patients had been taken off study for reasons other than disease progression, this information was collected where available, as well as the end of study date. In addition, the RMH and MDACC scores were calculated for patients with data available in all score items (score calculation was made accounting for 1 point per item). These included albumin < 35 g/L, lactate dehydrogenase (LDH) above the upper limit of normal (ULN) and the presence of ≥ 3 metastatic sites, for the RMH score [5, 6]; and the aforementioned RMH score items plus gastrointestinal tumor type and Eastern Cooperative Oncology Group (ECOG) performance status ≥ 1, for the MDACC score [7].
Descriptive statistics were used to present patients’ characteristics. Categorical data were compared using the Chi-squared test. Survival curves were estimated by the Kaplan–Meier method. Univariate log-rank test was used to compare survival distributions according to 24 clinical parameters. Multivariate Cox regression analysis was performed with those variables identifiable at study entry that correlated with survival in the univariate analysis. P values < 0.05 were considered statistically significant. Statistical analyses were conducted with SPSS® version 16.0.
Results
Baseline patient characteristics
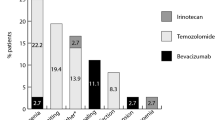
Overall, out of a cohort of 248 patients with relapsed/refractory solid tumours treated within their first phase I trial between 2000 and 2014, 114 patients (46%) had CNS tumors (Table 1) and were treated across 16 dose-finding trials (Suppl Table 1). The median age of patients with CNS tumors was 10.2 years (range 1–17.9) and male to female ratio was 1.15:1. The most frequent diagnoses were medulloblastoma/primitive neuroectodermal tumor (PNET), high grade glioma and diffuse intrinsic pontine glioma (DIPG) in 32.5, 23.7 and 17.5% of cases, respectively. Approximately half of the patients (48.2%) had metastatic disease at study entry. The patients had received a median of one line of chemotherapy (range 0–7) prior to enrollment. Fifteen patients (13.1%), including DIPG (n = 9), ependymoma (n = 4), high grade glioma (n = 1) and neurosarcoma (n = 1), had not received any chemotherapy at study entry. Previous surgical resection had been done in 76% cases and prior radiotherapy in 93%. The majority of patients (67.5%) were treated in trials with single targeted agents (Table 1).
Response rate and time to progression
Out of 12 patients (4.8%) not evaluable for response in the whole cohort (248 patients), 5 were diagnosed with CNS tumors and 7 with extra-CNS tumors. Overall, 109 patients with CNS tumors (95.6%) were evaluable for response. Best response in evaluable patients included complete/partial response (CR/PR) in 7.3%, stable disease (SD) in 23.9% and progressive disease (PD) in 68.8% (Table 2). CR occurred in patients diagnosed with medulloblastoma/PNET (n = 2) and high grade glioma (n = 1); and PR in patients with high grade glioma (n = 3), medulloblastoma/PNET (n = 1) and atypical teratoid rhabdoid tumor (n = 1). The clinical benefit ratio (CR + PR + SD) was 31.2%. Overall, 88% of patients with CR/PR (n = 7/8) and 50% of those with SD (n = 13/26) stayed on trial for ≥ 4 months. The median EFS for the CNS cohort was 1.8 months (95% CI 1.6–2.0).
Additionally, there were no statistically significant differences between the clinical benefit ratio and the rate of PD in the first evaluation of patients with CNS tumors versus those with extra-CNS tumors (data not shown; Chi square 1.4, p = 0.235).
Prognostic factors of overall survival and adult predictive scores
The median follow-up from C1D1 for the CNS cohort was 4.9 months (range 0.2–96). The median OS of patients with CNS tumors was 5.4 months (95% CI 3.8–7.0) versus 7.1 months (95% CI 5.5–8.7) in patients with extra-CNS tumors (log-rank, p = 0.301), Fig. 1a. Eleven patients with CNS tumors (9.6%; 95% CI 4.2–15.0) died within 30 days of C1D1; and 37 patients (32.5%; 95% CI 23.9–41.1) died within 90 days of C1D1. Among 14 patients discontinued from the trial due to toxicity in the whole cohort (i.e. 248 patients), only 5 (36%) were diagnosed with CNS tumors. No drug-related deaths were reported.
Kaplan–Meier curves of overall survival according to tumor location (a): CNS Vs extra-CNS, N = 248 patients (114 CNS Vs 134 extra-CNS); and radiological response (b) as per response evaluation criteria in solid tumors (RECIST), n = 43 patients (complete/partial response = 3; stable disease = 13; progressive disease = 27)
In the univariate analysis (log-rank test), factors significantly associated with improved OS included: performance status 90–100%, school/work attendance, alanine aminotransferase (ALT) or aspartate aminotransferase (AST) within normal ranges, and CR/PR or SD (Table 2).
Objective response and disease stabilization in patients with CNS tumors were associated with improved OS regardless of the response criteria applied in each case (Table 2). Additionally, objective response and disease stabilization also correlated with improved OS in the subset of patients who had been evaluated for efficacy according to RECIST guidelines (Table 3; Fig. 1b).
Response to treatment was excluded from the multivariate analysis (Cox regression), because this variable cannot be determined at enrollment and therefore does not constitute a prognostic factor assessable at baseline. No clinical variables were significantly associated with OS in the multivariate analysis, although performance status and school/work attendance were close to the 95% significance level: p = 0.059 and p = 0.063, respectively (Table 2).
The RMH and MDACC scores were calculated in 59 (51.8%) and 57 (50%) patients with all items, respectively. None of them correlated with OS in the univariate analysis (Table 2; Fig. 2).
Discussion
Despite advances in the understanding of the molecular biology and improvements in therapy for children with CNS tumors, treatment options for relapsed CNS tumors are generally limited and survival outcomes across tumor types are still modest. More novel therapies are therefore still needed for patients with recurrent/refractory CNS tumors. The fact that nearly half of all patients recruited to ITCC pediatric phase I trials within this time period were children with CNS tumors reflects this high medical need [8], as well as the feasibility of enrolling these patients in pediatric phase I trials. This is in stark contrast with the population of adults with CNS tumors, historically excluded from phase I trials due to their poor prognosis, concomitant drug interactions, concerns about excessive toxicities and limited efficacy [3]. For instance, in a multi-centric review of 2182 adult cancer patients participating in phase I trials, < 7% of patients had primary CNS tumors. Likewise, in a large institutional cohort of 1181 adults with cancer enrolled in phase I trials, only 12 (1%) had primary CNS tumors [7, 9]. Notwithstanding, adults with primary CNS tumors enrolled in phase I trials still seem to have a survival advantage compared to those not enrolled [3]. Since there is a paucity of data in children and adolescents with CNS tumors for reference, we assessed the outcomes of 114 children and adolescents with CNS tumors who participated in a dose-finding trial. To our knowledge, this is the largest reported series of its kind to date.
Patients with CNS tumors represented 46% of the population enrolled in dose-finding trials across 8 large pediatric oncology units in 4 European countries over a period of 15 years [8]. This is relatively similar to that reported in a former review of pediatric phase I trials in the United States conducted between 1992 and 2005, where 35% of the patients had brain tumors [10]. These findings highlight that, despite certain features potentially compromising the eligibility of children and adolescents with CNS tumors -such as uncertainty about drug penetration into the CNS and risk of specific adverse events (e.g. seizures, intracranial hypertension, etc)-, such patients constitute a substantial proportion of the population recruited to paediatric phase I trials.
The age and gender distributions in our sample are similar to those previously reported in two European centers reviewing the participation in pediatric phase I and phase II trials, with a median age of 10–12 years and a mild predominance of male patients [11, 12].
In our study approximately one-third of the patients who discontinued the trial due to toxicity were diagnosed with a CNS tumor and no toxic deaths were reported. Dose limiting toxicities (DLT) were not specifically reported. However, prior reports from Gustave Roussy and the Royal Marsden Hospital have shown a rate of DLTs of 12–13% in pediatric phase I trials [11, 12]: out of 28 patients experiencing DLTs, 15 (54%) were diagnosed with CNS tumors [personal communication from authors]. Additionally, there were 10 patients not evaluable for DLTs altogether; 7 of whom had a diagnosis of a CNS tumor and developed disease progression over the DLT-evaluation period [personal communication from authors]. Overall trial participation can be deemed safe for CNS tumor patients compared to those with extra-CNS tumors, although more specific criteria to identify those more likely to derive benefit from the study drug are still needed.
As regards efficacy, approximately one-third of the patients with CNS tumors enrolled in a phase I trial derived some clinical benefit, as defined by imaging criteria (CR + PR + SD). Patients assessed according to RECIST v1.0 or v1.1 were analyzed jointly for study purposes. This was based on evidence from a cohort of > 6500 adults with metastatic cancer evaluated according to both versions. The study showed that the reduction in the number target lesions, as per v1.1, did not affect the overall response rate and only minimally affected the assessment of progression-free survival [13], thereby simplifying the measurements, but without reducing the prognostic value of the response criteria. The response rates observed in our pediatric and adolescent cohort are comparable to those reported in previous reviews of pediatric phase I trials, showing objective responses in 3.8–9.6% of cases and disease stabilization in 17–37.7% [10,11,12, 14]. Likewise, the median EFS and OS in our cohort are similar to those previously reported in pediatric phase I trials: 1.3–2.8 months for EFS and 3.6–8.5 months for OS [10,11,12, 15]. However, these studies did not analyze efficacy in the subset of patients with CNS tumors separately. Hence, our findings could serve as a suitable reference for evaluation of early signs of activity in children and adolescents with CNS tumors in future phase I trials.
One of the main issues in drug development for children with CNS tumors is the concern about drug penetration across the blood–brain barrier, either due to the intrinsic properties of the molecule or due to disruption of the blood–brain barrier by the tumor itself. We could not find any significant differences between the response rates of children with CNS and extra-CNS tumors. Thus it can be assumed that the drugs tested in each group were reaching the target in a comparable way and drug penetration across the blood–brain barrier was not putting patients with CNS tumors in disadvantage compared to those with extra-CNS tumors.
In terms of survival outcomes, there were no differences in the median OS of patients diagnosed with CNS tumors compared to those with extra-CNS tumors. Furthermore, as is to be expected, we observed that response correlated with survival in the univariate analysis. This endpoint was excluded from the multivariate analysis, because our objective was to determine prognostic factors identifiable at study entry and response cannot be assessed at the time of enrolment. Therefore caution should be exercised when generalizing these results. In adults enrolled in phase I trials, a near-linear relationship between tumor shrinkage assessed by RECIST and OS has been demonstrable [16]. In pediatric phase I trials, we have previously shown that greater tumor shrinkage, assessed by RECIST, also correlates with a more prolonged response and increased OS [17].
Intuitively the underlying diagnosis might also be a relevant prognostic factor. However, given the heterogeneous population and the limited number of patients in each diagnostic category, this variable was excluded from the uni/multivariate analyses.
Additionally, and importantly, in agreement with previous reports [8, 17], in our cohort those patients with CNS tumors who achieved disease stabilization had survival rates comparable to those with objective responses. These findings suggest that novel targeted therapies, even if they cannot induce significant tumor shrinkage, may halt tumor growth sufficiently as to confer a survival advantage for some patients; whereas historically only objective responses have been considered a sign of anti-tumour activity in early phase trials. Although this observation should be validated in prospective phase II studies dedicated to patients with specific types of CNS tumors, our study raises the hypothesis that sustained disease stabilization in pediatric patients with CNS tumors can be a marker of anti-tumor activity in phase I trials of novel agents.
As regards other prognostic factors, we have previously shown that some indicators of the patient´s well-being, such as performance status and school/work attendance at enrollment, were associated with OS in pediatric phase I trials [8]. In the subset of patients with CNS tumors, performance status ≤ 80% and no school/work attendance at enrollment were associated with worse OS in the univariate analysis and there was a trend towards poorer OS in the multivariate analysis. Conversely, the association of elevated ALT and AST with worse OS in the univariate analysis might be anecdotal and should be regarded with caution. Bearing in mind that these elevations were mild, because patients could still be enrolled in their respective trials and the maximum transaminase values permitted for inclusion are normally up to 1.5–2.5 times the ULN, it could be argued that this is a random finding attributed to multiple comparisons. In addition, two clinical scores previously validated in adult cancer patients as good predictors of survival were assessed in this patient population: the RMH score and the MDACC score [5,6,7]. Neither score was predictive of survival in the limited subset of patients within our cohort. Likewise, the RMH score did not correlate with survival in 55 adults with CNS tumors enrolled in phase I trials [3]. These findings illustrate the lack of reliable indicators of OS and highlight the need to identify prognostic factors specific for children and adolescents with CNS tumors to optimize patient selection for future phase I trials.
Limitations of this study to be acknowledged include its retrospective nature, the use of different response assessment criteria depending on the trial and the lack of a validation cohort.
In summary, this study is the largest review of children and adolescents with CNS tumors participating in a dose-finding trial and is representative of the European drug development landscape over the past decade. Firstly, CNS tumors represented nearly half of the diagnoses of children enrolled in phase I trials. Secondly, up to one-third of the patients with CNS tumors derived clinical benefit, as defined by imaging criteria (CR + PR + SD), from enrollment in the phase I trial and response/stabilization was associated with improved OS. Interestingly, survival rates in patients with disease stabilization were comparable to those with objective responses. Therefore sustained disease stabilization showed a promising role as a marker of anti-tumor activity in children with CNS tumors participating in phase I trials. These response rates and survival outcomes will serve as a reference for future phase I trials for children and adolescents with CNS tumors.
Finally this study shows that entering children and adolescents with CNS tumors in phase I trials is feasible, safe and offers potential benefit for the patients; supports the inclusion of children and adolescents with CNS tumours in early phase studies; and may suggest that there could be further gains for them should early clinical trials designed for patients with CNS tumours be developed with specific consideration to e.g. targets of major interest and blood brain barrier penetrability by the agent being evaluated.
References
Gatta G, Botta L, Rossi S et al (2014) Childhood cancer survival in Europe 1999–2007: results of EUROCARE-5–a population-based study. Lancet Oncol 15:35–47
Johnson KJ, Cullen J, Barnholtz-Sloan JS et al (2014) Childhood brain tumor epidemiology: a brain tumor epidemiology consortium review. Cancer Epidemiol Biomark Prev 23:2716–2736
Coleman N, Michalarea V, Alken S et al (2016) Safety, efficacy and survival of patients (pts) with primary CNS tumors in phase 1 (Ph1) trials: a 12-year single institution experience. J Clin Oncol 34, 2016 (suppl; abstr 2043)
Bautista F, Gallego S, Cañete A et al (2016) Landscape of early clinical trials for childhood and adolescence cancer in Spain. Clin Transl Oncol 18:708–713
Arkenau H-T, Olmos D, Ang JE et al (2008) Clinical outcome and prognostic factors for patients treated within the context of a phase I study: the Royal Marsden Hospital experience. Br J Cancer 98:1029–1033
Arkenau H-T, Barriuso J, Olmos D et al (2009) Prospective validation of a prognostic score to improve patient selection for oncology phase I trials. J Clin Oncol 27:2692–2696
Wheler J, Tsimberidou AM, Hong D et al (2012) Survival of 1,181 patients in a phase I clinic: the MD Anderson Clinical Center for targeted therapy experience. Clin Cancer Res 18:2922–2929
Carceller F, Bautista FJ, Jiménez I et al (2016) Prognostic factors of overall survival in children and adolescents enrolled in dose-finding trials in Europe: an Innovative Therapies for Children with Cancer study. Eur J Cancer 67:130–140
Olmos D, A’Hern RP, Marsoni S et al (2012) Patient selection for oncology phase I trials: a multi-institutional study of prognostic factors. J Clin Oncol 30:996–1004
Kim A, Fox E, Warren K et al (2008) Characteristics and outcome of pediatric patients enrolled in phase I oncology trials. Oncologist 13:679–689
Bautista F, Di Giannatale A, Dias-Gastellier N et al (2015) Patients in pediatric phase I and early phase II clinical oncology trials at Gustave Roussy: a 13-year center experience. J Pediatr Hematol Oncol 37:e102–e110
Morgenstern DA, Hargrave D, Marshall LV et al (2014) Toxicity and outcome of children and adolescents participating in phase I/II trials of novel anticancer drugs: the Royal Marsden experience. J Pediatr Hematol Oncol 36:218–223
Bogaerts J, Ford R, Sargent D et al (2009) Individual patient data analysis to assess modifications to the RECIST criteria. Eur J Cancer 45:248–260
Lee DP, Skolnik JM, Adamson PC (2005) Pediatric phase I trials in oncology: an analysis of study conduct efficiency. J Clin Oncol 23:8431–8441
Corrales-Medina FF, Herzog C, Hess K et al (2014) Clinical characteristics and outcomes of pediatric oncology patients with aggressive biology enrolled in phase I clinical trials designed for adults: the university of Texas MD anderson cancer center experience. Oncoscience 1:522–530
Jain RK, Lee JJ, Ng C et al (2012) Change in tumor size by RECIST correlates linearly with overall survival in phase I oncology studies. J Clin Oncol 30:2684–2690
Carceller F, Bautista FJ, Fowkes LA et al (2016) Response assessment in paediatric phase I trials according to RECIST guidelines: survival outcomes, patterns of progression and relevance of changes in tumour measurements. Pediatr Blood Cancer 63:1400–1406
Acknowledgements
Ms Carole Lecinse, Innovative Therapies for Children with Cancer (ITCC) and Ms Gynette Cook, The Royal Marsden NHS Foundation Trust. This work was supported by the ITCC infrastructure. Additionally, F.C. holds a senior fellowship funded by the National Institute for Health Research Biomedical Research Centre (BRC) at the Royal Marsden and by the Sohn Foundation. I.J. holds a fellowship funded by the Nelia et Amadeo Barletta Foundation. D.H. is supported by the BRC at Great Ormond Street Hospital for Children NHS Foundation Trust and University College London. A.D.J.P. was supported by Cancer Research UK (CRUK): programme grant C1178/A10294 - Chair in Pediatric Oncology. L.Mo. is funded by the Juan Rodés senior fellowship from Instituto de Salud Carlos III. L.V.M. is funded by the Oak Foundation (Grant OCay-04-169).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
These results were presented in part at the International Symposium of Pediatric Neuro-Oncology (ISPNO) held in June 2016. I.J. acknowledges travel/accommodation expenses from MSD. F.D. has had a consulting role for Novartis and travel/accommodation expenses from Novartis. M.C. has had a consulting role for Novartis, Boehringer and Roche. D.H. has had a consulting role for Roche, Astra Zeneca, Boehringer, GSK and Thrombogenics, received honoraria from Roche, Astra Zeneca and Boehringer, and travel/accommodation expenses from Roche, Astra Zeneca, Boehringer, GSK, Thrombogenics and Merck. L.V.M. has had a consulting role for Astra Zeneca, GSK, Novartis and Eli Lilly. A.D.J.P. has received honoraria from Astra Zeneca, Boehringer and Novartis. L.Mo. has had a consulting role for Novartis, Astra Zeneca and Roche. All other authors declare no conflicts of interest to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Carceller, F., Bautista, F., Jiménez, I. et al. Outcome of children and adolescents with central nervous system tumors in phase I trials. J Neurooncol 137, 83–92 (2018). https://doi.org/10.1007/s11060-017-2698-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2698-z