Abstract
The surgical risk factors and neuro-imaging characteristics associated with cerebellar mutism (CM) remain unclear and require further investigation. Therefore, we aimed to examine surgical and MRI findings associated with CM in children following posterior fossa tumor resection. Using our data registry, we retrospectively collected data from pediatric patients who acquired CM and were matched based on age and pathology type with individuals who did not acquire CM after posterior fossa surgery. The strength of association between surgical and MRI variables and CM were examined using odds ratios (ORs) and corresponding 95% confidence intervals (CIs). A total of 22 patients (11 with and 11 without CM) were included. Medulloblastoma was the most common pathology among CM patients (91%); the remaining 9% were diagnosed with a pilocytic astrocytoma. Tumor attachment to the floor of the fourth ventricle (OR 6; 95% CI 0.7–276), calcification/hemosiderin deposition (OR 7; 95% CI 0.9–315.5), and post-operative peri-ventricular ischemia on MRI (OR 5; 95% CI 0.5–236.5) were found to have the highest measures of association with CM. Our results may suggest that tumor attachment to the floor of the fourth ventricle, pathological calcification, and post-operative ischemia have a relatively higher prevalence in patients with CM. Collectively, our work calls for a larger multi-institutional cohort study of CM patients to encourage further investigation of the determinants and management of CM in order to potentially minimize its development and predict onset.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cerebellar mutism (CM) is a condition characterized by a significant lack of speech or loss of speech in children following posterior fossa (PF) surgery [1]. The definition of CM in relation to Posterior Fossa Syndrome (PFS) is not consolidated in the literature [1]. We chose to define CM as a condition that is part of a larger constellation of symptoms which often involve ataxia, mood changes, and impaired swallowing and vision [1,2,3,4]. CM is acquired within 1 week following PF surgery and has a limited duration of weeks to months [5]. However, those affected may experience long-term effects including dysarthria, altered prosody of speech, and neurological imparments [3, 5].
The biological origin of CM remains largely unclear and there are no standardized treatments. The incidence of CM in children ranges from 8 to 39% of children following PF surgery [6]. The risk of CM has been reported to increase based on medulloblastoma tumor type, or brainstem or vermis invasion [1]. The condition may be triggered by the disruption of the dentato-thalamo-cortical (DTC) pathway during surgery, but an evidence-based proof of CM’s etiology has not been described [5, 6].
We sought to determine whether there are any surgical or MRI markers associated with CM in children after PF surgery for tumor resection. We aim to identify trends in the anatomical location of tumor at presentation, MRI features, and the amount of residual tumor in order to understand the pathophysiological factors leading to CM.
Methods
Following local ethics board approval, we conducted a retrospective cohort-comparative study among children diagnosed with PF brain tumors between 2003 and 2015 at McMaster University Medical Centre (MUMC), a pediatric and academic hospital in Ontario, Canada. Data were extracted from the Pediatric Brain Tumor Study Group (PBTSG) database, which compiles information from patient charts and McMaster’s Medical Records system. The database was compiled in 2015 to document the brain tumors of children up to 18 years old. Patients who presented to MUMC prior to 2002 were not included due to a lack of accessible MRI data and accessible physician’s notes. Double data entry was performed on 5% of the cases to verify the accuracy of data entry.
The senior author’s anecdotal clinical experiences noted that children who developed CM post-operatively often had notable intraoperative events (i.e. disruption of the floor of the fourth ventricle leading to changes in vital signs). This led to our hypothesis that significant intraoperative events may lead to post-operative MRI changes which may be predictive of CM. Study protocol was created a-priori; the patient population was defined in advance. CM was defined as a significant lack of speech or loss of speech acquired within 3 days post-operatively. The patients who acquired CM post-operatively (after their first surgery) were matched with patients who did not acquire this condition after the surgical removal of their brain tumor. Cases and controls were matched based on age and tumor type as closely as possible and the review was blinded to outcome, allowing the matching to be performed in an unbiased manner. When there were multiple controls to be matched for one case, one was randomly chosen. All patients included had tumors in the midline or cerebellar hemisphere region. The cases and comparisons extracted for this study were re-examined, and double data entry was performed for 100% of the study’s patients.
In addition to the data collected from the PBTSG database, pre-operative and post-operative MRIs of CM patients and their comparisons were reviewed by a single blinded neuro-radiologist. Variables recorded from the pre-operative scans included anatomical tumor location, size of lesion, MRI appearance, T1 turbo spin echo signal, T2 turbo spin echo signal, restricted diffusion, FLAIR signal, presence of metastasis, pattern of enhancement, leptomeningeal enhancement, calcification, necrosis, hydrocephalus, and vasogenic edema. Post-operative variables included residual tumor on MRI, extent of surgical resection, and peri-ventricular infarcts or bleeds around the fourth ventricle. A gross total resection (GTR) was defined as a residual tumor of less than 1.5 cubic centimeters [7]. Data were compared with original MRI scan reports in order to ensure consistency and accuracy, and the anatomical location variable was checked against operative reports. Variables were selected based upon expert opinion and a literature review; the study sought to include variables which had not been previously linked to the occurrence of CM. For data analysis, we reported the mean age with standard deviation (SD) and ratio of male to female in matched cases and comparisons. Odds ratios (OR) were reported with the corresponding 95% confidence interval (CI) to assess the strength of association between CM cases and MRI markers compared to matched comparisons.
Results
From the PBTSG database of 108 posterior fossa cases, 11 children who presented with CM after the resection of their tumor were identified (prevalence of CM among PF tumors = 10%). Eleven CM patients were matched with 11 comparisons from the PBTSG database, who also underwent PF surgery but did not acquire CM (Table 1). The mean age distribution of the CM cases was 7.43 years (SD 2.4), while the mean age of the matched comparisons was 7.03 years (SD 3.8). The tumor pathology in 10 of 11 CM patients was medulloblastoma, and the remaining one patient had a pilocytic astrocytoma; these tumor types were matched accordingly in the comparison group. Although patients were not matched based on sex, 3 of the 11 CM cases were female while 4 of the 11 comparison patients were female.
Surgical and MRI factors
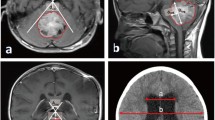
Based on pre-operative MRI scanning, the mean tumor size in the CM group was 3.73 cm compared to 4.64 cm in the comparison group. Table 2 depicts the number of cases and comparisons that were positive for each variable. Certain study participants were omitted from analysis of calcification and infarct variables due to an absence of gradient imaging or diffusion-weighted imaging. While the results did not reach statistical significance, Table 2 demonstrates the strength of association between MRI characteristics and CM (OR and 95% CI) for each variable. Of the listed factors, tumor attachment to the floor of the fourth ventricle (OR 6; 95% CI 0.7–276), calcification or hemosiderin deposits (OR 7; 95% CI 0.9–315.5), necrosis (OR 3; 95% CI 0.2–157.5), moderate/high hydrocephalus (OR 3; 95% CI 0.2–157.5), post-operative infarcts and bleeds (OR 5; 95% CI 0.5–236.5) and gross total surgical resection (OR 3; 95% CI 0.5–30.4) had positive association with CM. Tumor attached to floor of 4th ventricle (Fig. 1 A—a, b), calcification/hemosiderin deposits (Fig. 1 B—a, b), necrosis, moderate to severe hydrocephalus, gross total resection and post-operative infarcts (Fig. 1 C—a–d) had a higher incidence in the CM group. To validate anecdotal expert opinion of the intraoperative events thought to be associated with CM, we have included qualitative evidence, which have captured these events to occur more frequently in the CM group than the comparison group (please refer to Table 3). Vasogenic edema (OR 0.4; 95% CI 0.04–2.4), leptomeningeal enhancement (OR 0.3; 95% CI 0.01–4.1) and metastasis in head or spine (OR 0.6; 95% CI 0.05–5.8) were more prevalent in the comparison group.
A Pre-operative fourth ventricle floor attachment. Axial flair imaging was used to determine whether tumor was arising from the floor of the fourth ventricle. Figure 1 A (a) depicts an example of tumor attached and centered in the floor of the fourth ventricle in a CM case, which was present in 10 of 11 CM cases, and present in 5 of 11 non-cases. Figure 1 A (b) is an example of tumor not attached to the floor of the fourth ventricle in a control case, as the lesion is arising within the parenchyma of the right cerebellar hemisphere in the dentate nucleus area. B Pre-operative calcification and hemosiderin deposits. Susceptibility weighted imaging was used to determine if there was calcification in the tumor. Figure 1 B (a) depicts multiple foci of abnormal magnetic susceptibility within the tumor in a CM case, representing either micro-calcifications or hemosiderin deposits. This was present in 7 of 10 CM patients, and 2 of 11 non-cases. Figure 1 B (b) is an example of a tumor without evidence of areas with abnormal magnetic susceptibility in a control case. C Post-operative infarcts/contusions. Diffusion weighted imaging was used to determine whether the cases and comparisons showed infarcts post-operatively. Figure 1 C (a) is an example of a b1000 image used alongside a Fig. 1C (b) ADC map to determine a post-operative infarct/contusion. Figure 1 C (c) is a b1000 image used in conjunction with a susceptibility weighted image (Fig. 1 C (d)) to determine that there was no visible evidence of infarct but only blood products adjacent to the surgical bed walls. 8 of 11 CM cases had DWI infarcts in their immediate post-operative scan in comparison to 4 of 9 non-cases
Discussion
CM is a condition which occurs post-operatively, following the removal of a PF tumor in children. This condition may have an iatrogenic cause, as the disruption of the dentato-thalamo-cortical (DTC) pathway during surgery has been hypothesized as a potential trigger [1, 5]. Avula et al. reported a significant association between CM and diffusion abnormalities in the dentate nucleus, superior cerebellar peduncle, and mesencephalic tegmentum immediately post-operatively [8]. A recent case-control study employing diffusion tensor imaging noted that CM patients showed white matter changes in the superior cerebellar peduncle; these changes remained evident months following the surgery [9]. Perreault et al. evaluated time-dependent changes to the DTC pathway following posterior fossa tumor resection in children and found that post-operatively, the dentate nuclei underwent progressive atrophy and the DTC pathway showed continuous structural changes [10]. While certain diffusion tensor scans of CM patients have shown DTC disruption, some of these scans took place before, or years after surgery and thus cannot be associated with CM [5]. There was no temporal association between MRI scans showing DTC disruption and the patient’s CM symptoms. We aimed to determine whether there are any surgical or MRI factors associated with CM in order to improve the understanding of CM’s pathophysiology. Post-operative infarcts, calcification, and disruption of the floor of the fourth ventricle may be implicated in the development of CM rather than attributing this to DTC pathway disruption alone. If the presence of calcification is indeed associated with cerebellar mutism, this could serve to warn surgeons that there may be an increased likelihood of CM.
The majority (75–90%) of medulloblastomas arise from the roof of the fourth ventricle [11]. The higher prevalence of floor of the fourth ventricle attachment in CM patients may suggest that the disruption of the floor of the fourth ventricle during surgery may result in CM. A recent study examining the molecular subtypes of medulloblastoma found that the sonic hedgehog tumor group had a lower incidence of CM in comparison to wingless, Group 3, and Group 4 [12]. The sonic hedgehog subgroup does not tend to arise from the floor of the fourth ventricle, a trait more predominant in Groups 3 and 4 [13]. This supports the hypothesis that tumor attachment to the floor of the fourth ventricle is implicated in the development of cerebellar mutism. If disruption of this region is significantly associated with CM, then surgeons could take a less invasive approach while removing tumor from the floor of the ventricle, favoring a near-total resection over a GTR [14]. In addition, there could be an attempt to use the pre-operative imaging to predict outcome if the tumor is involving the floor of the fourth ventricle. Thompson et al. suggest that the influence of GTR on medulloblastoma survival rates is not as significant as previously suggested [14]. Interestingly, the large majority of the CM patients in our study were diagnosed with medulloblastoma [1, 3]. Outcomes and goals of gross-total resection and risk of CM should be considered when tumors such as medulloblastoma involve the floor of fourth ventricle [14]. CM’s association with the floor of the fourth ventricle may alter a surgeon’s approach but further research is required in order to determine the exact cerebellar tract affected, which could detail preventative measures. For every neurosurgeon operating in the proximity of the floor of the fourth ventricle, the result of each surgical movement dynamically changes the next. This pilot study supports our senior surgeon’s intraoperative anecdotal experience that disruption of the floor of the fourth ventricle is associated with post-operative MRI changes in our CM group. Our study serves as a caution for neurosurgeons. If disruption of the floor of the fourth ventricle is associated with CM, surgeons should exercise extreme caution until they have delineated the attachment of the tumour as we have observed a notable discrepancy between pre-operative MRI reports and intraoperative finding of tumour attachment.
Higher grade tumors such as medulloblastoma can be more difficult to resect completely relative to most pilocytic astrocytomas, as pilocytic astrocytomas are often well-delineated [15]. Medulloblastoma tumors can be infiltrative, requiring more dissection of the brain-tumor interface, which may account for the CM occurring post-operatively. The presence of areas with restricted diffusion surrounding the surgical bed post-operatively was higher in the CM group. This may represent areas of contusion or ischemia of the parenchyma, which is likely caused during surgery, and a lack of blood supply in these regions may be the underlying cause CM. The infarcts or contusions were located around the floor of the fourth ventricle, suggesting a relationship between these two variables. Therefore, disruption of the floor of the fourth ventricle may subsequently result in ischemia and thereby may predicate the development of CM.
The variables associated with a lack of CM (vasogenic edema, leptomeningeal enhancement, and metastasis in the head or spine) are factors that may cause a surgeon to avoid a GTR. Therefore, vasogenic edema, leptomeningeal enhancement, and metastasis may be related to the sub-total resection variable, all of which are correlated with a lack of CM.
Strengths and limitations
There are certain limitations to the design of this study, inherent to observational retrospective designs. This study was underpowered to draw a strong conclusion; 95% confidence intervals lacked precision due to the relatively small sample size. Certain patients did not have gradient imaging or diffusion-weighted imaging sequences on their immediate pre-operative and post-operative scans. This resulted in fewer cases and comparisons to be reviewed in the current study. MRI imaging within 48 h pre-operatively and post-operatively were reviewed, but post-operative time of MRI varied between the patients in the study.
The comparative nature of the study is a strength, as the case-comparison model allows for an examination of factors associated with CM. The data registry is another strength of the study as it contains patient data compiled from clinical, surgical and MRI charts and represents the total pediatric brain tumor population at McMaster from 2002 to 2015. Additionally, 5% of this database was double-checked for accuracy. The blinded neuro-radiologist examination is another strength of the current study, as MRI evaluation was not influenced by the knowledge of whether a patient had CM or not. The reports of this neuro-radiologist were also double-checked with the previous MRI reports for data accuracy.
Conclusion
Our study explores some of the putative factors leading to CM development. We found that post-operative peri-ventricular infarcts/bleeds, tumor attached to the floor of the fourth ventricle, and calcification were more prevalent in CM cases than in controls. It would be beneficial to undertake a prospective multi-center study in order to adequately address the question. Insights from these findings guides further investigation of the determinants and management of CM in order to potentially minimize its development and predict onset.
References
Reed-Berendt R, Phillips B, Picton S, Chumas P, Warren D, Livingston JH, Hughes E, Morrall M (2014) Cause and outcome of cerebellar mutism: evidence from a systematic review. Childs Nerv Syst 30:375–385. doi:10.1007/s00381-014-2356-0
Di Rocco C, Chieffo D, Frassanito P, Caldarelli M, Massimi L, Tamburrini G (2011) Heralding cerebellar mutism: evidence for pre-surgical language impairment as primary risk factor in posterior fossa surgery. Cerebellum 10:551–562. doi:10.1007/s12311-011-0273-2
Law N, Greenberg M, Bouffet E, Taylor MD, Laughlin S, Strother D, Fryer C, McConnell D, Hukin J, Kaise C, Wang F, Mabbott DJ (2012) Clinical and neuroanatomical predictors of cerebellar mutism syndrome. Neuro-Oncology 14:1294–1303. doi:10.1093/neuonc/nos160
Patay Z (2015) Postoperative posterior fossa syndrome: unraveling the etiology and underlying pathophysiology by using magnetic resonance imaging. Childs Nerv Syst 31(10):1853–1858. doi:10.1007/s00381-015-2796-1
Van Baarsen KM, Grotenhuis JA (2014) The anatomical substrate of cerebellar mutism. Med Hypotheses 82:774–780. doi:10.1016/j.mehy.2014.03.023
Pitsika M, Tsitouras V (2013) Cerebellar mutism. J Neuros-Pediatr 12:604–614. doi:10.3171/2013.8.peds13168
Gajjar A, Sanford RA, Bhargava R et al (1996) Medulloblastoma with brain stem involvement: the impact of gross total resection on outcome. Pediatr Neurosurg 25(4):182–187. doi:10.1159/000121121
Avula S, Kumar R, Pizer B, Pettorini B, Abernethy L, Garlick D, Mallucci C (2015) Diffusion abnormalities on intraoperative magnetic resonance imaging as an early predictor for the risk of posterior fossa syndrome. Neuro-oncology 17(4):614–622. doi:10.1063/neuonc/nou299
McEvoy, S et al (2016) Longitudinal cerebellar diffusion tensor imaging changes in posterior fossa syndrome. Neuroimage Clin 12:582–590. doi:10.1016/j.nicl.2016.09.007
Perreault S, Lober RM, Cheshier S, Partap S, Edwards MS, Yeom KW (2014) Time-dependent structural changes of the dentatothalamic pathway in children treated for posterior fossa tumor. Am J Neuroradiol 35:803–807. doi:10.3174/ajnr.a3735
Plaza M, Borja M, Altman N, Saigal G (2013) Conventional and advanced MRI features of pediatric intracranial tumors: posterior fossa and suprasellar tumors. Am J Roentgenol 200(5):1115–1124. doi:10.2214/AJR.12.9725
Moxon-Emre et al (2016) Intellectual outcome in molecular subgroups of medulloblastoma. J Clin Oncol 34:4161–4170. doi:10.1200/JCO.2016.66.9077
Perreault S et al (2014) MRI surrogates for molecular subgroups of medulloblastoma. Am J Neuroradiol 35(7):1263–1269. doi:10.3174/ajnr.A3990
Thompson E, Hielscher T, Bouffet E et al (2016) Prognostic value of medulloblastoma extent of resection after accounting for molecular subgroup. Lancet Oncol 17:484–495. doi:10.1016/s1470-2045(15)00581-1
Pollack I (2011) Multidisciplinary management of childhood brain tumors: a review of outcomes, recent advances, and challenges. J Neurosurg Pediatr 8:135–148. doi:10.3171/2011.5.PEDS1178
Funding
No funding to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declares that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Sheila Kumari Singh and Nina Stein are co-senior authors.
Rights and permissions
About this article
Cite this article
Sergeant, A., Kameda-Smith, M.M., Manoranjan, B. et al. Analysis of surgical and MRI factors associated with cerebellar mutism. J Neurooncol 133, 539–552 (2017). https://doi.org/10.1007/s11060-017-2462-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2462-4