Abstract
The treatment of medulloblastoma, the most common malignant brain tumor in children, has evolved over the last few decades. The objectives of this paper were to determine the survival of pediatric medulloblastoma in Canada, to determine if there has been an improvement in the survival rates between the years of 1990 and 2009, inclusive, and to determine prognostic factors for survival. All patients under the age of 18 years diagnosed with medulloblastoma from 1990 to 2009, inclusive, in Canada were included. Data collected included date of diagnosis, age at diagnosis, gender, stage, pathology, treatment, recurrence and current status. From these, survival rates were determined. Data were obtained on 628 eligible patients. The overall 5-year survival rate for the study time period was 69.2 ± 3.3 %. The survival rate increased during the interval of 1996–2000, then remained stable; 1990–1994: 60.2 ± 4.3 %; 1995–1999: 73.2 ± 3.5 %; 2000–2004: 68.8 ± 3.7 %; and 2005–2009: 72.1 ± 4.9 %, p = 0.05. Children over 14 years of age had a significantly better overall survival than those age 5–14 and those under 5 (85.7 ± 5.5 % vs 76.1 ± 2.7 % and 60.8 ± 3 % respectively, p = 0.001). Histologic medulloblastoma subtype and M stage of disease did not result in significant differences in survival. Despite changes in approaches to therapy, we demonstrate a steady survival rate for children with medulloblastoma after 1996. In our analyses, age over 14 years was associated with a higher survival rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medulloblastoma is the most common malignant brain tumor in children and accounts for approximately 20 % of all brain tumors in children and adolescents under the age of 18 years [1]. Current therapy includes maximal surgical resection, craniospinal radiation with a boost to the tumor bed, and adjuvant chemotherapy [2]. Using these modalities, the survival is approximately 80 % for patients with standard-risk disease (defined as residual tumor less than 1.5 cm2 and no evidence of disease in the head, spine or cerebrospinal fluid) and 65 % for those with high risk disease [3, 4]. Other factors shown to influence survival include histological subtype, age at diagnosis, and therapy utilized. The majority of publications on survival of medulloblastoma describe results of clinical trials, which have stringent eligibility criteria that necessarily influence the survival data [5–9]. As well, the majority of medulloblastoma studies are for specific age ranges, usually over age 3 or under age 3, and not for the whole population of affected children.
The Canadian Pediatric Brain Tumor Consortium (CPBTC) represents all Canadian pediatric oncology centers. The health care system in Canada is such that any child who is diagnosed with a brain tumor in Canada is treated at one of the institutions of the CPBTC. There is potential that a young adult (i.e. 16 or 17 years old) with medulloblastoma would be treated at an adult center, but this potential is very low given the cooperation between adult and pediatric centers in Canada, such that any person under the age of 18 with a pediatric diagnosis is sent to a pediatric institution. The CPBTC undertook a population-based study of all patients diagnosed with medulloblastoma during the past two decades. The primary objectives of this observational study were to determine the survival rate in children under the age of 18 years diagnosed with medulloblastoma in Canada and to determine if there was any change between each 5-year period of the 20 years surveyed. The secondary objective was to explore the prognostic risk factors for survival.
Methods
This study was designed as a multi-centered, national, retrospective observational study. A questionnaire was developed in order to collect data on Canadian pediatric patients with medulloblastoma. The inclusion criteria for the study were age 18 years or younger with a histologically confirmed diagnosis of medulloblastoma diagnosed in Canada in the years 1990–2009, inclusive. The data collected included date of diagnosis, age at diagnosis, gender, M stage, histologic subtype, treatment received, enrollment on a clinical trial, any recurrence and characteristics of the recurrence, and the status of patient at the time of the survey. Patients who were treated at more than one center were discussed among the centers to determine which center would include the patient in their data to ensure no duplication of data.
The study was approved by the local research ethics boards at each institution prior to completion of the questionnaires. The questionnaire was completed by all 16 Canadian member centers of the CPBTC for all patients meeting inclusion criteria. The data were anonymized at the center at the time of completion of the questionnaire. The completed questionnaires were centrally collected by the principal investigator and the data entered into a database. There was no central review of pathology or radiology for the cases.
Descriptive statistics were compared using Chi square analysis. Overall survival was calculated using Kaplan–Meier analysis. To examine for changes in survival over time, the study period was broken into 4 equal times periods (1990–1994, 1995–1999, 2000–2004 and 2005–2009, inclusive). These time periods reflected the standard Canadian census time periods. The age groupings were divided into under 5 years, 5–14 years and 14–19 years to reflect the statistics collected by Statistics Canada. The 5-year survival rates between groups were compared using log-rank test. Cox proportional hazard regression analysis was used to assess the relationship between different variables and time to death. A p value of <0.05 was considered statistically significant. Statistical calculations were done using SPSS.
Results
There were a total of 628 eligible patients from all 16 Canadian institutions who met all inclusion criteria. The mean age was 5.08 ± 3.3 years. The study population characteristics are summarized in Table 1.
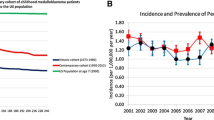
The overall 5-year survival rate was 69.2 ± 3.3 %. To determine if a change in the 5-year survival rate had occurred between 1990 and 2009, the data were broken down into 5 year periods (Table 2). Between the time period 1990–1994 and 1995–1999, the 5-year survival increased and then remained relative stable thereafter. The 2-year survival increased with each subsequent time period, and the 10-year survival increased after 1994 (Table 2).
There were changes in the therapy given during the different time intervals (Table 1). From 1990 to 1999, chemotherapy-only was more frequently used compared to other time periods. However, since 1995 the use of both chemotherapy and radiotherapy were more common. The use of high dose chemotherapy, though uncommonly used, has increased since 2000. In examining therapy received by patients under the age of 5 years 46.5 % received chemotherapy and radiation therapy, 10.1 % received radiotherapy only and 22.9 % received chemotherapy only.
The numbers of cases contributed by the various centers, as well as therapy and outcome are shown in Table 3. Of note, there was not a significant difference in outcome based on the number of cases contributed by the center.
The tumor was reported to have recurred in 32.2 % of the cases. The distribution of the site of recurrence varied over time; however the posterior fossa was the most common site of reoccurrence (60 % of recurrence in this location—data not shown). Patients with M0 disease who had a reoccurrence did so in the posterior fossa 56 % of this time, M1 disease 74 % of the time, M2 disease 78 % of the time, M3 disease 52 % of the time and M4 disease had no recurrence in the posterior fossa.
To examine the role that different known risk factors might have in the determining of the overall 5-year survival rates, Kaplan–Meier analysis stratifying for each of the variables was done (Table 4). An increase in the 5-year survival rate with age was noted (Fig. 1) and based on initial treatment. However, neither stage of disease, gender, nor histologic subtype of medulloblastoma were found to be significant predictors of the 5-year survival.
To explore if the various risk factors reported in the literature to be associated with a poor outcome had an association, Cox Regression Modeling was used (Table 5). The proportional risk attributed to the outcome for each of the following factors: being less than 5 years of age at the time of diagnosis and having a first relapse attributed an approximately two fold increased risk for poor outcome.
Discussion
The overall 5-year survival of patients with medulloblastoma in this study was 69.2 ± 3.3 % which is similar to several recently published studies. A recent study examining the survival of children, adolescents and adults with medulloblastoma and primitive neuroectodermal tumors (PNETs) found a cumulative relative survival of 62, 52 and 47 % at 5, 10 and 20 years [3]. The 5-year cumulative relative survival was 30 % for infants (<1 year), 62 % for children (1–9 years), 64 % for adolescents (10–19 years) and 59 % for adults (>20 years). At 10 years this disparity broadened with survivals of 26, 57, 54 and 46 % respectively. They also found a significant improvement in survival for all age groups over the 25 year time period of the study, similar to the improvement we saw in our study. Another recent study utilized SEER data for survival of medulloblastoma from 1974 to 2003 [4]. They found the 5-year survival rate for medulloblastoma and PNET increased over the study time period with 43.7 % in 1974–1978 to 62.8 % in 1999–2003, again similar to our data. The HIT 91 protocol for children over the age of 3 years with medulloblastoma had a 10-year overall survival of 91 % for patients with M0 disease, 70 % for patients with M1 disease and 42 % for patients with M2/3 disease [5]. The HIT-SIOP PNET 4 trial compared hyperfractionated to conventional radiotherapy for standard risk medulloblastoma and had a 5-year overall survival of 86 ± 2 % and an event free survival of 79 ± 2 % [6]. Our study did not show a difference in survival based on histologic subtype of medulloblastoma, although is limited by the fact that there was no central pathology review. Nevertheless, the lack of difference is contrary to previous studies, and may reflect the intensity of current therapies currently being used.
Many studies examine patients with either high-risk or standard-risk disease. The most recent Children’s Oncology Group (COG) study for standard-risk medulloblastoma, found a 5- and 10-year event free survival of 81 ± 2 and 75.8 ± 2.3 % respectively, and 5- and 10-year overall survival of 87 ± 1.8 and 81.3 ± 2.1 % respectively [7], while the COG protocol for patients with metastatic medulloblastoma had a 5-year overall survival was 82 ± 9 % and progression free survival was 71 ± 11 % [8]. The metastatic stage did not influence survival. Our study did not find a difference in survival based on stage of disease, similar to the COG studies which had similar survivals for patients with high risk and standard risk disease. The results of our study, similar to COG studies, likely reflect the difference in intensity of therapy utilized based on stage of disease.
A recent change in therapy is the use of high dose chemotherapy with stem cell rescue. In this study, the use of this modality of therapy varied by era with an increase in the more recent time periods. One of the first large studies examining the result of radiation therapy, high dose chemotherapy with stem cell rescue for the therapy of medulloblastoma was the St Jude medulloblastoma 96 protocol [9]. This study had a 5-year overall survival rate of 85 % in the average risk group and 70 % in the high risk group. In our study, only 43 of 628 children received high dose chemotherapy with stem cell rescue. Children who received high dose chemotherapy only had a 51.9 ± 1.7 % 5-year survival, while those who received high dose chemotherapy and radiotherapy had a 84.7 ± 8.7 % 5-year survival.
Another factor often determining survival is age at diagnosis. In this analysis, children under the age of 5 years had a significantly lower survival than older children. A study by the CPBTC of infants under the age of 3 years with medulloblastoma demonstrated a 2-year event free survival of 57 ± 5 % and a 5-year event free survival of 30 ± 5 % [10]. This study is similar to our study, where all children under the age of 3 years of age with medulloblastoma in Canada were included, and not just patients enrolled on a clinical trial who met the inclusion criteria for the trial. Similarly, the SEER data on infants with brain tumors showed a 12 month survival of 43.7 %, but at 3 years, infants treated with surgery and radiation therapy had a survival of 64.7 % compared to a survival of 22.1 % for those treated without radiation [11]. A Children’s Oncology Group study for children aged 8 months to 3 years with standard risk medulloblastoma utilized chemotherapy and conformal radiation therapy and found a 4-year overall survival was 69 ± 5.5 % and event free survival was 50 ± 6 % [12]. The HIT 2000 protocol for children under 4 years of age treated children with chemotherapy alone and had a 5-year overall survival of 80 ± 6 % and event free survival of 57 ± 8 % [13]. This study showed that patients with desmoplastic/nodular histology had a better survival than those with classic histology and much better survival than those with anaplastic histology.
Our study also found that for children who relapse with their medulloblastoma, the majority relapse in the posterior fossa. The HIT-SIOP PNET 4 trial also examined the site of relapse, and found that 17 % were in the posterior fossa only, 18 % in the posterior fossa and craniospinal, and 65 % craniospinal only [6].
Overall, a major strength of our study is that it represents data for all children diagnosed with medulloblastoma from 1990 to 2009. These are very helpful data, as they include not just patients who met criteria for study inclusion, as many previous studies do. This study was limited by the fact that it was a longitudinal, retrospective study, and there was no central radiology or pathology review nor was there data on extent of surgical resection. The study shows an overall survival of 69.2 %, which should provide impetus to clinicians to improve this through future clinical trials. One such improvement planned for future clinical trials is to focus on the molecular classification of medulloblastoma with therapies targeting specific molecular subgroups [14].
References
Packer RJ, Cogen P, Vezina G, Rorke LB (1999) Medulloblastoma: clinical and biological aspects. Neurooncology 1:232–250
Gajjar A, Packer RJ, Foreman NK, Cohen K, Haas-Kogan D, Merchant TE (2013) Children’s Oncology Group 2013 blueprint for research: central nervous system tumors. Pediatr Blood Cancer 60:1022–1026
Smoll NR (2012) Relative survival of childhood and adult medulloblastomas and primitive neuroectodermal tumors (PNETs). Cancer 118:1313–1322
Patel S, Bhatnagar A, Wear C, Osiro S, Gabriel A, Kimball D, John A, Fields PJ, Tubbs S, Loukas M (2014) Are pediatric brain tumors on the rise in the USA? Significant incidence and survival findings from the SEER database analysis. Childs Nerv Syst 30:147–154
Von Hoff K, Hinkes B, Gerber NU, Deinlein F, Mittler U, Urban C, Benesch M, Warmuth-Metz M, Soerensen N, Zweiner I, Goette H, Schlegel PG, Pietsch T, Kortmann RD, Kuehl J, Rutkowski S (2009) Long-term outcome and clinical prognostic factors in children with medulloblastoma treated in the prospective randomized multicenter trial HIT’91. Eur J Cancer 45:1209–1217
Lannering B, Rutkowski S, Doz F, Pizer B, Gustafsson G, Navajas A, Massimino M, Reddingius R, Benesch M, Carrie C, Taylor R, Gandola L, Bjork-Eriksson T, Giralt J, Olderberger F, Pietsch T, Figarella-Branger D, Robson K, Formi M, Clifford SC, Warmuth-Metz M, von Hoff K, Faldum A, Mosseri V, Kortmann R (2012) Hyperfractionated versus conventional radiotherapy followed by chemotherapy in standard-risk medulloblastoma: results from the randomized multicenter HIT-SIOP PNET 4 trial. J Clin Oncol 30:3187–3193
Packer RJ, Zhou T, Holmes E, Vezina G, Gajjar A (2013) Survival and secondary tumors in children with medulloblastoma receiving radiotherapy and adjuvant chemotherapy: results of Children’s Oncology Group trial A9961. Neuro-Oncology 15:97–103
Jakacki R, Burger PC, Zhou T, Holmes EJ, Kocak M, Onar A, Goldwein J, Mehta M, Packer RJ, Tarbell N, Fitz C, Vezina G, Hilden J, Pollack IF (2012) Outcome of children with metastatic medulloblastoma treated with carboplatin during craniospinal radiotherapy: a Children’s Oncology Group Phase I/II study. J Clin Oncol 30:2648–2653
Gajjar A, Chintagumpala M, Ashley D, Kellie S, Yun LE, Merchant TE, Woo S, Wheeler G, Ahern V, Krasin MJ, Fouladi M, Broniscer A, Krance R, Hale GA, Stewart CF, Dauser R, Sanford RA, Fuller C, Boyett JM, Wallace D, Gilbertson RJ (2006) Risk-adapted craniospinal radiotherapy and stem-cell rescue in children with newly diagnosed medulloblastoma (St Jude Medulloblastoma-96): long-term results from a prospective, multicenter trial. Lancet Oncol 7:813–820
Johnston DL, Keene D, Bartels U, Carret AS, Crooks B, Eisenstat DD, Fryer C, Lafay-Cousin L, Larouche V, Moghrabi A, Wilson B, Zelcer S, Silva M, Brossard J, Bouffet E (2009) Medulloblastoma in children under the age of three years: a retrospective Canadian review. J Neurooncol 94:51–56
Bishop AJ, McDonald MW, Chang AL, Esiashvili N (2012) Infant brain tumors: incidence, survival and the role of radiation based on surveillance, epidemiology and end result (SEER) data. Int J Radiat Oncol Biol Phys 82:341–347
Ashley D, Merchant TE, Strother D, Zhou T, Duffner P, Burger PC, Miller DC, Lyon N, Bonner MJ, Msall M, Buxton A, Geyer R, Kun LE, Coleman L, Pollack IF (2012) Induction chemotherapy and conformal radiation therapy for very young children with nonmetastatic medulloblastoma: Children’s Oncology Group study P9934. J Clin Oncol 30:3181–3186
Von Bueren AO, von Hoff K, Pietsch T, Gerber NU, Warmuth-Metz M, Deinlein F, Zwiener I, Faldum A, Fleischhack G, Benesch M, Krauss J, Kuehl J, Kortmann RD, Rutkowski S (2011) Treatment of young children with localized medulloblastoma by chemotherapy alone: results of the prospective, multicenter trial HIT 2000 confirming the prognostic impact of histology. Neuro-Oncology 13:669–679
De Souza RM, Jones BR, Lowis SP, Kurian KM (2014) Pediatric medulloblastoma—update on molecular classification driving targeted therapies. Front Oncol 4:176
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johnston, D.L., Keene, D., Kostova, M. et al. Survival of children with medulloblastoma in Canada diagnosed between 1990 and 2009 inclusive. J Neurooncol 124, 247–253 (2015). https://doi.org/10.1007/s11060-015-1831-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1831-0