Abstract
Paclitaxel (PTX) is a well-known antitumor drug, widely utilized in the treatment of breast, ovarian, head, and neck tumors, among others. The low aqueous solubility (< 1.0 μg/mL; log P = 3.96) limits its use by intravenous route, and alternatives found for the marketed products are associated with high toxicity. Incorporation of PTX into lipid nanocarriers has been considered an interesting nontoxic alternative for this route, but drug loading is usually low. This study aimed to analyze the influence of the lipid composition and three different lipid nanosystems—solid lipid nanoparticles, nanostructured lipid carriers (NLCs), and nanoemulsion—in PTX encapsulation and its biological response. The three proposed systems were prepared by hot melt homogenization followed by ultrasonication. Among the blank formulations first prepared, NLC had the smallest size (74 ± 1 nm), with negative zeta potential (− 11.4 ± 0.1 mV). The incorporation of 0.10 mg/mL PTX into this NLC formulation yielded high and stable encapsulation (0.089 ± 0.003 mg/mL), also supported by polarized light microscopy and differential scanning calorimetry curves. NLC-PTX was very effective against MCF-7 (IC50 25.33 ± 3.17 nM) and MDA-MB-231 breast cancer cell lines (IC50 2.13 ± 0.21 nM), compared to free PTX (IC50 > 500 nM). In addition, no significant cytotoxicity was found against fibroblast cells. Taken together, these results demonstrated that PTX was successfully incorporated into NLC with appropriate physicochemical characteristics for intravenous administration, suggesting that the use of NLC as vehicle to incorporate PTX may be a promising strategy in the treatment of breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paclitaxel (PTX) is a drug derived from the bark of the Pacific yew, Taxus brevifolia, which promotes assembly of microtubules inhibiting their disassembly. The direct activation of apoptotic pathways has also been suggested to be critical to the cytotoxicity of this drug. Although it plays an important role in the treatment of several types of human cancer, the low solubility of PTX in aqueous medium represents a barrier for intravenous administration. Therefore, the conventional PTX formulation contains a high concentration of Cremophor-EL™ (polyethoxylated castor oil), a surfactant associated with significant toxicities such as hypersensitivity reactions, myelosuppression, and peripheral neuropathy. In addition, this toxicity is frequently increased due to the prolonged systemic exposure of PTX micelles (Gelderblom et al. 2001; Donyai and Sewell 2006).
To overcome these limitations, PTX has been associated with cyclodextrins (Sharma et al. 1995; Yu et al. 2013; Jing et al. 2013) and with colloidal carriers (Zhang et al. 2011; Kataoka et al. 1993; Hamaguchi et al. 2005; Feng et al. 2004; Gaucher et al. 2007; Videira et al. 2012; Baek et al. 2012; Gibson et al. 2007; Hua et al. 2010). Although several studies have demonstrated that PTX encapsulation in colloidal carriers can increase the accumulation in the tumor tissue and minimize systemic toxicity, only one product was approved by the Food and Drug Administration for marketing, Abraxane™. This preparation consists of particles of PTX with a nanometer-sized range linked through hydrophobic interactions to human albumin. Abraxane™ has shown higher safety compared to Taxol™; thus, larger doses of PTX can be administered not only with better responses but also with enhanced risk for toxicity, especially in patients with altered metabolism (Green et al. 2006; Trickler et al. 2008).
Although several lipid nanocarriers, such as nanoemulsions (NE), solid lipid nanoparticles (SLNs), and nanostructured lipid carriers (NLCs), have also been studied as strategies to allow the intravenous administration of PTX (Baek et al. 2012; Zheng et al. 2016; Wu et al. 2010), in all of them, drug loading is very low. The main difference between these systems is related to the lipid core. While NE has only liquid lipids in its constitution, SLN and NLC have a solid matrix; thus, they have more potential for drug-controlled release (Weber et al. 2014; Naahidi et al. 2013; Muller et al. 2000). However, SLN often shows poor drug-loading capacity as well as the potential for drug expulsion after polymorphic transition during storage. In order to overcome these limitations, an alteration of SLN by the association of liquid lipids into the solid structure has been studied as the named NLC. The liquid lipid provokes imperfections in the solid lipid matrix, increasing the drug concentration and preventing its expulsion over time (Selvamuthukumar and Velmurugan 2012). Finally, all these systems have been associated with an ease of production by using the high-pressure homogenization method identical to that used in parenteral O/W emulsions, already available in the pharmaceutical industry, which favors large-scale production.
Recent studies have reported the use of lipid nanocarriers containing PTX for the treatment of skin disease by topical route (Tosta et al. 2014), lung cancer (Wang et al. 2016; Shao et al. 2015; Miao et al. 2015), breast cancer (Swidan et al. 2016; Xu and Lee 2015), and glioma (Banerjee et al. 2016). The results showed improvement in the bioavailability and/or toxicity (Tosta et al. 2014; Wang et al. 2016; Shao et al. 2015; Miao et al. 2015; Swidan et al. 2016; Xu and Lee 2015; Banerjee et al. 2016). However, it is known that the features and biologic response of the nanostructures depend on factors such as lipid composition, stabilizing agents, and the concentration of the incorporated drug. In this context, the aim of this study was to develop new lipid nanocarriers (NE, SLN, and NLC) containing PTX and to evaluate the effect of the composition on the physicochemical properties and the in vitro cytotoxic activity against breast cancer cell lines.
Materials and methods
Materials
Paclitaxel was supplied by Quiral Quimica do Brasil S.A. (Juiz de Fora, Brazil). Polysorbate 80 (Super Refined Tween 80™) and medium-chain triglycerides (MCTs: Crodamol™ GTCC) were purchased from Croda Inc. (Edison, USA). Glyceryl behenate (Compritol™ 888 ATO) was provided by Gattefossé (Lyon, France). Cholesterol, acetonitrile, and tetrahydrofuran HPLC grade were provided by Sigma-Aldrich (Saint Louis, MO, USA). Glycerol was purchased from Casa da Química Indústria e Comércio Ltda (São Paulo, Brazil). Water was purified using a Milli-Q apparatus (Millipore, Billerica, USA). All other chemicals were of analytical grade without further purification.
For the in vitro studies, Roswell Park Memorial Institute medium 1640 was obtained from Sigma-Aldrich (Saint Louis, MO, USA). Dulbecco’s modified Eagle medium, fetal bovine serum, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT), and staurosporine were purchased from Gibco Life Technologies (Carlsbad, CA, USA).
The cancer cell lines MCF-7 and MDA-MB-231 (human breast adenocarcinoma cells) were purchased from American Type Culture Collection (ATCC) (Manassas, USA). Cell line L929 (fibroblast from mouse) was kindly supplied by Professor Helen Rodrigues Martins (Laboratory of Parasitic Diseases, UFVJM, Diamantina, Brazil).
Methods
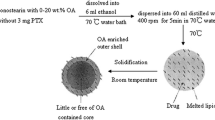
Preparation of nanocarriers
All formulations (NE, SLN, and NLC) were prepared by the hot melting homogenization method using an emulsification ultrasound (Castro et al. 2009; Carneiro et al. 2012). The composition of the formulations is shown in Table 1.
First, the oily (OP) and the aqueous phases (AP) were heated separately to the temperature of 85 °C. After the melting of the OP, the AP was slowly dropped into the OP and homogenized using a glass rod for 2 min. The obtained emulsion was immediately submitted to the high-intensity ultrasonic treatment (20% amplitude) for 10 min using a high-intensity ultrasonic processor (CPX 500 model; Cole-Palmer Instruments, East Bunker Court Vernon Hills, IL, USA). Then, these preparations were cooled to the room temperature resulting in the formation of SLN, NLC, or NE depending on the physical state of the used lipids. The pH of the preparations was finally adjusted to 7.0 with a solution of 0.01 M HCl. For formulations containing drug, PTX ethanolic solution equivalent to 0.10 or 0.25 mg/mL was added to the OP during heating. All products were stored at 4 °C.
Particle size and polydispersity index analysis
The mean particle diameter in the dispersion was determined by unimodal analysis through dynamic light scattering using a Zetasizer NanoZS90 (Malvern Instruments, Malvern, UK) at a fixed angle of 90° and temperature of 25 °C. The data were reported as mean particle diameter, evaluated as the intensity obtained from three repeat measurements and the polydispersity index (PDI).
Zeta potential
Zeta potential measurements were carried out by the electrophoretic light scattering determination using a Zetasizer NanoZS90 (Malvern Instruments, Malvern, UK), at 25 °C. All measurements were performed in triplicate.
Drug encapsulation efficiency
The encapsulation efficiency (EE) was based on the quantification of PTX concentration in the nanoparticles before (total PTX) and after filtration (cellulose ester membrane, 0.45 mm, Millipore, Billerica, MA, USA). The fraction of free PTX, soluble in the external AP of the formulations, was estimated by the ultrafiltration method (Amicon™ 100K, Millipore, Billerica, MA, USA) using a 100 kDa molecular weight cutoff membrane. Briefly, an aliquot of each nanoparticle was dissolved in tetrahydrofuran and diluted in a mixture of acetonitrile/water (55:45 v/v). The obtained dispersion was filtered in a 0.45-mm Millex HV filter (Millipore, Billerica, MA, USA) and analyzed by a high-performance liquid chromatography (HPLC) method previously described (Barbosa et al. 2015).
The chromatographic system consisted of an LC-6AD pump, a CTO-20A oven, a SIL-10AF auto injector, and a model SPD-M20A diode array detector (Shimadzu, Kyoto, Japan). The chromatographic system was operated using the LabSolution software. Separations were performed using a 250 × 4.6 mm, 5-μm Supelcosil™ LC-18-db column (Supelco Inc., Bellefonte, USA). The mobile phase consisted of an acetonitrile and distilled water (55:45 v/v) mixture, in isocratic flow. The eluate absorbance was monitored at 227 nm, with a flow rate of 1.2 mL/min and 20 μL of injection volume sample. The nine-point standard curve (4.0, 6.0, 8.0, 10.0, 12.0, 14.0, 16.0, 18.0, and 20.0 μg/mL) vs. area under curve obtained by linear regression analysis resulted in the following linear equation: y = − 16,013.5x + 36,000.2 (r = 0.9952). Based on the negligible values of PTX concentration (lower than 0.03 μg/mL), EE was calculated using the formula:
Polarized light microscopy
The presence of PTX crystals was analyzed by polarized light microscopy (Zeiss Axio Imager, M2, Carl Zeiss, Oberkochen, Germany). The undiluted samples were prepared on microscope slides and evaluated using the proper software (ZEN lite 2012, Carl Zeiss, Oberkochen, Germany). The microscope was equipped with an Axio Cam digital camera (Model ERc 5S, Carl Zeiss, Oberkochen, Germany).
Stability study
The determination of the storage stability of nanoparticles containing PTX was performed at 10, 20, and 30 days after preparation. All formulations (n = 3 batches) were maintained at 4 °C. The parameters evaluated included mean particle diameter, PDI, zeta potential, percentage of drug retention in the nanocarrier, and pH of the external phase. The mean values of these parameters in the predetermined times were compared with those obtained at zero time.
Differential scanning calorimetry
Firstly, lyophilized NLCs were obtained using a freeze dryer (Liofilizador LS300, Terroni™), after freezing with liquid nitrogen. The samples were lyophilized at − 45 °C for 24 h. After freeze-drying, the samples were placed in aluminum pans for differential scanning calorimetry (DSC) measurements. The analyses were obtained with a DSC 2910 (TA Instruments, New Castle, DE, USA), at a heating rate of 10 °C/min and a temperature range of 0–250 °C, under nitrogen purge (50 mL/min). Indium was used for temperature and enthalpy calibration. Data acquisition and analysis were performed on a microcomputer using an Isothermal Software Kit provided by TA Instruments.
Analysis of cell viability
Cytotoxicity was evaluated by the MTT assay, based on the reduction of the tetrazolium salt to an insoluble formazan crystal by living cells. Aliquots containing 4500 (MCF-7), 3600 (MDA-MB-231), or 18,000 (L929) cells/well were seeded into 96-well plates and incubated at 37 °C and 5% CO2 for 24 h. Afterwards, freshly prepared solutions of free PTX and NLC-PTX were added to the wells (PTX concentration ranged from 0.032 to 500 mM). Free PTX (6.0 mg/mL) was dissolved in a 50:50 Cremophor™ EL/absolute ethanol mixture prior to dilution. Blank NLC (without PTX) was diluted in the same way as NLC-PTX to simulate the same range of PTX concentration. After 48 h of incubation (37 °C and 5% CO2), 20 μL of the 5 mg/mL MTT solution was added to each plate. Plates were incubated at 37 °C for 4 h, and then, the medium was replaced by 200 μL of 0.04 mol/L HCl solution in isopropanol. Metabolic activity was estimated by measuring the rate of mitochondrial reduction of MTT of each treatment, determined by evaluating the absorbance of the converted dye at a wavelength of 595 nm. Absorbance values of the wells in which the cells were maintained in medium alone were considered as 100% of cellular viability. Afterwards, the inhibitory concentration (IC50) was calculated as the concentration that inhibited cell proliferation by 50%, compared to untreated controls, using Graphpad Prism 5.0 (Graphpad Software Inc., San Diego, USA). Data were expressed as the percentage of cell metabolic viability compared with the control (mean ± standard deviation). At least three independent experiments were performed.
Statistical analysis
Data were submitted to Lilliefors and Bartlett tests to evaluate normality and homogeneity of variances, respectively. The data of physicochemical characterization and the stability study were verified by one-way analysis of variance (ANOVA) test with Tukey’s post hoc test. Cytotoxicity analysis was performed using two-way ANOVA, followed by Bonferroni test. Differences were considered significant when P values were lower than 0.05. The statistical program used was GraphPad Prism (5.0 version, San Diego, CA, USA).
Results and discussion
Characterization of lipid nanocarriers
Lipid nanocarriers have been the object of many studies, due to their high biocompatibility. Among these systems, NE, SLN, and NLC have been widely proposed as nanocarrier systems due to the possibility of enhancement of drug loading and stability. Particularly, NLC has been very promising, since the mixture of solid and liquid lipids in the core has shown to provide better performance features such as higher drug incorporation and retention in the nanoparticles (Weber et al. 2014; Naahidi et al. 2013; Muller et al. 2000) Thus, in this work, we compared the association of PTX, a highly lipophilic drug (log P = 3.96; solubility in water < 1.0 μg/mL) with a high molecular weight (853.9), in different lipid nanocarriers (NE, SLN, and NLC) in order to evaluate the influence of the lipid composition in the PTX encapsulation. Table 2 shows the effect of the composition and PTX concentration on the physicochemical properties of nanoparticles.
First, blank formulations (without PTX) were developed. The larger diameter was obtained for SLN compared to NE and NLC. On the other hand, blank NLC showed diameter values approximately 2-fold and 1.7-fold lower than those obtained for SLN and NE, respectively. The incorporation of PTX into the lipid matrix increased the particle diameter for both SLN and NLC, which was proportional to the concentration (up to 70% increase in diameter). However, this was not observed for NE, which has a liquid core. The results clearly showed that the physical state of the lipid had a significant effect on the nanocarrier diameter. Compritol™ 888 ATO, a component of the lipid matrix of SLN, has a pronounced hydrophobic property attributed to a longer fatty acid chain length in behenic acid (C22) (Aburahma and Badr-Eldin 2014). On the other hand, Crodamol™ GTCC, a component of lipid matrix NE, is derived from a fully saturated medium fatty acid chain mainly of caprylic (C8) and capric acids (C10), which explain the low viscosity of this compound. The high viscosity of glyceryl behenate impairs its dispersion in the aqueous medium, resulting in large spaces between the lipid chains. Additionally, the presence of medium-chain triglycerides in the oil phase improves the fluidity of the blend and provides a better organization of the matrix, which resulted in a smaller diameter of the NLC (Mitri et al. 2011). The increase in diameter by PTX presence can be likely due to enlargement of the inner phase volume by the incorporated PTX, as previous reported (Xu and Lee 2015; Zhang et al. 2008). All formulations containing PTX showed PDI higher than 0.3, except NE with 0.1 mg/mL PTX (Table 2); however, populations with a diameter smaller than 500 nm were observed, and a percentage of nanocarriers greater than 5 μm to less than 0.5% could also be detected (data not shown). Thus, all formulations showed appropriate features for intravenous administration, according to the standards established by US Pharmacopeia for products intended for parenteral administration (USP 36-NF 34 2016).
Zeta potential analysis was performed to obtain information about the surface properties of the nanostructures. All developed formulations showed negative zeta potential values, which ranged from − 5.6 to − 15.3 mV (Table 2). The negative values of zeta potential obtained in this study can be attributed to polarization of the nonionic surfactant, followed by adsorption of polarized water molecules at the surface of the nanostructures (Zhao et al. 2014). In general, higher negative zeta potential absolute values (> 30 mV) are associated with the physical stability of a colloidal dispersion. On the other hand, the use of steric stabilizers can also favor the production of stable formulations (Mohanraj and Chen 2006; Baker and Naguib 2005). Although zeta potential values were not too negative, the nonionic surfactant Tween 80 provides an additional effect of steric stabilization on the nanostructure surface, due to its ethoxylated branch groups, thus avoiding agglomeration of the particles.
EE of PTX in 0.10 mg/mL formulations was high, regardless of the lipid nanocarrier utilized, ranging from 70% (NE) to 90% (NLC) (Fig. 1a), with significant differences among all of them (P < 0.05). It is also noteworthy that the increase of the PTX concentration clearly resulted in a significant reduction in EE, ranging from 38 to 50% in 0.25 mg/mL PTX formulations. This result suggests a saturation of the system, which did not allow the association of higher concentrations of PTX. This hypothesis is supported by the analysis of the PTX concentration incorporated into the systems, as can be seen in Fig. 1b. No significant difference was observed between the PTX encapsulated after addition of 0.10 and 0.25 mg/mL of drug in all evaluated lipid nanocarriers. However, the combination of liquid and solid lipids leads to an increase in the encapsulation of PTX in NLC compared to SLN (P < 0.05). This may be attributed to the formation of a less-ordered lattice defect in NLC with more space for guest molecules as well as the higher solubility of PTX in liquid oil than solid lipids (Swidan et al. 2016).
Encapsulation efficiency (a) and measured concentration of PTX (b) in different lipid nanocarriers. NE nanoemulsion, SLN solid lipid nanoparticles, NLC nanostructured lipid carriers, PTX paclitaxel. Significant difference as compared with NE at the same PTX concentration (a). Significant difference as compared with PTX concentration 0.10 mg/mL considering the same formulation (b). Significant difference between SLN and NLC (c). Data expressed as mean ± standard deviation (SD) of three batches. P values less than 0.05 were set as the level of significance (Student’s t test)
As can be seen in Fig. 2, the crystals of PTX were clearly observed at high intensity in the external AP of NE, but not in NLC. In fact, these drug crystals show that PTX has a strong tendency for crystallization in an aqueous medium and its efficient incorporation into a lipid matrix is a difficult task (Jain et al. 2012). These findings are consistent with our previous observations on PTX encapsulation obtained by HPLC assay, suggesting high PTX incorporation into the lipid matrix of NLC.
Stability study
Previous studies using other colloidal systems have shown that the increase in biological activity of PTX is dose dependent (Barbosa et al. 2015). Therefore, a highly desirable prerequisite is to obtain a high drug concentration associated with the system that remains incorporated over time. As the increased PTX concentration in the present study did not influence the amount of encapsulated drug, the stability study was performed with the formulations containing 0.10 mg/mL PTX. There were no significant variations in diameter and PDI of NE, SLN, or NLC over 30 days (Fig. 3), as well as no significant change in the zeta potential (Fig. 4a). The maintenance of these parameters may be explained by the steric repulsion provoked by the nonionic surfactant Tween™ 80 on the nanostructure surface, which could prevent aggregation and/or fusion, improving the stability of the formulations. On the other hand, a significant reduction in pH value for NE-PTX, ranging from 7.2 to 6.1, could be detected over time (Fig. 4b), which may be related to the hydrolysis of ester linkages of Tween™ 80 and/or MCT molecules (Bruxel et al. 2012). This reduction was not as evident for SLN and NLC formulations (Fig. 4b). However, all pH values remained in the acceptable range for intravenous administration (USP 36-NF 34 2016).
Diameter and PDI of NE (a), SLN (b), and NLC (c) with 0.10 mg/mL PTX over 30 days of storage at 4 °C. The 0-day column shows the particle diameter obtained after preparation of formulation. Data expressed as mean ± standard deviation (SD) of three batches. There was no significant difference during the evaluated time (P > 0.05, Tukey’s test)
Zeta potential (a), pH (b), and PTX retention rate (c) measurement of NE (black squares), SLN (red circles), and NLC (blue triangles) with 0.10 mg/mL PTX over 30 days of storage at 4 °C. The 0 day shows the particle diameter obtained right after the preparation. Data expressed as mean ± standard deviation (SD) of three batches. Significant difference compared to 0 day (a). P values less than 0.05 were set as the level of significance (Tukey’s test)
Concerning the PTX retention, Fig. 4c shows that SLN-PTX was less stable than NLC-PTX and NE-PTX. A significant alteration was observed from the 10th day of storage for SLN-PTX (from 82 ± 6 to 38 ± 16%). On the other hand, PTX remained encapsulated in NLC-PTX, suggesting the greater stability of this system as compared to NE-PTX and SLN-PTX as well as better affinity of the drug with the oil present in the NLC lipid matrices. Similar findings were observed by other researchers (Tosta et al. 2014; Jenning et al. 2000; Das et al. 2012) and can be explained by transition to highly ordered lipid particles, which promotes the drug expulsion from SLN. After production, lipids crystallize partially with more imperfections in the crystal lattice. During storage, a transition from the less stable crystalline modifications can occur, triggering the drug release from the lipid matrix (Wissing et al. 2004). However, this can be prevented by mixing solid lipids with small amounts of liquid lipids, forming nanocompartments or an amorphous solid matrix accommodating more of the drug. Furthermore, recent studies have shown that the oil could surround the solid matrix and form a layer of oil between the solid lipid and the surfactants (Yang et al. 2014). Based on the stability study, NLC-PTX showed adequate properties and high stability, and it was thus selected for subsequent studies.
Differential scanning calorimetry
DSC was used to investigate the thermal behavior of the blank NLC and NLC-PTX (Fig. 5). An intense DSC endothermic peak centered at 72.5 and 150 °C was observed for Compritol™ 888 ATO (Fig. 5a) and cholesterol (Fig. 5b), respectively, which can be associated with the melting point. DSC analysis of pure PTX (Fig. 5c) also showed an endothermic peak corresponding to a melting point of 225 °C, which indicated its crystalline nature. When Compritol™ 888 ATO was formulated as blank NLC (Fig. 5d) and NLC-PTX (Fig. 5e), a remarkably lower endothermic peak of lipid was observed as well as a shift in the melting point of NLC compared to pure Compritol 888 ATO. This may be attributed to the interaction between solid and liquid lipid during the preparation process, promoting disordered arrangement and lattice defects (Tran et al. 2014). It is noteworthy that the DSC curve of NLC-PTX did not show any peak for PTX, suggesting that the drug is incorporated into the lipid core in an amorphous state or a molecularly dispersed state (Fig. 5e).
Cytotoxicity analysis
In order to evaluate whether the cytotoxicity of PTX was affected by loading in NLC, an MTT assay was performed in MDA-MB-231 and MCF-7 (breast cancer cells) and L929 (normal cells). Mouse fibroblast L929 is recommended as normal cells by international standards for the testing of medical devices and responds more sensitively than primary cells (Schedle et al. 1995). MTT metabolism reflects the cell metabolic activity or the rate of glycolytic NADH production. Since the MTT assay is rapid, convenient, and economical, it has often been used to correlate with the number of viable cells growing in standard culture conditions. The data obtained, expressed as cell metabolic viability (percentage), are shown in Fig. 6. In addition, the inhibitory concentration (IC50) was defined as the concentration that inhibited tumor cell proliferation by 50% when compared to untreated controls.
MTT metabolism of NLC-PTX (circles), free PTX (triangles), and blank NLC (squares) evaluated against MDA-MB-231 (a), MCF-7 (b), and L929 (c) cells after 48-h exposure. Data were expressed as mean ± SD of three independent experiments. The asterisk represents significant difference between NCL-PTX and free PTX (P < 0.001)
Firstly, it is important to highlight that no significant cytotoxic activity (MTT metabolism was near 100%) was observed for the free PTX solvent (dehydrated ethanol/Cremophor EL™) in all tested cell lines (data not shown).
For MDA-MB-231 cells, blank NLC showed minimal cytotoxicity, with reduction to 18% of cell viability at a concentration of 500 nM (Fig. 6a). The activity of NLC-PTX was significantly higher (P < 0.001) than that observed for free PTX, except at a concentration of 0.032 nM (Fig. 6a). The IC50 of NLC-PTX (2.13 ± 0.21 nM) was significantly lower than that obtained for free PTX (> 500 nM).
Regarding MCF-7 cells, the data also demonstrated a minimum inhibitory effect for blank NLC, with metabolic activity near 80% at a higher concentration (Fig. 6b). The cytotoxicity of free PTX was also significantly lower (P < 0.001) than that for NLC-PTX at all concentrations evaluated. The IC50 of NLC-PTX (25.33 ± 3.17 nM) was significantly lower than that obtained for free PTX (> 500 nM). These results also suggest that MCF-7 cells were less sensitive to treatment with NLC-PTX compared with MDA-MB-231 cells. In addition, a dose-dependent relationship between drug concentration and metabolic activity was clearly observed for both breast cancer cell lines evaluated.
In the normal fibroblast cells (L929), a reduction of cell viability was observed for free PTX (74 ± 3%) and NCL-PTX (84 ± 4%) at the highest concentration (500 nM). However, according to ISO 10993–5 2009, a substance has cytotoxic potential if cellular viability is reduced to < 70%. Thus, no significant cytotoxicity was found for any of the formulations evaluated against L929 (Fig. 6c).
The low cytotoxicity observed for the NLC-PTX in the normal cell line (L929) and the reduction in cell viability in the breast cancer cell lines, MCF-7 and MDA-MB-231, suggest the selective and enhanced uptake of the nanoparticles by the tumor cells. This can result in an interesting strategy to enhance therapeutic efficacy of PTX. Similar results were previously reported by our research group using another lipid nanocarrier (Barbosa et al. 2015).
Conclusion
In conclusion, the results of the present study demonstrated that PTX was successfully incorporated into NLC, and this formulation showed appropriate physicochemical features for intravenous administration as well as increased stability compared to another lipid nanocarrier evaluated. Furthermore, NLC containing PTX showed greater cytotoxicity than free PTX against breast cancer cells. The results suggest that NLC might be a promising strategy to achieve an efficient antitumor effect in the treatment of breast cancer.
References
Aburahma MH, Badr-Eldin SM (2014) Compritol 888 ATO: a multifunctional lipid excipient in drug delivery systems and nanopharmaceuticals. Expert Opin Drug Deliv 11:1865–1883. https://doi.org/10.1517/17425247.2014.935335
Baek JS, So JW, Shin SC, Cho CW (2012) Solid lipid nanoparticles of paclitaxel strengthened by hydroxypropyl-beta-cyclodextrin as an oral delivery system. Int J Mol Med 30:953–959. https://doi.org/10.3892/ijmm.2012.1086
Baker MT, Naguib M (2005) Propofol: the challenges of formulation. Anesthesiology 103:860–876
Banerjee I, De K, Mukherjee D, Dey G, Chattopadhyay S, Mukherjee M, Mandal M, Bandyopadhyay AK, Gupta A, Ganguly S, Misra M (2016) Paclitaxel-loaded solid lipid nanoparticles modified with Tyr-3-octreotide for enhanced anti-angiogenic and anti-glioma therapy. Acta Biomater 38:69–81. https://doi.org/10.1016/j.actbio.2016.04.026
Barbosa MV, Monteiro LO, Carneiro G, Malagutti AR, Vilela JM, Andrade MS, Oliveira MC, Carvalho-Junior AD, Leite EA (2015) Experimental design of a liposomal lipid system: a potential strategy for paclitaxel-based breast cancer treatment. Colloids Surf B Biointerfaces 136:553–561. https://doi.org/10.1016/j.colsurfb.2015.09.055
Bruxel F, Laux M, Wild LB, Fraga M, Koester LS, Teixeira HF (2012) Nanoemulsions as parenteral drug delivery systems. Quim Nova 35:1827–1840. https://doi.org/10.1590/S0100-40422012000900023
Carneiro G, Silva EL, Pacheco LA, de Souza-Fagundes EM, Correa NC, de Goes AM, Oliveira MC, Ferreira LAM (2012) Formation of ion pairing as an alternative to improve encapsulation and anticancer activity of all-trans retinoic acid loaded in solid lipid nanoparticles. Int J Nanomedicine 7:6011–6020. https://doi.org/10.2147/IJN.S38953
Castro GA, Coelho AL, Oliveira CA, Mahecha GA, Orefice RL, Ferreira LA (2009) Formation of ion pairing as an alternative to improve encapsulation and stability and to reduce skin irritation of retinoic acid loaded in solid lipid nanoparticles. Int J Pharm 381:77–83. https://doi.org/10.1016/j.ijpharm.2009.07.025
Das S, Ng WK, Tan RB (2012) Are nanostructured lipid carriers (NLCs) better than solid lipid nanoparticles (SLNs): development, characterizations and comparative evaluations of clotrimazole-loaded SLNs and NLCs? Eur J Pharm Sci 47:139–151. https://doi.org/10.1016/j.ejps.2012.05.010
Donyai P, Sewell GJ (2006) Physical and chemical stability of paclitaxel infusions in different container types. J Oncol Pharm Pract 12:211–222. https://doi.org/10.1177/1078155206073589
Feng SS, Mu L, Win KY, Huang G (2004) Nanoparticles of biodegradable polymers for clinical administration of paclitaxel. Curr Med Chem 11:413–424. https://doi.org/10.2174/0929867043455909
Gaucher G, Poreba M, Ravenelle F, Leroux JC (2007) Poly(N-vinyl-pyrrolidone)-block-poly(D,L-lactide) as polymeric emulsifier for the preparation of biodegradable nanoparticles. J Pharm Sci 96:1763–1775. https://doi.org/10.1002/jps.20833
Gelderblom H, Verweij J, Nooter K, Sparreboom A (2001) Cremophor EL: the drawbacks and advantages of vehicle selection for drug formulation. Eur J Cancer 37:1590–1598. https://doi.org/10.1016/S0959-8049(01)00171-X
Gibson JD, Khanal BP, Zubarev ER (2007) Paclitaxel-functionalized gold nanoparticles. J Am Chem Soc 129:11653–11661. https://doi.org/10.1021/ja075181k
Green MR, Manikhas GM, Orlov S, Afanasyev B, Makhson AM, Bhar P, Hawkins MJ (2006) Abraxane, a novel Cremophor-free, albumin-bound particle form of paclitaxel for the treatment of advanced non-small-cell lung cancer. Ann Oncol 17:1263–1268. https://doi.org/10.1093/annonc/mdl104
Hamaguchi T, Matsumura Y, Suzuki M, Shimizu K, Goda R, Nakamura I, Nakatomi I, Yokoyama M, Kataoka K, Kakizoe T (2005) NK105, a paclitaxel-incorporating micellar nanoparticle formulation, can extend in vivo antitumour activity and reduce the neurotoxicity of paclitaxel. Br J Cancer 92:1240–1246. https://doi.org/10.1038/sj.bjc.6602479
Hua MY, Yang HW, Chuang CK, Tsai RY, Chen WJ, Chuang KL, Chang YH, Chuang HC, Pang ST (2010) Magnetic-nanoparticle-modified paclitaxel for targeted therapy for prostate cancer. Biomaterials 31:7355–7363. https://doi.org/10.1016/j.biomaterials.2010.05.061
ISO 10993–5 (2009) Biological evaluation of medical devices-part 5. Tests for Cytotoxicity: In vitro Methods. ISO, Geneve
Jain V, Swarnakar NK, Mishra PR, Verma A, Kaul A, Mishra AK, Jain NK (2012) Paclitaxel loaded PEGylated glecerylmonooleate based nanoparticulate carriers in chemotherapy. Biomaterials 33:7206–7220. https://doi.org/10.1016/j.biomaterials.2012.06.056
Jenning V, Mader K, Gohla SH (2000) Solid lipid nanoparticles (SLN) based on binary mixtures of liquid and solid lipids: a (1)H-NMR study. Int J Pharm 205:15–21. https://doi.org/10.1016/S0378-5173(00)00462-2
Jing J, Szarpak-Jankowska A, Guillot R, Pignot-Paintrand I, Picart C, Auzély-Velty R (2013) Cyclodextrin/paclitaxel complex in biodegradable capsules for breast cancer treatment. Chem Mater 25:3867–3873. https://doi.org/10.1021/cm4019925
Kataoka K, Kwon GS, Yokoyama M, Okano T, Sakurai Y (1993) Block copolymer micelles as vehicles for drug delivery. J Control Release 24:119–132. https://doi.org/10.1016/0168-3659(93)90172-2
Miao J, Du Y, Yuan H, Zhang X, Li Q, Rao Y, Zhao M, Hu F (2015) Improved cytotoxicity of paclitaxel loaded in nanosized lipid carriers by intracellular delivery. J Nanopart Res 17:10–22. https://doi.org/10.1007/s11051-014-2852-x
Mitri K, Shegokar R, Gohla S, Anselmi C, Muller RH (2011) Lipid nanocarriers for dermal delivery of lutein: preparation, characterization, stability and performance. Int J Pharm 414:267–275. https://doi.org/10.1016/j.ijpharm.2011.05.008
Mohanraj V, Chen Y (2006) Nanoparticles—a review. Trop J Pharm Res 5:561–573. https://doi.org/10.4314/tjpr.v5i1.14634
Muller RH, Mader K, Gohla S (2000) Solid lipid nanoparticles (SLN) for controlled drug delivery—a review of the state of the art. Eur J Pharm Biopharm 50:161–177. https://doi.org/10.1016/S0939-6411(00)00087-4
Naahidi S, Jafari M, Edalat F, Raymond K, Khademhosseini A, Chen P (2013) Biocompatibility of engineered nanoparticles for drug delivery. J Control Release 166:182–194. https://doi.org/10.1016/j.jconrel.2012.12.013
Schedle A, Samorapoompichit P, Rausch-Fan XH, Franz A, Fureder W, Sperr WR, Sperr W, Ellinger A, Slavicek R, Boltz-Nitulescu G, Valent P (1995) Response of L-929 fibroblasts, human gingival fibroblasts, and human tissue mast cells to various metal cations. J Dent Res 74:1513–1520. https://doi.org/10.1177/00220345950740081301
Selvamuthukumar S, Velmurugan R (2012) Nanostructured lipid carriers: a potential drug carrier for cancer chemotherapy. Lipids Health Dis 11:159–166. https://doi.org/10.1186/1476-511X-11-159
Shao Z, Shao J, Tan B, Guan S, Liu Z, Zhao Z, He F, Zhao J (2015) Targeted lung cancer therapy: preparation and optimization of transferrin-decorated nanostructured lipid carriers as novel nanomedicine for co-delivery of anticancer drugs and DNA. Int J Nanomedicine 10:1223–1233. https://doi.org/10.2147/IJN.S77837
Sharma US, Balasubramanian SV, Straubinger RM (1995) Pharmaceutical and physical properties of paclitaxel (Taxol) complexes with cyclodextrins. J Pharm Sci 84:1223–1230. https://doi.org/10.1002/jps.2600841015
Swidan SA, Ghonaim HM, Samy AM, Ghorab MM (2016) Comparative study of solid lipid nanoparticles and nanostructured lipid carriers for in vitro Paclitaxel delivery. J Chem Pharm Res 8:482–493
Tosta FV, Andrade LM, Mendes LP, Anjos JLV, Alonso A, Marreto RN, Lima EM, Taveir SF (2014) Paclitaxel-loaded lipid nanoparticles for topical application: the influence of oil content on lipid dynamic behavior, stability, and drug skin penetration. J Nanopart Res 16:2782–2793. https://doi.org/10.1007/s11051-014-2782-7
Tran TH, Ramasamy T, Truong DH, Choi HG, Yong CS, Kim JO (2014) Preparation and characterization of fenofibrate-loaded nanostructured lipid carriers for oral bioavailability enhancement. AAPS PharmSciTech 15:1509–1515. https://doi.org/10.1208/s12249-014-0175-y
Trickler WJ, Nagvekar AA, Dash AK (2008) A novel nanoparticle formulation for sustained paclitaxel delivery. AAPS PharmSciTech 9:486–493. https://doi.org/10.1208/s12249-008-9063-7
USP 36-NF 34 (2016) The United States Pharmacopeia and National Formulary. United States Pharmacopeial Convention, Rockville
Videira M, Almeida AJ, Fabra À (2012) Preclinical evaluation of a pulmonary delivered paclitaxel-loaded lipid nanocarrier antitumor effect. Nanomedicine 8:1208–1215. https://doi.org/10.1016/j.nano.2011.12.007
Wang Y, Zhang H, Hao J, Li B, Li M, Xiuwen W (2016) Lung cancer combination therapy: co-delivery of paclitaxel and doxorubicin by nanostructured lipid carriers for synergistic effect. Drug Deliv 23:1398–1403. https://doi.org/10.3109/10717544.2015.1055619
Weber S, Zimmer A, Pardeike J (2014) Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) for pulmonary application: a review of the state of the art. Eur J Pharm Biopharm 86:7–22. https://doi.org/10.1016/j.ejpb.2013.08.013
Wissing SA, Kayser O, Muller RH (2004) Solid lipid nanoparticles for parenteral drug delivery. Adv Drug Deliv Rev 56:1257–1272. https://doi.org/10.1016/j.addr.2003.12.002
Wu L, Tang C, Yin C (2010) Folate-mediated solid-liquid lipid nanoparticles for paclitaxel-coated poly(ethylene glycol). Drug Dev Ind Pharm 36:439–448. https://doi.org/10.3109/03639040903244472
Xu W, Lee M-K (2015) Development and evaluation of lipid nanoparticles for paclitaxel delivery: a comparison between solid lipid nanoparticles and nanostructured lipid carriers. J Pharm Investig 45:675–680. https://doi.org/10.1007/s40005-015-0224-x
Yang Y, Corona A 3rd, Schubert B, Reeder R, Henson MA (2014) The effect of oil type on the aggregation stability of nanostructured lipid carriers. J Colloid Interface Sci 418:261–272. https://doi.org/10.1016/j.jcis.2013.12.024
Yu S, Zhang Y, Wang X, Zhen X, Zhang Z, Wu W, Jiang X (2013) Synthesis of paclitaxel-conjugated beta-cyclodextrin polyrotaxane and its antitumor activity. Angew Chem Int Ed Engl 52:7272-7277. doi: https://doi.org/10.1002/anie.201301397
Zhang XG, Miao J, Dai YQ, Du YZ, Yuan H, Hu FQ (2008) Reversal activity of nanostructured lipid carriers loading cytotoxic drug in multi-drug resistant cancer cells. Int J Pharm 361:239-244. https://doi.org/10.1016/j.ijpharm.2008.06.002
Zhang W, Shi Y, Chen Y, Hao J, Sha X, Fang X (2011) The potential of Pluronic polymeric micelles encapsulated with paclitaxel for the treatment of melanoma using subcutaneous and pulmonary metastatic mice models. Biomaterials 32:5934-5944. https://doi.org/10.1016/j.biomaterials.2011.04.075
Zhao S, Yang X, Garamus VM, Handge UA, Berengere L, Zhao L, Salamon G, Willumeit R, Zou A, Fan S (2014) Mixture of nonionic/ionic surfactants for the formulation of nanostructured lipid carriers: effects on physical properties. Langmuir 30:6920-6928 https"//doi.org/10.1021/la501141m
Zheng N, Gao Y, Ji H, Wu L, Qi X, Liu X, Tang J (2016) Vitamin E derivative-based multifunctional nanoemulsions for overcoming multidrug resistance in cancer. J Drug Target 24:663-669 https://doi.org/10.3109/1061186X.2015.1135335
Funding
The authors would like to thank Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG-Brazil), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq-Brazil), and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES-Brazil) for their financial support and scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
de Sousa Marcial, S.P., Carneiro, G. & Leite, E.A. Lipid-based nanoparticles as drug delivery system for paclitaxel in breast cancer treatment. J Nanopart Res 19, 340 (2017). https://doi.org/10.1007/s11051-017-4042-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11051-017-4042-0