Abstract
Background
A reformulated skin test for coccidioidomycosis, Spherusol®, was recently approved for use in the USA. We hypothesized that it could be useful in predicting severity of illness and outcome in various types of coccidioidomycosis.
Methods
Subjects with non-meningeal coccidioidomycosis attending a clinic in the coccidioidal endemic region were skin tested with Spherusol® and clinical data were collected at the time of testing and at follow-up.
Results
Twenty-seven subjects were studied, eight of whom had extrathoracic dissemination. A total of 15 subjects had positive tests, including 11 of 19 subjects with non-disseminated pulmonary disease and four with extrathoracic disseminated coccidioidomycosis. Among those with non-disseminated pulmonary disease, age ≥ 65 years, female sex, and antifungal therapy were significantly associated with a negative test on univariate but not multivariate analysis. For 23 subjects, there was a trend for those not on antifungal therapy at the time of follow-up to have a positive test but no association with coccidioidal complement-fixation titer or overall outcome.
Conclusions
Not all subjects with non-disseminated pulmonary coccidioidomycosis were found to be skin test positive and half of those with extrathoracic disseminated disease manifested dermal hypersensitivity. In this small study, the results of the skin test were not clinically predictive of disease severity or outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coccidioidomycosis is a fungal infection due to the dimorphic fungi Coccidioides immitis and C. posadasii. It is endemic to large parts of the southwestern United States and is particularly prevalent and increasing in California and Arizona [1, 2]. The cellular immune response is thought to play a critical role in controlling coccidioidal infection and expression of that response is thought to confer lifelong immunity and reduced risk for dissemination and recurrence [3,4,5].
The classic procedure to assess cellular immunity is the measurement of delayed-type hypersensitivity after intradermal injection of an antigen preparation [6]. Smith and colleagues pioneered its use in coccidioidomycosis by using a preparation derived from the mycelial form of multiple strains of Coccidioides [7]. Subsequently, Levine and Stevens [8, 9] reported on a spherule-based preparation, called spherulin that was found to be more sensitive than mycelial-based coccidioidin. However, nonspecific reactions were later observed [10] and these were subsequently ascribed to thimerosal, a mercury-containing compound used as a preservative in the skin test. In 2000, spherulin became unavailable in the USA. A new preparation, named Spherusol®, was derived from original lots of spherulin in which the thimerosal had been diluted to a concentration of 1:1,000,000 and phenol was substituted as the preservative. A study of individuals with primary pulmonary coccidioidomycosis demonstrated that 52 of 53 subjects aged 23–64 years demonstrated delayed-type hypersensitivity to Spherusol® as manifested by ≥ 5 mm of induration 48 h after placement of the test. Alternatively, one of the 59 healthy subjects without pneumonia, aged 18–56 years, living outside of the coccidioidal endemic region had a positive test. This led to a calculated sensitivity of 98.0% and a specificity of 98.3% [11]. Based on this work, Spherusol® was approved for use and marketed in the USA specifically for individuals aged 18–64 years with a history of pulmonary coccidioidomycosis.
The use of Spherusol® has been proposed to be broader than the parameters of the initial study, including using it as a prognostic indicator for outcome [12, 13]. To examine the use of Spherusol® under a variety of clinical circumstances as it might be used in practice, we placed the skin tests on a group of subjects attending a clinic specializing in coccidioidomycosis at a Veterans Affairs medical center located within the coccidioidal endemic region. Our hypothesis was that those with pulmonary coccidioidomycosis would react nearly universally while those with extrathoracic disseminated infection would not. Moreover, we thought that those who developed a positive reaction would also be more likely to have an uncomplicated course of coccidioidomycosis compared to those who did not react to the test.
Materials and Methods
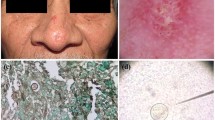
Adult patients with non-meningeal coccidioidomycosis seen in the clinic at the Southern Arizona Veterans Affairs Health Care System were eligible for the study. Because patients with coccidioidal meningitis are known to express delayed-type hypersensitivity to coccidioidal antigens and have a poor prognosis, they were excluded from the study. Eligible subjects with coccidioidomycosis were identified at each weekly clinic and asked to participate as they arrived. The precise weekly schedule was variable based on the availability of technical support to place and subsequently read the skin test. No list of declinations to participate among those potential subjects who were asked was kept. Because of this, the total number of subjects asked to participate is not known. After informed consent, 0.1 mL of Spherusol® was injected intradermally into the volar surface of either the right or left arm. After 48 h, the subject returned and the maximum diameter of induration was read and recorded. Palpable induration ≥ 5 mm was considered as positive.
Basic clinical data at the time of skin test placement were collected and correlated with the skin test result. A retrospective chart review was subsequently performed, and data that included the clinical outcome as related to coccidioidomycosis were collected. Statistical analysis was performed using Stata® 14.0. Discrete variables were tabulated and assessed using the χ2 test as well as logistic multivariable regression.
Results
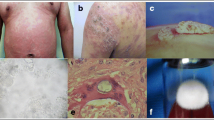
A total of 27 subjects had Spherusol® skin tests placed between February 2014 and June 2017. The clinical information on these subjects is shown in Table 1. The median age was 63 years, 24 were men, and six were African-American. Twenty-two had some underlying disease and seven were on immunosuppressive medication, including five on prednisone and two on a tumor necrosis factor-α antagonist. Thirteen were on antifungal therapy, all triazoles, including fluconazole in eight, itraconazole in four, and voriconazole in one. Nineteen had pulmonary disease including ten with primary pneumonia, five with a cavity or nodule, and four who were serologically positive only. Among the eight with extrathoracic dissemination, six had involvement of a single site, and two had multiple sites affected. None had coccidioidal meningitis. The median time from original diagnosis to skin testing was 463 days.
A total of 15 subjects had positive skin test reactions, manifested as ≥ 5 mm of induration 48 h after placement. This included 11 of 19 subjects with non-disseminated pulmonary disease, and four of eight patients with extrathoracic disseminated coccidioidomycosis. The median diameter of the reaction in the nine subjects with a positive reaction in whom it was measured was 20 mm (range 13–30 mm) compared to 0 mm for the 12 subjects without reaction.
Results were analyzed for those 19 subjects without dissemination by comparing their skin test response to age, sex, race, time from diagnosis, underlying disease, immunosuppression, serological response, and antifungal medication. These results are shown in Table 2. A similar assessment was not performed for those with disseminated disease because of the relatively small numbers. Female sex, age ≥ 65 years, and receiving antifungal medication were all significantly associated with a negative skin test response. However, none of these factors was found to be significant on multivariate analysis. Because of the association of a negative skin test with female sex, the characteristics of these three women were examined more closely. All three were white and had pulmonary disease. Two were tested within 1 year of diagnosis. All had underlying illnesses including Sjögren’s syndrome, chronic lung disease, and malignancy, and two were on prednisone at the time of skin testing.
A retrospective chart review was conducted in May 2018. Among the 27, one subject was lost to follow-up and three others had a follow-up of fewer than 90 days. The follow-up for the remaining 23 subjects was 513 days (91–1304 days). Of these subjects, all were found to be stable or improved on follow-up but one. This was a 77-year-old white male with diabetes and coccidioidomycosis disseminated to the knee on fluconazole. He had a positive skin test on initial testing. Results for subjects with regard to antifungal therapy, their coccidioidal complement-fixation (CF) titer and their outcome at the time of follow-up in relation to their initial skin test result are shown in Table 3. On follow-up, 11 subjects were still on antifungal therapy, including ten who were receiving this at the time of the skin test. Thirteen were off antifungal therapy, including ten who were off at the time of skin testing. There was a trend for those not on antifungal therapy at follow-up to have had an initial positive skin test result (P = 0.062). Coccidioidal CF titer and overall outcome were not associated with skin test result.
Discussion
Although this is a small study, it represents a real-world clinical experience and there are several findings of importance. First, only nine of the 15 subjects with non-disseminated coccidioidomycosis were skin test positive. These results are at variance with the original Spherusol® study [11], where nearly all subjects with primary pulmonary disease expressed coccidioidal delayed-type hypersensitivity. The reasons for this are unclear. Placement or reading of the test, which can present challenges [6], are not likely causes since the team that conducted this study was the same one that performed a portion of the original study. A more probable explanation is that the current study included a different group of subjects, who were older, with underlying illnesses and immunosuppression, and who possibly had more severe and persistent disease.
In addition, half of the subjects with extrathoracic disseminated coccidioidomycosis displayed dermal hypersensitivity. Although unexpected, this has been observed by others, including in an early study by Smith and colleagues using coccidioidin [7]. In a study of 53 subjects with various types of coccidioidomycosis, Stevens and colleagues noted no correlation between skin test result and serological results, race, or severity of illness. They also found that patients with disseminated coccidioidomycosis could express delayed-type hypersensitivity to spherulin if they had achieved clinical stability [14]. Oldfield and colleagues conducted a retrospective review between 1973 and 1993 on the risk of relapse among 34 patients with various types of coccidioidomycosis excluding those with meningitis. Overall, seven of 14 patients with persistently negative coccidioidin skin test reactions subsequently relapsed compared to two of 19 with serially positive skin tests. Among ten patients with disseminated coccidioidomycosis who relapsed, two expressed delayed-type hypersensitivity to coccidioidin [4].
Factors found related to a failure to express delayed-type hypersensitivity to Spherusol® in those without disseminated disease were female sex, age ≥ 65 years and those receiving antifungal medication. These were not predictive on multivariate analysis. It is likely that these factors are indicators of patients with less intact immunity or more severe coccidioidomycosis. For example, all three women in the study failed to express delayed-type hypersensitivity to skin testing with Spherusol®. However, all had underlying disease and two were on prednisone. Based on this, the reasons for their lack of response probably relate to their underlying diseases and immunosuppression, not to their sex.
Since the approval of Spherusol®, there has only been one published study on its use. In that work, the test was used to identify inmates with and without prior coccidioidal infection who were incarcerated at California Department of Corrections facilities as part of a plan for risk stratification. Among the 36,789 tested, 3169 (8.6%) were positive. Skin test reactivity was more likely in non-Hispanic whites than African-Americans, with older age, and among those incarcerated at two facilities within the endemic coccidioidal compared to elsewhere. The data suggested that Spherusol® were a reliable indicator of past coccidioidal infection [15]. Since the skin test was used in this study to screen for prior infection, there were no data presented on its use during acute or persistent disease.
This study had several limitations. First, it comprised a very small cohort of subjects and results may not be valid for a larger subject group. Moreover, the small sample size made it difficult to examine the relationship between underlying factors and expression of coccidioidal delayed-type hypersensitivity, particularly in the group with extrathoracic disease. Subjects had also been diagnosed with coccidioidomycosis for a variable amount of time prior to skin testing and this may have affected the results. Further, no list was kept of the number who declined to participate. Knowing this might have revealed potential biases of the study as well as illuminate subject perceptions with regard to barriers to skin testing, such as the need for an injection, the risk of discomfort at the injection site, and the requirement for a return visit. Finally, no control skin tests were placed to assess for general cellular immune response reactivity. Despite these limitations, the results were disparate with expectations and suggest that the meaning of a positive or negative test is not necessarily an indicator of a protective or non-protective immune response to coccidioidomycosis in patients with ongoing coccidioidal infection. It is hoped that the observations made here will lead to larger studies to examine these issues in more detail.
References
Bezold CP, Khan MA, Adame G, Brady S, Sunenshine R, Komatsu K. Notes from the field: increase in coccidioidomycosis—Arizona, October 2017–March 2018. MMWR Morb Mortal Wkly Rep. 2018;67(44):1246–7. https://doi.org/10.15585/mmwr.mm6744a6.
Cooksey GS, Nguyen A, Knutson K, Tabnak F, Benedict K, McCotter O, et al. Notes from the field: increase in coccidioidomycosis—California, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(31):833–4. https://doi.org/10.15585/mmwr.mm6631a4.
Smith CE, Whiting EG, Baker EE, Rosenberger HG, Beard R, Saito MT. The use of coccidioidin. Am Rev Tuberc. 1948;57:330–60.
Oldfield EC 3rd, Bone WD, Martin CR, Gray GC, Olson P, Schillaci RF. Prediction of relapse after treatment of coccidioidomycosis. Clin Infect Dis. 1997;25(5):1205–10.
Ampel NM. Measurement of cellular immunity in human coccidioidomycosis. Mycopathologia. 2003;156(4):247–62.
Sokal JE. Editorial: measurement of delayed skin-test responses. N Engl J Med. 1975;293(10):501–2. https://doi.org/10.1056/NEJM197509042931013.
Smith CE, Beard RR, Whiting EG, Rosenberger HG. Varieties of coccidioidal infection in relation to the epidemiology and control of the diseases. Am J Public Health. 1946;36:1394–402.
Levine HB, Gonzalez-Ochoa A, Ten Eyck DR. Dermal sensitivity to Coccidioides immitis. A comparison of responses elicited in man by spherulin and coccidioidin. Am Rev Respir Dis. 1973;107(3):379–86.
Stevens DA, Levine HB, TenEyck DR. Dermal sensitivity to different doses of spherulin and coccidioidin. Chest. 1974;65(5):530–3.
Galgiani JN. Development of dermal hypersensitivity to coccidioidal antigens associated with repeated skin testing. Am Rev Respir Dis. 1986;134(5):1045–7.
Johnson R, Kernerman SM, Sawtelle BG, Rastogi SC, Nielsen HS, Ampel NM. A reformulated spherule-derived coccidioidin (Spherusol) to detect delayed-type hypersensitivity in coccidioidomycosis. Mycopathologia. 2012;174(5–6):353–8. https://doi.org/10.1007/s11046-012-9555-6.
Wack EE, Ampel NM, Sunenshine RH, Galgiani JN. The return of delayed-type hypersensitivity skin testing for coccidioidomycosis. Clin Infect Dis. 2015;61(5):787–91. https://doi.org/10.1093/cid/civ388.
Pappagianis D, Johnson SM. Revision and return of a coccidioidal skin test reagent. Mycopathologia. 2012;174(5–6):351–2. https://doi.org/10.1007/s11046-012-9578-z.
Stevens DA, Levine HB, Deresinski SC, Blaine LJ. Spherulin in clinical coccidioidomycosis. Chest. 1975;65(8):697–702.
Wheeler C, Lucas KD, Derado G, McCotter O, Tharratt RS, Chiller T, et al. Risk stratification with coccidioidal skin test to prevent valley fever among inmates, California, 2015. J Correct Health Care. 2018;24(4):342–51. https://doi.org/10.1177/1078345818792679.
Acknowledgements
The authors thank Suzette Chavez for her efforts on this project. This research was funded by Nielsen Biosciences, the manufacturer of Spherusol®. They had no role in the design or execution of the study, in the analysis of the data, or with the manuscript preparation or writing. Some of the data in this manuscript were presented at the 7th International Conference on Coccidioidomycosis held at the Stanford University School of Medicine in August 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest with regard to the preparation or publication of this manuscript.
Informed Consent
This research involved human subjects and informed consent was obtained from all subjects involved in this study. The study was reviewed and approved by the Human Subjects Independent Review Board and the Research Committee of the Southern Arizona Veterans Affairs Health Care System.
Additional information
Handling Editor: Vishnu Chaturvedi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ampel, N.M., Robey, I. & Nguyen, C.T. An Analysis of Skin Test Responses to Spherulin-Based Coccidioidin (Spherusol®) Among a Group of Subjects with Various Forms of Active Coccidioidomycosis. Mycopathologia 184, 533–538 (2019). https://doi.org/10.1007/s11046-019-00356-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-019-00356-5