Abstract
We investigated the clinical and mycological characteristics of four cases of mycotic keratitis caused by Aspergillus flavus that occurred from July 2014 to May 2015 at Çukurova University Hospital, Adana, Turkey. In a 10-month period, a total of 64 corneal smear/scrapings were examined from patients with suspected mycotic keratitis. Fungal cultures were positive in six of these patients, indicating a 9.4% incidence of mycotic keratitis in this region, including four cases of A. flavus and two cases of Fusarium spp. The predisposing factors, clinical presentation, and success of the therapeutic approaches were further evaluated. For all cases, topical voriconazole was the first choice of treatment. Surgical procedures were required to control infection in 3 of the 4 cases, including intrastromal voriconazole injection for two cases and keratoplasty for one case. Predisposing factors included trauma (two cases, 50%), contact lens use (one case, 25%), and previous ocular surgery (one case, 25%). The clinical presentations also differed, including a well-limited ulcer (one case), an ulcer with an irregular feathery margin (one case), and ulcers with satellite lesions (two cases). The mean duration between the time of presentation and definitive diagnosis by culture was 14 days (8–25 days). We observed that A. flavus keratitis can present with different underlying factors and clinical conditions. A combination of antifungal therapy and supportive surgical intervention may resolve infections caused by A. flavus in the cornea.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mycotic keratitis is a challenging condition in ophthalmological practice. Ocular trauma, particularly trauma caused by vegetative material, is reported as the most common predisposing risk factor [1, 2]. Treatment options are limited, and many cases require surgery to maintain corneal integrity [3, 4]. Overall, the most common causes of filamentous mycotic keratitis worldwide are the Aspergillus and Fusarium genera [5, 6]. In the Aspergillus group, Aspergillus fumigatus followed by Aspergillus flavus (section Flavi) are the most commonly encountered opportunistic pathogens causing systemic infections and the leading causes of superficial infections in humans [7]. These fungi are predominantly associated with infections of the respiratory tract, sinuses, eye, and skin, and are prevalent in hot and arid climates, such as North Africa [8], the Middle East [9], and India [1]. For example, among 1737 culture-proven cases of mycotic keratitis in India, Aspergillus species were identified in 200 (11.5%) cases, and A. flavus (75%) was the predominant species [1].
The local epidemiology of mycotic keratitis, which may vary from country to country, as can the therapeutic modalities and the susceptibility patterns of causative agents (particularly the Aspergillus species) against a limited number of antifungal compounds. Understanding these differences can be important for ophthalmologists and may guide personalized therapy [1, 2]. In the current study, we present four cases with culture-proven A. flavus keratitis at Çukurova University, Balcalı Hospital, in Adana, Turkey. We discuss the predisposing factors, clinical manifestations, and epidemiological characteristics of the causative agents, and we describe the management strategies that have a high probability of successfully treating this disease.
Case 1
A 23-year-old woman presented with ocular pain, photophobia, and a mild disturbance of visual acuity in her left eye; these symptoms had begun 5 days previously. She had been wearing soft contact lenses for the past 5 years to correct myopia. During the last couple of months, she had not complied with the rules of contact lens use and had been sleeping in her contact lenses and using tap water to clean the lens case. A medical examination revealed that her visual acuity was 20/400 in the left eye. A slit lamp examination showed a corneal infiltration with irregular margins (Fig. 1a). A corneal scraping was performed to obtain samples for microbiological examination. A wide-spectrum antibiotic treatment [vancomycin (50 mg/mL) and amikacin (20 mg/mL) drops, hourly instillation] was initiated. In the subsequent days, the corneal infection progressed and visual acuity decreased to the hand motion level (Fig. 1b). Treatment was changed to an antifungal regimen (topical voriconazole, hourly, and systemic ketoconazole twice a day). The first scraping samples were negative for retrieval of any microorganism. Corneal collagen cross-linking with UV-A and riboflavin was performed at day 18 to control progressive corneal melting and deep invasion of the infection, and an intrastromal voriconazole injection was given at the same session. A second scraping was performed on day 20, and numerous fungal hyphae were found by cytological examination. Fungal culture for 4 days revealed A. flavus. Real-time PCR analysis was also positive for Acanthamoeba in the second sample analysis, indicating a mixed infection, so topical propamidine isethionate (Brolene® 0.1% eye drop, Sanofi-Aventis) and chlorhexidine (0.02%) were added to the treatment. The clinical findings regressed in the following days, and the patient recovered completely by the third month (Fig. 1c). The patient’s visual acuity was 20/400 at the end of the 6-month follow-up.
Case 2
A 28-year-old man complained of redness, pain, and a white fleck in his left eye for the past 20 days. He was referred to our cornea clinic with a mild, but resistant, keratitis that had not resolved with several different topical antibiotics. His visual acuity was 20/200 in the affected eye. He was a worker at an iron-steel factory, and he described a minor ocular trauma involving splashed iron dust. A slit lamp examination showed a well-defined corneal ulcer with conjunctival inflammation (Fig. 2a). Mycotic keratitis was the main suspicion for this persistent corneal infection. A. flavus was identified after culture for 3 days. A topical voriconazole (10 mg/mL) drop was initiated hourly. His clinical response was rapid. His visual acuity improved to 20/50 at day 5 and 20/40 at day 7 (Fig. 2b). Repeated smear exams were negative. The clinical findings were stable at his 1-month follow-up examination. One year after presentation, the patient’s visual acuity was 20/20, although a mild stromal haze remained (Fig. 2c).
Case 3
A 56-year-old woman was referred with a history of ocular trauma inflicted by an umbrella tip to the right eye 1 month previously. She had pain, redness, and low visual acuity, and her symptoms were unresponsive to topical antibiotic treatment. Upon examination, visual acuity was hand motion level in the right eye. A slit lamp examination revealed a corneal ulcer, satellite infiltrates, and hypopyon (Fig. 3a). Mycotic keratitis was the primary diagnosis, so a corneal scraping was examined for culture and cytological purposes. Empirical treatment included a topical voriconazole (10 mg/mL) drop hourly, with the addition of a vancomycin drop six times a day and an amikacin drop six times a day to the treatment regimen to cover possible bacterial contamination. A. flavus grew day 3 on culture. The patient’s clinical signs progressed in the following days, despite the ongoing wide-spectrum topical antibiotic therapy (Fig. 3b). We then switched to an intrastromal voriconazole injection on day 12. None of these measures controlled the infection, so a penetrating keratoplasty was performed 24 days after the initial examination. Topical voriconazole (10 mg/mL) and cyclosporine A (drop 0.05%) were prescribed postoperatively. The corneal graft remained clear, and no infection recurred during the 6 months of follow-up. At the last visit, the patient’s visual acuity was 20/200, and the patient had developed a cataract (Fig. 3c).
Case 4
A 50-year-old man had a history of lattice corneal dystrophy in both eyes. Penetrating keratoplasty had been performed on the left eye 2 years previously. He complained of pain, redness, and reduced visual acuity in his left eye over the last 2 days. Ophthalmologic examination revealed low visual acuity (20/400), as well as an abscess formation on the corneal graft (Fig. 4a). His clinical features were nonspecific at presentation. Corneal smear samples were obtained for a microbiological examination. The initial suspicion was a mixed bacterial and fungal infection for this patient; therefore, a topical antibacterial treatment of vancomycin and amikacin was initiated to cover gram-positive and gram-negative bacteria. After a few days, the clinical picture had deteriorated rapidly. Visual acuity dropped to a hand motion level, corneal edema and infiltrate size increased, and hypopyon was visible. At this point, the clinical diagnosis was switched to mycotic keratitis because of the appearance of satellite lesions in the cornea (Fig. 4b). A. flavus was detected in cultures after 3 days of incubation. A topical voriconazole (10 mg/mL) drop was added to the treatment. Corneal collagen cross-linking, using ultraviolet light and riboflavin, was performed at day 6 to control melting and infection. A favorable clinical response was observed with this treatment, and the patient’s visual acuity increased to 20/400 by day 10 (Fig. 4c). Repeated cytological examinations revealed no other pathogens. The antifungal treatment was reduced and stopped within 5 months. Visual acuity was 20/200, and the infection had subsided completely at the last visit.
Fungal Strains
All the corneal scraping and smear samples were inoculated onto Sabouraud glucose agar (SGA; Merck, Darmstadt, Germany), potato dextrose agar (PDA; Merck), blood agar (Biomark, Pune, India), brain–heart infusion agar (Merck), and Endo agar (HiMedia, Mumbai, India) in the form of a “C” streak. The SGA and PDA plates were incubated at 30 °C for 7 days, and the other plates were incubated at 37 °C for 3 days. Clinical samples were reported “positive” when the fungal growth was seen only the “C” streaks at least two media [2]. Table 1 lists all the fungal strains identified in this study, including their origin, identification number, and antifungal susceptibility data. All isolates were subcultured on SGA at 30 °C for 7 days. Morphological identifications were confirmed using sequence-based analysis of the rDNA internal transcribed spacer (ITS) and β-tubulin regions, as described previously [10].
Phylogeny, Identification, and Nomenclature of the Genus Aspergillus
The section Flavi represents a great diversity of species that cause infections in humans, such as A. flavus, A. oryzae, A. tamarii, Petromyces alliaceus, A. nomius, A. quzitongi, A. beijingensis, and A. novoparasiticus [11]. The β-tubulin gene, calmodulin, and, to a lesser degree, the ITS are considered the target genes for identifying A. flavus [12]. Molecular and phenotypic data indicate different genetic lineages within A. flavus. In addition, a higher molecular heterogeneity for A. flavus is reported, which further classifies this section into three main clades [13].
Antifungal Susceptibility Testing
In vitro antifungal susceptibility testing was performed against amphotericin B (AMB), flucytosine (5FC), itraconazole (ITC), voriconazole (VRC), posaconazole (POS), fluconazole (FLC), caspofungin (CAS), and anidulafungin (AFG) using the broth microdilution method of the European Committee on Antimicrobial Susceptibility [14]. The geometric mean MICs and MECs for the eight antifungals across all isolates, in increasing order, were as follows: AFG 0.02 mg/L, CAS 0.15 mg/L, POS 0.41 mg/L, ITC 0.44 mg/L, AMB 1.25 mg/L, VRC 1.50 mg/L, FLC >64 mg/L, and 5FC >64 mg/L.
Discussion
We described four cases of A. flavus keratitis observed in a 10-month period at a university hospital in the subtropical climate of Adana, Turkey. Our aim was to discuss the etiologic agents, epidemiological features, clinical characteristics, and antifungal susceptibility profiles of the corresponding fungi isolated from these patients. Although agricultural work has been considered the most commonly reported risk factor for Aspergillus keratitis [1], we identified several different risk factors in this case series, including trauma, wearing contact lenses, and previous corneal surgery.
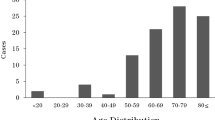
Over the 10-month period, a total of 64 corneal smear/scrapings were examined from patients with suspected mycotic keratitis. Overall, a corneal ulcer was detected in 7 (10.9%) of the cases. The fungal culture was positive for six patients with corneal ulcer, indicating a 9.4% incidence of mycotic keratitis in this region, including four cases of A. flavus and two cases of Fusarium spp. Notably, several studies have reported a seasonal difference, with a high prevalence of mycotic keratitis occurring between June and September [1]. Similarly, 3 of the 4 cases in our study appeared in September.
A study by Manikandan et al. [1] indicated that most (88%) of the mycotic keratitis cases occurred in adults, ranging from 21 to 70 years of age, and co-existing disease was diagnosed in 16.5% of these patients. Consistent with that study, all the patients in our study were adults, ranging from 23 to 56 years of age, but our cases had no history of systemic comorbidities. In addition, ocular trauma with vegetative materials, including soil, leaves, or tree branches, is the most reported source of mycotic keratitis, which is reported mainly in farmers and in agriculture-based tropical countries [1, 2].
In our study, the most difficult patient to treat (case 1) had a history of improper use of contact lenses, which had apparently led to serious complications, including mycotic keratitis [15]. In this patient, both Aspergillus and Acanthamoeba were detected coincidentally, both of which can cause sight-threatening complications. For this reason, the clinical course was more complicated in this case than in the others, and healing took 3 months.
Previously, Al-Wathiqi et al. [9] reported that the triazoles and echinocandins showed good activity against 92 clinical and 7 environmental A. flavus isolates. However, nearly 18% of the isolates showed a MIC >2 mg/L against AMB [9]. Consistent with those finding, Gonçalves et al. [11] tested 77 isolates belonging to Aspergillus section Flavi against 9 antifungals and reported that terbinafine and echinocandins demonstrated the lowest MICs and MECs, followed by posaconazole. Notably, AMB showed MICs ≥2 mg/L for 38 (49.4%) of the 77 isolates tested [11].
The treatment of mycotic keratitis is challenging because of the poor corneal penetration of medications and the limited efficacy of the available drugs. Voriconazole is a second-generation triazole that shows good corneal penetration [16]. Natamycin was not available, so we applied voriconazole therapy either as an empirical therapy or in culture-proven cases. Voriconazole is the drug of choice for treatment of Aspergillus spp. that show resistance to topical natamycin and amphotericin B [17]. Despite intensive antifungal treatment, perforation is not uncommon, so adjuvant treatments may be needed to prevent complications [18]. Intrastromal voriconazole injection can be used to achieve adequate intracorneal concentration of the drug [19, 20]. Amniotic membrane transplantation may also be warranted to control progressive melting [21].
Corneal collagen cross-linking is a novel therapeutic option for infectious keratitis. Cross-linking is effective as it has dual mechanisms: (1) it inactivates the pathogen by damaging nucleic acids and (2) it prevents enzymatic melting of the cornea [22, 23]. Several case reports confirm the beneficial effects of cross-linking as the primary treatment for small bacterial ulcers and as an adjuvant treatment for moderate to severe ulcers (of bacterial or fungal origin) [24, 25]. We performed cross-linking as an adjuvant treatment in cases 1 and 4. Symptomatic relief was clearly evident in the postoperative days, and the ulcers healed without complications. Based on these observations, cross-linking seems to be a safe and effective option for the management of mycotic keratitis.
In conclusion, we observed that A. flavus keratitis can present in response to several underlying factors and with different clinical conditions. In addition, our study suggests that mycotic keratitis caused by A. flavus may occur more often in a subtropical climate, such as in Adana, Turkey. A combination of antifungal therapy and supportive surgical intervention may successfully resolve the infection caused by A. flavus in the cornea.
References
Manikandan P, Varga J, Kocsube S, et al. Epidemiology of Aspergillus keratitis at a tertiary care eye hospital in South India and antifungal susceptibilities of the causative agents. Mycoses. 2013;56:26–33.
Thomas PA, Kaliamurthy J. Mycotic keratitis: epidemiology, diagnosis and management. Clin Microbiol Infect. 2013;19:210–20.
Jurkuna U, Behlau I, Colby K. Fungal keratitis: changing pathogens and risk factors. Cornea. 2009;28:638–43.
Chen WL, Wu CY, Hu FR, et al. Therapeutic penetrating keratoplasty for microbial keratitis in Taiwan from 1987–2001. Am J Ophthalmol. 2004;137:736–43.
Tanure MA, Cohen EJ, Sudesh S, et al. Spectrum of fungal keratitis at Wills Eye Hospital, Philadelphia, Pennsylvania. Cornea. 2000;19:307–12.
Thomas PA. Current perspectives on ophthalmic mycoses. Clin Microbiol Rev. 2003;16:730–97.
Hedayati MT, Pasqualotto AC, Warn PA, et al. Aspergillus flavus: human pathogen, allergen and mycotoxin producer. Microbiology. 2007;153:1677–92.
Cheikhrouhou F, Makni F, Neji S, et al. Epidemiological profile of fungal keratitis in Sfax (Tunisia). J Mycol Med. 2014;24:308–12.
Al-Wathiqi F, Ahmad S, Khan Z. Molecular identification and antifungal susceptibility profile of Aspergillus flavus isolates recovered from clinical specimens in Kuwait. BMC Infect Dis. 2013;13:126.
Samson RA, Visagie CM, Houbraken J, et al. Phylogeny, identification and nomenclature of the genus Aspergillus. Stud Mycol. 2014;78:141–73.
Gonçalves SS, Stchigel AM, Cano J, et al. In vitro antifungal susceptibility of clinically relevant species belonging to Aspergillus section Flavi. Antimicrob Agents Chemother. 2013;57:1944–7.
Tam EW, Chen JH, Lau EC, et al. Misidentification of Aspergillus nomius and Aspergillus tamarii as Aspergillus flavus: characterization by internal transcribed spacer, β-tubulin, and calmodulin gene sequencing, metabolic fingerprinting, and matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol. 2014;52:1153–60.
Gonçalves SS, Cano JF, Stchigel AM, et al. Molecular phylogeny and phenotypic variability of clinical and environmental strains of Aspergillus flavus. Fungal Biol. 2012;116:1146–55.
Subcommittee on Antifungal Susceptibility Testing of the ESCMID. European Committee for Antimicrobial Susceptibility Testing. EUCAST Technical Note on the method for the determination of broth dilution minimum inhibitory concentrations of antifungal agents for conidia-forming moulds. Clin Microbiol Infect. 2008;14:982–4.
Iyer SA, Tuli SS, Wagoner RC. Fungal keratitis: emerging trends and treatment outcomes. Eye Contact Lens. 2006;32:267–71.
Johnson LB, Kauffman CA. Voriconazole: a new triazole antifungal agent. Clin Infect Dis. 2003;36:630–7.
Mehta H, Mehta HB, Garg P, et al. Voriconazole for the treatment of refractory Aspergillus fumigatus keratitis. Indian J Ophthalmol. 2008;56:243–5.
Prajna NV, Mascarenhas J, Krishnan T, et al. Comparison of natamycin and voriconazole for the treatment of fungal keratitis. Arch Ophthalmol. 2010;128:672–8.
Sharma N, Agarwal P, Sinha R, et al. Evaluation of intrastromal voriconazole injection in recalcitrant deep fungal keratitis: case series. Br J Ophthalmol. 2011;95:1735–7.
Prakash G, Sharma N, Goel M, et al. Evaluation of intrastromal injection of voriconazole as a therapeutic adjunctive for the management of deep recalcitrant fungal keratitis. Am J Ophthalmol. 2008;146:56–9.
Lalitha P, Prajna NV, Kabra A, et al. Risk factors for treatment outcome in fungal keratitis. Ophthalmology. 2006;113:526–30.
Martins SA, Combs JC, Noguera G, et al. Antimicrobial efficacy of riboflavin/UVA combination (365 nm) in vitro for bacterial and fungal isolates: a potential new treatment for infectious keratitis. Invest Ophthalmol Vis Sci. 2008;49:3402–8.
Iseli HP, Thiel MA, Hafezi F, et al. Ultraviolet A/riboflavin corneal cross-linking for infectious keratitis associated with corneal melts. Cornea. 2008;27:590–4.
Makdoumi K, Backman A, Mortensen J, et al. Evaluation of antibacterial efficacy of photo-activated riboflavin using ultraviolet light (UVA). Graefes Arch Clin Exp Ophthalmol. 2010;248:207–12.
Said DG, Elalfy MS, Gatzioufas Z, et al. Collagen cross-linking with photoactivated riboflavin (PACK-CXL) for the treatment of advanced infectious keratitis with corneal melting. Ophthalmology. 2014;121:1377–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and the writing of the paper.
Rights and permissions
About this article
Cite this article
Erdem, E., Yagmur, M., Boral, H. et al. Aspergillus flavus Keratitis: Experience of a Tertiary Eye Clinic in Turkey. Mycopathologia 182, 379–385 (2017). https://doi.org/10.1007/s11046-016-0089-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-016-0089-1