Abstract
Chromoblastomycosis is a chronic subcutaneous mycosis caused by dematiaceous fungi. Fonsecaea monophora, a new species segregated from F. pedrosoi, may be the most prevalent pathogen of chromoblastomycosis in southern China. Herein, we report a rare case of chromoblastomycosis in a man with nephritic syndrome. He presented with an asymptomatic red plaque on the back of his left wrist that had appeared and enlarged over a period of 1.5 years, without any prior trauma. He was initially diagnosed with sporotrichosis. However, he did not respond to a 6-month course of potassium iodide treatment. The lesion slowly enlarged and became verrucous instead. Concurrently, a similar maculopapule appeared on his left forearm. Histopathological examination of a biopsy specimen indicated the presence of sclerotic bodies in the dermis. The fungus was identified as Fonsecaea spp. based on the results of a slide culture; in addition, the agent was confirmed to be F. monophora by using molecular methods. The patient demonstrated marked improvement after receiving appropriate antifungal therapy for 3 months. To our knowledge, this is the first case of chromoblastomycosis caused by F. monophora in an immunosuppressed patient. The identification of the agent by molecular techniques is important for epidemiological purposes. Thus, we believe that combination therapy with itraconazole and terbinafine would be a suitable option for infections caused by F. monophora.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chromoblastomycosis is a cutaneous and subcutaneous disease caused by dematiaceous fungi. Although such infections are noted in many countries, they appear to develop predominantly in tropical and subtropical regions, such as areas in Latin America, Africa, and Asia [1–6]. The infection develops mainly through the contamination of traumatic lesions in men who are engaged in farming. The lesions typically develop over a period of years and usually remain localized. However, the infection can also spread to other sites following direct contamination, autoinoculation, or hematogenous [7] or lymphatic spread [8]. The most frequent etiologic agents include Fonsecaea pedrosoi, Cladosporium carrionii, Phialophora verrucosa, and Rhinocladiella aquaspersa. Globally, F. pedrosoi is the most frequent cause of chromoblastomycosis [1–6]. However, during a recent taxonomic revision of the Fonsecaea genus, following molecular analysis, the three related species that most commonly cause human infections were found to be F. pedrosoi, F. monophora, and F. nubica [9]. F. monophora, a new species segregated from F. pedrosoi by De Hoog in 2004 [10], was shown to have a more variable clinical spectrum than F. pedrosoi. F. monophora, an opportunistic pathogen, is predominantly neurotropic in the human host, whereas F. pedrosoi and F. nubica seem to be associated exclusively with chromoblastomycosis [11, 12]. Most cases of chromoblastomycosis develop in otherwise healthy individuals; in fact, infections caused by F. monophora are rarely reported in immunocompromised patients [11, 12].
Here, we report a case of chromoblastomycosis, due to F. monophora, in a patient with nephritic syndrome; the patient was initially misdiagnosed with sporotrichosis. To our knowledge, this is the first such case to be reported in the literature. The isolated agent was finally identified based on an internal transcribed spacer (ITS) region sequence analysis of the ribosomal DNA (rDNA). Due to the likelihood of misdiagnosis, we emphasize the need for using molecular biological methods to accurately identify the fungal agent.
Case Report
A 57-year-old male farmer was prescribed prednisone (45 mg/day) for the treatment of nephritic syndrome. He presented to our outpatient department, in August 2012, with an asymptomatic red plaque on the back of his left wrist that had appeared and enlarged over a period of 1.5 years, without any prior trauma. Examination of the skin biopsy specimen from the lesion indicated the presence of spore structures in the dermis that were suggestive of a deep mycosis (Fig. 1). Fungal cultures of the biopsy specimen were grown on Sabouraud dextrose agar (SDA) at 27 °C for 40 days, but did not indicate any positive results. Based on these findings, the patient was diagnosed with sporotrichosis and was prescribed oral 10 % potassium iodide solution (15 mL, three times daily) for 6 months.
The first histopathological examination of the patient’s lesion show a dense, mixed inflammatory infiltrate containing lymphocytes, plasma cells, neutrophils, eosinophils, macrophages, and multinucleated giant cells in the dermis. A few spore structures (arrowhead) are seen outside the macrophages (periodic acid–Schiff stain; magnification, ×400)
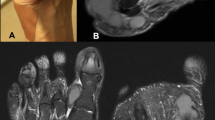
Although this treatment was administered, the lesion gradually increased in size, and another similar maculopapule appeared on his left forearm as well. A physical examination revealed a well-defined, 35 × 40 mm, infiltrated, erythematous plaque, with pale, gray scales, and black dots on the back of the patient’s left wrist. In addition, a 10 × 5 mm, erythematous papule had developed on his forearm (Fig. 2). Histopathological examination of a biopsy specimen, taken from the wrist lesion, indicated mild epidermal acanthosis and chronic granulomatous inflammation of the dermis. In addition, sclerotic bodies were observed in the abscess (Fig. 3a) and within giant cells (Fig. 3b).
Chronic granulomatous inflammation, consisting of lymphocytes, plasma cells, neutrophils, eosinophils, macrophages, and multinucleated giant cells, in the dermis. a Sclerotic bodies are observed in an abscess (periodic acid–Schiff stain; magnification, ×400). b The sclerotic bodies are present in giant cells (periodic acid–Schiff stain; magnification, ×400)
Mycological and Molecular Investigations
A fungal culture of the biopsy specimen was again performed on SDA at 27 °C. After 3 weeks, we observed dark brown colonies, covered with velvet-like mycelium and convex central protrusions (Fig. 4a). A microscopic examination of the slide culture showed abundant septate, dark brown hyphae, and suberect, highly branched conidiophores and unicellular ovoid conidia located either at the ends or on the sides of the conidiophores (Fig. 4b).
a Dark brown colonies, covered with velvet-like mycelium, with convex central protrusions, are seen in Sabouraud dextrose agar after culturing for 3 weeks, at 27 °C. b Microscopic features of the slide culture show septate, dark brown hyphae with suberect, highly branched conidiophores and ovoid conidia located either at the ends or on the sides of the conidiophores (magnification, ×400)
For further identification, the culture was transferred to a 1.5-mL Eppendorf tube, and the DNA was extracted using a simple boiling method. The DNA pellet was washed three times with 1.0 mL of 100 % ethanol for 10 min, centrifuged at 12,000×g for 10 min, and air-dried. Sodium caprylate solution (60 mL) was added to the Eppendorf tube, mixed for 10 min at room temperature, and centrifuged at 12,000×g for 5 min. The mixture was heated to 96 °C for 10 min and centrifuged at 12,000×g for 5 min. The top layer was removed and was added to a new tube and placed on ice. The DNA concentration was assessed using an ultraviolet spectrophotometer; a polymerase chain reaction (PCR) was performed by using universal primers such as ITS-1 (5′-TCC GTA GGT GAA CCT GCG G-3′) and ITS-4 (5′-TCC TCC GCT TAT TGA TAT GC-3′), which have been previously described [13, 14]. The 25-µL PCR amplification system included 12 µL of PCR pfu mix (dATP, dCTP, dGTP, dTTP, and pfu DNA Taq polymerase), 1 µL of each primer, 9 µL of double-distilled water, and 2 µL of the DNA sample. The PCRs were performed at 94 °C for 2 min, followed by 35 cycles of denaturation at 94 °C for 30 s, 47 °C for 15 s, and 72 °C for 1 min, as well as a final extension step at 72 °C for 10 min. The amplified products were loaded on a 2 % agarose gel in Tris–acetate–EDTA buffer and electrophoresed. The gel was stained using the GreenView Plus DNA Gel Stain (Applied BioProbes, Rockville, MD, USA) and visualized under ultraviolet light. Purification and sequence analysis were conducted at Invitrogen Life Technologies (Carlsbad, CA, USA). The DNA sequences of 18S DNA regions were submitted for BLAST analysis; a homology of 99.0 % to F. monophora (EF.513759.1.) was noted. The sequences were also submitted to the Centraalbureau voor Schimmelcultures for further identification; the strain showed 98.0 % similarity with F. monophora (CNRMAF/14-43).
After conclusively determining the causative pathogen, the patient was treated with terbinafine (500 mg/day) for 6 months, but no response was noted. Instead, the lesions gradually enlarged and became verrucous (Fig. 5a). Therefore, we switched the treatment to a combination of oral itraconazole, (400 mg/day), terbinafine (250 mg/day), and local heat therapy for 3 months. The patient exhibited partial remission of the lesions (Fig. 5b).
Discussion
Chromoblastomycosis is a chronic and disfiguring fungal infection. In China, C. carrionii is the causative fungus in the majority of cases in the northern part of the country, whereas F. pedrosoi is the main etiological agent in the southern part of the country [6]. Recently, Xi et al. [15] re-evaluated 24 isolates that were originally identified in chromoblastomycosis patients as F. pedrosoi. Using rDNA ITS sequence diversity, 20 of the strains were found to be F. monophora—this suggests that F. monophora may be the most prevalent chromoblastomycosis pathogen in southern China. F. pedrosoi and F. monophora are very similar in terms of morphology; however, F. monophora has a distinctive clinical aspect as compared to F. pedrosoi. Besides causing cutaneous and subcutaneous chromoblastomycosis, F. monophora also causes cerebral phaeohyphomycosis. In 2005, Surash et al. [11] reported a case of cerebral phaeohyphomycosis caused by F. monophora in an immunocompetent diabetic man. In 2007, Takei et al. [12] reported a case of cerebral phaeohyphomycosis, due to F. monophora, in a woman who had undergone liver transplantation. F. monophora appears to be likely to exhibit marked neurotropism, particularly in immunocompetent individuals. In fact, chromoblastomycosis, caused by F. monophora, primarily involves otherwise healthy individuals. To our knowledge, this is the first report of chromoblastomycosis caused by a F. monophora infection in a patient with nephritic syndrome who had an immunosuppressed state due to daily, oral prednisone use.
The clinical appearance of chromoblastomycosis is polymorphic. It usually presents as small papules and pustules and subsequently develops into nodules, tumors, verrucous lesions, plaques, and cicatrices; multiple morphologies are noted in most cases [6]. The fungus causing chromoblastomycosis usually only affects the subcutaneous tissue; however, cases of dissemination have also been reported and may primarily develop as a result of self-inoculation from the original lesion, hematogenous spread, or lymphatic spread [7, 8, 16]. Lesions complicated with ulcerations, edema, lymphedema, local pain or itching, or secondary bacterial infection may be particularly prone to metastases and self-inoculation. The host immune status is believed to play an important role in the clinical evolution of this disorder. In the present case, immunosuppression, resulting from daily, oral prednisone use, likely contributed to the spread of the left forearm lesion. Moreover, F. monophora exhibits a predisposition toward infecting sites other than the skin and the subcutaneous tissue and may thus spread through lymphatic or hematogenous pathways [11]. However, the spread of the infection through the lymphatic system, hematogenous route, or through autoinoculation cannot be confirmed in this patient.
Chromoblastomycosis can be clinically misdiagnosed as other types of infections or non-infectious lesions, such as skin tuberculosis [17], leprosy [18], squamous cell carcinoma [19], and psoriasis [20]. The diagnosis is routinely based on direct examination and cultures [21]. Direct mycological examination, a rapid diagnostic technique, has low specificity. In contrast, definitive fungal cultures are time-consuming. A chromoblastomycosis diagnosis can be easily made during a histopathological examination of a biopsy specimen in cases where the number of organisms is high and formation of “sclerotic bodies” is noted [22]. However, diagnoses are challenging for pathologists when (1) the number of organisms is low, (2) the lesion is not fully evolved (as in the early ulcer/plaque stage), and (3) there is no “clinical suspicion” of the infection [23]. In the present case, the patient was initially misdiagnosed with sporotrichosis, because the pathologist was unaware of the lesion, the number of organisms was low at the time of the first histopathological examination, and it lacked the characteristic sclerotic body morphology. In addition, various potential chromoblastomycosis pathogens present with similar macroscopic characteristics when cultured. Hence, molecular identification is required to ultimately identify the causative species. Although multiple PCR-based methods can be used for this identification, ITS sequence analysis is the most commonly used technique [13]. In the present case, F. monophora was identified via DNA sequence analysis of the rDNA ITS region. However, molecular identification is only important for epidemiological purposes, as in vitro studies indicate that there is no difference in the antifungal susceptibility of the different Fonsecaea species [24]. Nevertheless, there are differences among the different genera of chromoblastomycosis agents [25].
Although numerous treatments are available for chromoblastomycosis, including antimycotic agents, resection, local heat therapy, cryosurgery, and combination therapy, treatment remains a significant clinical challenge. Therapeutic success may be related to the causative agent, disease severity, choice of antifungal agent, and the host immune status. Itraconazole and terbinafine are common therapeutic medications for treating chromoblastomycosis [6]. Bonifaz et al. [26] treated four chromoblastomycosis patients with terbinafine (500 mg/day); three cases achieved clinical and mycological cure within a mean treatment period of 7 months. Yang et al. [13] reported that itraconazole therapy for Fonsecaea-associated chromoblastomycosis resulted in complete resolution of skin lesions after an average treatment duration of 4.1 months; relapses did not occur during a mean follow-up period of 43.4 months. However, in some cases, monotherapy with these antimycotics was unsatisfactory, and combination therapies may prove to be more effective due to their synergistic effects [13]. For example, Zhang et al. [27] reported the cases of two patients with chromoblastomycosis, caused by F. monophora, who were successfully treated with a combination of itraconazole and terbinafine. Zhang et al. [28] have also reported that itraconazole and terbinafine act synergistically against F. monophora isolates, using a checkerboard microdilution method. Therefore, the causative fungus, long-standing infection, multiple lesions, and host immunosuppression may have accounted for the poor response to terbinafine monotherapy in the present case.
In conclusion, we describe a rare case of chromoblastomycosis due to F. monophora, involving multiple lesions, in an immunosuppressed patient who was initially misdiagnosed with sporotrichosis. To correctly diagnose these infections, pathologists need to be more aware of the chromoblastomycosis lesions and the characteristic sclerotic body morphology. In addition, molecular identification should be encouraged to obtain accurate identification of the Fonsecaea species involved. Finally, itraconazole and terbinafine combination therapy may be a good therapeutic approach for this infection, particularly in immunocompromised patients.
References
Mouchalouat Mde F, Gutierrez Galhardo MC, Zancopé-Oliveira RM, et al. Chromoblastomycosis: a clinical and molecular study of 18 cases in Rio de Janeiro, Brazil. Int J Dermatol. 2011;50:981–6.
Pérez-Blanco M, Hernández Valles R, García-Humbría L, et al. Chromoblastomycosis in children and adolescents in the endemic area of the Falcón State, Venezuela. Med Mycol. 2006;44:467–71.
Kondo M, Hiruma M, Nishioka Y, et al. A case of chromomycosis caused by Fonsecaea pedrosoi and a review of reported cases of dematiaceous fungal infection in Japan. Mycoses. 2005;48(3):221–5.
Verma S, Verma GK, Singh G, et al. Facial chromoblastomycosis in sub-Himalayan region misdiagnosed as cutaneous leishmaniasis: brief report and review of Indian literature. Dermatol Online J. 2012;18:3.
Hofmann H, Choi SM, Wilsmann-Theis D, et al. Invasive chromoblastomycosis and sinusitis due to Phialophora verrucosa in a child from northern Africa. Mycoses. 2005;48:456–61.
Lu S, Lu C, Zhang J. Chromoblastomycosis in Mainland China: a systematic review on clinical characteristics. Mycopathologia. 2013;175:489–95.
Azulay RD, Serruya J. Hematogenous dissemination in chromoblastomycosis. Report of a generalized case. Arch Dermatol. 1967;95:57–60.
Muhammed K, Nandakumar G, Asokan KK, et al. Lymphangitic chromoblastomycosis. Indian J Dermatol Venereol Leprol. 2006;72:443–5.
Sun J, Najafzadeh MJ, van den Ende AHG, et al. Molecular characterization of pathogenic members of the genus Fonsecaea using multilocus analysis. PLoS One. 2012;7:e41512.
De Hoog GS, Attili-Angelis D, Vicente VA, et al. Molecular ecology and pathogenic potential of Fonsecaea species. Med Mycol. 2004;42:405–16.
Surash S, Tyagi A, de Hoog GS, et al. Cerebral phaeohyphomycosis caused by Fonsecaea monophora. Med Mycol. 2005;43:465–72.
Takei H, Goodman JC, Powell SZ. Cerebral phaeohyphomycosis caused by ladophialophora bantiana and Fonsecaea monophora: report of three cases. Clin Neuropathol. 2007;26:21–7.
Yang YP, Li W, Huang WM, Zhou Y, Fan YM. Chromoblastomycosis caused by Fonsecaea: clinicopathology, susceptibility and molecular identification of seven consecutive cases in Southern China. Clin Microbiol Infect. 2013;19:1023–8.
Daboit TC, Magagnin CM, Heidrich D, et al. A case of relapsed chromoblastomycosis due to Fonsecaea monophora: antifungal susceptibility and phylogenetic analysis. Mycopathologia. 2013;176:139–44.
Xi L, Sun J, Lu C, et al. Molecular diversity of Fonsecaea (Chaetothyriales) causing chromoblastomycosis in southern China. Med Mycol. 2009;47:27–33.
Verma GK, Verma S, Singh G, et al. A case of extensive chromoblastomycosis from North India. Braz J Microbiol. 2014;45:275–7.
Bandyopadhyay A, Majumdar K, Gangopadhyay M, et al. Cutaneous chromoblastomycosis mimicking tuberculosis verrucosa cutis: look for copper pennies! Turk Patoloji Derg. 2013;. doi:10.5146/tjpath.2013.01197.
Pavithran K. Chromoblastomycosis masquerading as tuberculoid leprosy. Int J Lepr Other Mycobact Dis. 1992;60:657–8.
Roy AD, Das D, Deka M. Chromoblastomycosis-A clinical mimic of squamous carcinoma. Australas Med J. 2013;6:458–60.
Lakshmi TS, Rao G, Shekhar VA. Chromoblastomycosis masquerading as palmo-plantar psoriasis. Indian J Dermatol Venereol Leprol. 1999;65:83–4.
Torres-Guerrero E, Isa-Isa R, Isa M, et al. Chromoblastomycosis. Clin Dermatol. 2012;30:403–8.
Chavan SS, Reddy P. Cytological diagnosis of chromoblastomycosis. J Cytol. 2013;30:276–7.
Chavan SS, Kulkarni MH, Makannavar JH. ‘Unstained’ and ‘de stained’ sections in the diagnosis of chromoblastomycosis: a clinico-pathological study. Indian J Pathol Microbiol. 2010;53:666–71.
Najafzadeh MJ, Badali H, Illnait-Zaragozi MT, et al. In vitro activities of eight antifungal drugs against 55 clinical isolates of Fonsecaea spp. Antimicrob Agents Chemother. 2010;54:1636–8.
Daboit TC, Massotti Magagnin C, Heidrich D, et al. In vitro susceptibility of chromoblastomycosis agents to five antifungal drugs and to the combination of terbinafine and amphotericin B. Mycoses. 2014;57:116–20.
Bonifaz A, Saúl A, Paredes-Solis V, et al. Treatment of chromoblastomycosis with terbinafine: experience with four cases. J Dermatolog Treat. 2005;16(1):47–51.
Zhang J, Xi L, Lu C, et al. Successful treatment for chromoblastomycosis caused by Fonsecaea monophora: a report of three cases in Guangdong. China Mycoses. 2009;52:176–81.
Zhang JM, Xi LY, Zhang H, et al. Synergistic effects of terbinafine and itraconazole on clinical isolates of Fonsecaea monophora. Eur J Dermatol. 2009;19:451–5.
Acknowledgment
Funding Sources — The National Natural Science Foundation of China (No. 81271771).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Tan, H., Xu, Y., Lan, Xm. et al. Chromoblastomycosis Due to Fonsecaea monophora in a Man with Nephritic Syndrome. Mycopathologia 179, 447–452 (2015). https://doi.org/10.1007/s11046-014-9856-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-014-9856-z