Abstract
Background
Parkinson’s disease (PD) is a progressive neurodegenerative disorder characterized by oxidative stress and neuroinflammation. Sofalcone (SFC), a chalcone derivative known for its antioxidative and anti-inflammatory properties, is widely used clinically as a gastric mucosa protective agent. However, its therapeutic potential in PD remains to be fully explored. In this study, we investigated the neuroprotective effects of SFC in a 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced PD mouse model.
Methods and results
We found that SFC ameliorated MPTP-induced motor impairments in mice, as assessed by the rotarod and wire tests. Moreover, SFC administration prevented the loss of dopaminergic neurons and striatal degeneration induced by MPTP. Subsequent investigations revealed that SFC reversed MPTP-induced downregulation of NRF2, reduced elevated levels of reactive oxygen species (ROS) and malondialdehyde (MDA), and increased total antioxidant capacity (TAOC). Furthermore, SFC suppressed MPTP-induced activation of microglia and astrocytes, downregulated the pro-inflammatory cytokine TNF-α, and upregulated the anti-inflammatory cytokine IL-4. Additionally, SFC ameliorated the MPTP-induced downregulation of phosphorylation of Akt at Ser473.
Conclusions
This study provides evidence for the neuroprotective effects of SFC, highlighting its antioxidative and anti-inflammatory properties and its role in Akt activation in the PD model. These findings underscore SFC’s potential as a promising therapeutic candidate for PD, warranting further clinical investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD), the second most prevalent neurodegenerative disorder after Alzheimer’s disease (AD), affects approximately 1% of individuals over the age of 60 [1, 2]. The pathological hallmark of PD is the selective and progressive degeneration of dopaminergic neurons in the substantia nigra pars compacta (SNpc) [3]. While various therapies target the resulting motor symptoms, they fail to halt the underlying neurodegenerative process of PD. Therefore, identifying effective neuroprotective drugs for PD is of paramount importance.
The exact pathogenesis of PD remains elusive; however, accumulating evidence suggests that oxidative stress and neuroinflammation play pivotal roles in the progression of PD [4]. Elevated levels of free radicals and proinflammatory mediators observed in the SN of both PD patients and animal models contribute to the degeneration of dopaminergic neurons [5]. Studies using PD animal models have shown that inhibiting oxidative stress and neuroinflammation can mitigate dopaminergic neuron degeneration [6]. Consequently, targeting oxidative stress and neuroinflammation is crucial for protecting dopaminergic neurons and developing therapeutic interventions for PD.
Sofalcone (SFC), chemically known as 20-carboxymethoxy-4,40-bis(3-methyl-2-butenyloxy) chalcone, has been demonstrated to possess anti-inflammatory and antioxidant properties [7] and is primarily employed as an anti-ulcer agent for gastric mucosa protection [8]. Structurally classified as a chalcone derivative, SFC is synthesized from soforadine, extracted from the roots of the Chinese plant Sophora subprostrata [9]. Recent research has identified chalcone derivatives as potential new therapeutics for PD, acting as promising enzyme inhibitors (MAO B, COMT, AChE), α-synuclein imaging probes and showing anti-neuroinflammatory activity (inhibition of iNOS or activation of Nrf2 signaling), as well as antagonists of adenosine A1 and/or A2A receptors [10]. In contrast to other chalcone derivatives, SFC has been clinically approved for treating gastric ulcers and gastritis in Japan for over two decades, confirming its safety and efficacy profile [11]. However, its potential role in PD remains unexplored. This study aims to investigate neuroprotective effects of SFC and elucidate the underlying mechanisms in a 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced PD animal model.
Materials and methods
Animals
Male C57BL/6 mice, weighing 22–26 g and aged 8 weeks, were sourced from Vital River Laboratory Animal Technology (Beijing, China). Prior to experimentation, the mice were acclimatized under controlled conditions with a constant temperature (24 ± 1 °C), humidity (50–70%), low noise (< 40 dB), and a 12-hour light/dark cycle. They were provided sterilized and disinfected food and water ad libitum. After a one-week habituation period, the mice were randomly assigned to one of three groups: Control (CTR), MPTP, and MPTP + SFC.
Drugs and treatments
MPTP was purchased from Sigma-Aldrich (purity: > 99%, Cat#: M0896) and dissolved in sterile saline. SFC was obtained from MCE (purity: > 98%, Cat#: HY-B2184) and suspended in 4% sodium carboxymethyl cellulose (CMC-Na). Mice in the MPTP and MPTP + SFC groups received intraperitoneal injections of MPTP (30 mg/kg) once daily for 5 consecutive days. In addition to MPTP injections, mice in the MPTP + SFC group were orally gavaged with SFC daily throughout the experimental period. Mice in the CTR group were administered with the same volume of 4% CMC-Na and sterile saline. Western blot, immunofluorescence and qPCR analyses were performed on the day following the last MPTP injection. Behavioral tests, immunohistochemistry and Nissl staining were conducted on the 21st day after the final MPTP injection. Please refer to Fig. 1A for a timeline schematic. This study was approved by the Ethics Committee of the Children’s Hospital of Chongqing Medical University (Approval number: CHCMU-IACUC20220323014).
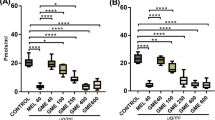
SFC treatment rescues motor dysfunctions in MPTP-induced PD mice. (A) A schematic of the experiment timeline. (B) The latency to fall off the rod in the rotarod test. (C) The latency to hanging on the iron rope in the wired test. n = 6–8/group. Data were expressed as mean ± SEM. **p < 0.01, ***p < 0.001
Antibodies
The following primary antibodies were used in this study: Anti-TH (Cell Signaling Technology, #58844, 1:1000), Anti-DAT (Abcam, ab184451, 1:1000), Anti-Akt (Cell Signaling Technology, 9272 S, 1:1000), Anti-p-Akt (Cell Signaling Technology, 4060 S, 1:1000), Anti-Nrf2 (Proteintech, 16396-1-AP, 1:1000), and Anti-β-actin (Transgen, HC201-02, 1:3000) for western blot analysis; Anti-TH (Millipore, AB9702, 1:1000), Anti-GFAP (Invitrogen, 13–0300, 1:500), and Anti-CD11b (Invitrogen, 14-0112-85, 1:500) for immunofluorescence; and Anti-TH (Cell Signaling Technology, #58844, 1:1000) for immunohistochemistry. The following secondary antibodies were also used: Anti-Mouse IgG (Goat), HRP-Labeled (Perkin-Elmer, NEF822001EA, 1:3000); Anti-Rabbit IgG (Goat), HRP-Labeled (Perkin-Elmer, NEF812001EA, 1:3000); Donkey Alexa Fluor™488 (Thermofisher, A21206, 1:1000); Rat Alexa Fluor™555 (Thermofisher, A78945, 1:500); and Chicken Alexa Fluor™647 (Thermofisher, A78952, 1:1000).
Rotarod test
Before the final assessment on the 21st day after the last MPTP injection, mice underwent a two-day training period on the rotarod. During training, mice were acclimated to a constant speed of 20 rpm for 3 min each day. For the formal test, mice were placed on the rotarod, which accelerated from 4 to 40 rpm. The test had a cut-off time of 300 s, and the latency to fall was recorded as the measure of motor coordination and balance.
Wired test
The device comprises two brackets and a U-shaped wire positioned 30 cm above the ground, cushioned to prevent injury from falls. Mice were suspended by their paws in the center of the wire, and the latency to fall was recorded. A two-day training period was implemented to acclimate mice and minimize stress, with each training session lasting 5 min. During the formal test, the maximum hanging time allowed was 600 s.
Preparation of brain samples
For biochemical experiments, mice were euthanized by cervical dislocation, SN tissues were collected and immediately placed on ice. All samples were subsequently transferred to a -80 °C freezer for long-term storage. For the morphological experiment, mice were anesthetized with 20% urethane and rapidly perfused with PBS and 4% PFA. After fixed in 4% PFA for 16 h at 4℃, brain tissues were dehydrated in 20% and 30% sucrose solutions, respectively, in sequence for 24 h at 4℃. Finally, brain tissues were embedded in tissue OCT-freeze medium to be cut into sections, with thicknesses of 20 μm for immunofluorescence and 40 μm for immunohistochemistry and Nissl’s staining. The different thicknesses were chosen to optimize visualization for the respective techniques. Brain sections were stored in cryoprotective fluid for preservation.
Immunohistochemistry
Brain sections were initially rinsed in PBS and subsequently incubated in 0.01 M PBST (PBS containing 0.3% Triton X-100) for 30 min. To eliminate endogenous peroxidase activity, the sections were then treated with 3% H2O2 for 45 min at room temperature. After washing twice with PBS, brain sections were blocked with diluted normal goat serum (150 µl in 10 ml PBS) at room temperature for 60 min, followed by overnight incubation with the anti-TH antibody at 4 °C. After washing three times in PBS, the sections were incubated with a secondary antibody at room temperature for 60 min. Subsequently, the sections were incubated with ABC dilution (Vector Laboratories, PK-6101) and stained with DAB (Vector Laboratories, SK-4105). Finally, brain sections were mounted onto slides, dehydrated, and permeabilized.
Nissl staining
The brain sections were rinsed twice in 1× PBS for 10 min, then mounted onto glass slides and air-dried. Subsequently, the slides were immersed in Nissl staining solution (Beyotime, C0117, China) at 45 °C for 45 min. After staining, they were dehydrated twice in 95% ethanol for 2 min each, followed by two rounds of clearing in xylene for 2 min each. Finally, the sections were mounted with neutral resin, air-dried and photographed.
Western blot
Brain tissues were lysed using Laemmli buffer at a ratio of 50 µL/mg of tissue. The Laemmli buffer composition included Tris-Cl (62.5 mM, pH 6.8), dithiothreitol (DTT, 8 mg/ml), sodium dodecyl sulfate (SDS, 2% w/v), glycerol (10% v/v), and bromophenol blue (BPB; 0.005% w/v). Lysates were boiled at 98 °C for 6 min, then separated by 7.5–12.5% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred onto polyvinylidene fluoride (PVDF) membranes (Bio-Rad, USA). The membranes were blocked with 5% non-fat dry milk in PBST (0.1% Tween-20) for 2 h at room temperature, followed by overnight incubation with primary antibodies at 4 °C. After washing, membranes were incubated with secondary antibodies for 2 h at room temperature. Subsequently, the membranes were visualized using the Bio-Rad Imager with enhanced chemiluminescence (ECL) developing solution (Bio-Rad, 1705061). Band intensities were quantified using ImageJ software and normalized to β-actin protein levels.
Measurement of dopamine content and oxidative stress-related indexes
We utilized the Mouse Dopamine ELISA Kit (DA, Jianglai Bio, JL11187) to quantify dopamine levels in striatum (STR) tissues. Oxidative stress analysis was conducted in SN tissues, including reactive oxygen species (ROS), malondialdehyde (MDA) and total antioxidant capacity (T-AOC), using commercial kits (E004-1-1 for ROS, A003-1 for MDA, and A015-2-1 for T-AOC) from Nanjing Jiancheng Bioengineering Institute (Nanjing, China), following the manufacturer’s instructions.
For dopamine measurement, samples were sequentially reacted with biotinylated detection antibody working solution, HRP conjugate working solution, substrate reagent, and stop solution. Absorbance at 532 nm was measured for quantification.
For ROS detection, single-cell suspensions of SN tissue were incubated with 10 µM DCFH-DA in PBS for 30 min at 37 °C. After washing with PBS, ROS levels were measured using a fluorescence microplate reader (excitation wavelength: 485 nm; emission wavelength: 550 nm).
For MDA detection, supernatants were combined with reagents 1, 2, and 3, followed by incubation at 95 °C for 60 min. After centrifugation, absorbance at 532 nm was measured.
T-AOC was assessed by mixing supernatants with solution ABTS and reagents 4, incubating for 6 min at room temperature, and recording absorbance at 405 nm.
Immunofluorescence
After washing, brain sections were permeabilized with a blocking solution for 1 h at room temperature. Subsequently, the sections were incubated with primary antibodies overnight at 4 °C, followed by incubation with secondary antibodies for 1 h at room temperature. Finally, images acquired using a confocal laser scanning microscope (Nikon A1R).
Reverse transcription-qPCR
Total RNAs were extracted from the SN tissues using the RNA extraction Kit (Spark jade, AC0202). The extracted RNA was reverse transcribed into cDNA using the reverse transcription kit (Takara, RR047A). The synthesized cDNA was subsequently amplified using SYBR Green (Roche, KK4601) for real-time PCR analysis. The following primer sequences were utilized: Il-4, forward: 5′-CAGCAACGAAGAAC ACCA-3′, reverse: 5′-CGAAAAGCCCGAAAGAG-3′; Tnf-α, forward: 5′-ATCGGTCCCCAAAGGGA TGA-3′, reverse: 5′-GCTACAGGCTTGTCACTCGAA-3′; Actb, forward: 5′-GGCTG TATTCCCCTC C ATCG-3′, reverse: 5′-CCAGTTGGTAACAATGCCATGT-3′.
Statistical analysis
All data were assessed for normal distribution and variance homogeneity using the Shapiro-Wilk and Brown-Forsythe tests, respectively. Statistical analyses were performed using One-way ANOVA with Tukey’s multiple comparison test and Fisher’s LSD test for comparisons between multiple groups, using GraphPad Prism 9.5 software. Results are presented as mean ± standard error of the mean (SEM), and statistical significance was set at P < 0.05.
Results
SFC alleviates motor deficits in MPTP-induced PD mice
We administered SFC to MPTP-induced PD mice to investigate its potential therapeutic efficacy. Initially, we employed two classical behavioral tests, the rotarod test and wire test, to assess the motor capabilities of the mice. In the rotarod test, mice in the MPTP-treated group exhibited a significantly reduced time spent on the rotating rod compared to the CTR group. However, administration of SFC resulted in a notable increase in the duration spent on the rod (Fig. 1B). Similarly, in the wire test, the MPTP group showed a shortened latency to fall compared to the CTR group, whereas SFC treatment extended the latency on the wire (Fig. 1C). These results collectively indicate that MPTP-induced mice experience impairments in coordinated movement and endurance, whereas SFC treatment ameliorates the motor deficits induced by MPTP.
SFC prevents MPTP-induced degeneration of dopaminergic neurons
Next, we conducted immunohistochemistry assays to evaluate tyrosine hydroxylase (TH)-positive neurons in the SN and TH-positive terminals in the STR. Our results revealed a significant reduction in the number of TH-positive neurons in the SN of MPTP-treated mice, while SFC treatment effectively mitigated this loss (Fig. 2A, B). Nissl staining further supported these findings, confirming genuine nigral neuronal loss rather than a mere reduction in TH expression (Fig. 2A, C). Similarly, in the STR, SFC treatment reduced the loss of TH-positive terminals compared to the MPTP-treated group (Fig. 2A, D). These findings demonstrate that SFC exerts neuroprotective effects on dopaminergic neurons in the MPTP-induced model.
SFC treatment reduces the MPTP-induced DA neurodegeneration. (A) Representative images of immunohistochemical staining of TH (left) in SN, Nissl body (middle) in SN and TH (right) in STR. Scale bar: 100 μm (SN), 500 μm (STR), n = 6–8/group. (B-D) Quantitative analysis of TH-positive neurons in SN (B), Nissl-stained neurons in SN (C) and TH-positive terminals in STR (D). Data were expressed as mean ± SEM. *p < 0.05, ***p < 0.001
SFC restores the function of dopaminergic neurons in the MPTP model
Since TH is the rate-limiting enzyme for dopamine production and dopamine transporter (DAT) is responsible for dopamine neurotransmission [12, 13], we assessed the functional integrity in the nigrostriatal dopamine system by detecting the expression of TH and DAT in SN and STR respectively. Western blot analysis indicated downregulation of TH and DAT expression in both SN and STR following MPTP administration, but mice treated with SFC exhibited significant restoration of TH and DAT expression (Fig. 3A-F). Furthermore, we quantified striatal dopamine content using an Enzyme-Linked Immunosorbent Assay (ELISA) kit. Our results revealed that SFC administration restored dopamine levels of the STR in the MPTP-induced model (Fig. 3G). Together, SFC reverses the dysfunction of dopaminergic neurons in the MPTP Model.
SFC treatment alleviates the expression of TH and DAT and restores the dopamine content in MPTP-induced PD mice. (A) Representative western blot images for TH and DAT expression in SN, n = 3–4/group. (B-C) Quantitative analysis of western blot bands for TH (B) and DAT (C) in SN, normalized to β-actin. (D) Representative western blot images for TH and DAT expression in STR, n = 4/group. (E-F) Quantitative analysis of western blot bands for TH (E) and DAT (F) in STR, normalized to β-actin. (G) Quantitative analysis of dopamine content detected by ELISA assay in STR, n = 5–6/group. Data were expressed as mean ± SEM. *p < 0.05, **p < 0.01, ***p < 0.001
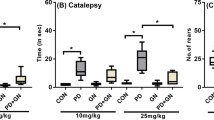
SFC attenuates MPTP-induced oxidative stress
MPTP disrupts complex I of oxidative phosphorylation, leading to reduced ATP production and increased ROS generation, resulting in oxidative stress and ultimately causing the death of dopaminergic neurons [14]. NRF2 is a crucial antioxidant protein [15], and studies have shown that SFC can activate NRF2 by covalently binding to Keap1 [7]. Therefore, we first observed the effect of SFC on NRF2 expression. Our findings revealed that NRF2 expression was downregulated in the MPTP model; however, treatment with SFC significantly restored NRF2 expression (Fig. 4A, B). Subsequently, we investigated the impact of SFC on oxidative stress. Our results demonstrated that MPTP-induced ROS and MDA levels were significantly elevated, accompanied by a marked reduction in TAOC, compared to the CTR group, indicating an imbalance in oxidative reactions following MPTP exposure (Fig. 4C-E). As expected, treatment with SFC led to a significant reduction in ROS and MDA levels and partially restored TAOC (Fig. 4C-E). These results suggest that SFC restores NRF2 expression in the MPTP model, thereby mitigating oxidative stress.
SFC treatment attenuates oxidative stress in MPTP-induced PD mice. (A) Representative western blot images for Nrf2 expression in SN, n = 5/group. (B) Quantitative analysis of western blot bands for Nrf2 normalized to β-actin. (C-E) Quantitative analysis of ROS (C), MDA (D) and T-AOC (E) in SN, n = 5–7/group. Data were expressed as mean ± SEM. *p < 0.05, **p < 0.01, ***p < 0.001
SFC inhibits MPTP-induced neuroinflammation
Neuroinflammation is a prominent pathological feature in PD patients [16]. The aberrant activation of microglia and astrocytes plays a pivotal role in neuroinflammation. When activated, they release inflammatory mediators and cytokines such as TNF-α and IL-1β, which can induce neuronal damage and death [17]. Research has reported that in the MPTP-induced PD animal model, activation of microglia and astrocytes leads to the death of dopaminergic neurons [18]. Previous studies have demonstrated that SFC inhibits the production of NO and TNF-α in a lipopolysaccharide (LPS)-treated co-culture system of RAW264.7 macrophages and 3T3-F442A adipocytes, thereby attenuating inflammation [19]. Therefore, we investigated whether SFC could inhibit inflammation in the MPTP model. Our results revealed that administration of MPTP significantly activated microglia and astrocytes in the SN. (Fig. 5A). However, treatment with SFC significantly inhibited the activation of microglia and astrocytes (Fig. 5A). Fluorescence quantitative analysis further confirmed these findings (Fig. 5B, C). Moreover, MPTP induced a significant upregulation of the level for the pro-inflammatory cytokine Tnf-α mRNA and downregulation of the level for the anti-inflammatory cytokine Il-4 mRNA (Fig. 5D-E). However, SFC treatment significantly suppressed the upregulation of the mRNA level of Tnf-α and upregulated the mRNA level of Il-4 (Fig. 5D-E). These results suggest that SFC inhibits the activation of microglia and astrocytes in the MPTP model, thereby suppressing neuroinflammation.
SFC treatment mitigates neuroinflammation of MPTP-induced PD mice. (A) Representative immunofluorescence staining of TH (Red), CD11b (Green) and GFAP (Green) in SN. Scale bar: 100 μm, n = 5–9/group. (B-C) Quantification of CD11b (B) and GFAP (C) fluorescence intensity in the SN. (D-E) Quantitative analysis of RT-qPCR for the mRNA of Tnf-α(D) and Il-4(E), n = 4–6/group. Data were expressed as mean ± SEM. *p < 0.05, **p < 0.01, ***p < 0.001
SFC restores the activity of Akt in the MPTP Model
Postmortem examination of PD patients reveal downregulation of p-Akt (Ser473) in dopaminergic neurons [20], whereas the phosphorylation of Ser473 is crucial for Akt activity [21]. Studies have demonstrated that activating Akt confers neuroprotective effects in PD models [22]. Therefore, we assessed whether SFC influences Akt activity by modulating phosphorylation at the Ser473 position in MPTP-induced PD mice. Our results demonstrate that MPTP administration decreased the level of Ser473 phosphorylation of Akt in the SN, while having no effect on total Akt (Fig. 6A-D). This indicates reduced Akt activity in the MPTP model, consistent with prior studies [23]. However, SFC treatment alleviated the downregulation of p-Akt (Ser473) induced by MPTP (Fig. 6A-D). These findings suggest that SFC can restore the activity of Akt in the MPTP model by modulating the phosphorylation of Akt at Ser473.
SFC treatment ameliorates the activity of Akt in MPTP-induced PD mice. (A) Representative western blot images for p-Akt (Ser473) and Akt expression in SN, n = 4/group. (B-D) Quantitative analysis of western blot bands for p-Akt (B) and Akt (C), which is normalized to β-actin; and the quantitative analysis for p-Akt/Akt (D). Data were expressed as mean ± SEM. *p < 0.05, **p < 0.01
Discussion
PD is a progressive neurodegenerative disorder characterized by motor dysfunction, for which current therapies only provide symptomatic relief without halting disease progression or degeneration of dopaminergic neurons. Thus, developing neuroprotective drugs is critical. In this study, we present novel findings demonstrating that SFC inhibits oxidative stress and neuroinflammation, while activating Akt in the MPTP-induced PD mouse model, thereby improving motor dysfunction and exerting neuroprotective effects.
SFC belongs to the chalcone derivatives, known for their ability to cross the blood-brain barrier due to their lipophilic nature and low polar surface area [24]. Several studies have demonstrated the neuroprotective effects of chalcone analogs in animal models of PD [25, 26]. Nevertheless, despite being one of the three chalcone drugs currently approved for clinical use [27], the therapeutic potential of SFC for PD remains unclear. Our results show that SFC ameliorated motor impairments and mitigated dopaminergic neuron loss and striatal degeneration induced by MPTP. Moreover, SFC reversed the downregulation of TH and DAT, restoring dopamine metabolism and transport in the MPTP model, ultimately normalizing dopamine levels in the STR. These findings provide initial evidence of the neuroprotective effects of SFC in an animal model of PD.
Oxidative stress is implicated in PD pathogenesis, and antioxidants have shown neuroprotective effects in PD models [28]. It has been reported that SFC can facilitate the dissociation of NRF2 from Keap1 by binding to Keap1, thereby inhibiting NRF2 degradation [7]. Our findings also show that SFC reversed the MPTP-induced downregulation of NRF2. Upon dissociation from Keap1, NRF2 translocates to the nucleus where it binds to antioxidant response elements (AREs), thereby promoting the transcription of multiple antioxidant proteins [29]. Further results also indicate that SFC significantly inhibits the production of ROS and MDA, and enhances the activity of T-AOC. These findings suggest that SFC may attenuate oxidative stress in the MPTP model by restoring NRF2 expression and subsequently enhancing the expression of antioxidant proteins.
Neuroinflammation is a key pathological feature of PD, and targeting neuroinflammation is considered a potential target for PD treatment [30]. Previous research has demonstrated that SFC significantly attenuates the production of inflammatory mediators such as NO, TNF-α, and MCP-1 in co-cultures of RAW264.7 macrophages and 3T3-F442A adipocytes stimulated with LPS [19]. Additionally, SFC has been shown to inhibit inflammation by targeting HMGB1 in Caco-2 cells [31]. In our study using PD animal models, we observed that SFC administration effectively suppressed the activation of microglia and astrocytes, reduced the expression of the pro-inflammatory cytokine TNF-α, and increased the expression of the anti-inflammatory cytokine IL-4. Other studies have reported that derivatives of chalcones, such as 2-hydroxy-3’,5,5’-trimethoxychalcone (DK-139), inhibit inflammation in BV2 cell models stimulated with LPS by targeting Toll-like receptor 4 (TLR4) [32]. Thus, further investigations are warranted to elucidate the precise mechanism through which SFC modulates neuroinflammation in PD models.
Akt is a pivotal pro-survival protein whose activity is enhanced by phosphorylation at the Ser473 site. Studies have established that activation of Akt in the MPTP model confers neuroprotective effects through the Akt/Gsk3β and Akt/mTOR signaling pathways [33, 34]. Our results demonstrate that SFC administration significantly prevented MPTP-induced downregulation of p-Akt, thereby restoring Akt activity in the MPTP model. Previous studies have reported that Akt activation can suppress oxidative stress in AD mouse models via the Akt/Nrf2/Ho-1 pathway [35], and activation of the AKT/FoxO1 pathway reduces TLR4 expression, thereby inhibiting neuroinflammation [36]. Therefore, SFC may inhibit oxidative stress and neuroinflammation in the MPTP model by restoring Akt activity.
Conclusions
In conclusion, our findings provide the first evidence that SFC can attenuate neurodegeneration and improve motor deficits by inhibiting oxidative stress and neuroinflammation and activating Akt in the MPTP-induced PD model. This study broadens the therapeutic potential of SFC and underscores its promise as a neuroprotective agent for the treatment of PD.
Data availability
The datasets generated or analyzed during this study are available from the corresponding author upon reasonable request.
Abbreviations
- AD:
-
Alzheimer’s disease
- DAT:
-
Dopamine transporter
- MDA:
-
Malondialdehyde
- MPTP:
-
1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine
- PD:
-
Parkinson’s disease
- ROS:
-
Reactive oxygen species
- SFC:
-
Sofalcone
- SN:
-
Substantia nigra
- STR:
-
Striatum
- T-AOC:
-
Total antioxidant capacity
- TH:
-
Tyrosine hydroxylase
References
Draoui A, El Hiba O, Aimrane A, El Khiat A, Gamrani H (2020) Parkinson’s disease: from bench to bedside. Rev Neurol (Paris) 176:543–559
Samii A, Nutt JG, Ransom BR (2004) Parkinson’s disease. Lancet 363:1783–1793
Dickson DW (2018) Neuropathology of Parkinson disease. Parkinsonism Relat Disord 46(Suppl 1):S30–S33
Chakrabarti S, Bisaglia M (2023) Oxidative Stress and Neuroinflammation in Parkinson’s Disease: The Role of Dopamine Oxidation Products. Antioxid (Basel) 12
He J, Zhu G, Wang G, Zhang F (2020) Oxidative Stress and Neuroinflammation Potentiate Each Other to Promote Progression of Dopamine Neurodegeneration. Oxid Med Cell Longev. 2020: 6137521
Jiang T, Sun Q, Chen S (2016) Oxidative stress: a major pathogenesis and potential therapeutic target of antioxidative agents in Parkinson’s disease and Alzheimer’s disease. Prog Neurobiol 147:1–19
Kim W, Lee H, Kim S, Joo S, Jeong S, Yoo JW et al (2019) Sofalcone, a gastroprotective drug, covalently binds to KEAP1 to activate Nrf2 resulting in anti-colitic activity. Eur J Pharmacol 865:172722
Higuchi K, Watanabe T, Tanigawa T, Tominaga K, Fujiwara Y, Arakawa T (2010) Sofalcone, a gastroprotective drug, promotes gastric ulcer healing following eradication therapy for Helicobacter pylori: a randomized controlled comparative trial with cimetidine, an H2-receptor antagonist. J Gastroenterol Hepatol 25(Suppl 1):S155–160
Onda K, Tong S, Nakahara A, Kondo M, Monchusho H, Hirano T et al (2015) Sofalcone upregulates the nuclear factor (erythroid-derived 2)-like 2/heme oxygenase-1 pathway, reduces soluble fms-like tyrosine kinase-1, and quenches endothelial dysfunction: potential therapeutic for preeclampsia. Hypertension 65:855–862
Krolicka E, Kiec-Kononowicz K, Lazewska D (2022) Chalcones as Potential Ligands for the Treatment of Parkinson’s Disease. Pharmaceuticals (Basel) 15
Rona G, Zeke A, Miwatani-Minter B, de Vries M, Kaur R, Schinlever A et al (2022) The NSP14/NSP10 RNA repair complex as a pan-coronavirus therapeutic target. Cell Death Differ 29:285–292
Vidyadhara DJ, Somayaji M, Wade N, Yucel B, Zhao H, Shashaank N et al (2023) Dopamine transporter and synaptic vesicle sorting defects underlie auxilin-associated Parkinson’s disease. Cell Rep 42:112231
Daubner SC, Le T, Wang S (2011) Tyrosine hydroxylase and regulation of dopamine synthesis. Arch Biochem Biophys 508:1–12
Tryphena KP, Nikhil US, Pinjala P, Srivastava S, Singh SB, Khatri DK (2023) Mitochondrial Complex I as a Pathologic and Therapeutic Target for Parkinson’s Disease. ACS Chem Neurosci
de Vries HE, Witte M, Hondius D, Rozemuller AJ, Drukarch B, Hoozemans J et al (2008) Nrf2-induced antioxidant protection: a promising target to counteract ROS-mediated damage in neurodegenerative disease? Free Radic Biol Med 45:1375–1383
Guzman-Martinez L, Maccioni RB, Andrade V, Navarrete LP, Pastor MG, Ramos-Escobar N (2019) Neuroinflammation as a common feature of neurodegenerative disorders. Front Pharmacol 10:1008
Kwon HS, Koh SH (2020) Neuroinflammation in neurodegenerative disorders: the roles of microglia and astrocytes. Transl Neurodegener 9:42
Pajares M, Manda AIR, Bosca G, Cuadrado L (2020) A. Inflammation in Parkinson’s Disease: Mechanisms and Therapeutic Implications. Cells 9
Tanaka H, Nakamura S, Onda K, Tazaki T, Hirano T (2009) Sofalcone, an anti-ulcer chalcone derivative, suppresses inflammatory crosstalk between macrophages and adipocytes and adipocyte differentiation: implication of heme-oxygenase-1 induction. Biochem Biophys Res Commun 381:566–571
Malagelada C, Jin ZH, Greene LA (2008) RTP801 is induced in Parkinson’s disease and mediates neuron death by inhibiting akt phosphorylation/activation. J Neurosci 28:14363–14371
Liao Y, Hung MC (2010) Physiological regulation of akt activity and stability. Am J Transl Res 2:19–42
Long HZ, Cheng Y, Zhou ZW, Luo HY, Wen DD, Gao LC (2021) PI3K/AKT Signal Pathway: a target of Natural products in the Prevention and Treatment of Alzheimer’s Disease and Parkinson’s Disease. Front Pharmacol 12:648636
Liu Y, Geng L, Zhang J, Wang J, Zhang Q, Duan D et al (2018) Oligo-porphyran ameliorates neurobehavioral deficits in Parkinsonian mice by regulating the PI3K/Akt/Bcl-2 pathway. Mar Drugs 16
Mathew B, Mathew GE, Ucar G, Joy M, Nafna EK, Lohidakshan KK et al (2017) Monoamine oxidase inhibitory activity of methoxy-substituted chalcones. Int J Biol Macromol 104:1321–1329
Jing H, Wang S, Wang M, Fu W, Zhang C, Xu D (2017) Isobavachalcone attenuates MPTP-Induced Parkinson’s Disease in mice by inhibition of Microglial activation through NF-kappaB pathway. PLoS ONE 12:e0169560
Parambi DGT, Saleem U, Shah MA, Anwar F, Ahmad B, Manzar A et al (2020) Exploring the therapeutic potentials of highly selective oxygenated chalcone based MAO-B inhibitors in a Haloperidol-Induced Murine Model of Parkinson’s Disease. Neurochem Res 45:2786–2799
Melrose J, Smith MM (2022) Natural and semi-synthetic flavonoid Anti-SARS-CoV-2 agents for the treatment of long COVID-19 Disease and neurodegenerative disorders of Cognitive decline. Front Biosci (Elite Ed) 14:27
Percario S, da Silva Barbosa A, Varela ELP, Gomes ARQ, de Ferreira MES et al (2020) Nazare Araujo Moreira T, Oxidative Stress in Parkinson’s Disease: Potential Benefits of Antioxidant Supplementation. Oxid Med Cell Longev. 2020: 2360872
Liu S, Pi J, Zhang Q (2022) Signal amplification in the KEAP1-NRF2-ARE antioxidant response pathway. Redox Biol 54:102389
Cinar E, Tel BC, Sahin G (2022) Neuroinflammation in Parkinson’s Disease and its Treatment opportunities. Balkan Med J 39:318–333
Yang T, Liu D, Li Y, Zhang Y, Zhu Y, Zhang J et al (2023) Chemoproteomics reveals Sofalcone inhibits the inflammatory response of Caco-2 cells by covalently targeting HMGB1. Chem Commun (Camb) 59:8981–8984
Lee YH, Jeon SH, Kim SH, Kim C, Lee SJ, Koh D et al (2012) A new synthetic chalcone derivative, 2-hydroxy-3’,5,5’-trimethoxychalcone (DK-139), suppresses the toll-like receptor 4-mediated inflammatory response through inhibition of the Akt/NF-kappaB pathway in BV2 microglial cells. Exp Mol Med 44:369–377
Zhang W, He H, Song H, Zhao J, Li T, Wu L et al (2016), Neuroprotective Effects of Salidroside in the MPTP Mouse Model of Parkinson’s Disease: Involvement of the PI3K/Akt/GSK3beta Pathway. Parkinsons Dis. 2016: 9450137
Zheng M, Chen M, Liu C, Fan Y, Shi D (2021) Alkaloids extracted from Uncaria rhynchophylla demonstrate neuroprotective effects in MPTP-induced experimental parkinsonism by regulating the PI3K/Akt/mTOR signaling pathway. J Ethnopharmacol 266:113451
Ali T, Kim T, Rehman SU, Khan MS, Amin FU, Khan M et al (2018) Natural dietary supplementation of anthocyanins via PI3K/Akt/Nrf2/HO-1 pathways mitigate oxidative stress, neurodegeneration, and memory impairment in a mouse model of Alzheimer’s Disease. Mol Neurobiol 55:6076–6093
Guo LT, Wang SQ, Su J, Xu LX, Ji ZY, Zhang RY et al (2019) Baicalin ameliorates neuroinflammation-induced depressive-like behavior through inhibition of toll-like receptor 4 expression via the PI3K/AKT/FoxO1 pathway. J Neuroinflammation 16:95
Funding
This study was supported by National Natural Science Foundation of China (Grant No. 32371030 and 82071395), CQMU Program for Youth Innovation in Future Medicine (W0044) and Natural Science Foundation of Chongqing (grant No. CSTB2022NSCQ-BHX0022 and CSTB2024NSCQ-LZX0008).
Author information
Authors and Affiliations
Contributions
Mulan Chen: Investigation, Methodology, Validation, Data Curation, Formal analysis, Writing - Original Draft. Xin He: Methodology, Visualization, Project administration, Conceptualization, Writing - Review & Editing, Funding acquisition. Yepeng Fan: Investigation, Methodology. Lei Xia: Methodology. Zhifang Dong: Supervision, Writing - Review & Editing, Funding acquisition.
Corresponding author
Ethics declarations
Ethical approval
All experimental procedures were conducted in accordance with the Chongqing Science and Technology Commission guidelines and approved by the Animal Ethics Committee of Children’s Hospital of Chongqing Medical University (Approval number: CHCMU-IACUC20220323014).
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, M., He, X., Fan, Y. et al. Sofalcone attenuates neurodegeneration in MPTP-induced mouse model of Parkinson’s disease by inhibiting oxidative stress and neuroinflammation. Mol Biol Rep 51, 908 (2024). https://doi.org/10.1007/s11033-024-09852-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-024-09852-4