Abstract
Background
Overexpression of lysophosphatidylcholine acyltransferase 1 (LPCAT1) has been found in various solid cancers and is associated with disease progression, metastasis, and recurrence. However, the expression pattern of LPCAT1 in acute myeloid leukemia (AML) bone marrow remains unknown. The present study aimed to compare LPCAT1 expression differences in bone marrow samples from AML patients and healthy controls and assess the clinical relevance of LPCAT1 in AML.
Methods and results
LPCAT1 expression in bone marrow was significantly lower in AML than in healthy controls predicted by public databases. Furthermore, real-time quantitative PCR (RQ-PCR) validated that LPCAT1 expression in bone marrow was significantly down-regulated in AML compared to healthy controls [0.056 (0.000–0.846) vs 0.253 (0.031–1.000)]. The DiseaseMeth version 2.0 and The Cancer Genome Atlas analysis revealed that the LPCAT1 promoter was hypermethylated in AML, and there was a strong negative correlation between LPCAT1 expression and methylation (R = − 0.610, P < 0.001). RQ-PCR revealed that the frequency of LPCAT1 low expression was lower in the FAB-M4/M5 subtype than in the other subtypes (P = 0.018). The ROC curve revealed that LPCAT1 expression could serve as a potential diagnostic marker for differentiating AML from controls with an area under the ROC curve of 0.819 (95% CI 0.743–0.894, P < 0.001). In cytogenetically normal AML, patients with LPCAT1 low expression had significantly longer overall survival than those without LPCAT1 low expression (median 19 versus 5.5 months, P = 0.036).
Conclusions
LPCAT1 is down-regulated in AML bone marrow, and LPCAT1 down-regulation could be used as a potential biomarker for AML diagnosis and prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) is a malignant clonal disorder characterized by blocked differentiation and uncontrolled proliferation of immature myeloid progenitors in bone marrow [1]. Despite significant advances in treatment strategies, the prognosis of AML patients is still unsatisfactory [2, 3]. Cytogenetic aberrations play important roles in classifying diagnosis, evaluating prognosis, and guiding individual treatment [4, 5]. In addition to cytogenetic aberrations, molecular biological abnormalities including gene mutations and abnormal gene expressions such as ERG, BAALC, and MN1 have recently been associated with leukemogenesis and substantially impact the clinical outcome of AML patients [6, 7]. These findings support further research into leukemogenesis and the development of better diagnostic and prognostic biomarkers in AML, particularly cytogenetically normal AML (CN-AML).
Aberrant lipid metabolism is a well-known feature of cancer cells and affects numerous cancer-related cellular processes, including cell growth, proliferation, differentiation and motility [8]. Phosphatidylcholine (PC) is the predominant phospholipid in eukaryotic membranes [9], and its rapid turnover is thought to be required during cancer development. Lysophosphatidylcholine acyltransferase (LPCAT) is a family of enzymes responsible for converting lysophosphatidylcholine (LPC) to PC. To date, four LPCAT members have been identified, including LPCAT1, LPCAT2, LPCAT3, and LPCAT4 [10]. Among these members, LPCAT1 has attracted much attention in various cancers. Currently, LPCAT1 has been found to be overexpressed in various solid cancers, including prostate cancer [11], hepatocellular carcinoma [12,13,14,15,16], breast cancer [17, 18], endometrial cancer [19], oral squamous cell carcinoma [20], esophageal squamous cell carcinoma [21], cutaneous squamous cell carcinoma [22], and lung adenocarcinoma [23, 24] and its overexpression promoted the progression, metastasis, recurrence and worsened survival of these solid cancers. However, the pattern of LPCAT1 expression in the bone marrow and its clinical significance in AML have been rarely studied in AML. The present study aimed to determine the expression difference of LPCAT1 gene in bone marrow samples from AML patients and healthy controls and clinical relevance of altered LPCAT1 in primary AML patients.
Materials and methods
Patients and samples
The first cohort from Gene Expression Omnibus (GEO) was used in this study to compare the expression difference of the LPCAT1 gene in bone marrow from AML patients and healthy controls. The cohort included 252 AML patients (GSE13159) and 34 healthy donors (GSE42519). We used BloodSpot to investigate the LPCAT1 gene expression differences in these AML and healthy controls (https://servers.binf.ku.dk/bloodspot/?gene=LPCAT1&dataset=AML_MILE_VERHAAK_vs_nl). BloodSpot is a database of gene expression profiles and transcriptional programs for healthy and malignant hematopoiesis [25, 26]. Furthermore, another GSE9476 database was included in the study to analyze LPCAT1 expression differences in AML and normal controls both in bone marrow (7 AML, 10 controls) and peripheral blood samples (19 AML, 10 controls).
DNA methylation plays crucial roles in regulating gene expression. Therefore, the second cohort of 171 AML patients with LPCAT1 expression and methylation data from The Cancer Genome Atlas (TCGA) databases was included in the present study and used to analyze the association of LPCAT1 expression and methylation. Data were extracted from TCGA and analyzed. Furthermore, the methylation difference of LPCAT1 promoter between AML patients and normal controls was compared using DiseaseMeth version 2.0 (http://bio-bigdata.hrbmu.edu.cn/diseasemeth/analyze.html).
The third cohort of 39 healthy donors and 92 newly diagnosed AML patients treated at the Affiliated People’s Hospital of Jiangsu University were also enrolled and used in the validation stage for real-time quantitative PCR (RQ-PCR) of LPCAT1 expression. The cohort was also used to investigate the clinical significance of LPCAT1 expression. 92 de novo AML patients with cryopreserved bone marrow mononuclear cells (BMNCs) were enrolled in this study. The BMNCs samples collected from 39 healthy donors were used as controls. All patients signed written informed consent. The diagnosis and classification of AML patients were established according to French-American-British (FAB) and World Health Organization (WHO) criteria (blast ≥ 20%) combined to immunophenotyping and cytogenetic analysis [27,28,29,30]. Karyotypes were analyzed by conventional R-banding method and karyotype risk was classified according to the reported study [30]. All patients received supportive and symptomatic treatment and chemotherapy such as induction therapy and subsequent consolidation treatment, none of them were transplanted. The main clinical and laboratory features of the patient cohort were listed in Table 1. This study was approved by the Ethics Committee of the Affiliated People’s Hospital of Jiangsu University.
RNA isolation and reverse transcription
Total RNA was extracted from the BMNCs using Trizol reagent (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions. Reverse transcription was carried out using the reactions of random hexamers 10 mM, dNTPs 10 mM, RNase inhibitor 80 units, 200 units of MMLV reverse transcriptase (MBI Fermentas, Hanover, MD) and 2 µg of total RNA. The reverse transcription protocols were 25 °C for 10 min, 42 °C for 60 min, and then the cDNA was stored at − 20 °C.
Real-time quantitative PCR (RQ-PCR)
RQ-PCR was performed on a 7500 Thermo cycler (Applied Biosystems, CA, USA) to determine the LPCAT1 expression levels in bone marrow specimens from primary AML patients and healthy controls. The primer sequences of LPCAT1 expression were 5’- CGTGACCGACCTATTCCGAG -3’ (forward) and 5’- GTCTGAGTTTTCCGGGCTGA -3’ (reverse) with expected products of 205 bp. The reaction mixture with a final volume of 20 µL contained 20 ng cDNA, 0.8 µM of specific primers, 10 µM of AceQTM qPCR SYBR Green Master Mix (Vazyme Biotech Co., Piscataway, NJ, USA), and 0.4 µM of ROX Reference Dye 2 (Invitrogen, Carlsbad, CA, USA). PCR running protocols consisted of an initial denaturation step of 5 min at 95 °C, followed by an amplification program of 40 cycles of 10 s at 95 °C, 30 s at 56 °C, 32 s at 72 °C, and 32 s at 80 °C for collecting data. At the end of the PCR cycles, a melting program of 15 s at 95 °C, 60 s at 60 °C, 15 s at 95 °C, and 15 s at 60 °C was performed to validate the specificity of the expected PCR products. PCR products were sequenced randomly to verify the correctness of primers. For all experiments, positive and negative controls were included. The housekeeping gene ABL was used as the reference sequence to calculate the abundance of LPCAT1 mRNA. Relative expression levels of LPCAT1 were determined by the 2−ΔΔCt method using ABL levels for normalization.
Gene mutation detection
The detections of IDH1/2, DNMT3A, NRAS or KRAS, NPM1, C-KIT and U2AF1 mutations were performed by high-resolution melting analysis (HRMA) as reported previously [31,32,33,34]. All positive samples were confirmed by direct DNA sequencing. FLT3-ITD and CEBPA mutations were detected by direct DNA sequencing (BGI Tech Solutions Co., Shanghai, China) [35].
Statistical analysis
The Statistical Program for Social Sciences (SPSS) 17.0 software (SPSS, Chicago, IL, USA) was used to conduct the statistical analysis in this study. Pearson chi-square analysis and Fisher exact test were employed to compare the difference of categorical variables. Mann–Whitney’s U-test was performed to compare the difference of continuous variables. Spearman’s rank correlation was used to assess the correlation between LPCAT1 expression and methylation in the bone marrow. Kaplan–Meier method was applied to determine the prognostic value of LPCAT1 expression in AML. Receiver operating characteristic curve (ROC) and area under the ROC curve (AUC) were carried out to determine the value of LPCAT1 expression in distinguishing AML patients from normal controls. For all analyses, a two-tailed P value of 0.05 or less was considered statistically significant.
Results
Down-regulation of LPCAT1 in AML bone marrow
In the discovery stage, we used the BloodSpot database to analyze the variations in LPCAT1 mRNA levels in bone marrow specimens from 252 patients and 34 healthy controls. The results showed that LPCAT1 expression in bone marrow samples was lower in AML patients than in healthy controls (Fig. 1). Furthermore, the raw data from the GSE9476 database also revealed that LPCAT1 was down-regulated in AML bone marrow and peripheral blood specimens (Fig. 2A). In the validation stage, RQ-PCR results showed a significantly lower expression of LPCAT1 in bone marrow of AML patients compared to healthy controls [0.056 (0.000–0.846) vs 0.253 (0.031–1.000)] (P < 0.0001, Fig. 2B). RQ-PCR results were consistent with those from the BloodSpot and the GSE9476 databases, confirming that LPCAT1 was down-regulated in the bone marrow of AML patients.
The expression of LPCAT1 in bone marrow in AML vs normal from BloodSpot. The expression of LPCAT1 was determined using a microarray. The short horizontal lines represented the median expression for each subtype. The transverse line represented the cut-off value when the AML vs normal ratio was 1; the ratio was < 1 below or for > 1 above the line
Methylation of LPCAT1 gene and its correlation with LPCAT1 expression
DiseaseMeth version 2.0 and TCGA databases were used to seek the possible reasons for expression changes of LPCAT1 gene in AML. The LPCAT1 methylation difference between AML and controls was analyzed using DiseaseMeth version 2.0. A significant hypermethylation of LPCAT1 promoter was observed in AML compared to controls, as shown in Fig. 3A (P < 0.001). The TCGA database was used to explore the association between LPCAT1 expression and methylation. Data from the TCGA database showed a strong negative association between LPCAT1 expression and methylation (R =—0.610, P < 0.001, Fig. 3B).
The association of LPCAT1 expression and promoter methylation in AML. A LPCAT1 promoter methylation level was obtained from the human disease methylation database DiseaseMeth version 2.0 (http://bio-bigdata.hrbmu.edu.cn/diseasemeth/analyze.html). B Association of LPCAT1 genes expression and methylation among AML patients from the TCGA databases. The correlation analysis was performed by Spearman test
Correlation between LPCAT1 low expression and clinical characteristics in AML
To explore the clinical relevance of LPCAT1 expression in AML, the patients in the third whole-cohort were divided into two groups (low LPCAT1 expression and high LPCAT1 expression) based on a median value of 0.056. Clinical features and laboratory parameters representation between the two groups were listed in Table 1. There were no significant differences in sex, white blood cells, hemoglobin and platelets between low LPCAT1 expression and high LPCAT1 expression groups (P > 0.05). However, there was a trend that patients in LPCAT1 low-expressed group were younger than those in LPCAT1 high-expressed groups (P = 0.088). Further investigation revealed that LPCAT1 expression was positively correlated with patients’ age (R = 0.202, P = 0.05). LPCAT1 low expression could be observed in each AML subtype analyzed (Table 1). There were no significant differences in the frequency of LPCAT1 low expression among FAB subtypes (Table 1, P > 0.05). However, the frequency of LPCAT1 low expression in the FAB-M4/M5 subtype was lower than in other subtypes [34% (12/35) versus 60% (34/57), P = 0.018]. There was no statistically significant difference in the frequency of LPCAT1 low expression between patients with different karyotypes. Furthermore, no significant difference was observed in the distribution of gene mutations between patients with and without LPCAT1 low expression.
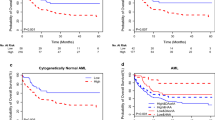
Evaluation of LPCAT1 expression as a potential diagnostic marker
ROC curve was performed to evaluate the capacity of LPCAT1 expression to distinguish AML patients from normal controls. It indicated that LPCAT1 level could serve as a potential diagnostic marker for AML with an AUC value of 0.819 (95% CI: 0.743–0.894, P < 0.001, Fig. 4A). At the cutoff value of 0.171 of LPCAT1 expression, the sensitivity and the specificity were 84.8% and 66.7%, respectively. ROC curves also disclosed the diagnostic value of LPCAT1 expression level in CN-AML (AUC = 0.795, 95% CI 0.703–0.887, P < 0.001, Fig. 4B).
Impact of LPCAT1 expression on prognosis
To investigate the prognostic impact of LPCAT1 expression on AML, survival was analyzed in 71 cases with follow-up data. There was no significant difference in the rates of complete remission (CR) between patients with and without LPCAT1 low expression (60% versus 48%, P = 0.298). However, there was a trend that the OS of AML patients with LPCAT1 low expression (median 14 months) was longer than those without LPCAT1 low expression (median 4 months) (P = 0.073, Fig. 5A). Furthermore, in CN-AML, patients with LPCAT1 low expression had a significantly longer OS than those without LPCAT1 low expression (median 19 versus 5.5 months, P = 0.036, respectively, Fig. 5B).
Discussion
In the present study, for the first time, we used BloodSpot and GEO databases to analyze LPCAT1 expression difference and RQ-PCR to validate the LPCAT1 expression in bone marrow specimens from newly diagnosed AML and healthy controls. BloodSpot, the GSE9476 database, and RQ-PCR results all showed that LPCAT1 expression in bone marrow samples was significantly lower in AML than in healthy controls. Few studies have reported the expression of LPCAT1 in hematologic malignancies, including AML. Wang et al. used quantitative PCR to examine the expression of LPCAT1 in peripheral blood samples from a small amount of AML patients and healthy controls. They found that LPCAT1 expression in peripheral blood specimens was increased in patients with newly diagnosed AML [36]. However, this expression analysis only using peripheral blood specimens does not perfectly represent the expression status of LPCAT1 in AML, a malignant disorder derived from immature myeloid progenitors in the bone marrow and diagnosed depends on a series of bone marrow abnormalities. Compare to peripheral blood samples, the bone marrow specimens are more representative for AML. The present study revealed that LPCAT1 expression significantly decreased in AML bone marrow. Notably, GSE9476 database results indicated that LPCAT1 expression in peripheral blood was also reduced in AML compared to normal controls, which contradicts the findings of Wang et al. [36]. However, because the patient numbers of both cohorts are limited, the status of LPCAT1 expression in peripheral blood requires further investigation.
LPCAT1 has recently been linked to cancer initiation and progression in various cancer types. LPCAT1 up-regulation has been observed in numerous solid cancers and associated with multiple tumor malignant characteristics such as progression, metastasis, recurrence, and poor prognosis by promoting epithelial-mesenchymal transition, tumor microenvironment, tumor immune infiltration, and chemoresistance [11,12,13,14,15,16,17,18,19,20,21,22,23,24]. Mechanistically, LPCAT1 inhibited tumor suppressor gene STAT1 expression and up-regulated Cyclins to promote hepatocellular carcinoma (HCC) progression [14]. Furthermore, LPCAT1 promoted disease progression via accelerating epithelial-mesenchymal transition by activating the Wnt/b-catenin signaling pathway in HCC [16]. LPCAT1 activated EGFR-mediated Akt signaling and MAPK signaling pathways in cutaneous squamous cell carcinoma, contributing to the cancer progression [22]. Additionally, LPCAT1 played an important role in brain metastasis of lung adenocarcinoma by up-regulating PI3K/AKT/MYC signaling and in gefitinib chemoresistance through promoting the activation of EGFR/PI3K/AKT signaling in lung adenocarcinoma cell line [23, 24]. These findings suggest that LPCAT1 may act as a tumor promoter and an oncogene in these solid tumors. However, the present study revealed that LPCAT1 expression was down-regulated in AML bone marrow, contrary to the high expression in solid tumors. Another study showed that LPCAT1 expression was down-regulated in bladder urothelial carcinoma cases and that LPCAT1 low expression may participate in carcinoma tumorigenesis and promote tumor aggression [37]. These findings imply that LPCAT1 may play different roles in different tumors types. The discrepancy in LPCAT1 expression could be attributed to tissue origin and tumor pathology. So far, the LPCAT1 function in AML has been unclear. As previously reported, the levels of various PCs in the plasma of AML patients were significantly lower than those in normal people [38]. The reason could be a decreased level of the LPCAT1, an enzyme that catalyzes PC production. Furthermore, the cholesterol level of blood leukocytes in AML was lower than that of normal leukocytes [39]. Because LPCAT1 could promote cholesterol synthesis [21], the lower cholesterol level might be related to the decreased level of LPCAT1.
Abnormal DNA methylation and gene expression profiles are critical in malignant transformation. Our research group showed that genome-wide DNA hypermethylation was frequent during MDS progression to AML [40]. As the most studied epigenetic alteration, DNA methylation has been well-established as a molecular mechanism leading to gene expression silencing [41, 42]. By bioinformatics analysis, we found that the LPCAT1 promoter was hypermethylated and that LPCAT1 methylation was strongly negatively associated with LPCAT1 expression in AML, implying that LPCAT1 expression may be inactivated by promoter hypermethylation. Of course, the LPCAT1 methylation status and the association between LPCAT1 expression and methylation need further verification.
We assessed the clinical significances of LPCAT1 low expression. There was no significant association between LPCAT1 low expression with patients’ sex, WBC, hemoglobin, platelets (Table 1). LPCAT1 low expression was found in each subtype of AML. The present study revealed that LPCAT1 low expression was less frequent in AML patients with the FAB-M4/M5 subtype than in other individuals. No significant difference was observed in the distribution of gene mutations between patients with and without LPCAT1 low expression. The prognostic value of LPCAT1 low expression was also evaluated. In CN-AML, patients with LPCAT1 low expression had significantly longer OS than those without LPCAT1 low expression, implying that LPCAT1 low expression may be a beneficial factor for AML patients.
Conclusions
In summary, our findings reveal that LPCAT1 expression is down-regulated in AML bone marrow. Low LPCAT1 expression could be used as a potential biomarker in AML for diagnosis and prognosis. The significance of LPCAT1 down-regulation in the pathogenesis and development of AML need to be further investigated.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Estey E, Döhner H (2006) Acute myeloid leukaemia. Lancet 368:1894–1907
Ferrara F (2004) Unanswered questions in acute myeloid leukaemia. Lancet Oncol 5:443–450
Avivi I, Rowe JM (2005) Prognostic factors in acute myeloid leukemia. Curr Opin Hematol 12:62–67
Grimwade D (2001) The clinical significance of cytogenetic abnormalities in acute myeloid leukaemia. Best Pract Res Clin Haematol 14:497–529
Byrd JC, Mrózek K, Dodge RK et al (2002) Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood 100:4325–4336
Mrózek K, Marcucci G, Paschka P et al (2007) Clinical relevance of mutations and gene-expression changes in adult acute myeloid leukemia with normal cytogenetics: are we ready for a prognostically prioritized molecular classification? Blood 109:431–448
Mrózek K, Döhner H, Bloomfield CD (2007) Influence of new molecular prognostic markers in patients with karyotypically normal acute myeloid leukemia: recent advances. Curr Opin Hematol 14:106–114
Santos CR, Schulze A (2012) Lipid metabolism in cancer. FEBS J 279:2610–2623
Kent C (2005) Regulatory enzymes of phosphatidylcholine biosynthesis: a personal perspective. Biochim Biophys Acta 1733:53–66
Shindou H, Shimizu T (2009) Acyl-CoA: lysophospholipid acyltransferases. J Biol Chem 284:1–5
Grupp K, Sanader S, Sirma H et al (2013) High lysophosphatidylcholine acyltransferase 1 expression independently predicts high risk for biochemical recurrence in prostate cancers. Mol Oncol 7:1001–1011
He RQ, Li JD, Du XF et al (2021) LPCAT1 overexpression promotes the progression of hepatocellular carcinoma. Cancer Cell Int 21(1):442
Sun Q, Liu X, Peng Q et al (2022) ncRNA-mediated high expression of LPCAT1 correlates with poor prognosis and tumor immune infiltration of liver hepatocellular carcinoma. J Immunol Res 2022:1584397
Ji W, Peng Z, Sun B et al (2021) LPCAT1 promotes malignant transformation of hepatocellular carcinoma cells by directly suppressing STAT1. Front Oncol 11:678714
Morita Y, Sakaguchi T, Ikegami K et al (2013) Lysophosphatidylcholine acyltransferase 1 altered phospholipid composition and regulated hepatoma progression. J Hepatol 59:292–299
Shen L, Gu P, Qiu C et al (2022) Lysophosphatidylcholine acyltransferase 1 promotes epithelial-mesenchymal transition of hepatocellular carcinoma via the Wnt/β-catenin signaling pathway. Ann Hepatol 27(3):100680
Lebok P, von Hassel A, Meiners J et al (2019) Up-regulation of lysophosphatidylcholine acyltransferase 1 (LPCAT1) is linked to poor prognosis in breast cancer. Aging (Albany NY) 11:7796–7804
Abdelzaher E, Mostafa MF (2015) Lysophosphatidylcholine acyltransferase 1 (LPCAT1) upregulation in breast carcinoma contributes to tumor progression and predicts early tumor recurrence. Tumour Biol 36:5473–5483
Zhao T, Zhang Y, Ma X et al (2021) Elevated expression of LPCAT1 predicts a poor prognosis and is correlated with the tumour microenvironment in endometrial cancer. Cancer Cell Int 21(1):269
Shida-Sakazume T, Endo-Sakamoto Y, Unozawa M et al (2015) Lysophosphatidylcholine acyltransferase1 overexpression promotes oral squamous cell carcinoma progression via enhanced biosynthesis of platelet-activating factor. PLoS ONE 10:e0120143
Tao M, Luo J, Gu T et al (2021) LPCAT1 reprogramming cholesterol metabolism promotes the progression of esophageal squamous cell carcinoma. Cell Death Dis 12(9):845
Huang Y, Wang Y, Wang Y et al (2022) LPCAT1 promotes cutaneous squamous cell carcinoma via EGFR-mediated protein kinase B/p38MAPK signaling pathways. J Invest Dermatol 142(2):303-313.e9
Wei C, Dong X, Lu H et al (2019) LPCAT1 promotes brain metastasis of lung adenocarcinoma by up-regulating PI3K/AKT/MYC pathway. J Exp Clin Cancer Res 38:95
Ding J, Ding X, Leng Z (2022) LPCAT1 promotes gefitinib resistance via upregulation of the EGFR/PI3K/AKT signaling pathway in lung adenocarcinoma. J Cancer 13(6):1837–1847
Yin C, Zhang J, Guan W et al (2021) High expression of CLEC11A predicts favorable prognosis in acute myeloid leukemia. Front Oncol 11:608932
Bagger FO, Sasivarevic D, Sohi SH et al (2016) BloodSpot: a database of gene expression profiles and transcriptional programs for healthy and malignant haematopoiesis. Nucleic Acids Res 44:D917–D924
Bennett JM, Catovsky D, Daniel MT et al (1985) Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-American-British Cooperative Group. Ann Intern Med 103:620–625
Vardiman JW, Harris NL, Brunning RD (2002) The World Health Organization (WHO) classification of the myeloid neoplasms. Blood 100:2292–2302
Lo Coco F, Foa R (1995) Diagnostic and prognostic advances in the immunophenotypic and genetic characterization of acute leukaemia. Eur J Haematol 55:1–9
Slovak ML, Kopecky KJ, Cassileth PA et al (2000) Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood 96:4075–4083
Lin J, Yao DM, Qian J et al (2012) IDH1 and IDH2 mutation analysis in Chinese patients with acute myeloid leukemia and myelodysplastic syndrome. Ann Hematol 91:519–525
Lin J, Yao DM, Qian J et al (2011) Recurrent DNMT3A R882 mutations in Chinese patients with acute myeloid leukemia and myelodysplastic syndrome. PLoS ONE 6:e26906
Yang X, Qian J, Sun A et al (2013) RAS mutation analysis in a large cohort of Chinese patients with acute myeloid leukemia. Clin Biochem 46:579–583
Qian J, Yao DM, Lin J et al (2012) U2AF1 mutations in Chinese patients with acute myeloid leukemia and myelodysplastic syndrome. PLoS ONE 7:e45760
Wen XM, Lin J, Yang J et al (2014) Double CEBPA mutations are prognostically favorable in non-M3 acute myeloid leukemia patients with wild-type NPM1 and FLT3-ITD. Int J Clin Exp Pathol 7:6832–6840
Wang K, Wu Z, Si Y et al (2021) Identification of LPCAT1 expression as a potential prognostic biomarker guiding treatment choice in acute myeloid leukemia. Oncol Lett 21:105
Abdelzaher Ahmed E, Abdel Bary Abdel-Latif A, Fahmy AM et al (2021) Differential lysophosphatidylcholine acyltransferase 1 (LPCAT1) expression confers aggressiveness and independently predicts recurrence in bladder urothelial carcinomas. J Histotechnol 44(4):196–205
Pabst T, Kortz L, Fiedler GM et al (2017) The plasma lipidome in acute myeloid leukemia at diagnosis in relation to clinical disease features. BBA Clin 7:105–114
Gottfried EL (1967) Lipids of human leukocytes: relation to celltype. J Lipid Res 8(4):321–327
Zhou JD, Zhang TJ, Xu ZJ et al (2020) Genome-wide methylation sequencing identifies progression-related epigenetic drivers in myelodysplastic syndromes. Cell Death Dis 11:997
Taby R, Issa JP (2010) Cancer epigenetics. CA Cancer J Clin 60:376–392
Yamashita K, Hosoda K, Nishizawa N et al (2018) Epigenetic biomarkers of promoter DNA methylation in the new era of cancer treatment. Cancer Sci 109:3695–3706
Funding
This study was supported by National Natural Science foundation of China (81970118), the Youth Medical Talents Project of “Ke Jiao Qiang Wei” project of Jiangsu province (QNRC2016449), and Zhenjiang Clinical Research Center of Hematology (SS2018009).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by Qin Chen, Zijun Xu, and Jiang Lin. The first draft of the manuscript was written by Qin Chen and Zhaoqun Deng. The manuscript revision was conducted by Jun Qian and Wei Qian. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was conducted in compliance with the 1964 Helsinki declaration and was approved by the Ethics Committee of the Affiliated People’s Hospital of Jiangsu University (No. K-20180063-Y).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Q., Xu, Z., Lin, J. et al. The validation and clinical significance of LPCAT1 down-regulation in acute myeloid leukemia. Mol Biol Rep 50, 4955–4963 (2023). https://doi.org/10.1007/s11033-023-08449-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-023-08449-7