Abstract
Background
Cerebral malaria is often pronounced as a major life-threatening neurological complication of Plasmodium falciparum infection. The complex pathogenic landscape of the parasite and the associated neurological complications are still not elucidated properly. The growing concerns of drugresistant parasite strains along with the failure of anti-malarial drugs to subdue post-recovery neuro-cognitive dysfunctions in cerebral malaria patients have called for a demand to explore novel biomarkers and therapeutic avenues. Due course of the brain infection journey of the parasite, events such as sequestration of infected RBCs, cytoadherence, inflammation, endothelial activation, and blood–brain barrier disruption are considered critical.
Methods
In this review, we briefly summarize the diverse pathogenesis of the brain-invading parasite associated with loss of the blood-brain barrier integrity. In addition, we also discuss proteomics, transcriptomics, and bioinformatics strategies to identify an array of new biomarkers and drug candidates.
Conclusion
A proper understanding of the parasite biology and mechanism of barrier disruption coupled with emerging state-of-art therapeutic approaches could be helpful to tackle cerebral malaria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral malaria (CM) is the most severe neurological syndrome of Plasmodium falciparum malaria affecting mostly children in sub-Saharan Africa and adults in Asia. The disease has emerged as a massive burden of morbidity and mortality to low- and middle-income countries. The complications of CM are frequently characterized by coma, cerebral seizures, neuroinflammation, and other neurological impairments [1]. Long-term cognitive deficits such as behavioral abnormalities, epilepsy, impaired hearing ability, sensory disorders, and motor weakness, collectively referred to as post malaria neurological sequelae, have also been observed in the case of CM survivors [2]. Owing to the widespread malaria transmission in sub-Saharan Africa, the acquisition of natural immunity during childhood is observed, leading to decreased infection in adults. Whereas, in parts of South-East Asia, due to restricted malaria transmission and inadequate natural immunity, CM generally occurs in grown-up children and adults [3]. Despite tremendous progress in malaria diagnosis, research, and prevention over the past decade, a thorough understanding of the parasite and the deadliest complication, CM, is lacking, demanding effective therapies. In the absence of adjuvant treatment, mortality remains high.
Clinically, CM can be described as a reversible syndrome with unarousable coma with the presence of asexual forms of P. falciparum on peripheral blood smears [1, 4]. CM, if remain untreated for an extended period of time can initiate organ dysfunction in patients. However, the pattern of this dysfunction can differ significantly in the adults and children. In adults, nervous system dysfunction occurs along with renal and respiratory organ system failure, whereas in children, though neurological issues are frequent with coma, seizures, and anemia but respiratory or renal complications are usually absent [5]. Neuropathologically, deposits of platelets, fibrin, and other inflammatory infiltrates have been observed within the neurovasculature of African children, which is generally absent or less prominent in adults [5]. Further, it is also unknown why only some individuals develop CM, after being infected with the malaria parasite; thus indicating the role of host immune factors and parasite interaction in the manifestation of the disease.
Three different hypotheses have been described to implicate the complex pathogenesis of CM. First, the sequestration hypothesis depicting the obstruction of microvasculature by the adhesion of Plasmodium-infected RBCs to endothelial cells [6]. Second, the inflammation hypothesis, which explains the excessive pro-inflammatory cytokine production owing to the dysregulated balance between the immune system modulators after the parasite infection [7]. Finally, the homeostasis hypothesis that explains the loss of endothelial barrier integrity leading to the loss of brain homeostasis [8]. Though interrelation between host immune system evasion, barrier disruption, and cellular inflammation in the context of CM is yet to be elucidated, a synergistic interplay between these mechanisms is supposed to be responsible for the complexity of the disease [9].
In order to understand the diverse patho-physiology of the parasite and develop effective therapeutics for CM by defying the odds of drug resistance, a renewed interest in host immune system–pathogen interaction is essential. In addition, using advanced proteomics and bioinformatics strategies, the discovery of a novel set of biomarkers and drug targets is necessary. The present review will focus on the pathogenesis of CM involving sequestration, inflammation induction, endothelial cell activation, cell toxicity, and tight junction-BBB disruption. Furthermore, the use of advanced strategies for biomarkers and drug target discovery will also be evaluated.
Pathogenesis of the malarial parasite
Sequestration of infected RBCs
The blood–brain barrier (BBB), often considered a hotspot in CM, is formed at the blood-cerebrospinal fluid barrier and the brain capillary endothelial cell junction [8]. Tight junctions are created by the transmembrane proteins along the brain endothelial cells obstructing free passage between peripheral blood and the brain extracellular fluid (ECF). Such a physical and metabolic barrier maintains brain homeostasis by protecting the central nervous system (CNS) from neurotoxins, and pathogens. Various cellular milieu of the CNS, i.e., neurons, endothelium, pericytes, vascular smooth muscles, and astroglial cells together constitute the neurovascular unit (NVU), which further adds to BBB integrity (Fig. 1). [10]. Neuroinflammation, often an underlying reason for brain infection and other neuroimmune diseases results from a compromised BBB leading to the passage of peripheral immune components into the CNS [8]. Major population-based studies on patients in Africa and Asia have reported a relation between seizures, hemorrhage, and axonal disruption with the compromised BBB in CM [11]. Though the exact mechanism of BBB disruption and neuroinflammation during CM is unclear, however independent studies have shown sequestration of parasite-infected RBCs to the brain epithelial cells and secretion of proinflammatory cytokines in animal models of CM [6].
Structural overview of the BBB. The BBB is formed by the monolayer of brain endothelial cells and the underlying basal lamina, creating tight junctions eliminating the passage between blood and brain, maintaining homeostasis. The BBB integrity is further reinforced by astrocytes and pericytes. The BBB, in association with neurons and microglia, forms the neurovascular unit (NVU). Specific receptors on the endothelial cells are helpful in the passage of essential metabolites into the brain for neuro maintenance.
Adhesion of P. falciparum-infected RBCs to the luminal side of endothelial cell lining blood vessels is often called sequestration and is responsible for immune evasion of the parasite [6]. A diverse array of host surface receptors as well as that of the parasite facilitates an easy sequestration process. This sequestration process triggers a cascade of cellular signaling events, eventually disrupting the integrity of tight junctions and BBB inducing localized hypoxia and hemorrhages inside brain parenchyma (Fig. 2) [12]. Sequestration and eventual microvascular congestion were found associated with coma in CM [13].
Series of events that lead to the P. falciparum-induced brain infection. Sequestration of parasite-infected RBCs onto the brain microvasculature results in the obstruction of blood flow, inviting pro-inflammatory molecules. Platelet adhesion onto the clubbed RBCs can block the blood and nutrient passage leading to hypoxia and activation of endothelial cells. Heightened intracerebral inflammation and cytokine release compromise the endothelial cell integrity leading to eventual BBB breakdown.
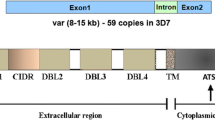
Host intercellular adhesion molecule-1 (ICAM-1) (also called cluster of differentiation 54—CD54) is expressed on endothelial cells and is responsible for interaction with the infected RBCs through the duffy binding-like (DBLβ-C2) domain of parasitic erythrocyte membrane protein 1 (PfEMP1) [14]. PfEMP1 gets localized into specific pockets on the plasma membrane of the infected RBCs. PfEMP1 has been reported to bind various other receptors like the vascular cell adhesion molecule-1 (VCAM-1), and the cytokine-activated endothelial protein C receptor (EPCR), effectively immobilizing the infected RBCs on the endothelium [6]. ICAM1 also synergizes with CD36 for enhanced adhesion, which can bind to the PfEMP-1 through its cysteine-rich interdomain region (CIDR) [15]. Considering the significant role of the DBLβ motif of PfEMP1, various studies have reported antibodies against the motif, which can inhibit ICAM-1-specific RBC adhesion in vitro [16]. Similarly, antibodies against EPCR have also been indicated to inhibit PfEMP1 binding to endothelial cells [17].
Various other adhesion-specific receptors, like the neural cell adhesion molecule (NCAM) receptor, selectins, von Willebrand Factor (vWF), and platelet endothelial cell adhesion molecule have been implicated in vitro to adhere infected RBCs [18, 19]. Though these receptors are speculated to have a specific role in CM, but extended research on these receptors is warranted. Platelets provide an indirect mechanism for cytoadhesion by becoming bridges between RBCs and endothelial cells at sites of low adhesion molecule expression [19]. Increased intravascular platelet deposition has also been demonstrated in Malawian and South-East Asian CM patients [20]. Another in vitro study, where the adoptive transfer of platelets in CD40-KO CM resistant mice developed signs of CM, indicated the pathological effects of platelets [21]. The sequestration process of infected RBCs and platelets is a central event in malarial brain infection which eventually leads to endothelial cell activation initiating cellular immune response modulated by cytokines and lymphotoxins [22]. From a therapeutic point of view, the prevention of sequestration of the infected RBCs could serve as an attractive way against CM [23]. Rapamycin has been reported to negatively affect the cytoadherence of infected RBCs by reducing the expression of ICAM-1 and VCAM-1 in a mice model termed as the experimental murine model of cerebral malaria (ECM) [24]. Similarly, anti-inflammatory substances such as the ethanolic extracts from the Trichoderma stromaticum fungus reduce the cerebral expression of ICAM-1 and VCAM-1, keeping the BBB integrity intact in ECM [25]. Heparin-like molecules of the glycosaminoglycan family have been reported to inhibit RBC invasion. Sevuparin, a member of the heparin family has been demonstrated recently to reduce cytoadherence and RBC invasion in an in vitro setting [26], as well as in phase-I and II human studies [27]. Further, atorvastatin has also been shown to reduce endothelial damage by preventing cytoadherence of the parasite in human primary culture [28]. However, one should be careful while translating these drugs from ECM to human trials, considering the potential limitations of the murine model in RBC sequestration [29].
Various studies have shown the anti-inflammatory properties of the anticoagulant serine protease, activated protein C (aPC) [30]. The protein binds to EPCR, exerting its anti-apoptotic effects protecting the barrier functions. However, EPCR binding of PfEMP1 diminishes the interaction between EPCR-aPC, leading to the generation of thrombin & fibrin, which in turn induces the NF-κB pathway instigating pro-inflammatory cytokine generation and BBB disruption [31]. Therefore, aPC might have the therapeutic key to prevent BBB disruption in CM.
Neuroinflammation and cytokine release
Activated inflammatory processes and a heightened pro-inflammatory cytokine release are often regarded as the hallmarks of CM [8]. Higher concentrations of localized productions of tumor necrosis factor-α (TNF-α), interferon-γ (IFN-γ), lymphotoxin-α (LT-α), interleukin (IL-1β), IL-10, and IL-6 has been reported in African children suffering from acute CM [32]. The released cytokines from immune cells such as macrophages or monocytes activate the endothelial cells, which release chemokines, such as, CCL2, CCL4, CXCL4, CXCL8, and CXCL10 [33]. Studies have reported that the IFN-γ receptor signaling pathway can induce the IFN-γ-inducible protein-10 (IP-10)/CXCL10, which recruits immune cells such as T-cells, natural killer (NK), and NKT cells expressing the corresponding chemokine receptor CXCR3 [34]. CXCL10 is often regarded as a faithful serum biomarker for CM. These chemokines might further initiate an inflammatory cascade injuring the endothelium, tight junction, and BBB, indicating that these chemokine receptor down-regulations or chemical inhibitors against these receptors might serve as potential therapeutic targets against CM [35]. It has also been reported that IRF1 negatively regulates CXCR3 expression suppressing the production of IFN-γ in ECM [36]. Further, antibiotic doxycycline has been demonstrated to reduce the expression of IFN-γ, matrix metalloproteinase 2 (MMP2), and other factors associated with the ECM. The authors also depicted an intact BBB with successful reduction of cerebral infiltration with the antibiotic [37]. Similarly, the use of synthetic oleanane triterpenoids (SO) has been demonstrated to reduce plasma levels of key inflammatory cytokines such as TNF-α, IFN-γ, and IL-10 thereby enhancing the BBB integrity [38]. Moreover, the downregulation of LTα in the parenchymal cells could also be a therapeutic consideration against neurological complications in ECM. LTα upregulates ICAM-1 expression and has a role in RBC sequestration. LTα knockout mice, on the other hand, are protected from ECM [39]. However, though TNF-α levels are usually associated with CM, TNF-α-deficient mice were not protected from ECM, and anti-TNF-α antibodies or pentoxifylline-mediated inhibition of TNF-α was also not found fruitful in human CM patients [40]. As blocking TNF-α was found insufficient for CM prevention, additional underlying mechanisms could be critical. Further, higher serum TNF-α levels could also result from some secondary immune responses and should not be considered as a direct outcome of CM pathogenesis. Hence while developing future therapeutic interventions targeting such immune components, one needs to keep the intricate nature of the host immune system in mind.
The intravascular accumulation of infected RBCs and platelets is considered to begin the cascade of severe neurological damage and is a key step in the development of ECM. The immune cellular components were observed to be mostly monocytes, T cells, and natural killer (NK) cells. It is well documented that T cells (CD8+ & CD4+) play an active role in the ECM pathology. Accumulation of immune cells is followed by BBB disruption and perforin and granzyme-B-mediated endothelial cell apoptosis and cell toxicity [41]. By using anti-CD4 and anti-CD8 antibody-based depletion strategies and knockout models, it is depicted that these animals do not develop ECM despite infection, and there is a substantial reduction of severity. Similar results were also obtained with perforin-or granzyme-B-deficient mice suggesting an effector role of CD8+ T-cells and a helper role of CD4+ T-cells in ECM pathogenesis [42]. It has further been demonstrated that for the development of ECM, along with T-cells, the presence of infected RBCs is also necessary. In other words, in ECM models, reduction of T-cells correlates with decreased RBC sequestration/infected RBC accumulation. From a therapeutic point of view, blocking adhesion molecules LFA-1 and VLA-4 in late stages of ECM decrease CD8+ T-cell adhesion in cerebral blood vessels [42].
Cells of myeloid origin, like monocytes, also play a vital role in CM. It has been reported using the advanced microscopic observation that monocytes accumulate in the infected brain several days before the beginning of clinical symptoms, and increased adhesion of monocytes is also observed with endothelial cell activation [43]. Flow cytometric analysis further reported the prevalence of CD11b+ cells in infected mice even before the heavy presence of T-cell, dendritic cells, or NK cells, indicating a role of monocytes during the early stages of parasite infection [43]. Moreover, monocyte/macrophage depletion has also been shown to reduce ECM in mice [44]. It is probable that in CM pathogenesis, locally activated monocytes recruit other leukocytes and CD8+ T cells and potentiates endothelial cell activation [43].
Other immune cells such as γδ T-cells and innate lymphoid cells have been suggested as contributors to the CM pathogenesis, as their depletion prevents ECM [45]. Though targeting varieties of immune cells might prevent ECM, direct targeting of CD8+ T-cells and monocytes has been deemed effective often along with other anti-malarial drugs [43]. The current research point towards a mechanism depicting higher levels of certain cytokines such as IFN-γ and TNF-α leads to binding of infected RBCs to brain endothelium, activating them and further recruiting T-cells. Presentation of malarial antigens (on cerebral blood vessels) to parasite-specific CD8+ T-cells might cause local endothelial cell demise, eventually causing BBB breakdown and neurological damage (Fig. 2).
Other associated effectors of CM pathology
Host-derived microparticles/microvesicles (MVs) are regarded as effectors and immunomodulators of CM pathology [46]. Microparticles are tiny vesicles of 1 μM diameter often derived from the outer membrane of cells when cells are subjected to stress or demise signals. They bud off from the outer membrane as it undergoes membrane rearrangement containing phosphatidylserine, surface antigens, and other proteins [46]. These vesicles could also function as a biological messenger between parasite cells or parasites and host cells. MVs were found to be overproduced in murine CM model [47]. Further investigation revealed the MVs to be of platelet origin [18]. The presence of MVs was also observed in Malawian patients with CM, suggesting a relationship between MVs and CM neuropathology [48]. The platelet-derived MVs were found to stimulate infected RBCs, enhancing their association with endothelial cells. Further studies in CM patients indicated infected RBCs as a major source of MVs. These MVs have been shown to alter the gene expression pattern-function in endothelial cells, ultimately compromising BBB permeability [49]. Elevated levels of cell-specific MVs have also been observed in the plasma of CM patients from Asia and Africa [46].
MVs have been found to be pro-inflammatory and can also induce inflammation by targeting the TLR4-MyD88 axis pathway, thereby upregulating the level of CD40 and TNF-α [50]. In a study involving parasite-infected mice, a treatment strategy with an anti-CD40L monoclonal antibody reduced MV levels and thrombocytopenia [47]. Since MVs have been associated with activating inflammatory macrophages and NK cells, blocking TLR4 in the ECM model limits the macrophage activation pattern [50]. Furthermore, since MVs have antigen presentation capabilities (MHC II, CD40, β2-microglobulin, and inducible costimulator ligand), they can prime accessory immune molecules and can amplify T-cell & monocyte proliferation, helping in the process of immunomodulation [51]. One study indicated that EVs released from infected RBCs contain genomic DNA of the parasite and could stimulate monocytes thereby activating the innate immune response in host [52]. Blocking MVs have been shown to reduce cellular activation and passive transfer of purified MVs have been demonstrated to exacerbate the condition in an in vitro setting [53]. Pharmacological blocking of MVs by a thiol pantethine has been shown to have a positive effect on endothelial cell integrity and can prevent cell demise in ECM [54]. In another setting, administration of N-acetylcysteine has been reported to inhibit microparticles being released from RBCs [55]. ATP-binding cassette transporter (ABCA1) deletion, which affects the MV release, has been shown to halt CM in an ABCA1-KO mouse model of malaria [56].
It has further been noted that certain plasma MVs carry a set of microRNAs (miRNAs) in relation to CM development, and the parasite-infected RBCs also release EVs containing regulatory RNAs [57]. These miRNAs have been shown to have an important role in host–parasite interactions and are regarded as promising biomarkers for CM severity [58]. Though P. falciparum does not express miRNA-specific proteins such as dicer or Argonaute (Ago), host Ago protein and miRNA could translocate to the parasite and can be associated with them [49]. The EVs containing such miRNA-related complex affect the host vascular cell function, endocytosis, host adherens junction permeability, and gene expression pattern of the parasite [49]. Though there is a limited number of studies regarding the role of miRNAs in cerebral malaria, one study demonstrated increased survival, reduced endothelial activation, and BBB integrity preservation in miR-155-KO ECM mice [59]. The authors also used an ex vivo endothelial microvessel model to depict anti-miR-155 pretreatment, which can reduce vascular leakage and endothelial dysfunction. Considering the role of several miRNAs: let-7a, miR-15b-5p, miR-16-5p, miR-19b, miR-150-5p, miR-155, miR-223-3p, and hsa-miR-451a in malaria, these should be evaluated in CM samples for a better understanding of the host–microbe interactions [58, 59]. With proper characterization and quantification of these released EVs, the therapeutic role of such vesicles can be established in CM prognosis.
Metabolic pathways significantly affect the pathogenesis of CM. Metabolic changes to the amino acid metabolism, such as hypoglycemia are observed in ECM models and human CM [60]. ECM mice have been reported to contain a higher concentration of alanine, lactate, and glutamate, which is absent in non-ECM mice [60]. Interestingly, these metabolic changes are often associated with the occurrence of hypoxia/ischemia, which is responsible for the obstruction of brain microvasculature as in ECM. Some early reports observed prevention of ECM through a dietary restriction in a prophylactic setting [61]. Recent studies now report treatment with rapamycin, a potent inhibitor of the mTOR pathway that can be used to prevent ECM [62]. The authors suggest a dietary restriction that affects the leptin signaling, reduces the parasite burden in the brain, increasing their clearance in the spleen. Similarly, using specific compounds, 6-diazo-5-oxo-l-norleucine (DON), glutamine metabolism can be manipulated thereby reducing the ECM burden [63]. Another in vitro study reported the use of 2-deoxy glucose (2DG) for ECM [64]. Pre-exposure to a high-fat diet has also been demonstrated to reduce ECM burden via an antioxidant-mediated mechanism [65].
Furthermore, BBB damage in CM can also be accelerated by the abnormal deposition of toxic metabolites. Several intermediates of the kynurenine pathway essential for tryptophan metabolism, such as kynurenic acid, picolinic acid, and quinolinic acid have been reported to have elevated levels in the cerebrospinal fluid (CSF) of CM patients [66]. Owing to the cytotoxic effect of quinolinic acid on neurons and astroglial cells [67], it can disrupt the integrity of the BBB. Picolinic acid, on the other hand, can stimulate the macrophages to produce pro-inflammatory chemokine [68], which eventually can lead to BBB damage.
Proteomics approach for novel biomarkers and drug targets
Despite several active anti-malarial drugs and viable chemotherapy, there is a growing instance of drug resistance in malaria treatment. This has paved a way for research into strategies to unlock novel drugs and vaccine targets. The discovery of new specific diagnostic markers by advanced proteomic techniques might lead to more appropriate disease management and might also be helpful in better understanding the host–pathogen interaction [69]. Proteomic profiling techniques are necessary for shedding light on the structure, function, and post-translation modifications (PTMs) of proteins from specific stages of a microorganism, allowing scientists to compare across life stage-specific cell signals, protein expression patterns, immune pathways, and pathogenicity [70]. Proteomic tools in parallel with genomic information can be used for biomarker detection for CM. A comparative analysis of host immune response before and after malarial infection/treatment could be a strategy to detect and develop novel vaccine targets [71].
A proteomic profiling study using the comparative trypsin-induced surface shaving approach in P. falciparum revealed infected RBC surface antigens, such as, PfEMP1, repetitive interspersed families of polypeptides (RIFINs), surface-associated interspersed gene family (SURFIN), and sub-telomeric variable open reading frame (STEVOR) as possible malaria vaccine targets [72]. Another study using the suspension-bead-array-based affinity proteomics approach depicted increased levels of platelet adhesion, endothelial activation, and muscular damage markers in plasma samples collected from Nigerian CM-affected children. This study further suggests probable muscle damage and microvasculature lesions in CM [73]. Gitau et al. performed a comparative proteomics identification approach of the CSF and plasma in Plasmodium falciparum-infected children diagnosed with CM and other non-malarial encephalopathies [74]. The authors detected a host protein, spectrin β chain brain 3 as a binding partner with several parasitic proteins involved in parasite invasion, and sequestration in the cellular microvasculature. Several other host protein levels were also found altered in this study [74].
After the infection of host RBCs by the parasite, drastic changes occur in the host proteome leading to the upregulation or downregulation of new proteins leading to the production of altered membranes and protein exchanges between the host and the parasite. Such comparisons can be extremely critical to better understand the parasite–host immune system interactions [75]. Parasite-infected erythrocyte surface proteins (PIESP) have been recognized as possible markers in the shotgun proteomics approach. PIESP1 and PIESP2 have been depicted to be associated with the protrusion/knob of the infected RBCs, making them suitable targets for CM [76]. A mass spectrometry-based analysis revealed P. falciparum antigen 332 (Pf332) and mature parasite-infected erythrocyte surface antigen (MESA) to have an over-expression profile on infected RBC membrane of CM patients [77]. Though their antigenic properties remain unclear requiring further investigation, the authors propose these two proteins as specific biomarkers involving protein networking, and export of variant surface antigens (VSAs). Since these two proteins are involved in the physiology of CM, extended drug-target research is warranted. A tandem mass tag (TMT)-based mass spectrometry from autopsy brain samples of CM patients revealed increased expression of proteins associated with innate immune response, platelet activation, and coagulation in CM. However, proteins associated with reactive oxygen species generation (ROS), and Na+ and Ca2+ transport are found to be reduced in CM [78]. The authors also identified three parasite proteins, that is, 14-3-3 protein, enolase, and l-lactate dehydrogenase as CM-specific biomarkers. The study also revealed the up-regulation of anti-inflammatory α1-antitrypsin and alpha-1-acid glycoprotein-1 (ORM1), which could be related to host immune defense against CM [78].
Mass spectrometric analysis of extracellular microvesicles (MVs) derived from a P. falciparum-infected Kenyan child identified about 153 enriched parasite proteins associated with cytoadhesion, virulence, and host cell remodeling [79]. This result significantly overlaps with another proteomic study which reported 84 parasite proteins modulating the host–parasite and parasite–parasite interactions [80]. These proteins can act as possible biomarkers for MVs released by the P. falciparum-infected RBCs. In a similar manner, as discussed, MVs might also contain miRNAs, which also act as diagnostic markers for CM. Differential transcriptome analysis of blood samples of children with cerebral malaria identified overexpression of miRNA recognition sites, such as miR-4, miR-15, miR-16, and miR-195 [81]. Further, a metabolomics approach to unveil intricate relations between the host & parasite revealed distinct metabolite profiles of lipid and amino acid metabolism pathways across the parasite life stages. The study also indicated an increase in the amount of four key metabolites, such as: γ-aminobutyric acid (GABA), pipecolic acid, nicotinamide adenine dinucleotide (NAD), α-ketoglutarate, in the infected-RBCs. These metabolites can also be used as diagnostic markers for malaria [82].
Another proteomic study in the ECM mice model reaffirmed brain endothelial damage and subsequent protein leak theory across the BBB [83]. The authors found an enhanced concentration of coagulation cascade proteins asserting the fact of possible platelet adhesion to brain microvasculature. Further, along with coagulation cascade proteins, competent factors and immune components were also upregulated, indicating a cross-talk between inflammation and coagulation in ECM. The authors further suggested BBB invasion as a final delayed effect, probably at later stages of CM [83].
In addition, another proteomic study in 52 hospitalized Gambian children suffering from CM depicted diverse protein associations [84]. The study asserted the role of upregulated cell adhesion proteins, such as, VCAM, ICAM-1 & ICAM-2, and depleted coagulation factor-associated proteins indicating endothelial activation, and tissue damage. Interestingly, several parasite proteins from the glycolytic pathway, purine salvage pathway, and cell membrane were also found overexpressed, indicating increased parasitic presence within brain vasculature [84]. The authors also reported decreased expression of two microparticle proteins, named profilin-1 and immunoglobulin J-chain. For nutrient fulfillment and host immune system evasion [85], most pathogens secrete varieties of molecules packed in MVs. Therefore, analysis of secretory MVs in CM patients could be a possible therapeutic goal of future studies. Table 1 summarizes different proteomics studies conducted on CM patients and the experimental murine model of CM (ECM). The use of advanced high-throughput affinity-proteomic tools of specific antibodies for potential screening candidates would allow a faster analysis of diagnostic biomarkers and novel drug/vaccine candidates.
Use of bioinformatics approach for biomarkers and drug targets
Genomics and bioinformatics techniques contribute immensely to our understanding of the infectious disease paradigm in terms of disease pathogenesis, host–pathogen interactions, immune system evasion for the identification of putative biomarkers and vaccine candidates. Figure 3 depicts the bioinformatics-based steps involved from patient sample collection to putative drug discovery. Gene expression profiling in blood samples of Senegalese CM patients using microarray analysis followed by hierarchical clustering and the support vector machine (SVM) method revealed many differentially expressed genes [86]. Associated proteins were then identified by mapping the key genes onto the human protein–protein interaction map. Later pathway analysis and functional gene annotation map indicated the involvement of immune pathways like TLR, cytokine, and Fc-gamma receptor (FCGR), and other cytotoxic pathways [86]. Such genetic analysis would help identify the bias involved in terms of infection pattern and host immune system involvement across CM patients of different geographical locations. Another study in Cameroonian school children using microarray-bioinformatics approach revealed about 3–14-fold up-regulation in specific genes involved in pathogenesis, cytoadherence (VSA proteins, such as PfEMP1, RIFIN), remodeling of the host cell membrane, and RBC aggregation in parasites obtained from CM patients compared to parasites obtained from asymptomatic patients [87]. Such studies will be helpful in understanding pathogen biology and parasite–host interactions.
Representation of steps involved from patient sample collection to putative drug discovery After blood or CSF sample collection from patients, advanced molecular techniques such as whole genome sequencing and transcriptomics can be performed, which can further be used for comparative bioinformatics strategies to study host responses against the parasite, pathogen genomic signatures, and transmission probabilities. Bioinformatics studies like GWAS can be employed to measure genetic diversity among species, determination of drug resistance-related mutations, and surveillance. In silico and cheminformatics studies can be performed for the discovery of new vaccine targets and putative drug candidates.
Another recent bioinformatics-only preliminary study reported the use of the weighted gene co-expression network analysis (WGCNA) for uncovering the malarial pathogenesis and developing novel therapeutics [88]. Analysis of blood transcriptomic dissimilarities between CM and severe malarial anemia in Ugandan children by Nallandhighal et al. pointed out the nuclear factor-erythroid-2-related factor-2 (Nrf2) and erythropoiesis-related genes to be downregulated in CM patients [89]. Nrf2 has been targeted to mitigate neuroinflammation & oxidative stress in neurodegenerative disorders. The study also indicated a significant enrichment in three neurodegenerative disease-specific pathways (KEGG pathway ID: hsa05010, hsa05012, and hsa05016) in CM children. Another comparative microarray hybridization-based blood transcriptomics study in Gabonese children depicted downregulation of Parkinson’s α-synuclein protein (SNCA), signal transducer STAT1, MHC-II genes, glutamate metabolism-involved gene hydroxyacylglutathione hydrolase (HAGH), fraktalkine receptor (CX3CR1), IFN signaling-based genes, and several ubiquitin-pathway genes [81]. The authors propose the downregulation of important genes in CM as a response to hypoxia and vessel obstruction after the sequestration of infected RBCs [81]. A similar microarray-based blood transcriptomics comparison study in resistant mice and ECM susceptible mice depicted the downregulation of clotting and platelet-related genes in ECM mice [90]. Further, genetic signatures of immune response factors, cell surface glycosylation factors, erythropoiesis, and transcription-related factors were found altered in ECM mice. Such genome-wide circulatory biomarker identification studies could help future studies in ECM mice [90].
Genome-wide association studies (GWAS) on samples collected from 11 countries by the malaria genomic epidemiology network (MalariaGEN) identified a new locus on chromosome 6 found to be associated with CM, which is situated over 700 kilo bases from the nearest coding gene [91]. The study, however, was unable to find the exact genomic function. The other GWAS studies on malaria population susceptibility are extensively reviewed here [92]. There exist several databases for comparative genomics and transcriptomics for the Plasmodium species helping the in silico analytical studies, and making the genome-wide visualization convenient for the end-users [93, 94]. Several in silico studies have been described in recent years using comparative genomics, molecular modeling, molecular dynamics, small molecule inhibitor screening, and docking against specific parasite proteins like M17 Leucine Amino Peptidase (LAP), M18 aspartyl aminopeptidase (M18AAP), and calcium-dependent protein kinases (PfCDPK5) [95, 96]. After comparison among metabolic pathways of the host and parasite, a study predicted the list of 21 essential proteins of the parasite out of which 11 proteins were selected as anti-malarial drug targets based on various prioritization parameters. The selected proteins were modeled into 3D structures and docked with small molecules from the ZINC database [97]. A comparative genomics analysis across six Plasmodium species followed by clustering and fast Fourier transformation (FFT) provided 55 candidate genes involved in CM [98]. After domain analysis of all individual genes, the authors finally selected the parasite-infected erythrocyte surface protein 2 (PIESP2) as the final virulence factor. Later investigations of the PIESP2 protein indicated its presence on the membrane of the infected RBCs and the protein might be responsible for sequestration, host inflammation response, and impairment of BBB integrity [99]. A comprehensive list of bioinformatics and transcriptomics studies discussed in this section is provided in Supplementary Table 1.
Considering the instances of malarial drug-resistance, a next-generation sequencing coupled with bioinformatics analysis study against specific genes and mitochondrial genome of the parasite found mutations in the chloroquine resistance transporter gene (crt), the pyrimethamine-resistant dihydropteroate synthase gene (dhps), the sulfadoxine-resistant dhps strain, dihydrofolate reductase, multidrug resistance (mdr1) genes [100]. Drug resistance demands the use of new effective replacements and new targets to which the parasite has not developed resistance yet. The use of preliminary chemoinformatics-based approach for new chemical moieties and functional groups could provide quick solutions for this biological scenario.
Concluding remarks
Cerebral malaria remains one of the deadly manifestations of P. falciparum-malaria, affecting the low and middle-income countries in Africa and Asia. The occurrence of drug resistance has threatened the CM treatment by traditional anti-malarial drugs. In such a biological scenario, novel therapeutic strategies harnessing the knowledge of host–parasite interactions, advanced proteomics, genomics, and bioinformatics strategies could be extremely helpful. Despite decades of extended clinical research, the exact pathogenesis of the disease remains unclear. Since the events of cytoadherence, inflammation, endothelial activation, and BBB disruption are interrelated during CM infection, drug candidates against specific proteins involved in these events could be critical for the parasite. Proper understanding of the events leading to BBB disruption might help in developing effective therapies for CM. Furthermore, new emerging technologies could also be employed to identify novel prognosis biomarkers and explore advanced therapeutic avenues. After gaining insights on the transcriptomic analytical studies, efforts should be made to replicate the treatment in CM-relevant animal models, which can later be translated into human clinical trials. Together with better diagnosis facilities, revamped clinical efforts could help decrease CM-related mortalities worldwide.
References
Idro R, Jenkins NE, Newton CRJ (2005) Pathogenesis, clinical features, and neurological outcome of cerebral malaria. Lancet Neurol 4:827–840. https://doi.org/10.1016/S1474-4422(05)70247-7
Idro R, Ndiritu M, Ogutu B et al (2007) Burden, features, and outcome of neurological involvement in acute falciparum malaria in Kenyan children. JAMA 297:2232–2240. https://doi.org/10.1001/jama.297.20.2232
Snow RW, Guerra CA, Noor AM et al (2005) The global distribution of clinical episodes of Plasmodium falciparum malaria. Nature 434:214–217. https://doi.org/10.1038/nature03342
World Health Organization (2000) Severe falciparum malaria. Trans R Soc Trop Med Hyg 94:1–90. https://doi.org/10.1016/S0035-9203(00)90300-6
Hawkes M, Elphinstone RE, Conroy AL, Kain KC (2013) Contrasting pediatric and adult cerebral malaria. Virulence 4:543–555. https://doi.org/10.4161/viru.25949
Storm J, Jespersen JS, Seydel KB et al (2019) Cerebral malaria is associated with differential cytoadherence to brain endothelial cells. EMBO Mol Med 11(2):e9164
Storm J, Craig AG (2014) Pathogenesis of cerebral malaria—inflammation and cytoadherence. Front Cell Infect Microbiol 4:100
Nishanth G, Schlüter D (2019) Blood–brain barrier in cerebral malaria: pathogenesis and therapeutic intervention. Trend Parasitol 35:516–528. https://doi.org/10.1016/j.pt.2019.04.010
van der Heyde HC, Nolan J, Combes V et al (2006) A unified hypothesis for the genesis of cerebral malaria: sequestration, inflammation and hemostasis leading to microcirculatory dysfunction. Trend Parasitol 22:503–508. https://doi.org/10.1016/j.pt.2006.09.002
Kadry H, Noorani B, Cucullo L (2020) A blood–brain barrier overview on structure, function, impairment, and biomarkers of integrity. Fluids Barrier CNS 17:69. https://doi.org/10.1186/s12987-020-00230-3
Adams Y, Olsen RW, Bengtsson A et al (2021) Plasmodium falciparum erythrocyte membrane protein 1 variants induce cell swelling and disrupt the blood–brain barrier in cerebral malaria. J Exp Med 218:e20201266. https://doi.org/10.1084/jem.20201266
Tunon-Ortiz A, Lamb TJ (2019) Blood brain barrier disruption in cerebral malaria: beyond endothelial cell activation. PLoS Pathog 15:e1007786. https://doi.org/10.1371/journal.ppat.1007786
Ponsford MJ, Medana IM, Prapansilp P et al (2012) Sequestration and microvascular congestion are associated with coma in human cerebral malaria. J Infect Dis 205:663–671. https://doi.org/10.1093/infdis/jir812
Brown A, Turner L, Christoffersen S et al (2013) Molecular architecture of a complex between an adhesion protein from the malaria parasite and intracellular adhesion molecule 1. J Biol Chem 288:5992–6003. https://doi.org/10.1074/jbc.M112.416347
Hsieh F-L, Turner L, Bolla JR et al (2016) The structural basis for CD36 binding by the malaria parasite. Nat Commun 7:12837. https://doi.org/10.1038/ncomms12837
Lennartz F, Adams Y, Bengtsson A et al (2017) Structure-guided identification of a family of dual receptor-binding PfEMP1 that is associated with cerebral malaria. Cell Host Microbe 21:403–414. https://doi.org/10.1016/j.chom.2017.02.009
Marion A, Maria B, Maxwell B et al (2016) Interaction between endothelial protein c receptor and intercellular adhesion molecule 1 to mediate binding of Plasmodium falciparum-infected erythrocytes to endothelial cells. MBio 7:e00615-e616. https://doi.org/10.1128/mBio.00615-16
Faille D, Combes V, Mitchell AJ et al (2009) Platelet microparticles: a new player in malaria parasite cytoadherence to human brain endothelium. FASEB J 23:3449–3458. https://doi.org/10.1096/fj.09-135822
Wassmer SC, Combes V, Grau GER (2011) Platelets and microparticles in cerebral malaria: the unusual suspects. Drug Discov Today Dis Mech 8:e15–e23. https://doi.org/10.1016/j.ddmec.2011.11.004
Hochman SE, Madaline TF, Wassmer SC et al (2015) Fatal pediatric cerebral malaria is associated with intravascular monocytes and platelets that are increased with HIV coinfection. MBio 6(5):e01390-e1415
Gramaglia I, Velez J, Combes V et al (2017) Platelets activate a pathogenic response to blood-stage Plasmodium infection but not a protective immune response. Blood 129:1669–1679. https://doi.org/10.1182/blood-2016-08-733519
Sierro F, Grau GER (2019) The ins and outs of cerebral malaria pathogenesis: immunopathology, extracellular vesicles, immunometabolism, and trained immunity. Front Immunol 10:830
Burns AL, Dans MG, Balbin JM et al (2019) Targeting malaria parasite invasion of red blood cells as an antimalarial strategy. FEMS Microbiol Rev 43:223–238. https://doi.org/10.1093/femsre/fuz005
Mejia P, Treviño-Villarreal JH, Reynolds JS et al (2017) A single rapamycin dose protects against late-stage experimental cerebral malaria via modulation of host immunity, endothelial activation and parasite sequestration. Malar J 16:455. https://doi.org/10.1186/s12936-017-2092-5
Cariaco Y, Lima WR, Sousa R et al (2018) Ethanolic extract of the fungus Trichoderma stromaticum decreases inflammation and ameliorates experimental cerebral malaria in C57BL/6 mice. Sci Rep 8:1547. https://doi.org/10.1038/s41598-018-19840-x
Saiwaew S, Sritabal J, Piaraksa N et al (2017) Effects of sevuparin on rosette formation and cytoadherence of Plasmodium falciparum infected erythrocytes. PLoS ONE 12:e0172718. https://doi.org/10.1371/journal.pone.0172718
Leitgeb AM, Charunwatthana P, Rueangveerayut R et al (2017) Inhibition of merozoite invasion and transient de-sequestration by sevuparin in humans with Plasmodium falciparum malaria. PLoS ONE 12:e0188754. https://doi.org/10.1371/journal.pone.0188754
Taoufiq Z, Pino P, N’dilimabaka N et al (2011) Atorvastatin prevents Plasmodium falciparum cytoadherence and endothelial damage. Malar J 10:52. https://doi.org/10.1186/1475-2875-10-52
Franke-Fayard B, Janse CJ, Cunha-Rodrigues M et al (2005) Murine malaria parasite sequestration: CD36 is the major receptor, but cerebral pathology is unlinked to sequestration. Proc Natl Acad Sci USA 102:11468–11473. https://doi.org/10.1073/pnas.0503386102
Bernabeu M, Smith JD (2017) EPCR and malaria severity: the center of a perfect storm. Trend Parasitol 33:295–308. https://doi.org/10.1016/j.pt.2016.11.004
Kessler A, Dankwa S, Bernabeu M et al (2017) Linking EPCR-binding PfEMP1 to brain swelling in pediatric cerebral malaria. Cell Host Microbe 22:601-614.e5. https://doi.org/10.1016/j.chom.2017.09.009
Mandala WL, Msefula CL, Gondwe EN et al (2017) Cytokine profiles in malawian children presenting with uncomplicated malaria, severe malarial anemia, and cerebral malaria. Clin Vaccine Immunol 24:e00533-e616. https://doi.org/10.1128/CVI.00533-16
Dunst J, Kamena F, Matuschewski K (2017) Cytokines and chemokines in cerebral malaria pathogenesis. Front Cell Infect Microbiol 7:324
Sorensen EW, Lian J, Ozga AJ et al (2018) CXCL10 stabilizes T cell–brain endothelial cell adhesion leading to the induction of cerebral malaria. JCI Insight. https://doi.org/10.1172/jci.insight.98911
Wilson NO, Solomon W, Anderson L et al (2013) Pharmacologic inhibition of CXCL10 in combination with anti-malarial therapy eliminates mortality associated with murine model of cerebral malaria. PLoS ONE 8:e60898. https://doi.org/10.1371/journal.pone.0060898
Gun SY, Claser C, Teo TH et al (2018) Interferon regulatory factor 1 is essential for pathogenic CD8+ T cell migration and retention in the brain during experimental cerebral malaria. Cell Microbiol 20:e12819. https://doi.org/10.1111/cmi.12819
Schmidt KE, Kuepper JM, Schumak B et al (2018) Doxycycline inhibits experimental cerebral malaria by reducing inflammatory immune reactions and tissue-degrading mediators. PLoS ONE 13:e0192717. https://doi.org/10.1371/journal.pone.0192717
Crowley VM, Ayi K, Lu Z et al (2017) Synthetic oleanane triterpenoids enhance blood brain barrier integrity and improve survival in experimental cerebral malaria. Malar J 16:463. https://doi.org/10.1186/s12936-017-2109-0
Engwerda CR, Mynott TL, Sawhney S et al (2002) Locally up-regulated lymphotoxin α, not systemic tumor necrosis factor α, is the principle mediator of murine cerebral malaria. J Exp Med 195:1371–1377. https://doi.org/10.1084/jem.20020128
Lell B, Köhler C, Wamola B et al (2010) Pentoxifylline as an adjunct therapy in children with cerebral malaria. Malar J 9:368. https://doi.org/10.1186/1475-2875-9-368
Schmid U, Stenzel W, Koschel J et al (2017) The deubiquitinating enzyme cylindromatosis dampens CD8+ T cell responses and is a critical factor for experimental cerebral malaria and blood–brain barrier damage. Front Immunol 1(8):27
Swanson PA II, Hart GT, Russo MV et al (2016) CD8+ T cells induce fatal brainstem pathology during cerebral malaria via luminal antigen-specific engagement of brain vasculature. PLoS Pathog 12:e1006022. https://doi.org/10.1371/journal.ppat.1006022
Niewold P, Cohen A, van Vreden C et al (2018) Experimental severe malaria is resolved by targeting newly-identified monocyte subsets using immune-modifying particles combined with artesunate. Commun Biol 1:227. https://doi.org/10.1038/s42003-018-0216-2
Schumak B, Klocke K, Kuepper JM et al (2015) Specific depletion of Ly6Chi inflammatory monocytes prevents immunopathology in experimental cerebral malaria. PLoS ONE 10:e0124080. https://doi.org/10.1371/journal.pone.0124080
Besnard A-G, Guabiraba R, Niedbala W et al (2015) IL-33-mediated protection against experimental cerebral malaria is linked to induction of type 2 innate lymphoid Cells, M2 macrophages and regulatory T cells. PLoS Pathog 11:e1004607. https://doi.org/10.1371/journal.ppat.1004607
Pankoui Mfonkeu JB, Gouado I, Fotso Kuaté H et al (2010) Elevated cell-specific microparticles are a biological marker for cerebral dysfunctions in human severe malaria. PLoS ONE 5:e13415. https://doi.org/10.1371/journal.pone.0013415
Piguet PF, Kan CD, Vesin C (2002) Thrombocytopenia in an animal model of malaria is associated with an increased caspase-mediated death of thrombocytes. Apoptosis 7:91–98. https://doi.org/10.1023/A:1014341611412
Combes V, Taylor TE, Juhan-Vague I et al (2004) Circulating endothelial microparticles in malawian children with severe falciparum malaria complicated with coma. JAMA 291:2542–2544. https://doi.org/10.1001/jama.291.21.2542-b
Dandewad V, Vindu A, Joseph J, Seshadri V (2019) Import of human miRNA-RISC complex into Plasmodium falciparum and regulation of the parasite gene expression. J Biosci 44:50. https://doi.org/10.1007/s12038-019-9870-x
Ye W, Chew M, Hou J et al (2018) Microvesicles from malaria-infected red blood cells activate natural killer cells via MDA5 pathway. PLoS Pathog 14:e1007298. https://doi.org/10.1371/journal.ppat.1007298
Wheway J, Latham SL, Combes V, Grau GER (2014) Endothelial microparticles interact with and support the proliferation of T cells. J Immunol 193:3378–3387. https://doi.org/10.4049/jimmunol.1303431
Sisquella X, Ofir-Birin Y, Pimentel MA et al (2017) Malaria parasite DNA-harbouring vesicles activate cytosolic immune sensors. Nat Commun 8:1985. https://doi.org/10.1038/s41467-017-02083-1
El-Assaad F, Wheway J, Hunt NH et al (2014) Production, fate and pathogenicity of plasma microparticles in murine cerebral malaria. PLoS Pathog 10:e1003839. https://doi.org/10.1371/journal.ppat.1003839
Penet M-F, Abou-Hamdan M, Coltel N et al (2008) Protection against cerebral malaria by the low-molecular-weight thiol pantethine. Proc Natl Acad Sci USA 105(44):1321–1326. https://doi.org/10.1073/pnas.0706867105
Nantakomol D, Dondorp AM, Krudsood S et al (2011) Circulating red cell-derived microparticles in human malaria. J Infect Dis 203:700–706. https://doi.org/10.1093/infdis/jiq104
Combes V, Coltel N, Alibert M et al (2005) ABCA1 gene deletion protects against cerebral malaria: potential pathogenic role of microparticles in neuropathology. Am J Pathol 166:295–302. https://doi.org/10.1016/S0002-9440(10)62253-5
Cohen A, Zinger A, Tiberti N et al (2018) Differential plasma microvesicle and brain profiles of microRNA in experimental cerebral malaria. Malar J 17:192. https://doi.org/10.1186/s12936-018-2330-5
Ketprasit N, Cheng IS, Deutsch F et al (2020) The characterization of extracellular vesicles-derived microRNAs in Thai malaria patients. Malar J 19:285. https://doi.org/10.1186/s12936-020-03360-z
Barker KR, Lu Z, Kim H et al (2017) miR-155 modifies inflammation, endothelial activation and blood–brain barrier dysfunction in cerebral malaria. Mol Med 23:24–33. https://doi.org/10.2119/molmed.2016.00139
Ghosh S, Sengupta A, Sharma S, Sonawat HM (2012) Metabolic fingerprints of serum, brain, and liver are distinct for mice with cerebral and noncerebral malaria: a 1H NMR spectroscopy-based metabonomic study. J Proteome Res 11:4992–5004. https://doi.org/10.1021/pr300562m
Hunt NH, Manduci N, Thumwood CM (1993) Amelioration of murine cerebral malaria by dietary restriction. Parasitology 107:471–476. https://doi.org/10.1017/S0031182000068049
Mejia P, Treviño-Villarreal JH, Hine C et al (2015) Dietary restriction protects against experimental cerebral malaria via leptin modulation and T-cell mTORC1 suppression. Nat Commun 6:6050. https://doi.org/10.1038/ncomms7050
Gordon EB, Hart GT, Tran TM et al (2015) Targeting glutamine metabolism rescues mice from late-stage cerebral malaria. Proc Natl Acad Sci USA 112:13075–13080. https://doi.org/10.1073/pnas.1516544112
Wang A, Huen SC, Luan HH et al (2018) Glucose metabolism mediates disease tolerance in cerebral malaria. Proc Natl Acad Sci USA 115:11042–11047. https://doi.org/10.1073/pnas.1806376115
Zuzarte-Luís V, Mello-Vieira J, Marreiros IM et al (2017) Dietary alterations modulate susceptibility to Plasmodium infection. Nat Microbiol 2:1600–1607. https://doi.org/10.1038/s41564-017-0025-2
Holmberg D, Franzén-Röhl E, Idro R et al (2017) Cerebrospinal fluid kynurenine and kynurenic acid concentrations are associated with coma duration and long-term neurocognitive impairment in Ugandan children with cerebral malaria. Malar J 16:303. https://doi.org/10.1186/s12936-017-1954-1
Guillemin GJ (2012) Quinolinic acid, the inescapable neurotoxin. FEBS J 279:1356–1365. https://doi.org/10.1111/j.1742-4658.2012.08485.x
Bosco MC, Rapisarda A, Massazza S et al (2000) The tryptophan catabolite picolinic acid selectively induces the chemokines macrophage inflammatory protein-1α and -1β in macrophages. J Immunol 164:3283–3291. https://doi.org/10.4049/jimmunol.164.6.3283
Mathema VB, Na-Bangchang K (2015) A brief review on biomarkers and proteomic approach for malaria research. Asian Pac J Trop Med 8:253–262. https://doi.org/10.1016/S1995-7645(14)60327-8
Swearingen KE, Lindner SE (2018) Plasmodium parasites viewed through proteomics. Trend Parasitol 34:945–960. https://doi.org/10.1016/j.pt.2018.08.003
Galassie AC, Link AJ (2015) Proteomic contributions to our understanding of vaccine and immune responses. Proteomics Clin Appl 9(11–12):972–989. https://doi.org/10.1002/prca.201500054
Nilsson Bark SK, Ahmad R, Dantzler K et al (2018) Quantitative proteomic profiling reveals novel Plasmodium falciparum surface antigens and possible vaccine candidates. Mol Cell Proteomics 17:43–60. https://doi.org/10.1074/mcp.RA117.000076
Bachmann J, Burté F, Pramana S et al (2014) Affinity proteomics reveals elevated muscle proteins in plasma of children with cerebral malaria. PLoS Pathog 10:e1004038. https://doi.org/10.1371/journal.ppat.1004038
Gitau EN, Kokwaro GO, Karanja H et al (2013) Plasma and cerebrospinal proteomes from children with cerebral malaria differ from those of children with other encephalopathies. J Infect Dis 208:1494–1503. https://doi.org/10.1093/infdis/jit334
Zhang Y, Huang C, Kim S et al (2015) Multiple stiffening effects of nanoscale knobs on human red blood cells infected with Plasmodium falciparum malaria parasite. Proc Natl Acad Sci USA 112:6068–6073. https://doi.org/10.1073/pnas.1505584112
Florens L, Liu X, Wang Y et al (2004) Proteomics approach reveals novel proteins on the surface of malaria-infected erythrocytes. Mol Biochem Parasitol 135:1–11. https://doi.org/10.1016/j.molbiopara.2003.12.007
Bertin GI, Sabbagh A, Argy N et al (2016) Proteomic analysis of Plasmodium falciparum parasites from patients with cerebral and uncomplicated malaria. Sci Rep 6:26773. https://doi.org/10.1038/srep26773
Kumar M, Varun CN, Dey G et al (2018) Identification of host-response in cerebral malaria patients using quantitative proteomic analysis. Proteomics Clin Appl 12(4):1600187
Abdi AI, Yu L, Goulding D et al (2017) Proteomic analysis of extracellular vesicles from a Plasmodium falciparum Kenyan clinical isolate defines a core parasite secretome. Wellcome Open Res 2:50
Mantel P-Y, Hoang AN, Goldowitz I et al (2013) Malaria-infected erythrocyte-derived microvesicles mediate cellular communication within the parasite population and with the host immune system. Cell Host Microbe 13:521–534. https://doi.org/10.1016/j.chom.2013.04.009
Boldt ABW, van Tong H, Grobusch MP et al (2019) The blood transcriptome of childhood malaria. EBioMedicine 40:614–625. https://doi.org/10.1016/j.ebiom.2018.12.055
Beri D, Ramdani G, Balan B et al (2019) Insights into physiological roles of unique metabolites released from Plasmodium-infected RBCs and their potential as clinical biomarkers for malaria. Sci Rep 9:2875. https://doi.org/10.1038/s41598-018-37816-9
Moussa E, Huang H, Ahras M et al (2018) Proteomic profiling of the brain of mice with experimental cerebral malaria. J Proteomics 180:61–69. https://doi.org/10.1016/j.jprot.2017.06.002
Moussa EM, Huang H, Thézénas ML et al (2018) Proteomic profiling of the plasma of Gambian children with cerebral malaria. Malar J 17:337. https://doi.org/10.1186/s12936-018-2487-y
Sampaio NG, Cheng L, Eriksson EM (2017) The role of extracellular vesicles in malaria biology and pathogenesis. Malar J 16:245. https://doi.org/10.1186/s12936-017-1891-z
Thiam A, Sanka M, Ndiaye Diallo R et al (2019) Gene expression profiling in blood from cerebral malaria patients and mild malaria patients living in senegal. BMC Med Genomic 12:148. https://doi.org/10.1186/s12920-019-0599-z
Almelli T, Nuel G, Bischoff E et al (2014) Differences in gene transcriptomic pattern of Plasmodium falciparum in children with cerebral malaria and asymptomatic carriers. PLoS ONE 9:e114401. https://doi.org/10.1371/journal.pone.0114401
Nambou K, Nie X, Tong Y, Anakpa M (2021) Weighted gene co-expression network analysis and drug–gene interaction bioinformatics uncover key genes associated with various presentations of malaria infection in african children and major drug candidates. Infect Genet Evol 89:104723. https://doi.org/10.1016/j.meegid.2021.104723
Nallandhighal S, Park GS, Ho Y-Y et al (2019) Whole-blood transcriptional signatures composed of erythropoietic and NRF2-regulated genes differ between cerebral malaria and severe malarial anemia. J Infect Dis 219:154–164. https://doi.org/10.1093/infdis/jiy468
Oakley MS, Anantharaman V, Venancio TM et al (2011) Molecular correlates of experimental cerebral malaria detectable in whole blood. Infect Immun 79:1244–1253. https://doi.org/10.1128/IAI.00964-10
Malaria Genomic Epidemiology Network (2019) Insights into malaria susceptibility using genome-wide data on 17,000 individuals from Africa. Asia Ocean Nat Commun 10:5732. https://doi.org/10.1038/s41467-019-13480-z
Damena D, Denis A, Golassa L, Chimusa ER (2019) Genome-wide association studies of severe P. falciparum malaria susceptibility progress, pitfalls and prospects. BMC Med Genomics 12(1):120
Tan QW, Mutwil M (2020) Malaria.tools—comparative genomic and transcriptomic database for Plasmodium species. Nucleic Acid Res 48:D768–D775. https://doi.org/10.1093/nar/gkz662
Aurrecoechea C, Brestelli J, Brunk BP et al (2009) PlasmoDB: a functional genomic database for malaria parasites. Nucleic Acid Res 37:D539–D543. https://doi.org/10.1093/nar/gkn814
Rout S, Mahapatra RK (2019) In silico analysis of Plasmodium falciparum CDPK5 protein through molecular modeling, docking and dynamics. J Theor Biol 461:254–267. https://doi.org/10.1016/j.jtbi.2018.10.045
Rout S, Mahapatra RK (2019) In silico study of M18 aspartyl amino peptidase (M18AAP) of Plasmodium vivax as an antimalarial drug target. Bioorg Med Chem 27:2553–2571. https://doi.org/10.1016/j.bmc.2019.03.039
Rout S, Warhurst DC, Suar M, Mahapatra RK (2015) In silico comparative genomics analysis of Plasmodium falciparum for the identification of putative essential genes and therapeutic candidates. J Microbiol Method 109:1–8. https://doi.org/10.1016/j.mimet.2014.11.016
Liu X, Wang Y, Liang J et al (2018) In-depth comparative analysis of malaria parasite genomes reveals protein-coding genes linked to human disease in Plasmodium falciparum genome. BMC Genomics 19:312. https://doi.org/10.1186/s12864-018-4654-5
Liu X, Wu Y, Zhao Y et al (2021) Identification of Plasmodium falciparum-specific protein PIESP2 as a novel virulence factor related to cerebral malaria. Int J Biol Macromol 177:535–547. https://doi.org/10.1016/j.ijbiomac.2021.02.145
Talundzic E, Ravishankar S, Kelley J et al (2018) Next-generation sequencing and bioinformatics protocol for malaria drug resistance marker surveillance. Antimicrob Agent Chemother 62:e02474-e2517. https://doi.org/10.1128/AAC.02474-17
Funding
The work has not been sponsored by any external funding agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that no conflict of interest exists.
Ethical approval
The review article is complied with ethical standard.
Research involving human and/or animal participants
The current report contains no human or animal studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Panda, C., Mahapatra, R.K. An update on cerebral malaria for therapeutic intervention. Mol Biol Rep 49, 10579–10591 (2022). https://doi.org/10.1007/s11033-022-07625-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07625-5