Abstract
Background
This study explored the applicability of serum level and tissue expression of Ribonucleotide-diphosphate Reductase subunit M2 B (RRM2B) as reliable biomarkers for colorectal cancer (CRC) progression and metastasis.
Methods and results
The present descriptive-analytic cohort study was conducted on 50 newly diagnosed CRC patients (stage II, III) and 50 healthy individuals. The new cases had not received any therapeutic intervention and underwent surgery immediately after the initial diagnosis. Tumorous tissues and marginal healthy tissues (as control) were excised to determine the mRNA tissue expression of RRM2B by Real-Time PCR. Serum RRM2B protein was measured using an ELISA method once in the control group. In the patients, serum RRM2B protein was evaluated before, 1 and 3 months after surgery. The tumor metastasis node (TMN) classification system and liver metastasis were evaluated in CRC patients. The results showed significantly lower RRM2B serum levels in 1 and 3 months after surgery compared with the pre-surgery condition (P = 0.014, P < 0.001 respectively). The mean RRM2B gene expression was 51% lower in tumor tissue than its adjacent normal tissue (P < 0.001). No significant relationship was found between serum level of RRM2B and tumor staging and metastasis in patients before surgery (P = 0.373, P = 0.189), 1 month after surgery (P = 0.960, P = 0.088), and 3 months after surgery (P = 0.407, P = 0.724). RRM2B expression in tumor tissue is not associated with tumor staging and metastasis (P = 0.254, P = 0.721).
Conclusion
These data suggest measuring serum protein level of RRM2B could have a role in CRC progression, although this study should be considered preliminary due to small sample size and short follow-up duration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most deadly cancer globally. It is a multifactorial disease resulting from genetic, environmental, and lifestyle risk factors [1, 2]. The burden of CRC on public health is estimated to be increased by 60% during the next decade. CRC-related deaths are expected to reach 1.1 million by 2030 [3]. Noteworthy, CRC is the fourth most common cancer in Iran, with an average incidence rate of 11.6–10.5 for men and women, respectively [4]. Furthermore, CRC is more prevalent in Iran than in western countries among the population older than 45 [5]. As developing countries experience a rising incidence of CRC cases [1], developing a reliable prognostic biomarker is of crucial significance. The CRCs are highly heterogeneous, driven by different arrays of mutations and mutagens that progress through various morphological stages, including polyp formation and malignant conversion. This situation is caused by mutations targeting oncogenes, tumor suppressor genes, and genes related to DNA repair mechanisms [1, 6]. Cancer cells require deoxynucleotide triphosphates (dNTP) synthesis for their growth, and dNTP pool imbalances enhance mutagenesis mainly by DNA insertion mutation and impaired proofreading [7,8,9]. The ribonucleotide reductase (RR) enzyme is a key player in dNTP synthesis [9]. RR is a highly regulated rate-limiting enzyme with a vital role in DNA synthesis by converting ribonucleoside diphosphate to 2’-deoxyribonucleoside diphosphate. Human RR consists of one large subunit (RRM1) and two small subunits (RRM2 and RRM2B) [9, 10]. RRM2B can counteract reactive oxygen species (ROS) and is involved in DNA replication and repair, cell cycle, and mitochondrial homeostasis [11, 12]. A small subunit of RRM2B also known as p53R2 contains a tyrosine-free radical and a non-heme iron for enzymatic activity [13]. An increase in RR activity and dNTP pools is necessary to ensure accurate DNA synthesis in response to DNA damage or replicative stress [14]. Notably, previous findings determined the amount of RRM2B gene expression in cancer tissue, while its serum has not been considered yet. This motivated the authors to examine the possibility of applying RRM2B as a biomarker in the metastatic stage of CRC. To this end, serum levels of RRM2B were screened in CRC patients before, 1 and 3 months after surgery. The RRM2B expression was also assessed at the mRNA level in surgically excised tumor tissues. The results could provide valuable evidence in support of RRM2B potential as a diagnostic CRC biomarker.
Materials and methods
Participants
This descriptive-analytic cohort study was conducted on 100 individuals who were referred to the hospital affiliated with Tehran University of Medical Sciences, Imam Khomeini hospital of Tehran, Iran, between 2018 and 2020. The participants were divided into two groups: fifty new cases of colorectal cancer, who had not received any therapeutic interventions as a case group, and fifty healthy subjects who came for routine check-ups as the control group. Our control group was matched with the case group in terms of demographic characteristics such as age and sex. The new cases underwent colorectal surgery immediately after diagnosis and, tissue sections were excised for further assessment. The clinical stage was determined according to the International Joint Cancer TNM (tumor, node, and metastasis) Classification System. Pregnant, smoker, and alcoholic participants or those suffering from underlying diseases such as diabetes, myocardial infarction, metabolic disorders, thyroid problems, kidney diseases, congenital liver diseases, and malignancies other than colorectal cancer were excluded from the study. Before the study, all participants signed a written informed consent form approved by National Institute for Medical Research Development (NIMAD).
Blood samples and measurement of serum RRM2B
Peripheral venous blood (5 mL) was sampled from the patients before surgery, 1 month, and 3 months after surgery. The same amount of peripheral venous blood was also collected from healthy controls on the day of routine check-ups. The blood samples were immediately transferred to the biochemistry laboratory, and the serum was separated and preserved at − 80 °C until the day of assessment. Serum RRM2B levels were evaluated using Human RRM2B ELISA Kit (Ribonucleotide Reductase M2B (TP53 inducible))-ABIN1155810, as instructed by the manufacturer.
Quantitative real-time PCR (qRT-PCR)
Tumor and its marginal healthy tissues were sampled from the patients on the day of surgery. After pathological confirmation of CRC and marginal healthy tissues (as controls), the sections were kept in tubes containing RNA LATER (Sigma-Aldrich) for better conservation of the tissue mRNA. Subsequently, total RNA was extracted using tissue homogenizer and TRIzol™ plus RNA purification, and RNA concentration was measured by the nanodrop method. For the reverse transcription reaction, approximately 2 μg of total RNA was used for cDNA (complementary DNA) synthesis (Fermentas, USA) by Random hexamer and oligo-dT as primers according to the manufacturer's instructions. The qRT-PCR was performed by ABI system SYBR Green Master Mix (Takara, RR820A) at 95 °C for 2 min, followed by 40 cycles of 95 °C for 5 s and extension at 60 °C for 45 s. The results were analyzed by Rest 2009 Software QIAGEN. Data were normalized based on the glyceraldehyde-3-phosphate dehydrogenase (GAPDH) expression in each sample.
Statistical analysis
The quantitative and qualitative data are reported as mean ± standard deviation (SD) and percent. Independent t-tests were used to examine the differences between the two groups in terms of main outcomes, demographic data, and other measurements. One sample t-test was used to compare RRM2B expression between tumor and normal tissue. Repeated measure ANOVA with normal distribution was employed to compare RRM2B expression/protein level of the groups. If the result of repeated measure ANOVA was significant, the LSD post hoc test was performed for pairwise comparison between different times. P-values below 0.05 were considered to be statically significant. All statistical analysis was performed using the SPSS software, version 21.
Results
The baseline characteristics of participants are summarized in Table 1. An independent t-test was utilized to evaluate the differences between the two study groups in terms of demographic, clinical, and pathological variables. As shown in Table 1, CRC patients had significantly lower mean corpuscular volume (MCV) (P = 0.015). On the other hand, blood sugar (BS) and platelet (PLT) count were significantly higher in CRC patients (125.92 ± 48.13 vs. 93.7 ± 7.16 and 291.62 ± 129.71 vs. 239.34 ± 55.53, respectively). Other baseline characteristics showed no statistically significant difference. Table 1 also indicates the number and percentage of cases with different stages. Most of the patients were in stage II with no liver metastasis.
According to Table 2, The means of RRM2B gene expression were 0.49 ± 0.70 and 1.01 ± 1.35 in tumor tissue and normal tissue respectively. RRM2B gene expression levels were 51% lower in tumor tissue when compared with normal tissue (P < 0.001, t = 4.94, and degree of freedom = 49). However, no significant differences were detected between RRM2B gene expression levels in terms of gender, tumor stage, and liver metastasis (P = 0.258, P = 0.721, and P = 0.254).
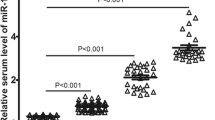
Table 3 provides the mean and standard deviation (SD) of serum RRM2B protein levels in 50 CRC patients. The CRC patients were classified into three different groups regarding the measurement time (before surgery, 1 month, and 3 months after surgery). Furthermore, the sera of the healthy subjects (N = 50) were evaluated. F-test derived from repeated measure ANOVA test was employed to calculate the significance between four mentioned groups. Based on Table 3, the serum expression of RRM2B was significantly different in four groups (P2 = 0.003, F = 5.334, and degree of freedom = 3/147). Figure 1 provides a pair-wise comparison of the serum RRM2B protein levels using the LSD post hoc test. What stands out in this figure was the statistically lower level of RRM2B protein 3 months after surgery compared to the healthy subjects (P < 0.001). Moreover, surgery managed to substantially decrease the level of RRM2B protein 1 month (P = 0.014) and 3 months (P < 0.001) after surgery the same as the healthy group (P = 0.043). No significant difference was detected in serum RRM2B level during 2 months (from months 1–3) after surgery (0.366 ± 0.005 vs 0.365 ± 0.001, = 0.619). T-tests were applied to analyze the inter-gender relationship. No difference was observed in males and females in terms of the serum level of the RRM2B protein (Table 3).
As a subsidiary goal, the RRM2 expression was also explored in tumor cells and compared with the RRM2B expression level. Higher expression of RRM2 (0.6.56 ± 6.03) was found compared to RRM2B (0.49 ± 0.70) (P < 0.001).
Tumor stage and metastasis were not correlated with serum RRM2B protein level before surgery and by a short while follow-up after surgery (P > 0.05) (Table 4).
Discussion
Genomic instability, defined as an elevated rate of acquisition of genetic mutations, has been postulated as a key player in tumor development, progression, and resistance to treatment [15]. The various biological markers which are known to be related to the prognosis of CRC are studided [16]. Their biological roles are centered on regulating prooxidant state and potential invasion in cancer cells which could be beneficial in therapeutic goals and survival prediction.
Malignancy suppresses the potential of RRM2B due to its p53-inducible nature. However, the precise role of RRM2B in human cancer progression and metastasis has not been fully understood as it is found to be tumor type-specific as well as stage-specific. According to prior analytic findings, RRM2B could suppress the invasion of pancreatic, oropharyngeal, prostate, and colon cancer cells [17]. Genetic variation of RRM2B has been previously reported in non-small cell lung cancer (NSCLC), Hepatocellular carcinoma (HCC), gastric, and urothelial carcinoma [18,19,20,21]. Tian et al. reported down-regulation of RRM2B in HCC commonly. Cell migration, invasion, and metastasis in HCC have been suggested to be inhibited by RRM2B in vitro and in vivo [20]. On the contrary, widespread overexpression of RRM2B in transgenic mice induces NSCLC [21]. However, no correlation was found between RRM2B expression and grade, stage, and histological type of gastric cancer [18]. Nevertheless, RRM2B is highly expressed in some human cancers as noted above. Experimental suppression of RRM2B expression impairs cancer cell proliferation in vitro [22]. A possible explanation for the controversial role of the RRM2B gene in different cancers might be dependent on the time of gene expression. Prior to the formation of cancer cells, p53R2 provides dNTPs for DNA repair and increases expression of P21 while declining the expression of cyclin D in wild-type cells to arrest the cell cycle for repairing the damaged DNA. After the formation of malignancy and their increasing demands for nutrients and support, p53R2 may contribute to cancer cell progression, especially when p21 presents in the cytoplasm [23]. In particularly, RRM2B amplifications among several tumors accompanying other oncogenes such as MYC are aspiring biological models in context of survival outcome [24].
The current study set out to evaluate the expression level of the RRM2B gene and protein as biological marker in CRC patients compared to normal controls. This investigation has shown that RRM2B gene expression was significantly lower in CRC tumor tissue (51% lower, p < 0.001), strengthening the idea that down-regulation of the RRM2B gene may contribute to poor prognosis. In line with the present findings, previous studies have shown markedly better survival in CRC patients with elevated RRM2B expression [16]. Another study reported significantly lower expression levels of RRM2b in patients with distant metastasis and late-stage CRC compared with those having no metastasis and early-stage CRC. However, the present study found no association between and RRM2b expression and Overall Survival in CRC patients [25]. On the other hand, in some other types of cancers (e.g., Esophageal, oral, and small cell lung cancer), it is found that RRM2B overexpression is positively correlated with increased metastasis and poor prognosis [25].
Contrary to prior studies which were mainly focused on measuring nuclear and cytosolic RRM2B levels, this project determined the serum level of RRM2B protein for the first time. Therefore, it can be speculated that only a single serum specimen from suspected individuals could explain the colon tumorigenesis. Besides, the obtained results indicated significantly different RRM2B serum levels before and after surgery, suggesting the clinical relevance of serum RRM2B levels in CRC patients. Serum RRM2B protein showed a decline after surgery. This discrepancy could be attributed to the elimination of the source of RRM2B protein expression by surgery. Regarding the short-time follow-up in the present study, it is not clear whether the altered level of serum RRM2B could impress the patient prognosis and survival. Further research should be focused on determining the possible role of this biomarker in overall survival. Despite a significant decrease of RRM2B gene expression in CRC patients, the results indicated no difference between CRC patients before surgery and the healthy group regarding serum RRM2B protein levels.
This study does not demonstrate any difference in RRM2B gene expression between patients with stage II and III. Furthermore, advanced stages of CRC and occurrence of metastasis did not alter RRM2B protein expression. The effect of RRM2B gene expression on tumor metastasis was also assessed which showed no association (Table 2, P = 0.254). These outcomes differ from earlier findings revealing a negative relationship between RRM2B expression and cancer cell invasiveness, lymph node involvement, and metastasis [16, 17].
Prior investigations have mentioned gender as an essential factor influencing survival results among CRC patients. Females have been reported to have significantly better overall survival (OS) and cancer‐specific survival (CSS) than males [26]. This result seems consistent with our findings, revealing higher expression of RRM2B protein in females after surgery. Hence, elevated levels of this biomarker may contribute to the better survival of females. However, both genders did not show any significant difference in the expression of the RRM2B gene in their tumor tissue (Table 1, P = 0.258).
RRM2 plays a critical role in tumor invasiveness and malignancy [27]. As a Subsidiary finding, significantly higher levels of RRM2 were determined in tumor cells as compared with RRM2B (P < 0.001). Although RRM2 and RRM2B are highly homologous in their gene sequences, their expressional levels and subcellular localizations are differently regulated in cells. Similar to our results, immunohistochemistry studies of Ding Y et al. showed that RRM2 gene expression levels were higher than that of the other two subunits in almost all the studied cancer types, especially CRC. Dysregulated expression of RR small subunit genes and the related enzyme activities operate under different mechanisms regarding cancer progression or patient survival in colorectal tumor cells [28].
As reported by several studies, up-regulation of RRM2B expression could result in resistance to treatment. Moreover, cell hypersensitivity to DNA-damaging agents was observed in the absence of RRM2B [22, 29,30,31,32]. Hence, evaluation of RRM2B expression, in addition to its prognostic role, seems to help physicians to make optimal treatment decisions.
However, this study must be regarded preliminary on account of limited sample size and short follow up. Because, finding newly-diganosed CRC patients without any therapeutic intervention was burdensome and time-consuming and we were not able to do a longer follow up due to restricted budget and timeframe. Taken together, we first investigated the potential of RRM2B in serum as a CRC biomarker. Though a great deal of further researches are needed to confirm the prognostic value of this marker along with other cancer-related genes in CRC.
Conclusion
This study highlights further possible implications of RRM2B as a routine diagnostic and prognostic biomarker for CRC. The expression of RRM2B was downregulated in tumor cells compared to adjacent normal tissue. To the best of the authors’ knowledge, this study presented the serum RRM2B as a biomarker of CRC progression and compared its level among the healthy group and CRC patients before surgery, 1 month, and 3 months after surgery which was significantly diminished over time. Large cohort studies with longer follow-up duration should be designed to explore more variables and calculate OS and CSS of CRC patients regarding their serum RRM2B level. A more accurate understanding of the molecular basis of CRC could aid in estimating tumor behavior and thus developing novel molecular targets for therapeutic strategy in CRC.
Data availability
The original contributions presented in this study are included in the article, further inquiries can be directed to the corresponding author.
References
Rawla P, Sunkara T, Barsouk A (2019) Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol 14(2):89
Lucas C, Barnich N, Nguyen HTT (2017) Microbiota, inflammation and colorectal cancer. Int J Mol Sci 18(6):1310
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F (2017) Global patterns and trends in colorectal cancer incidence and mortality. Gut 66(4):683–691
Dolatkhah R, Somi MH, Bonyadi MJ, Asvadi Kermani I, Farassati F, Dastgiri S (2015) Colorectal cancer in Iran: molecular epidemiology and screening strategies. J Cancer Epidemiol. https://doi.org/10.1155/2015/643020
Shadmani FK, Ayubi E, Khazaei S, Sani M, Hanis SM, Khazaei S et al (2017) Geographic distribution of the incidence of colorectal cancer in Iran: a population-based study. Epidemiol Health. https://doi.org/10.4178/epih.e2017020
Mármol I, Sánchez-de-Diego C, Pradilla Dieste A, Cerrada E, Rodriguez Yoldi MJ (2017) Colorectal carcinoma: a general overview and future perspectives in colorectal cancer. Int J Mol Sci 18(1):197
Chen C-W, Tsao N, Huang L-Y, Yen Y, Liu X, Lehman C et al (2016) The impact of dUTPase on ribonucleotide reductase-induced genome instability in cancer cells. Cell Rep 16(5):1287–1299
Aye Y, Li M, Long M, Weiss R (2015) Ribonucleotide reductase and cancer: biological mechanisms and targeted therapies. Oncogene 34(16):2011–2021
Mazumder A, Tummler K, Bathe M, Samson LD (2013) Single-cell analysis of ribonucleotide reductase transcriptional and translational response to DNA damage. Mol Cell Biol 33(3):635–642
Zhang H, Liu X, Warden CD, Huang Y, Loera S, Xue L et al (2014) Prognostic and therapeutic significance of ribonucleotide reductase small subunit M2 in estrogen-negative breast cancers. BMC Cancer 14(1):1–16
Cho E-C, Kuo M-L, Liu X, Yang L, Hsieh Y-C, Wang J et al (2014) Tumor suppressor FOXO3 regulates ribonucleotide reductase subunit RRM2B and impacts on survival of cancer patients. Oncotarget 5(13):4834–4844
Jiang C, Xu R, Li X-X, Wang Y-Y, Liang W-Q, Zeng J-D et al (2017) p53R2 overexpression in cervical cancer promotes AKT signaling and EMT, and is correlated with tumor progression, metastasis and poor prognosis. Cell Cycle 16(18):1673–1682
Shao J, Liu X, Zhu L, Yen Y (2013) Targeting ribonucleotide reductase for cancer therapy. Expert Opin Ther Targ 17(12):1423–1437
Sanvisens N, De Llanos R, Puig S (2013) Function and regulation of yeast ribonucleotide reductase: cell cycle, genotoxic stress, and iron bioavailability. Biomed J 36(2):51
Weinert T (1998) DNA damage and checkpoint pathways: molecular anatomy and interactions with repair. Cell 94(5):555–558
Liu X, Lai L, Wang X, Xue L, Leora S, Wu J et al (2011) Ribonucleotide reductase small subunit M2B prognoses better survival in colorectal cancer. Can Res 71(9):3202–3213
Liu X, Zhou B, Xue L, Shih J, Tye K, Lin W et al (2006) Metastasis-suppressing potential of ribonucleotide reductase small subunit p53R2 in human cancer cells. Clin Cancer Res 12(21):6337–6344
Byun DS, Chae KS, Ryu BK, Lee MG, Chi SG (2002) Expression and mutation analyses of P53R2, a newly identified p53 target for DNA repair in human gastric carcinoma. Int J Cancer 98(5):718–723
Hayashi H, Furihata M, Kuwahara M, Kagawa S, Shuin T, Ohtsuki Y (2004) Infrequent alteration in the p53R2 gene in human transitional cell carcinoma of the urinary tract. Pathobiology 71(2):103–106
Tian H, Ge C, Li H, Zhao F, Hou H, Chen T et al (2014) Ribonucleotide reductase M2B inhibits cell migration and spreading by early growth response protein 1-mediated phosphatase and tensin homolog/Akt1 pathway in hepatocellular carcinoma. Hepatology 59(4):1459–1470
Xu X, Page JL, Surtees JA, Liu H, Lagedrost S, Lu Y et al (2008) Broad overexpression of ribonucleotide reductase genes in mice specifically induces lung neoplasms. Can Res 68(8):2652–2660
Matsushita S, Ikeda R, Fukushige T, Tajitsu Y, Gunshin K, Okumura H et al (2012) p53R2 is a prognostic factor of melanoma and regulates proliferation and chemosensitivity of melanoma cells. J Dermatol Sci 68(1):19–24
Yousefi B, Rahmati M, Ahmadi Y (2014) The roles of p53R2 in cancer progression based on the new function of mutant p53 and cytoplasmic p21. Life Sci 99(1):14–17
Iqbal W, Demidova EV, Serrao S, ValizadehAslani T, Rosen G, Arora S (2021) RRM2B is frequently amplified across multiple tumor types: implications for DNA repair, cellular survival, and cancer therapy. Front Genet. https://doi.org/10.3389/fgene.2021.328758
Zhang Q, Zhu B, Qian J, Wang K, Zhou J (2019) miR-942 promotes proliferation and metastasis of hepatocellular carcinoma cells by inhibiting RRM2B. Onco Targets Ther 12:8367–8378
Yang Y, Wang G, He J, Ren S, Wu F, Zhang J et al (2017) Gender differences in colorectal cancer survival: a meta-analysis. Int J Cancer 141(10):1942–1949
Nana AW, Wu SY, Yang Y-CS, Chin Y-T, Cheng T-M, Ho Y et al (2018) Nano-diamino-tetrac (NDAT) enhances resveratrol-induced antiproliferation by action on the RRM2 pathway in colorectal cancers. Horm Cancer 9(5):349–360
Ding Y, Zhong T, Wang M, Xiang X, Ren G, Jia Z et al (2019) Integrative analysis reveals across-cancer expression patterns and clinical relevance of ribonucleotide reductase in human cancers. Front Oncol. https://doi.org/10.3389/fonc.2019.00956
Ding Y, Zhong T, Wang M, Xiang X, Ren G, Jia Z et al (2019) Integrative analysis reveals across-cancer expression patterns and clinical relevance of ribonucleotide reductase in human cancers. Front Oncol 9:956
Guittet O, Tebbi A, Cottet M-H, Vésin F, Lepoivre M (2008) Upregulation of the p53R2 ribonucleotide reductase subunit by nitric oxide. Nitric Oxide 19(2):84–94
Yanamoto S, Iwamoto T, Kawasaki G, Yoshitomi I, Baba N, Mizuno A (2005) Silencing of the p53R2 gene by RNA interference inhibits growth and enhances 5-fluorouracil sensitivity of oral cancer cells. Cancer Lett 223(1):67–76
Yokomakura N, Natsugoe S, Okumura H, Ikeda R, Uchikado Y, Mataki Y et al (2007) Improvement in radiosensitivity using small interfering RNA targeting p53R2 in esophageal squamous cell carcinoma. Oncol Rep 18(3):561–567
Acknowledgements
We thank all patients and participants involved in the study.
Funding
This project is funded by the National Institute for Medical Research Development (NIMAD, Contact Grant No. 962765).
Author information
Authors and Affiliations
Contributions
NM: designed the study. KAA: collected the samples. RP and SR: analyzed the data and conducted the statistical analyses. HG and FTA: wrote the manuscript with the assistance of MSM and MR. The final version of the manuscript was approved by all the authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interests to declare.
Ethical approval and consent to participate
This study was approved by the Ethics Committee of the Imam Khomeini’s Hospital affiliated with Tehran University School of Medicine.
Consent for publication
The patients signed a written informed consent form for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mobarra, N., Gholamalizadeh, H., Abdulhussein, K.A. et al. Serum level and tumor tissue expression of Ribonucleotide-diphosphate Reductase subunit M2 B: a potential biomarker for colorectal cancer. Mol Biol Rep 49, 3657–3663 (2022). https://doi.org/10.1007/s11033-022-07205-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07205-7