Abstract
Toll-like receptor (TLR)-mediated signaling pathways induce a proinflammatory microenvironment to eradicate pathogens. However, in rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE), TLRs can promote chronic inflammation. It has been shown that some TLR4 and TLR9 single nucleotide polymorphisms (SNPs) are risk factors for RA and SLE, but these findings have not been replicated in all populations; thus, results are inconclusive. We evaluated the TLR4 Asp299Gly, Thr399Ile, − 1892G/A SNPs, and the TLR9 Pro545Pro SNP to assess potential associations with RA and SLE in Mexican patients. This study included 474 patients with RA, 283 patients with SLE, and 424 healthy controls. We used a 5′ nuclease allelic discrimination assay to genotype individuals for the four TLR4 and TLR9 polymorphisms. We found that the genotype or allelic frequencies of the TLR4 Asp299Gly, Thr399Ile, − 1892G/A, and TLR9 Pro545Pro polymorphisms were similar between patients and controls. We found no association under different genetic models. A haplotype analysis of TLR4 showed no association with either RA or SLE. We found no significant differences in the allelic or genotypic frequencies of TLR4 Asp299Gly, Thr399IIe, − 1892G/A, or TLR9 Pro545Pro between patients and controls. These findings suggested that these variants are not risk factors for RA or SLE in Mexican patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Toll-like receptors (TLRs) are fundamental in the innate immune response, because they induce phagocytosis, the production of proinflammatory cytokines, etc. [1]. In addition, it has been shown that TLRs lead to the generation of apoptotic bodies, hypomethylated CpG islands, etc., which induce TLR-mediated inflammatory signaling pathways. TLRs and TLR-ligands also participate in breaking the tolerance to self-antigens and promoting inflammatory responses [1,2,3]. For example, it has been reported that TLR4 expression is increased in various immune cells of patients with different autoimmune diseases (ADs) [1]. In addition, it has also been shown that different single nucleotide polymorphisms (SNPs) affected TLR4 function, including rs4986790 (Asp299Gly) and rs4986791 (Thr399Ile). These SNPs have been associated with both rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) in a few populations [4,5,6]. However, because TLR4 polymorphisms have rarely been evaluated in both RA and SLE, the data are inconclusive. Moreover, different studies have shown associations between TLR4 Asp299Gly and reductions in the risk of RA [4]; the susceptibility to RA [7], and the severity of RA [6], but other studies could not replicate the findings [8,9,10,11,12]. Additionally, although the TLR4 Thr399IIe SNP has been evaluated in RA, it has not shown an association with this AD [6,7,8, 10, 11], mean, the − 1892G/A (rs10983755) polymorphism has not been evaluated in this AD yet.
A few studies have evaluated the TLR4 Asp299Gly and/or Thr399Ile SNPs in patients with SLE; however, the results were inconclusive. Only one study, carried out in an Indian population, showed an association between SLE and TLR4 Asp299Gly [5, 8, 13]. The other two studies, carried out in Caucasians and Africans, failed to replicate that association [8, 13]. To the best of our knowledge, TLR4 − 1892G/A has not been evaluated in patients with SLE to date.
Only one study investigated TLR9 Pro545Pro in RA, and it did not report an association [12]. However, TLR9 Pro545Pro conferred the risk of SLE in Chinese [14,15,16] and African [17] populations, but not in Brazilian, Polish, or Korean [18,19,20] populations. TLR4 and TLR9 polymorphisms have rarely been investigated in both RA and SLE. Therefore, here, we evaluated four polymorphisms to determine their potential roles in RA and SLE susceptibility in a Latin American population.
Materials and methods
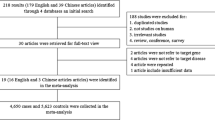
We enrolled 474 patients with RA, 283 patients with SLE, and 424 controls with no history of ADs or chronic inflammation. Patients with RA and SLE were selected and recruited according to the ACR-EULAR 2010 and SLICC 2012 criteria, respectively. Patients with both RA and SLE were excluded from the study. Our original study population had a 9.4:0.6 female to male ratio; therefore, we decided to include only females both in cases and controls to avoid biasing the results. All patients and controls were over 18 years old and unrelated to each other. All participants provided informed consent.
We performed the following protocols as previously described [21]: DNA isolation, PCR reactions, TLR4 polymorphism genotyping (rs4986790A/G: Asp299Gly; rs4986791C/T: Thr399Ile; and rs10983755G/A: − 1892), TLR9 polymorphism genotyping (rs352140G/A: Pro545Pro), and the TaqMan allelic discrimination assays.
Hardy–Weinberg equilibrium (HWE) values for each of the SNPs in the control group were obtained with Finetti software (https://ihg.gsf.de/cgi-bin/hw/hwa1.pl). A p-value < 0.05 indicated a deviation from HWE. We calculated odds ratios (ORs) and p-values with Epidat software (V 3.1) (http://www.sergas.es/MostrarContidos_N3_T01.aspx?IdPaxina=62715). The four TRL4 and TLR9 SNPs were evaluated with allelic, codominant, dominant, and recessive models. Haplotype analyses and linkage disequilibrium (LD) calculations were performed with Haploview (V4.2) software, as previously described [21].
Results
Clinical and demographic data of patients with RA and SLE are shown in Table 1. The genotypic distributions of the TLR4 and TLR9 polymorphisms were in HWE in both patient and control groups. The genotypic and allelic frequencies of TLR4 rs4986790A/G, rs4986791C/T, rs10983755G/A, and TLR9 rs352140G/A were distributed similarly in patients with RA, SLE, and controls (Tables 2 and 3, respectively). Thus, we could not identify an association between the SNPs and either of the ADs, under the different genetic models. To note, no patient or control individual was homozygous for any of the minor genotypes; TLR4 rs4986790A/G, rs4986791C/T, or rs10983755G/A; consequently, we could not test the recessive model (Tables 2 and 3). We also analyzed whether TLR4 or TLR9 variants were associated with serological markers for RA and SLE or with lupus nephritis. However, we did not identify any association (data not shown). Moreover, we did not observe any association between TLR4 haplotypes and RA or SLE. We did not detect LD among the three TLR4 SNPs (data not shown).
Discussion
TLR-mediated signaling pathways are activated by multiple foreign agents. This activation results in phagocytosis, cytokine secretion, lymphocyte activation, and chronic inflammation in RA and SLE [1,2,3]. Genetic alterations can affect the normal functions of different TLRs, including TLR4 [22,23,24,25,26]. For example, studies have shown that TLR4 Asp299Gly and Thr399IIe variants caused hyporesponsiveness to lipopolysaccharides [22] and impaired TLR4/MD-2 responses by altering ligand-dependent dimerization [23]. However, other studies have shown that Asp299Gly, but not Thr399Ile, could affect the binding of ligands and TLR4-mediated signaling [25]. Moreover, the TLR4 − 1892G/A SNP appeared to have no effect on gene expression [24].
Three previous studies showed that TLR4 Asp299Gly was associated with protection against, susceptibility to, and severity of RA in individuals from the Netherlands, China, and Poland, respectively [4, 6, 7]. However, those findings were not replicated in other populations, including another study conducted in the Netherlands [8,9,10,11,12]. In contrast, to date, no study has shown an association between TLR4 Thr399IIe and RA [8, 10, 11]. Our results were consistent with previous findings that showed no association between TLR4 variants and RA. Although TLR4 − 1892G/A was shown to be a risk factor for chronic inflammation in pathogen-induced diseases [26], no study has reported its role in RA (or SLE) susceptibility. Additionally, the TLR9 Pro545Pro variant has only been evaluated in one study that investigated patients with RA, and no association was identified [12]. Similarly, the present study could not identify any association between RA and the TLR4 − 1892G/A or TLR9 Pro545Pro variant. Our finding for TLR4 Pro545Pro was similar to that reported in a French population [12].
Only one study conducted in an Indian population identified an association between SLE and TLR4 Asp299Gly [5]; however, that finding was not replicated in Spanish or Tunisian populations [8, 13]. Similarly, TLR4 Thr399IIe was only evaluated in two studies on SLE, and no association was reported [5, 8]. The present study investigated Mexican patients with SLE, and our results agreed with both previous studies. We found no association between SLE and either TLR4 Asp299Gly or Thr399IIe. On the other hand, although TLR4 − 1892G/A was previously associated with chronic inflammation [26], to our knowledge, it has not been evaluated in patients with SLE. In the present study, our data indicated that TLR4 − 1892G/A was not a risk factor for SLE.
Previously, TLR9 Pro545Pro showed associations with SLE in three different subgroups of a Chinese population and in Tunisians [14,15,16,17]. However, no association was found in Brazilian, Polish, or Korean populations [18,19,20]. Similarly, we did not identify an association in our population. However, the Tunisian and Chinese populations, where TLR9 Pro545Pro was associated with SLE, had different ancestries than the ancestry of our population. Therefore, this variant might only contribute to SLE susceptibility in specific populations.
Our study had some limitations. For example, we lacked ancestry-informative markers. The sample size was only moderate for patients with SLE. We did not evaluate other variants of both genes that could be associated with both RA and SLE in our population. The allele frequencies of the SNPs evaluated in our patients and controls were different from those reported in some populations. This difference could affect the susceptibility to, or protection against, one or both ADs. For example, the minor alleles of both TLR4 variants, rs4986790A/G and rs4986791C/T, were found at frequencies of 2.2%, and 2.0%, respectively, in our controls. These frequencies were similar to those reported in Asians (0.6% and 4%, respectively) (6), but different from those found in Europeans (8%, and 7%, respectively) (8), and Africans (7.4% and 5.6%, respectively) [27]. Finally, the associations between polymorphisms and diseases are evaluated under the allelic and genotypic models [28]. However, the minor allele frequencies for the three TLR4 variants were extremely low (less than 3.3%) in both the patients and controls in our population; consequently, we could not identify minor homozygous genotypes in either group, under the allelic (1 vs. 2) or genotypic (codominant; 11 vs. 12) models, the frequencies of these genetic markers were practically identical; consequently, our results suggested no association between TLR4 and TLR9 variants in RA or SLE.
Conclusion
Our results suggested that three TLR4 variants were not associated with the susceptibility to SLE or RA. This conclusion was based on the evaluation of minor alleles and analyses with the codominant model (11 vs. 12), but not other genetic models, including a recessive model. Additionally, we showed that a TLR9 SNP was not a risk factor for RA or SLE in a Mexican population.
References
Joosten LAB, Abdollahi-Roodsaz S, Dinarello CA et al (2016) Toll-like receptors and chronic inflammation in rheumatic diseases: New developments. Nat Rev Rheumatol 12:344–357
Jiménez-Dalmaroni MJ, Gerswhin ME, Adamopoulos IE (2016) The critical role of toll-like receptors - from microbial recognition to autoimmunity: a comprehensive review. Autoimmun Rev 15:1–8
Elshabrawy HA, Essani AE, Szekanecz Z, Shahrara S (2017) TLRs, future potential therapeutic targets for RA. Autoimmun Rev 16:103–113
Radstake TRDJ, Franke B, Hanssen S et al (2004) The Toll-like receptor 4 Asp299Gly functional variant is associated with decreased rheumatoid arthritis disease susceptibility but does not influence disease severity and/or outcome. Arthritis Rheum 50:999–1001
Rupasree Y, Naushad SM, Rajasekhar L et al (2015) Association of TLR4 (D299G, T399I), TLR9 -1486T>C, TIRAP S180L and TNF-α promoter (-1031, -863, -857) polymorphisms with risk for systemic lupus erythematosus among South Indians. Lupus 24:50–57
Wang Y, Chen L, Li F et al (2017) TLR4 rs41426344 increases susceptibility of rheumatoid arthritis (RA) and juvenile idiopathic arthritis (JIA) in a central south Chinese Han population. Pediatr Rheumatol Online J 15:12
Gębura K, Świerkot J, Wysoczańska B et al (2017) Polymorphisms within genes involved in regulation of the NF-κB pathway in patients with rheumatoid arthritis. Int J Mol Sci 18:1432
Sánchez E, Orozco G, López-Nevot MÁ et al (2004) Polymorphisms of toll-like receptor 2 and 4 genes in rheumatoid arthritis and systemic lupus erythematosus. Tissue Antigens 63:54–57
Sheedy FJ, Marinou I, O’Neill LAJ et al (2008) The Mal/TIRAP S180L and TLR4 G299D polymorphisms are not associated with susceptibility to, or severity of, rheumatoid arthritis. Ann Rheum Dis 67:1328–1331
Zheng B, Li Q, Wei C et al (2010) Lack of association of TLR4 gene Asp299Gly and Thr399Ile polymorphisms with rheumatoid arthritis in Chinese Han population of Yunnan Province. Rheumatol Int 30:1249–1252
Emonts M, Hazes MJMW, Houwing-Duistermaat JJ et al (2011) Polymorphisms in genes controlling inflammation and tissue repair in rheumatoid arthritis: a case control study. BMC Med Genet 12:36
Jaen O, Petit-Teixeira E, Kirsten H et al (2009) No evidence of major effects in several Toll-like receptor gene polymorphisms in rheumatoid arthritis. Arthritis Res Ther 11:R5
Dhaouadi T, Sfar I, Haouami Y et al (2013) Polymorphisms of Toll-like receptor-4 and CD14 in systemic lupus erythematosus and rheumatoid arthritis. Biomark Res 1:20
Xu CJ, Zhang WH, Pan HF et al (2009) Association study of a single nucleotide polymorphism in the exon 2 region of toll-like receptor 9 (TLR9) gene with susceptibility to systemic lupus erythematosus among Chinese. Mol Biol Rep 36:2245–2248
Wen SJ, Wu FY, Fang L et al (2015) Associations of genetic polymorphisms of TLR5, TLR9 and transduction molecules in MyD88 signaling pathway with systemic lupus erythematosus in Zhuang and Han ethnics of Guangxi province, China. Int J Clin Exp Med 8:7872–7880
Zhang J, Zhu Q, Meng F et al (2014) Association study of TLR-9 polymorphisms and systemic lupus erythematosus in northern Chinese Han population. Gene 533:385–388
Elloumi N, Fakhfakh R, Abida O et al (2017) Relevant genetic polymorphisms and kidney expression of Toll-like receptor (TLR)-5 and TLR-9 in lupus nephritis. Clin Exp Immunol 190:328–339
Dos Santos BP, Valverde JV, Rohr P et al (2012) TLR7/8/9 polymorphisms and their associations in systemic lupus erythematosus patients from Southern Brazil. Lupus 21:302–309
Piotrowski P, Lianeri M, Wudarski M et al (2013) Contribution of toll-like receptor 9 gene single-nucleotide polymorphism to systemic lupus erythematosus. Rheumatol Int 33:1121–1125
Hur JW, Shin HD, Park BL et al (2005) Association study of Toll-like receptor 9 gene polymorphism in Korean patients with systemic lupus erythematosus. Tissue Antigens 65:266–270
Ramírez-Bello J, Jiménez-Morales S, Montufar-Robles I et al (2019) BLK and BANK1 polymorphisms and interactions are associated in Mexican patients with systemic lupus erythematosus. Inflamm Res 68:705–713
Arbour NC, Lorenz E, Schutte BC et al (2000) TLR4 mutations are associated with endotoxin hyporesponsiveness in humans. Nat Genet 25:187–191
Yamakawa N, Ohto U, Akashi-Takamura S et al (2013) Human TLR4 polymorphism D299G/T399I alters TLR4/MD-2 conformation and response to a weak ligand monophosphoryl lipid A. Int Immunol 25:45–52
Chen K, Wang YT, Gu W et al (2010) Functional significance of the Toll-like receptor 4 promoter gene polymorphisms in the Chinese Han population. Crit Care Med 38:1292–1299
Figueroa L, Xiong Y, Song C et al (2012) The Asp299Gly polymorphism alters TLR4 signaling by interfering with recruitment of MyD88 and TRIF. J Immunol 188:4506–4515
Wang N, Zhao GQ, Gao A et al (2014) Association of TLR2 and TLR4 gene single nucleotide polymorphisms with fungal keratitis in Chinese Han population. Curr Eye Res 39:47–52
Abida O, Bahloul E, Elloumi N et al (2020) Toll-like-receptor gene polymorphisms in tunisian endemic pemphigus foliaceus. Biomed Res Int 2020:6541761
Lunetta KL (2008) Genetic association studies. Circulation 118:96–101
Acknowledgement
The authors thank Isela Montufar-Robles for having supported the data analysis. The authors are grateful to all participants of this study.
Author information
Authors and Affiliations
Contributions
M.D. REB-C participated with the recruitment of patients with RA and SLE. MSc. JCL-V and PhD. ISA-U implemented the experiments, also participated with the evaluation and data analysis. PhD JR-B was responsible for the conception and design of the experiments. PhD JR-B and ISA-U contributed to the writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no personal or financial conflicts of interest regarding the present study.
Ethical approval
This study was conducted according to the Declaration of Helsinki and approved by the Research and Bioethics Committee of HJM (Registry Number 0446/18-I).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aranda-Uribe, I.S., López-Vázquez, J.C., Barbosa-Cobos, R.E. et al. TLR4 and TLR9 polymorphisms are not associated with either rheumatoid arthritis or systemic lupus erythematosus in Mexican patients. Mol Biol Rep 48, 3561–3565 (2021). https://doi.org/10.1007/s11033-021-06371-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-021-06371-4