Abstract
Genetic variations of microRNA encoding genes influence various sorts of diseases by modifying the expression or activity of microRNAs. MicroRNA 146a is an epigenetic regulator of immune response through controlling the type I interferon (IFN) and nuclear factor kappa B (NF-κB) pathways. Genetic variations of microRNA 146a impact the susceptibility to systemic lupus erythematosus (SLE) and its clinical presentations. This study aimed to investigate the polymorphisms of microRNA-146a gene (rs2431697 and rs57095329) in patients with SLE and its association with disease activity. Sixty-five patients with SLE and 40 apparently healthy controls were enrolled in this study. Patients were subjected to history taking, clinical examination, and disease activity evaluation by SLEDAI score. The microRNA-146a variants were determined by allele discrimination real-time PCR method in all participants. We found a statistically significant association between rs2431697 T allele and SLE (P-value < 0.05), but there was no significant association between rs57095329 and SLE. The T/T genotype of microRNA-146a rs2431697 was associated with lupus nephritis, higher disease activity, and autoantibodies production. The microRNA-146a rs2431697 T allele could be a potential risk factor that contributes to SLE susceptibility, development of lupus nephritis, and disease activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is characterized by variable clinical presentations as a result of autoimmunity in genetically susceptible individuals upon environmental trigger factors. The obscured pathogenesis and the ongoing scientific discoveries of this disease susceptibility urge the research for more specific biomarkers and gene expression analyses; aiming for providing the optimum management [1, 2].
Epigenetics is the study which concerns with the inherited variations of gene expression modification rather than the alteration of the genetic code itself (do not involve alterations in the DNA sequence). Epigenetic mechanisms include the DNA CpG methylation, a diversity of covalent histone alterations, and microRNAs. These mechanisms may result in various disorders such as autoimmune, inflammatory diseases, and cancer [3].
The microRNA-146a; an epigenetic regulator of immune response, interferes with the IFN type I production and signaling cascade which is a key pathway in SLE pathogenesis. This interference is mediated by targeting both the tumor necrosis factor receptor-associated factor 6 (TRAF6), and the signal transducer and activator of transcription 1 (STAT1) [4]. Also, microRNA-146a acts as a crucial molecular constraint and prevents the hyperactivity of the immune system and malignant transformation by attenuating NF-κB signaling. This may be caused by targeting mRNAs that encode interleukin-1 (IL-1), receptor-associated kinase l (IRAK1), and TRAF6 which are members of NF-κB signaling pathways [5].
Single nucleotide polymorphism (SNP) is a substitution of a single nucleotide that occurs at a specific position in a certain gene. SNPs; found in microRNA genes, can control their biogenesis and/or modify their target specificity. A SNP may be located in the seed sequence of microRNA; changing their target specificity, or in the primary microRNA stem-loop or passenger strand; interfering with processing and biogenesis of the mature microRNA [6].
Numerous SNPs of microRNA-146a gene can modify the expression level of mature microRNA-146a. The analysis of gene expression revealed that rs2431697(C/T) decreases the expression level of mature microRNA-146a [7].The SNP rs57095329 (A/G) present in the microRNA-146a promoter, diminishes the level of the mature microRNA-146a by lowering the binding affinity of its transcription factor to the microRNA-146a promoter [8].
The previous proved relation between the microRNA-146a and SLE (4) was our impulsion in this study to investigate the polymorphisms of microRNA-146a gene (rs2431697 and rs57095329) in patients with SLE and to evaluate its association with disease susceptibility and activity.
Methodology
Subjects
The present study was conducted on 105 subjects: 65 patients with SLE, presented at inpatients and the outpatients’ clinic of Rheumatology, Rehabilitation and Physical Medicine Department, Benha University Hospitals and 40 age and gender matched apparently healthy individuals as a control group during the period from March 2018 to October 2019. The study was approved by the ethical committee of Benha Faculty of Medicine. Informed written consents were taken from both the patients and control group subjects before the beginning of the study. Both males and females were recruited. Inclusion criteria included age of 18 or above and the diagnosis of SLE was established according to the existence of 4 criteria of the Systemic Lupus Collaborating Clinics (SLICC) classification criteria [9]. This work excluded patients below 18 years old, subjects with drug-induced SLE, and those with autoimmune disease other than SLE as their main diagnosis. Full personal and medical history taking in addition to a thorough clinical examination was done. Assessment of SLE disease activity in patients was done according to the SLEDAI-2K score [10]. The assessed laboratory investigations included complete blood count (CBC) using Sysmex xp-300AM automated hematology analyzer (Sysmex Corporation, Kobe, Japan), erythrocyte sedimentation rate (ESR) according to Westergen method, kidney function tests using Cobas C 501 auto-analyzer (Roche Diagnostics, Mannheim, Germany), antinuclear antibody (ANA) test and anti-double stranded deoxyribonucleic acid (Anti-dsDNA) antibodies by indirect immunofluorescence kits (Inova Diagnostics, Inc., San Diego, USA), anti-smith by ELISA kits (Orgentec Diagnostika Gmbh, Mainz, Germany), Serum level of complement 3 (C3) and complement 4 (C4) levels by turbidimetry using Cobas C 501 auto-analyzer (Roche Diagnostics GmbH, Mannheim, Germany) and urine protein and creatinine levels were measured using Cobas C 501 auto-analyzer (Roche Diagnostics GmbH, Mannheim, Germany). Protein to creatinine ratio (P/C) was calculated by dividing the urinary protein level (mg/dl) by the urinary creatinine level (g/dl) [11].
Molecular testing for microRNA-146a polymorphisms (rs2431697 and rs57095329) by allele discrimination real-time PCR method
DNA extraction
Total DNA was extracted from EDTA treated blood samples using Thermo Scientific Gene JET Genomic DNA Purification Kit (catalogue # k0781, lot 00602330, Thermo Fisher Scientific, MA, USA). EDTA blood samples were digested with proteinase K in the lysis solution. Then, the cell lysates were applied to the spin columns after being mixed with ethanol. These conditions allow the DNA to bind to the silica membrane. The spin columns were efficiently washed with the prepared wash buffers to remove impurities. Genomic DNA was then eluted using a low ionic strength elution buffer. The purity of the eluted DNA was evaluated using Nanodrop 2000 spectrophotometer (Thermo Fischer Scientific, MA, USA). DNA was considered pure when the A260/A280 ratio is approximately 1.8.
Genotyping
Genotyping was performed using the real-time allelic discrimination technique which depends on 2 principles: the 5′-nuclease property of the polymerase enzyme and fluorescence resonance energy transfer. This assay utilizes specific forward and reverse primers in addition to 2 allele-specific TaqMan probes created to target the polymorphism. TaqMan probes possess a fluorescent reporter dye (FAM specific for one allele and VIC specific for the other allele) attached to its 5′ end and a quencher dye at its 3′ end.
The rs57095329 SNP in microRNA-146a gene was determined using the ABI TaqMan allelic discrimination kit (catalogue # 4351379, assay ID C_90078480_10, Applied Biosystems, Carlsbad, CA, USA). The Context Sequence [VIC/FAM] was: CCCCGCGGGGCTGCGGAGAGTACAG[A/G]CAGGAAGCCTGGGGACCCAGCGCCT (VIC dye for allele A, FAM dye for allele G).
The rs2431697 SNP in microRNA-146a gene was determined using the ABI TaqMan allelic discrimination kit (catalogue # 4351379, assay ID C__26693319_10, Applied Biosystems, Carlsbad, CA, USA). The context Sequence [VIC/FAM] was: ATTGGTGGGGCTGAAATAAAAAACC[C/T]CGATTTAGAAATCTGATACAAAAGC (VIC dye for allele C, FAM dye for allele T).
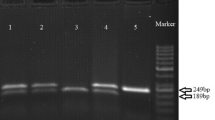
DNA amplification was executed in a 20-μL volume comprising 10 μL of TaqMan genotyping Master Mix 2x (catalogue # 4371353, lot 00722943, Applied Biosystems: Foster City, CA, USA), 0.5 μL of primer/probe, 4.5 μL of nuclease-free water and 5 μL of template DNA. The PCR cycling conditions: after a denaturation time of 10 min at 95 °C and 40 cycles at 95 °C for 15 s and 60 °C for 1 min for annealing and extension were carried out. The fluorescence was determined at the end of each cycle and at the endpoint. Also, two no-template controls were executed with each run to allow correction of background noise from fluorescent probes and to enable the detection of possible DNA contamination. During amplification each distinctively labeled probe paired preferentially with one of the two alleles of the target SNP with different affinity. As amplification continued, a fluorescent signal was generated as the Taq polymerase enzyme cut down the bound probe. Fluorescent signals were deduced automatically using sequence detection software dedicated to Rotor-Gene Q System Real-Time PCR System (Qiagen GmbH, Hilden, Germany).
Statistical analysis
Results were collected, tabulated and statistically analyzed by statistical package SPSS version 20 (SSPS, Inc., Chicago, IL, USA). The Hardy–Weinberg equilibrium was tested for all SNPs by the Pearson chi-square (χ2) test. Differences in alleles and genotype frequencies between cases and controls were weighed by the Pearson x2 test. Odds ratios and 95% Confidence Interval were calculated. For the comparison of clinical and laboratory variables with the distribution of different genotypes, the χ2 test was used for qualitative data and analysis of variance (ANOVA (F)) or Kruskal–Wallis (k) for quantitative data. Statistical significance was considered when the P-value was < 0.05.
Results
The current study included 65 SLE patients, 93.8% females, and 6.2% males with a mean age of 31.85 ± 8.44 years and mean age of disease onset 28.09 ± 8 years. Family history was positive in 12.3% of patients. Clinical and laboratory findings of patients are allocated in Table 1. Thirty-five out of 65 SLE patients (53.8%) had lupus nephritis which was proven by the clinical manifestations (hypertension and lower limb oedema), laboratory investigations (proteinuria, cellular casts and positive anti-ds-DNA) and the histopathological evidence of lupus nephritis obtained from the renal biopsy that was previously done for those patients in their disease course(retrospective data from their files). The mean SLEDAI score was 13.94 ± 6.62.
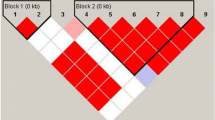
Deviations from Hardy–Weinberg equilibrium were not observed in the data from the studied polymorphisms. This study found a significant association between microRNA-146a rs2431697 polymorphism and SLE. The frequency of the risk allele T was significantly higher in SLE patients than in controls (P = 0.009; OR 2.10, 95%CI 1.19–3.69). The genotype T/T was more frequently observed in the cases (38.5%) compared to the controls (15.0%). On the other hand, no statistically significant association was found between microRNA-146a rs57095329 polymorphism and SLE with a P-value > 0.05 (Table 2).
The T/T genotype of microRNA-146a rs2431697 was significantly more frequent in patients with renal involvement (P = 0.03) and a higher disease activity according to SLEDAI-2k score (P = 0.03) (Table 3). The T/T genotype of microRNA-146a rs2431697 was significantly associated with higher protein creatinine ratio (P = 0.01) (Fig. 1). The T/T genotype of microRNA-146a rs2431697 was significantly more frequent in patients with positive anti dsDNA (P = 0.007) and anti-smith (P = 0.02). There was significant difference between SLE patients with different genotypic patterns of microRNA-146a rs2431697 polymorphisms regarding serum C3 (P = 0.04) and C4 (P = 0.03) (Table 4).
Discussion
The pathogenesis of SLE is multifactorial involving genetic, epigenetic, environmental, and immunological factors. MicroRNA-146a is one of the key regulators of innate and adaptive immune responses. Genetic variation in microRNA genes can control their level of expression thus mediate the pathogenesis and susceptibility of autoimmune diseases [12].
Because of the potential significance of microRNA-146a SNPs in SLE pathogenesis, several studies attempted to evaluate its relationship with SLE development [13,14,15]. These studies reported inconsistent results among different populations. So, the aim of the present study is the investigation of the polymorphisms of microRNA-146a gene (rs2431697 and rs57095329) in a group of Egyptian patients with SLE and its possible association with disease activity.
In this study, we demonstrated an association between the microRNA-146a rs2431697 polymorphism and the incidence of SLE in addition to a specific clinical course variety. On the other hand, there was no significant impact of rs57095329 in the studied SLE patients.
The T/T genotype of microRNA-146a rs2431697 was found in the patients with lupus nephritis. In parallel, we found a significant association between the T/T genotype and the presence of anti-ds-DNA, anti-smith antibodies, and low C3-C4 serum levels. Another significant finding was the association with the higher disease activity that was denoted by high SLEDAI scores in patients with T/T genotype.
The association of rs2431697 polymorphism presence and SLE risk was reported previously. Related studies like genome-wide association study [16], some meta-analyses [13, 14] and some case–control studies [15, 17,18,19] enrolled patients from different populations such as European and Asian. Their results support the hypothesis of the rs2431697 polymorphism relation to SLE susceptibility among different populations.
The anti-ds-DNA and anti-smith antibodies presence and their association with the rs2431697 polymorphism was reported in European [20] and in Asian SLE patients [19].
Gene expression analysis revealed that rs2431697 SNP reduces the level of microRNA-146a expression [8]. A decreased microRNA-146a results in enhanced production and signaling of type I IFN. Also, decreased microRNA-146a in B lymphocytes is associated with enhanced production of autoantibodies through failure of regulation of CD40 signaling [21]. The effect of microRNA-146a on autoantibodies production (anti-ds-DNA and anti-smith) and type I IFN pathway may mediate its role in lupus nephritis pathogenesis and lupus disease activity [22].
There will be a potential value of the proved association between microRNA-146a and lupus nephritis or its autoantibodies production. Animal studies reported that the therapeutic use of microRNA-146a mimics could significantly reduce the renal insult in SLE animal model, down-regulate the proteinuria, and reduction in serum anti-dsDNA antibodies [23]. MicroRNA-146a mimic therapies could be a prospective treatment of the human lupus nephritis.
The unexpected absence of association between the promotor SNP rs57095329 and SLE was interesting and somewhat confusing because literatures suggested that this promotor SNP influence the level of expression of microRNA-146a. It is noteworthy that these literatures clarified that the functional effect of rs57095329 alleles relied on altering the binding affinity of the transcription factor (Ets-1) to the microRNA-146a promotor. It was also demonstrated that this effect can be compensated by increasing the level of Ets-1 in vitro. Also, the epistatic effects of some SNPs in Ets-1 gene should be studied in conjunction with rs57095329 to clarify the gene–gene interaction. One of Ets-1 SNPs that are recommended to be studied is rs10893872 because it was suggested to increase the Ets-1 level. Some other Ets-1 SNPs were previously studied in conjunction with rs57095329 such as rs1128334 which showed no epistatic but additive effect and rs6590330 which showed no effect [17, 24, 25].
It should also be noted that SLE pathogenesis is a very complex process involving the interaction between genetic, epigenetic and environmental factors and even the microRNA-146a expression process is tightly controlled by many factors other than the SNP. These factors include other transcription factors (such as NF-κB) and post-transcriptional regulators (Dicer and Drosha enzymes) [26].
Limitations of the current study included the small sample size, the absence of data about the expression level of mature microRNA146a and INF type 1 that could give better and clear information about the molecular mechanisms underlying our findings and the lack of studying the epistatic effect of Ets-1 SNPs. These limitations should be taken in consideration in future studies.
Conclusion
The results of the present study in keeping with evidence from literature revealed that the microRNA-146a rs2431697 T allele represents a potential genetic risk factor to the susceptibility of SLE. This SNP may have a role in the pathogenesis of autoantibodies production and subsequently lupus nephritis development and a higher possibility of disease activity. On contrary, the role of microRNA-146a rs57095329 as a genetic risk factor could not be elucidated in the studied SLE patients.
References
Jung JY, Suh CH (2017) Infection in systemic lupus erythematosus, similarities, and differences with lupus flare. Korean J Intern Med 32(3):429–438. https://doi.org/10.3904/kjim.2016.234
Gergianaki I, Bertsias G (2018) Systemic lupus erythematosus in primary care: an update and practical messages for the general practitioner. Front Med 5:161. https://doi.org/10.3389/fmed.2018.00161
Richardson BC, Patel DR (2014) Epigenetics in 2013: DNA methylation and miRNA—key roles in systemic autoimmunity. Nat Rev Rheumatol 10(2):72–74. https://doi.org/10.1038/nrrheum.2013.211
Husakova M (2016) MicroRNAs in the key events of systemic lupus erythematosus pathogenesis. Biomed Pap Med Faculty Palacky Univ Olomouc 160(3):327–342. https://doi.org/10.5507/bp.2016.004
Lee HM, Kim TS, Jo EK (2016) MiR-146 and miR-125 in the regulation of innate immunity and inflammation. BMB Rep 49(6):311–318. https://doi.org/10.5483/bmbrep.2016.49.6.056
Króliczewski J, Sobolewska A, Lejnowski D, Collawn JF, Bartoszewski R (2018) microRNA single polynucleotide polymorphism influences on microRNA biogenesis and mRNA target specificity. Gene 640:66–72. https://doi.org/10.1016/j.gene.2017.10.021
Wang Y, Wang X, Li Z, Chen L, Zhou L, Li C et al (2017) Two single nucleotide polymorphisms (rs2431697 and rs2910164) of miR-146a are associated with risk of coronary artery disease. Int J Environ Res Public Health 14(5):514. https://doi.org/10.3390/ijerph14050514
Zha L, Li S, Liu X, Li Z, Jiang J, Huang L et al (2019) Association of miR-146a gene polymorphism at loci rs2910164 G/C, rs57095329 A/G, and rs6864584 T/C with susceptibility to kawasaki disease in Chinese children. Pediatr Cardiol 40(3):504–512. https://doi.org/10.1007/s00246-018-2002-9
Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR et al (2012) Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64(8):2677–2686. https://doi.org/10.1002/art.34473
Gladman DD, Ibanez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29(2):288–291
Karkar A, Abdelrahman M (2010) Protein-to-creatinine ratio: a valid estimate and alternative to 24 hour proteinuria. Saudi J Kidney Dis Transpl 21:949–950
Chen JQ, Papp G, Póliska S, Szabó K, Tarr T, Bálint BL et al (2017) MicroRNA expression profiles identify disease-specific alterations in systemic lupus erythematosus and primary Sjögren's syndrome. PLoS ONE 12(3):e0174585. https://doi.org/10.1371/journal.pone.0174585
Ji JD, Cha ES, Lee WJ (2014) Association of miR-146a polymorphisms with systemic lupus erythematosus: a meta-analysis. Lupus 23(10):1023–1030. https://doi.org/10.1177/0961203314534512
Park R, Lee WJ, Ji JD (2016) Association between the three functional miR-146a single-nucleotide polymorphisms, rs2910164, rs57095329, and rs2431697, and autoimmune disease susceptibility: a meta-analysis. Autoimmunity 49(7):451–458
Löfgren SE, Frostegård J, Truedsson L, Pons-Estel BA, D'Alfonso S, Witte T et al (2012) Genetic association of miRNA-146a with systemic lupus erythematosus in Europeans through decreased expression of the gene. Genes Immunity 13(3):268–274. https://doi.org/10.1038/gene.2011.84
Sheng YJ, Xu JH, Wu YG, Zuo XB, Gao JP, Lin Y et al (2015) Association analyses confirm five susceptibility loci for systemic lupus erythematosus in the Han Chinese population. Arthritis Res Ther 17(1):85. https://doi.org/10.1186/s13075-015-0602-9
Luo X, Yang W, Ye DQ, Cui H, Zhang Y, Hirankarn N et al (2011) A functional variant in microRNA-146a promoter modulates its expression and confers disease risk for systemic lupus erythematosus. PLoS Genet 7(6):e1002128
Lee HS, Kim T, Bang SY, Na YJ, Kim I, Kim K et al (2014) Ethnic specificity of lupus-associated loci identified in a genome-wide association study in Korean women. Ann Rheum Dis 73(6):1240–1245
Tang ZM, Wang P, Chang PP, Hasahya T, Xing H, Wang JP, Hu LH (2015) Association between rs2431697 T allele on 5q33. 3 and systemic lupus erythematosus: case-control study and meta-analysis. Clin Rheumatol 34(11):1893–1902. https://doi.org/10.1007/s10067-015-3045-4
Chung SA, Taylor KE, Graham RR, Nititham J, Lee AT, Ortmann WA et al (2011) Differential genetic associations for systemic lupus erythematosus based on anti–dsDNA autoantibody production. PLoS Genet 7(3):e1001323
Cho S, Lee HM, Yu IS, Choi YS, Huang HY, Hashemifar SS et al (2018) Differential cell-intrinsic regulations of germinal center B and T cells by miR-146a and miR-146b. Nat Commun 9(1):2757
Lai NS, Koo M, Yu CL, Lu MC (2017) Immunopathogenesis of systemic lupus erythematosus and rheumatoid arthritis: the role of aberrant expression of non-coding RNAs in T cells. Clin Exp Immunol 187(3):327–336
Fu HX, Fan XP, Li M, Liu MJ, Sun QL (2019) miR-146a relieves kidney injury in mice with systemic lupus erythematosus through regulating NF-κB pathway. Eur Rev Med Pharmacol Sci 23(16):7024–7032
Leng RX, Wang W, Cen H, Zhou M, Feng CC, Zhu Y et al (2012) Gene–gene and gene-sex epistatic interactions of MiR146a, IRF5, IKZF1, ETS1 and IL21 in systemic lupus erythematosus. PLoS ONE 7(12):e51090. https://doi.org/10.1371/journal.pone.0051090
Wei L, Zhou Q, Hou S, Bai L, Liu Y, Qi J et al (2014) MicroRNA-146a and Ets-1 gene polymorphisms are associated with pediatric uveitis. PLoS ONE 9(3):e91199. https://doi.org/10.1371/journal.pone.0091199
Michlewski G, Cáceres JF (2019) Post-transcriptional control of miRNA biogenesis. RNA 25(1):1–16. https://doi.org/10.1261/rna.068692.118
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflict of interest.
Ethical approval
The study design was approved by the Institutional Research Ethics Committee at the Faculty of Medicine, Benha University (REC-FOMBU) (No. 000014). MoHP No.:0018122017 Certificate No.:1017. All procedures performed were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed written consent was obtained either from all participants.
Research involving animal and human rights
This research involves human participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fouda, M.E., Nour El Din, D.M., Mahgoub, M.Y. et al. Genetic variants of microRNA-146a gene: an indicator of systemic lupus erythematosus susceptibility, lupus nephritis, and disease activity. Mol Biol Rep 47, 7459–7466 (2020). https://doi.org/10.1007/s11033-020-05802-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-020-05802-y