Abstract
Noscapine is an antitumor alkaloid derived from Papaver somniferum plants. Our previous study has demonstrated that exposure of noscapine on primary murine fetal cortical neurons exposed to oxygen–glucose deprivation/reperfusion (OGD/R) has neuroprotective effects. In current study, the effects of noscapine on cardiomyocytes (H9c2 cells) damage caused by 120 minutes (min) of OGD/R were evaluated and we determined whether the addition of BD1047, sigma-one receptor antagonist, prevents the protective effects of noscapine in H9c2 cells through the production of nitric oxide (NO) and apoptosis. To initiate OGD, H9c2 cells was transferred to glucose-free DMEM, and placed in a humidified incubation chamber. Cell viability was assessed with noscapine (1–5 μM) in the presence or absence of BD1047, 24 hours (h) after OGD/R. Cell viability, NO production and apoptosis ratio were evaluated by the MTT assay, the Griess method and the quantitative real-time PCR. Noscapine considerably improved the survival of H9c2 cells compared to OGD/R. Also, noscapine was extremely capable of reducing the concentrations of NO and Bax/Bcl-2 ratio expression. While the BD1047 administration alone diminished cell viability and increased the Bax/Bcl-2 ratio and NO levels. The addition of noscapine in the presence of BD1047 did not increase the cell viability relative to noscapine alone. Noscapine exerted cardioprotective effects exposed to OGD/R-induced injury in H9c2 cells, at least partly via attenuation of NO production and Bax/Bcl-2 ratio, which indicates that the sigma-one receptor activation is involved in the protection by noscapine of H9c2 cells injured by OGD/R.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemic heart disease and many cardiovascular diseases are the most leading causes of human mortality globally and one of the most susceptible organs to both ischemia/reperfusion (I/R) damage is the heart that leads to myocardial cell damage [1, 2]. The imbalance between myocardial oxygen supply and demand was exacerbated when cells were subjected to prolonged reperfusion restoration and concurrent reoxygenation [3]. Critical strategies should therefore be regarded for the prevention and reduction of myocardial injury following I/R. One of the methods currently used to treat myocardial I/R injury is the use of conservative drug therapy. It is therefore very essential to define a new drug therapy that may restrict the harm caused by a reduction in I/R injury [3, 4].
In reality, the absence of oxygen and glucose creates ischemia, leading to an enormous accumulation of glutamate. Glutamergic excitation contributes to a rise in intracellular calcium in the cells, which can eventually boost NO concentrations [5, 6]. These events lead to irreversible apoptotic and necrotic cell death, which could play a significant part in myocardial I/R injury [7, 8].
In many researches, OGD is frequently used as an in vitro model for ischemic injury in cultured cardiomyocytes because it is similar to in vivo cardiac ischemia models. Therefore, in this inquiry, an in vitro OGD model is used to study I/R injury to cardiomyocytes cells [2].
Dumont & Lemaire [9] for the first time reported that sigma receptors were present in the heart after that, Novakova et al. [10] proved that 75% of the sigma receptors in the heart were associated with sigma-one receptors. Many researchers have concentrated their studies on sigma-one cardiac receptor functions to explore several experimental models [11,12,13]. According to studies sigma-one receptors are expressed in intracardiac neurons, atrial and ventricular cardiomyocytes in rats and guinea pigs [14, 15]. These receptors have therefore shown much promise as a pharmacological goal for the therapy of many myocardial illnesses [13].
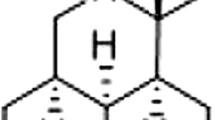
Noscapine is an antitumor alkaloid derived from Papaver somniferum plants, which causes various bioactivity, such as antitussives, antitumor and anti-inflammatory effects, over many years [6, 16, 17].
Our previous study showed that noscapine may reduce the OGD of primary murine fetal cortical neurons by decreasing the production of NO and intracellular calcium modulation [6]. Another study also demonstrated that noscapine pretreatment for renal ischemia–reperfusion injury in rats protected both renal tissue composition and function [18]. However, the effect of noscapine on OGD/R in H9c2 cardiomyocyte cells has not yet been investigated.
In this research, we evaluated the effects of noscapine on H9c2 cell damage induced by 120 min of OGD/R to imitate myocardial I/R conditions and also defined whether the addition of BD1047 in the presence of noscapine could inhibit the protective effects of noscapine in H9c2 cells through the production of NO and apoptosis.
Material and methods
Materials
The H9c2 cells, a cardiomyocyte cell line, were a gift from Cellular and Molecular Research Center, Iran University of Medical Science, Tehran, Iran. Noscapine, NG nitro-L-arginine methyl ester (L-NAME), 3-(4,5-dimethylthiazol-2- yl)-2,5-diphenyl-tetrazolium bromide (MTT), N-[2-(3,4-Dichlorophenyl)ethyl]-N-methyl-2-(dimethylamino)ethylamine dihydrobromide (BD1047 dihydrobromide) and modified Griess reagent were obtained from sigma-aldrich. Dulbecco’s Modified Eagle’s Medium (DMEM) without glutamine, fotal bovine serum (FBS), horse serum and 1% penicillin- streptomycin were obtained from Gibco. All other chemicals were obtained from Merck Co. (Darmstadt, Germany).
H9c2 cell culture
Rat embryonic ventricular H9c2 cardiomyocytes were maintained in DMEM medium, supplemented with a 10% (v/v) fetal bovine serum (FBS) and 1% penicillin/streptomycin, in a CO2 incubator at 37 °C [19]. Briefly, H9c2 cells were seeded on 96-well plates at a density of 104 cells in each well and cultured for 24 h. H9c2 cells were seeded at 104 cells/well in 96-well culture plates, incubated for 48 h and then treated with noscapine for 24 h. MTT assay was performed for the determination of cell viability. To examine the noscapine effects, cell cultures were treated 24 h before oxygen–glucose deprivation with different concentration of noscapine (1-5 µM).
H9c2 OGD/Reperfusion model
For the OGD/R experiments, the medium was replaced with glucose free DMEM medium and subjected to small anaerobic chamber (95% N2, 5% CO2) for 120 min to mimic an in vitro model of myocardial OGD/R at 37 °C. After this time, the anaerobic chamber was opened and medium was replaced with DMEM. Cell cultures were incubated in normoxic conditions (95% air, 5% CO) at 37 °C for 24 h.[20]. All measurements were made in duplicate, and each experiment was repeated at least three times.
Cell viability assay (MTT assay)
The cell viability was examined using the colorimetric 3-[4,5-dimethylthylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide (MTT) assay as described [20].
24 h after the OGD, the cell cultures were added with 0.5 mg/mL MTT in DMEM, at 37 °C under 5% CO2, for 4 h. Then, solution was removed, and the formazan crystals were solubilized in 100μL dimethyl sulfoxide at 37 °C for 15 min. The absorbance of the reaction solution at 570 nm was read by using ELISA-plate reader (Dynex, Richfield, MN, USA).
Quantitative real-time PCR (qRT-PCR)
Total RNA of H9c2 cells was extracted from tissue using RNXplus (Cinagen, Iran). The quantity and quality of the isolated RNA was extracted by measurement of the optical density at 260 and 280 nm using Ultrospec 2000 UV/VIS Spectrophotometer (Pharmacia) and agarose gel electrophoresis, respectively. cDNAs were generated from 1 µg of total RNA by reverse transcription using the CycleScript Reverse Transcription system (Bioneer, Korea) according to the manufacturer’s instructions. The mRNA expression levels of Bax, Bcl-2 and B-actin were determined by quantitative real-time RT-PCR, using a Rotor-Gene 6000 Real-Time Thermal Cycler (Qiagen, Germany). B-actin mRNA was used as the internal control. All primers were purchased from Qiagen. The PCR reactions were performed in a volume of 10 µL, containing 1 µL of cDNA, 5 µL of AccuPower® 2X GreenStar qPCR Master Mix (Bioneer, Korea), and 10 pM of each forward and reverse specific primer based on suggestions from the supplier. One RNA sample of each preparation without a real-time reaction was provided as a negative control in the subsequent PCR.
According to the following program: reaction mode was set at 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s and 60 °C for 1 min. In order to determine the melting temperature of the product the melting curve is checked after amplification.
The sequences of the primers are as follows:
B-actin forward: CGGTCAGGTCATCACTATCGG, B-actin reverse: ATGCCACAGGATTCCATACCCA, Bax forward: GAGGCAGCGGCAGTGATG, Bax reverse: GATCCTGGATGAAACCCTGTAGC, Bcl2 forward: GGAGCGTCAACAGGGAGATG TACATC, Bcl2 reverse: AGCCAGGAGAAATCAAACAGAGG.
All samples and controls are standardized against B-actin, the reference gene. There were no template controls and reverse transcriptase controls in each PCR run. All tests were performed three times as independent PCR runs for each cDNA sample. The ΔΔCT (Cycle Threshold) procedure was used to measure targeted mRNA fold changes in samples. Each gene expression was standardized with respect to the content of B-actin mRNA [21].
Measurement of nitrite levels
To detect NO production in the culture medium, we used modified Griess reagent, a widely-accepted colorimetric method for measuring NO levels. 24 h after OGD/R, the supernatant of medium in each well was removed and transferred to microtube to centrifuge at 10,000 RCF for 10 min at 4 °C. 100 μL of the supernatant and 100 μL Griess reagent should be mixed and incubate at dark room temperature for 15 min [6]. The results were read at 570 nm using a microplate reader. A sodium nitrite standard curve was constructed from sodium nitrite in a serial dilution.
Statistical analysis
All results are presented as means ± SEM. P < 0.05 was considered statistically significant. Significant differences among multiple groups were examined using one-way analysis of variance (ANOVA) followed with Dunnett test. Data were analyzed using Graph Pad Prism 6.0 software.
Results
The effect of noscapine on cell viability
We analyzed the cell viability of different concentrations of noscapine on H9c2 cells by MTT assay (Fig. 1). H9c2 cells were treated with different concentrations of noscapine (ranging from 1 µM to 10 µM) for 24 h, and cell viability was evaluated. Noscapine did not have a significant effect on cell viability, up to a concentration of 5 µM compared with external control group. At dose of 6 µM and above the cell viability was decreased. The viability of external control cells was set at 100%.
The effects of noscapine in the presence and absence of BD1047 on H9c2 cells against OGD-induced cell injury
H9c2 cells lost their normal shape in the OGD / R group from spindle form to round and smaller shape, with reduced cell refraction due to morphological alterations. The cell morphology improved after treatment with 5 μM of noscapine (Fig. 2a). The viability of H9c2 cells against 120 min OGD/R-induced injury alone or with different concentrations of BD1047 was determined by the MTT assay, which demonstrated that the cell viability caused by BD1047 was diminished in a dose-dependent manner (Fig. 2b). Then, we investigated the effects of various concentrations of noscapine (1–5 µM) in the presence and absence of BD1047 on the response of H9c2 cultures to OGD followed by 24 h reperfusion (Fig. 2c). Pretreatment with 1–5 µM of noscapine dramatically increased the viability of the H9c2 cells against OGD/R. Effect of noscapine on cell viability reached a plateau at 5 µM (80.02% ± 2.28). When 5 µM BD1047 was added to H9c2 cells alone, a significant decrease in cell viability was observed (39.83% ± 1.19).
Effect of noscapine on cell viability in H9c2 cells after OGD/R. (a) Cytomorphological changes after OGD/R with or without noscapine. (b) The effects of different concentrations of BD1047 on H9c2 cells subjected to a 120 min OGD/24 h reperfusion. ***p < 0.001 compared to OGD group. (c) The effects of different concentrations of noscapine in the presence and absence of BD1047 on H9c2 cells subjected to a 120 min OGD/24 h reperfusion. #p < 0.01 compared to noscapine group. ###p < 0.001 compared to noscapine 5 µM groups. The data are expressed as the percentage of viable cells in OGD-exposed plates relative to external control group (100%). OGD group: the plates exposed to OGD conditions without addition of drugs, external control group: the plates not exposed to OGD and without addition of drugs
To ensure the involvement of the sigma-one receptors in OGD-treated cells, cell survival was defined against 120 min OGD with concomitant addition of 5 µM BD1047 and various concentrations of noscapine (Fig. 2c). Our results showed that different concentrations of noscapine in the presence of BD1047 could not have an effect on cell survival compared to noscapine alone indicated that BD1047 eliminated the cardioprotective effects of noscapine in H9c2 cells after 120 min OGD/R. The viability of the external control cells was regarded as 100% and used to standardize 120 min OGD treatment group.
The effect of noscapine in the presence and absence of BD1047 on OGD/R and NO production in H9c2 cells culture
The level of NO production of H9c2 cells injured by 120 min OGD/R was explored to further investigate the protective effects of different concentrations of noscapine.
The measurements of NO production against OGD-R-induced cardiotoxicity were evaluated using the modified Griess reagent. Treatment of H9c2 cells to OGD/R significantly increased nitrite production (2.44 ± 0.03) relative to the external control group. Our result showed that exposure of noscapine, decreased OGD/R-induced NO production compared with the BD1047 treated group (2.90 ± 0.02). While H9c2 cells were treated with noscapine in the presence of BD1047, the level of NO production decreased as shown in Fig. 3 compared with BD1047 treated group alone. Although there is no difference between the noscapine group and the BD1047 + noscapine group, 5 μM noscapine in combination with BD1047 has been shown to significantly reduce NO production compared to other noscapine + BD1047 concentrations. The effects of L-NAME (100 µM), a NOS inhibitor, on NO production were also evaluated. The results demonstrated that NO production induced by 120 min of OGD/R was significantly decreased by L-NAME (0.68 ± 0.02).
The effects of noscapine in the presence and absence of BD1047 on NO production in H9c2 cells during a 120 min OGD/R-induced cell injury. ###p < 0.001 compared to noscapine 5 µM group. *p < 0.01 compared to BD1047 + noscapine 5 µM group. ***p < 0.001 compared to BD1047 + noscapine 5 µM group. OGD group: the plates exposed to OGD conditions without addition of drugs, external control group: the plates not exposed to OGD and without addition of drugs
The effect of noscapine in the presence and absence of BD1047 on Bax/Bcl-2 ratio expression against OGD-induced cell injury
To further confirm the cardioprotective effect of noscapine on cardiomyocyte injury, we examined the Bax/Bcl-2 ratio expression of H9c2 cells against 120 min OGD/R.
qRT PCR analysis revealed that OGD-R resulted in a marked increase in the Bax/Bcl-2 ratio (3.49 ± 0.09) relative to that of the external control group. In addition, the results showed that the Bax/Bcl-2 ratio was significantly attenuated by 5 μM noscapine in H9c2 cells treated with OGD/R (2.34 ± 0.08), while BD1047 reversed the Bax/Bcl-2 ratio expression changes (5.19 ± 0.07). After OGD/R, noscapine in the presence of BD1047 failed to evoke a significant decrease in Bax/Bcl-2 ratio expression relative to noscapine alone. (Fig. 4).
Discussion
Noscapine is an alkaloid antitumor of Papaver somniferum plants with no significant analgesic, sedative or euphoric effects. Recently, our lab and others have shown a protective impact of noscapine against OGD/R caused injury to primary murine fetal cortical cells and kidney I/R injuries in male Wistar rats, respectively [6, 18].
However, it has not been clarified whether noscapine could have a cardioprotective effect following OGD/R-induced injury to H9c2 cells. H9c2 cells are rat embryonic myoblast cells and maintain several cardiac-like characteristics and have been widely used in in vitro models to study cardiac ischemia/hypoxia [22]. Therefore, in the present investigation, we used the pretreatment protocol to demonstrate distinct concentrations of noscapine cardioprotection effects against OGD/R-induced injury in H9c2 cells. Another objective of this research was to determine whether BD1047, modulated noscapine effects via sigma-one receptor through NO production and apoptosis (Bax/Bcl-2 ratio).
Recent research has shown that OGD/R-induced ischemic heart damage has been widely used to study the cardioprotective and cardiotoxic impacts of multiple agents and to build a cell model of myocardial ischemia reperfusion injury such as H9c2 cardiomyocyte [4, 23, 24]. Therefore, we used OGD/R injury model to mimic myocardial I/R and to explore the impact of noscapine with and without BD1047. In this research, cell viability was evaluated using MTT assay based on OGD/R induced H9c2 cell damage.
Sigma receptors specifically sigma-one receptor have been revealed to be a distinctive receptor and have been expressed in the central nervous system and other peripheral tissues. Subsequent studies demonstrated that activation of sigma-one receptor play an important role in many diseases such as Alzheimer disease, depression, Parkinson disease, neuropathic pain, cancer, amnesia, and ischemic brain injury [11, 13, 25, 26]. Recently, the function of sigma-one receptors in the protection against myocardial I/R and cardiovascular arrhythmias has also been clarified [13, 26, 27]. For instance, Novakova et al. [27] have shown that the gene expression of sigma receptors has been increased by multiple stress variables, such as immobilization and/or hypoxia in the left ventricles of rat hearts. Also, Novakova et al. [28] and Stracina et al. [14] also discovered that sigma-one receptor expression was boosted when long-term haloperidol was administered in rats and guinea pigs. However, few studies have been recorded on the function of sigma-one receptors in cardiac cells [13].
Some trials have shown that noscapine impacts have been inhibited by sigma receptor antagonists. For instance, Kamei et al. [29] have shown that the antitussive impacts of non-narcotic drugs such as noscapine and dextromethorphane have reduced in the presence of rimicazole, a sigma site antagonist. Based on these features of sigma receptors, we thought that noscapine could also have a cardioprotective impact by modulating sigma-one receptor.
In this study, we examined the potential mechanism by which noscapine would protect the cell viability of H9c2 cells exposed to OGD. H9c2 cells exposed to 120 min OGD/R showed reduced cell viability over a 24-h period. This information shows that the OGD/R model has been effectively performed. By comparison, distinct concentrations of noscapine efficiently enhanced the viability of H9c2 cells caused by OGD/R in a dose-dependent manner (with the exception of noscapine concentrations in 4 and 5 μM), indicating the cardioprotective effect of noscapine. In order to confirm the involvement of sigma-one receptors in restoring cell viability in OGD-treated cells, H9c2 cells were pre-treated with BD 1047, sigma-one receptor antagonist, and noscapine was subsequently added. Our results have shown that enhanced cell survival with pretreatment of BD1047 in H9c2 cells against OGD / R has been abolished. As well as, BD1047 decreased the noscapine-induced increase in cell viability following 120 min OGD/R.
This means that although noscapine was cardioprotective against OGD/R, it did not provide a cardioprotective advantage to H9c2 cells by pretreatment with BD1047, indicating that noscapine could cause this protection by growing cell survival associated with the activation of sigma-one receptors. In reality, the pharmacological stimulation of the sigma-one receptor showed protective impacts in this experimental OGD/R model. This is consistent with prior studies which have shown that the antitussive effects of dextromethorphan and noscapine (non-narcotic antitussive drugs) in mice abolished by rimicazole, sigma-one receptor antagonist. On the contrary, morphine (narcotic antitussive drugs) has not been shown to have this effect [29]. Also, our previous study has shown that the neuroprotective effects of noscapine have been inhibited by co-administration of BD1047, a sigma-one receptor antagonist against 60 min OGD/R [30].
Furthermore, we investigated the mechanisms responsible for the H9c2 cardiomyocyte effects of noscapine against OGD/R process by determining the levels of NO and apoptosis. To further confirm the role of the sigma-one receptors in mediating the cardioprotective effect of noscapine on H9c2 cells, we studied the effects of co-administration of BD1047 and noscapine on OGD/R-induced NO production.
Nitric oxide synthases (NOS) are a family of enzymes catalyzing the production of NO from L-arginine [31]. The reaction of NO with superoxide anion to form the potent oxidant peroxynitrite is a key element which can interacts with lipids, DNA, and proteins and caused oxidative and DNA damage [32]. NO is a major factor in the cardiovascular system which was implicated to play an important mediator in the pathophysiology of myocardial I/R injury [33, 34].
In many studies elucidated that under pathological conditions such as myocardial I/R injury, myocardial infarction and chronic heart failure, peroxynitrite production induced cell damage [35, 36]. In addition, mechanisms of different types of sigma receptor ligands have been documented in recent decades, including in vitro [37] decrease in glutamate-and NMDA-induced NO synthase (NOS) activation and attenuate ischemia-induced NO in vivo production [38]. For example, Wang et al. [36] explained that in isolated rat hearts, 30 min of ischemia followed by 45 min of reflow, the release of nitric oxide, superoxide, and peroxynitrite was increased in the first 2 min of reperfusion, resulting in cellular injury. Schulz et al. [31] demonstrated that interstitial NO production was increased after early ischemia and reperfusion in cardiac cells through the activated NOS isoforms (dependent) and NOS-independent pathways. In addition, Bhardwaj et al. [38] showed that one possible mechanism for in vivo defense of striatum ischemic neuronal injury is to decrease the rate of NO production by potent sigma-one receptor 4-phenyl-1-(4-phenylbutyl) piperidine (PPBP). However, this effect was inhibited by DuP 734, a sigma-one receptor antagonist.
In the present study, we noted that NO levels in H9c2 cells were markedly elevated in response to OGD/R. Treatment with noscapine decreased NO levels in H9C2 cells, which indicated that the influence of noscapine on the NO levels against OGD/R might be a significant component of its cardioprotective effect for H9c2 cells.
Our next experiment showed that BD1047 increased the level of NO in H9c2 cells, and 5 μM noscapine significantly reduced this effect, but not significantly at 3 and 4 μM noscapine concentrations. The effect of noscapine on NO production seems to have reached a plateau of 4 μM. Although there was no significant reduction in NO production during OGD / R in the presence of noscapine and BD1047 + noscapine, 5 μM of noscapine + BD1047 significantly reversed the effect of BD1047 on NO production compared to other noscapine + BD1047 concentrations. This means that high concentrations of noscapine may have an impact on the sigma-one receptor. Our findings suggested the involvement of stimulating sigma-one receptors in the cardioprotective effects of noscapine during OGD / R-induced NO production injury in H9c2 cells.
These data appears to be in agreement with the work carried out by our previous study which indicated that in primary cultured murine cortical neurons, noscapine could decrease NO production against 30 min OGD/R [6]. In another study, it was examined that pre-treatment of murine RAW 264.7 and human THP-1 macrophages with brominated noscapine analogs can significantly reduce NO and TNFa release compared to cells treated with DMSO (untreated control) [39]. Therefore, our result suggested that noscapine activates the sigma-one receptors to reduce NO production against OGD/R-induced injury in H9c2 cells.
It has been demonstrated that high concentrations of NO caused inflammatory processes during I/R, inhibit the function of heart and led to induce necrosis and apoptosis in isolated cardiomyocytes and hearts [31]. Taimor et al. [34] have shown that incubation of isolated adult cardiomyocytes from rats with NO-donor against ischemic conditions induces cGMP-dependent apoptosis. Another study have shown that 30 min of exposure of rats isolated perfused hearts to the NO donor ( ±)-Snitroso-N-acetylpenicillamine (SNAP) induced apoptosis, which could lead to an anti-apoptotic gene program in cardiomyocytes [40]. Accordingly, to confirm that noscapine could protect OGD-induced H9c2 cell injury from apoptosis, the Bax/Bcl-2 ratio was detected by quantitative real-time PCR.
It has been well acknowledged that the phenomenon of myocardial ischemia can trigger apoptosis during heart failure progression which can be accelerated by reperfusion [22, 41, 42]. Immediately after the onset of ischemia and during reperfusion, an apoptotic process was significantly established and rise irreversible destructive effects of I/R. Thus blocking of apoptosis was believed to be an effective therapeutic strategy for treatment of myocardial I/R injury [42]. As well as, a number of investigations indicated that OGD/R injury is one of the most important methods to induce myocardial apoptosis [22, 43]. Hence, in this work we created OGD/R injury to investigate the apoptosis process during ischemia.
In the present study, the results indicated that noscapine significantly reduced Bax/Bcl-2 ratio from OGD-stimulated H9c2 cells. This observation suggests that by upregulating the expression of Bcl‐2 and downregulating Bax, noscapine can decrease OGD/R-induced apoptosis of H9c2 cells. On the other hand, noscapine significantly reduced the Bax / Bcl-2 ratio compared to BD1047 + noscapine. This evidence suggests that noscapine could not have had an effect on the Bax / Bcl-2 ratio in the presence of BD1047.
These results are consistent with previous studies which demonstrate that during ischemia, the level of mRNA expressions of Bax/Bcl-2 ratio in H9c2 cells was up-regulated [22, 44]. For example, Gao et al., [11] showed that PRE-084, sigma-one receptor agonist, has a cardioprotective effect by reducing myocardial ischemia/reperfusion damage in rats as demonstrated by preserved cardiac function and diminished myocardial apoptosis, such as upregulating the expression of Bcl‐2 while reducing Bax expression and thus increasing the Bcl‐2 to Bax ratio. Jing et al. [22] showed that treatment of H9c2 cells against hypoxia led to an increase in the level of mRNA expressions of the Bax/Bcl-2 ratio. Wang et al. [44] also demonstrated that the treatment of H9c2 cells against OGD can induce Bax/Bcl-2 ratio activation. Yang et al. [45] recorded that an active, prototypic sigma-one receptor agonist, PPBP protects primary cortical neuronal cultures against 120 min OGD through increased anti-apoptotic protein Bcl-2 mRNA levels. This effect was fully blocked by rimcazole, an antagonist of sigma-one receptors. According to these results indicated that reducing of Bax/Bcl-2 ratio against OGD-induced injury on H9c2 cells mediated by noscapine may be involved in the function of sigma-one receptors.
In conclusion, the results of this study show that noscapine increased H9c2 cell survival against 120 min OGD/R-induced injury. These findings also suggest that noscapine decreases Bax/Bcl-2 ratio and NO production following OGD / R injury, probably due to the modulation of the sigma-one receptor.
References
Li Y-Y, Xiang Y, Zhang S et al (2017) Thioredoxin-2 protects against oxygen-glucose deprivation/reperfusion injury by inhibiting autophagy and apoptosis in H9c2 cardiomyocytes. Am J Transl Res 9(3):1471–1482
Zheng K, Sheng Z, Li Y et al (2014) Salidroside inhibits oxygen glucose deprivation (ogd)/re-oxygenation-induced h9c2 cell necrosis through activating of akt–nrf2 signaling. Biochem Biophys Res Commun 451(1):79–85
Kalogeris T, Baines CP, Krenz M et al (2016) Ischemia/Reperfusion. Compr Physiol, Hoboken
Sun N, Yang L, Zhang Q et al (2018) Pioglitazone alleviates oxygen and glucose deprivation-induced injury by up-regulation of miR-454 in H9c2 cells. IJBMS 21(10):1050
Tavakoli-Far B, Rahbar-Roshandel N, Rahimi-Moghaddam P et al (2009) Neuroprotective effects of mebudipine and dibudipine on cerebral oxygen–glucose deprivation/reperfusion injury. Eur J Pharmacol 610(1–3):12–17
Vahabzadeh G, Rahbar-Roshandel N, Ebrahimi S-A et al (2015) Neuroprotective effect of noscapine on cerebral oxygen–glucose deprivation injury. Pharmacol Rep 67(2):281–288
Huang X, Zuo L, Lv Y et al (2016) Asiatic acid attenuates myocardial ischemia/reperfusion injury via Akt/GSK-3β/HIF-1α signaling in rat H9c2 cardiomyocytes. Molecules 21(9):1248
Zhao L, Zhuang J, Wang Y et al (2019) Propofol ameliorates H9c2 cells apoptosis induced by oxygen glucose deprivation and reperfusion injury via inhibiting high levels of mitochondrial fusion and fission. Front Pharmacol 10:61
Dumont M, Lemaire S (1991) Interaction of 1, 3-di (2-[5-3H] tolyl) guanidine with σ2 binding sites in rat heart membrane preparations. Eur J Pharmacol 209(3):245–248
Novakova M, Ela C, Barg J et al (1995) Inotropic action of σ receptor ligands in isolated cardiac myocytes from adult rats. Eur J Pharmacol 286(1):19–30
Gao Q-J, Yang B, Chen J et al (2018) Sigma-1 receptor stimulation with PRE-084 ameliorates myocardial ischemia-reperfusion injury in rats. Chin Med J 131(5):539
Maurice T, Su T-P (2009) The pharmacology of sigma-1 receptors. Pharmacol Ther 124(2):195–206
Stracina T, Novakova M (2018) Cardiac sigma receptors-an update. Physiol Res 67(4):5561–5576
Stracina T, Slaninova I, Polanska H et al (2015) Long-term haloperidol treatment prolongs QT interval and increases expression of sigma 1 and IP3 receptors in guinea pig hearts. Tohoko j Eex Med 236(3):199–207
Zhang H, Cuevas J (2005) σ Receptor activation blocks potassium channels and depresses neuroexcitability in rat intracardiac neurons. J Pharmacol Exp Ther 313(3):1387–1396
Altinoz MA, Topcu G, Hacimuftuoglu A et al (2019) Noscapine, a non-addictive opioid and microtubule-inhibitor in potential treatment of glioblastoma. Neurochem Res 44(8):1–11
Vahabzadeh G, Ebrahimi S-A, Rahbar-Roshandel N et al (2016) The effect of noscapine on oxygen-glucose deprivation on primary murine cortical neurons in high glucose condition. IJPR 15(2):501
Khanmoradi M, Mard SA, Aboutaleb N et al (2014) The protective activity of noscapine on renal ischemia–reperfusion injury in male Wistar rat. IJBMS 17(4):244
Cao A, Li X (2019) Bilobalide protects H9c2 cell from oxygen-glucose-deprivation-caused damage through upregulation of miR-27a. Artif Cells Blood Substit Biotechnol 47(1):2980–2988
Liu J, Sui H, Zhao J et al (2017) Osmotin protects H9c2 cells from simulated ischemia-reperfusion injury through AdipoR1/PI3K/AKT signaling pathway. Front Psychol 8:611
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 25(4):402–408
Jing L, Li Q, He L et al (2017) Protective effect of tempol against hypoxia-induced oxidative stress and apoptosis in H9c2 cells. Med Sci Monit Basic Res 23:159
Li W, Li Y, Sun R et al (2017) Dual character of flavonoids in attenuating and aggravating ischemia-reperfusion-induced myocardial injury. Exp Ther Med 14(2):1307–1314
Liu J, Yang S, Zhang X et al (2016) Isoflurane reduces oxygen-glucose deprivation-induced oxidative, inflammatory, and apoptotic responses in H9c2 cardiomyocytes. Am J Transl Res 8(6):2597
Abdullah CS, Alam S, Aishwarya R et al (2018) Cardiac dysfunction in the sigma 1 receptor knockout mouse associated with impaired mitochondrial dynamics and bioenergetics. J Am Heart Assoc 7(20):e009775
Rousseaux CG, Greene SF (2016) Sigma receptors [σ Rs]: biology in normal and diseased states. J Recept Signal Transduct 36(4):327–388
Novakova M, Bruderova V, Sulova Z et al (2007) Modulation of expression of the sigma receptors in the heart of rat and mouse in normal and pathological conditions. Gen Physiol Biophys 26(2):110–117
Novakova M, Sedlakova B, Sirova M et al (2010) Haloperidol increases expression of the inositol 1, 4, 5-trisphosphate receptors in rat cardiac atria, but not in ventricles. Gen Physiol Biophys 29(4):381
Kamei J, Iwamoto Y, Misawa M et al (1993) Effects of rimcazole, a specific antagonist of σ sites, on the antitussive effects of non-narcotic antitussive drugs. Eur J Pharmacol 242(2):209–211
Vahabzadeh G, Rahbar-Roshandel N, Ebrahimi S-A (2020) Noscapine modulates neuronal response to oxygen-glucose deprivation/reperfusion injury via activation of sigma-1 receptor in primary cortical cultures. IJPR 19(1):331–342. https://doi.org/10.22037/ijpr.2019.112317.13683
Schulz R, Kelm M, Heusch G (2004) Nitric oxide in myocardial ischemia/reperfusion injury. Cardiovasc Res 61(3):402–413
Forstermann U, Sessa WC (2012) Nitric oxide synthases: regulation and function. Eur Heart J 33(7):829–837
Andrew PJ, Mayer B (1999) Enzymatic function of nitric oxide synthases. Cardiovasc Res 43(3):521–531
Taimor G, Hofstaetter B, Piper HM (2000) Apoptosis induction by nitric oxide in adult cardiomyocytes via cGMP-signaling and its impairment after simulated ischemia. Cardiovasc Res 45(3):588–594
Pacher P, Beckman SJ, Liaudet L (2007) Peroxynitrite in Health and Disease, ed. Physiol Rev 87(1):315–424
Wang P, Chen H, Qin H et al (1996) Measurement of nitric oxide and peroxynitrite generation in the postischemic heart. Evidence for peroxynitrite-mediated reperfusion injury. J Biol Chem 271(46):29223–29230
Vagnerova K, Hurn PD, Bhardwaj A et al (2006) Sigma 1 receptor agonists act as neuroprotective drugs through inhibition of inducible nitric oxide synthase. Anesth Analg 103(2):430–434
Bhardwaj A, Sawada M, London ED et al (1998) Potent ~ 1-receptor ligand 4-phenyl-1-(4-phenylbutyl) piperidine modulates basal and N-methyl-D-aspartate-evoked nitric oxide production in vivo. Stroke 29:2404–2410
Zughaier S, Karna P, Stephens D et al (2010) Potent anti-inflammatory activity of novel microtubule-modulating brominated noscapine analogs. PLoS ONE 5(2):e9165
Hofstaetter B, Taimor G, Inserte J et al (2002) Inhibition of apoptotic responses after ischemic stress in isolated hearts and cardiomyocytes. Basic Res Cardiol 97(6):479–488
Ekhterae D, Lin Z, Lundberg MS et al (1999) ARC inhibits cytochrome c release from mitochondria and protects against hypoxia-induced apoptosis in heart-derived H9c2 cells. Circ Res 85(12):e70–e77
Wu W-Y, Wang W-Y, Ma Y-L et al (2013) Sodium tanshinone IIA silate inhibits oxygen-glucose deprivation/recovery-induced cardiomyocyte apoptosis via suppression of the NF-κB/TNF-α pathway. Br J Pharmacol 169(5):1058–1071
Yang C, Li B, Liu Y et al (2019) Ginsenoside Rb1 protects cardiomyocytes from oxygen-glucose deprivation injuries by targeting microRNA-21. Exp Ther Med 17(5):3709–3716
Wang L, Zhang Y, Wan H et al (2017) Glycyrrhetinic acid protects H9c2 cells from oxygen glucose deprivation-induced injury through the PI3K/AKt signaling pathway. J Nat Med 71(1):27–35
Yang S, Bhardwaj A, Cheng J et al (2007) Sigma receptor agonists provide neuroprotection in vitro by preserving bcl-2. Anesth Analg 104(5):1179
Acknowledgement
The authors thank Dr. Mansour Torab for skillful technical assistance.
Funding
This work was supported by Iran University of Medical Sciences (IR.IUMS.REC1393.25042).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declared that they have no conflict of interest. No human or animal was used in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vahabzadeh, G., Soltani, H., Barati, M. et al. Noscapine protects the H9c2 cardiomyocytes of rats against oxygen–glucose deprivation/reperfusion injury. Mol Biol Rep 47, 5711–5719 (2020). https://doi.org/10.1007/s11033-020-05549-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-020-05549-6