Abstract
Angiogenesis is a new vessel formation process that plays a role in various physiological and pathological conditions. This process is controlled by the balance between pro-angiogenic and anti-angiogenic mediators in the organism. Angiogenesis is needed for the growth and metastasis of solid tumors. Therefore, the anti-angiogenic treatment approach is seen as an interesting option in cancers. Fenretinide, a synthetic retinoic acid analog, is an effective agent on angiogenesis. In this study, we aimed to investigate the effects of the fenretinide on some miRNAs involving in angiogenesis process and on the expression of CDH5, FOXM1 and eNOS genes upregulated in angiogenesis. In addition, it was shown the effects of this agent on cell proliferation, cell migration and capillary-like tube formation. In our study, the data were analyzed using Kruskal–Wallis and Dunn’s test. Fenretinide applied to the cells for 24 and 48 h periods reduced cell proliferation (P < 0.001) and cell migration, and suppressed tube formation (P < 0.001) as a dose dependent manner. Endothelial cells were cultured in growth-inducing media containing a variety of growth factors such as VEGF, FGF, IGF and EGF. As a result of simultaneous PCR analysis, we found that angiogenesis-promoting miR-10b was effectively suppressed (P < 0.001) and interestingly angiogenesis-modulating miR-126 was slightly increased (P < 0.05), but other miRNAs, including miR-31, miR-21, miR-101, miR-340, miR-29c, miR-206 and miR-146a were not affected. Besides, a significant decrease was observed in the levels of some angiogenesis-inducing genes, CDH5 (P < 0.001), FOXM1 (P < 0.001) and eNOS (P < 0.01 and P < 0.001) in endothelial cells treated with fenretinide. Our results have shown that fenretinide exhibited anti-angiogenic activity through the down-regulation of CDH5, FOXM1 and eNOS genes, and suppression of miR-10b.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The formation of new blood vessels, termed angiogenesis, is thought to be an essential step in the growth of solid tumors and metastasis. Tumor angiogenesis is largely associated with poor prognosis. Since oxygen and nutrient requirements increase in growing tumor, cancer cells need to induce angiogenesis. In addition to cancer, angiogenesis process also plays a serious role in a variety of human pathologies including diabetic retinopathy, psoriasis, rheumatoid arthritis etc.[1, 2]. Consecutive angiogenesis process involves complex interaction between the cells, extracellular matrix components and soluble factors such as vascular endothelial growth factors (VEGF). These sequential steps in angiogenesis consist of the degradation of basement membrane, cell migration, sprouting, cell proliferation, lumen formation, the construction of new basement membrane by pericyte cells, generation of anastomoses and eventually blood flow [3]. This tightly regulated angiogenesis process is controlled by some genes among of which the most important ones are VEGF and fibroblast growth factor (FGF). Additionally, some genes, e.g., oncogenic transcription factor forkhead box M1 (FOXM1), endothelial nitric oxide synthase (eNOS) and cadherin 5 (VE-cadherin, CDH5) are also involved in this process. When upregulated, FOXM1, eNOS and CDH5 genes promote angiogenesis, i.e., they are pro-angiogenic genes [4,5,6]. The development and application of angiogenesis inhibitors against to factors in these steps has been known to be a useful approach to prevent the growing of tumor and to improve the prognosis.
Fenretinide (N-4-hydroxyphenyl retinamide; 4-HPR) is a synthetically produced analogue of retinoic acid. As it is well known retinoic acid isomers are ligands for retinoic acid receptors and retinoid X receptors (RAR/RXR) and play essential roles in cell differantiation and development. RAR and RXR receptors are the members of nuclear hormone receptor family that are ligand-dependent DNA-binding transcription factors [7, 8]. In some studies, it was demonstrated that fenretinide exhibited anti-proliferative properties and may be an anti-angiogenic agent [9,10,11]. Sogno et al. [9] reported that fenretinide could decrease the tumor growth via suppressing angiogenesis process. In few previous studies, this retinoic acid analogue was shown to repress capillary-like tube formation, migration and proliferation of endothelial cells [12, 13]. Fenretinide has been used as chemopreventive agent against prostate cancer and against the development risk of contralateral breast cancer at the present time. This agent can bind to RAR and activates it, thus it can induce apoptosis and cell differentiation in some cell types [14].
Only about 2% of the human genome has been known to encode protein. With respect to the rest of the genome, some regions serve as epigenetic regulators. MicroRNAs (miRNAs) which are transcribed but not translated to protein are a class of small functional non-coding RNA molecules. Single stranded miRNAs, approximately 18–24 nucleotides in length, post-transcriptionally regulate the target mRNA mostly via binding to 3′-UTR or 5′-UTR, thus it inhibits the translation of targeted mRNA or causes its destruction [15]. In summary, miRNAs are involved in many molecular biological processes such as differentiation, proliferation and metabolism of cells. Moreover, some miRNAs have been found to exhibit pro-angiogenic and anti-angiogenic properties. In a previous study, miR-9 was demonstrated to be a pro-angiogenic molecule in endothelial cells [16]. Besides, many angiogenesis-related miRNAs such as miR-206, miR-126, miR-29c, let-7a and miR-340 have been shown in a variety of study [17,18,19,20,21].
Although there are very few studies in the literature examining the relationship between fenretinide and miRNA in cancer cells [22, 23], we have not found any study investigating the effects of fenretinide on miRNA in angiogenesis process. In this study, we aimed to clarify the effects of fenretinide on eNOS, FOXM1 ve CDH5 genes and miRNAs that are involved in angiogenesis.
Materials and methods
Reagents
Some primary materials used in this study are as follows: Human Umbilical Vein Endothelial Cells (HUVEC) (Lonza C2519A), EGM-2 Endothelial Cell Growth Medium-2 BulletKit (Lonza CC-3162), Matrigel Matrix (Corning 354234), Fenretinide (Sigma-H7779), MTT (3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide) (Sigma M5655). Fenretinide (5 mg) was dissolved in 1000 μl of DMSO as stock solution.
Cell culture
HUVECs were grown in EGM-2 medium which consists of EBM-2 basal medium plus growth supplements (VEGF, rhFGF, insulin-like growth factor (IGF), epidermal growth factor (EGF), ascorbic acid, hydrocortisone, heparin, gentamicin sulfate and 2% FBS). Cells were cultured in a humidified atmosphere and 5% CO2 at 37 °C. HUVECs at passage 3–6 were used for angigenesis assay and other experimental procedures. Fenretinide applied to the cells at a final concentration of 1 μM, 5 μM and 10 μM for 24 h and 48 h. Cells in control group was treated with DMSO (0.1%, v/v).
Cell proliferation assay
After treatment with fenretinide for 24 h and 48 h, viability of the cells was assayed using MTT methods. MTT stock solution was prepared in PBS at a concentration of 5 mg/ml, and then it was diluted by 10 times to make working solution. HUVECs were plated at a density of 5 × 104 cells per well in 24-well plate. After reached to about 70% confluence, the cells were incubated overnight with EBM-2 basal medium plus 2% FBS except for growth supplements. At the end of the incubation period, the serum starved medium was exchanged with EGM-2 medium and then, fenretinide at a concentration of 1 μM, 5 μM and 10 μM was applied to the cells for 24 h and 48 h. The medium was removed and cells were treated with 500 μl of the MTT working solution at 37 °C for 3 h. The converted dye formed by living cells from MTT was solubilized with 500 μl of acidic isopropanol solution (0.04 M HCl in absolute isopropanol) and its absorbance was measured at 570 nm using colorimetric plate reader (Thermo Scientific Multikan GO, USA). Experiments were repeated three times.
In vitro angiogenesis assay
Matrigel matrix, which is generated from Engelbreth-Holm-Swarm (EHS) mouse sarcoma, includes many growth factors, e.g., TGF-beta, EGF, IGF and FGF. After thawed at 4 °C overnight, matrigel matrix (300 μl) was immediately added to each well and incubated at 37 °C for 1 h to solidify in 24-well plate. After HUVECs were serum starved overnight, they were added into the wells at a density of 4 × 104 cells per well. Fenretinide at specified concentrations were treated with cells after the cells had adhered to the matrix. Capillary-like tubular structures formed by HUVECs were visualized and photographed using photomicroscope (Leica DFC450, USA) under 4 × objective. The lengths (pixel) of tubular structure were calculated as the average of three different areas using ImageJ software program. Experiments were repeated three times.
Cell migration assay
For endothelial cell migration, we used the technique named wound healing assay measuring the movement of endothelial cells towards each other. In this assay, full-confluent cells were scratched across the diameter of 6-well petri using a pipette tip after serum starvation overnight. Afterward, fenretinide at the indicated concentrations were applied to the cells. HUVECs were photographed under × 4 magnification after approximately 10–12 h using an inverted microscope (Leica DFC450, USA). Experiments were repeated three times.
Relative gene expression levels by quantitative real-time polymerase chain reaction (qRT-PCR)
After cells which reached to about 70% confluence in 6-well plate were serum starved overnight, fenretinide at a concentration of 1 μM, 5 μM and 10 μM were applied. After 24 h and 48 h, RNA content was immediately purified using Qiagen miRNeasy mini kit (Qiagen 217004) according to the manufacturer’s instructions. RNA concentrations and quality were calculated using a nanodrop spectrophotometer (Thermo Fisher ND-1000, USA). The obtained RNAs were adjusted to 5 ng/μl in RNase-free water as described in kit protocol (Thermo Fisher A28007). After that, 2 μl of RNA sample were reverse transcribed with TaqMan Advanced miRNA Assays cDNA Synthesis Kit (Thermo Fisher A28007) according to the manufacturer’s instructions using a thermal cycler (Veriti Thermo Fisher, USA).
To evaluate the relative expression of angiogenesis-related miRNAs, quantitative real time PCR analysis was performed using miScript SYBR Green PCR Kit (Qiagen 218073) and qRT-PCR Rotor-Gene Q equipment (Qiagen, USA). These miRNA primer assays are as follows: Hs_miR-126 (MS00003430), Hs_miR-21 (MS00009079), Hs_miR-340 (MS00031759), Hs_miR-31 (MS00003290), Hs_miR-10b (MS00031269), Hs_miR-101 (MS00008372), Hs_miR-29c (MS00003269), Hs_miR-206 (MS00003787), Hs_miR-146a (MS00003535). Hs_RNU6 (MS00033740) was used for normalization of RT-PCR results in miRNA quantification. The steps for real-time PCR is as follows: initial denaturing step at 95 °C for 10 min; PCR cycle (total 40 cycles) at 94 °C for 15 s, at 55 °C for 30 s, at 70 °C for 30 s, and single read at the end of the each cycle. In addition, melting curves were generated using the program that is as follows: denaturation at 95 °C for 30 s, cooling at 50 °C for 60 s and then the temperature was increased from 50 to 95 °C. Temperature rise was 0.2 °C at each step and fluorescence signals were continuously collected.
The expression levels of FOXM1, eNOS, CDH5 and Beta-actin (as a reference gene) genes were measured using SYBR Green I Master PCR Kit (Roche Applied Science, Germany). Amplification curves were generated with heat activation at 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s, at 57 °C for 30 s and at 72 °C for 30 s. In addition we added a melting curve analysis that is as follows: PCR products were denatured at 95 °C for 30 s, cooled at 55 °C for 60 s. The temperature was increased from 55 to 95 °C (0.2 °C at each step) and fluorescence signals were continuously collected.
Primers for these genes are as follows: eNOS: Forward: 5′-GAAGGCGACAATCCTGTATGGC-3′; Reverse: 5′-TGTTCGAGGGACACCACGTCAT-3′. FOXM1: Forward: 5′-TCTGCCAATGGCAAGGTCTCCT-3′; Reverse: 5′-CTGGATTCGGTCGTTTCTGCTG-3′, CDH5: Forward: 5′-GAAGCCTCTGATTGGCACAGTG-3′; Reverse: 5′-TTTTGTGACTCGGAAGAACTGGC-3′, Beta-Actin: Forward: 5′-CATGTACGTTGCTATCCAGGC-3′; Reverse: 5′-CTCCTTAATGTCACGCACGAT-3′.
All experiments were performed three times. The results for the relative gene expression levels were calculated using the 2−ΔΔCt method.
Statistical analysis
For stasistical analyses, we used Prism Program of GraphPad Software (San Diego, CA). Mean and standart deviation (SD) of data were analysed by Column Statistics Test. Comparision of data obtained from the experimental groups was performed using non-parametric Kruskal–Wallis test, and Dunn’s test was also used for Post-Hoc analyses. Data were expressed as mean ± standard deviation (SD). P values less than 0.05 (P < 0.05) were statistically considered as significant.
Results
Fenretinide suppresses cell proliferation
In the present study, we observed that 1 µM, 5 µM and 10 µM concentrations of fenretinide significantly suppressed the endothelial cell proliferation in a dose-dependent manner in the 24 h subgroup compared to control (P < 0.001). We also observed that the suppression of proliferation of HUVECs was higher in the 48 h subgroup in a dose-dependent manner (P < 0.001) (Fig. 1). The differences among the fenretinide concentrations were significant (P < 0.01, P < 0.001).
Percentage of the proliferation of endothelial cells incubated for 24 h and 48 h. After cells were treated with MTT solution, converted dye was measured spectrophotometrically at 570 nm. Values were normalized to control group. Data represent means ± SD of three different assays. Significance values were expressed as ** and *** indicating P < 0.01 and P < 0.001, respectively
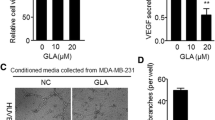
Fenretinide inhibits in vitro angiogenesis formed by endothelial cells
When analyzed the effect of the agent in all three concentrations on the capillary-like tube formation on matrigel matrix, we observed that 1 µM and 5 µM of fenretinide blocked tubular structures created by HUVECs as compared to control group (P < 0.001) (Fig. 2). Moreover, cells treated with fenretinide at a concentration of 10 µM produced almost no tubular structure. We calculated the lenght of tubular structure as pixel to obtain quantitative results and expressed the data on bar graphs (Fig. 2).
Microphotographs of the capillary-like tubular structures formed by HUVECs on matrigel matrix. Fenretinide at a concentration of 1 μM and 5 μM suppresses tube formation in 24-well plate. Bar graph represents the tube lengths as pixel. Data were expressed as means ± SD of three different experiments. *** indicates the intergroup significance and P < 0.001
Fenretinide decreases the cell migration
For migration experiments, we performed the wound healing assay and observed the capacity of cells to fulfill the gap. Fenretinide in all three concentrations decreased the migration in a dose dependent manner (Fig. 3).
Fenretinide downregulates angiogenesis-related genes, eNOS, FOXM1 and CDH5
The expression levels of the genes were determined by qRT-PCR. The relative expression values of eNOS, FOXM1 and CDH5 genes were normalized to the levels of beta-actin expression as a housekeeping gene. Normalized Ct data were compared to the data obtained from control group. Fenretinide at a concentration of 1 µM and 5 µM was found to significantly diminish the mRNA levels of eNOS (P < 0.01 and P < 0.001), FOXM1 (P < 0.001) and CDH5 (P < 0.001) genes in a dose-dependent manner. These downregulations in the levels of angiogenesis-related gene expression were observed in both 24 h and 48 h subgroups (P < 0.001) (Fig. 4).
Bar graphs showing the effects of fenretinide (1 µM and 5 µM) on the relative mRNA expression levels of eNOS, FOXM1 and CDH5 genes. Dark and light colored bars indicate the expression levels of HUVECs treated with fenretinide for 24 h and 48 h, respectively. Values were given as means ± SD of triplicate experiment per group and intergroup significance were **P < 0.01, ***P < 0.001
Results on angiogenesis-related miRNA profile
After cells had incubated overnight in serum starved conditions as in the other experiments, fenretinide at a concentration of 1 µM and 5 µM was applied for 24 h and 48 h. qRT-PCR assay was used for determining miRNA expression levels. We found that the levels of miR-10b, which is a pro-angiogenic miRNA, was significantly repressed (P < 0.001) by fenretinide (Fig. 5). However, we observed that the levels of miR-126, which has both anti-angiogenic and pro-angiogenic properties as depending on the types of cells or environment, was slightly increased at a 1 µM concentration of fenretinide for 24 h and 48 h (P < 0.05, P < 0.01) (Fig. 5). But it was observed that 5 µM of fenretinide increase its levels approximately twofold (P < 0.001) (Fig. 5). In addition, we didn’t get any significant results from the other miRNAs, including miR-31, miR-21, miR-101, miR-340, miR-29c, miR-206 and miR-146a.
The relative expression levels of miR-10b and miR-126. Dark and light colored bars indicate the expression levels of HUVECs treated with fenretinide for 24 h and 48 h, respectively. Values were given as means ± SD of triplicate experiment per group and intergroup significance were *P < 0.05, **P < 0.01, ***P < 0.001
Discussion
Angiogenesis, which is the process of formation of new vessels from pre-existing ones, has a tightly controlled mechanism under normal conditions. However, in some pathological processes, this control is disabled and an uncontrolled vascularization occurs. Researches on the suppression of angiogenesis in some pathological conditions such as cancer and retinopathy have been ongoing. When the tumor mass exceeds 0.5 mm, it generally needs extra vascularization, and therefore abnormal angiogenesis has been seen to begin in the tumor region [24, 25].
Several studies have shown that fenretinide repressed the migration, proliferation, and capillary-like tube formation of endothelial cells [4, 26, 27]. In this study, we also examined the effects of fenretinide on endothelial cell proliferation, migration and capillary-like tube formation. When we measured the cell proliferation, we found that fenretinide significantly suppressed the endothelial cell proliferation compared to the control group in a dose- and time-dependent manner (P < 0.01 and P < 0.001) (Fig. 1). We also examined the effect of fenretinide treatment on the ability of cells to form capillaries on the matrigel matrix. Similarly, fenretinide dramatically suppressed the capillary-like tube formation in a dose dependent manner as compared to control group (P < 0.001) (Fig. 2). For tube formation assays, the quantitative results were given as pixel length (Fig. 2). With respect to the capacity of cells to fill the gaps opened in the wound healing migration experiment, we observed that fenretinide decreased the migration of endothelial cells in a dose-dependent manner (Fig. 3). Our results obtained from all the in vitro angiogenesis assays of endothelial cells are in accordance with the literature [4, 26, 27].
It was shown that the genes we selected in our study, which are eNOS, FOXM1 and CDH5 genes, had affected the pathways related with angiogenesis [4,5,6]. An increase in the expression of eNOS gene was reported to induce angiogenesis [6]. The eNOS gene catalyzes the production of nitric oxide (NO), a short-term signaling molecule involved in angiogenesis. Some factors suc as the formation of veins, endothelial cell morphology, cell–cell contact and some others which create fluid leakage stress in the veins can stimulate NO release and eNOS expression [6]. In other words, eNOS is stimulated by many external factors in the angiogenesis process. In this study, HUVECs treated with 1 µM of fenretinide for 24 h showed a 35% decrease in the expression of eNOS gene (P < 0.01), and also a 20% decrease (P < 0.01) in the treatment with 5 µM of fenretinide as compared to the control group (Fig. 4). Fenretinide treatment at both concentrations for 48 h exhibited about 70% and 75% suppression in the eNOS expression, respectively (P < 0.001) (Fig. 4).
FOXM1 gene is also one of the angiogenesis-inducing genes [5]. In our study, FOXM1 expression in the cells treated with fenretinide at a concentration of 1 µM and 5 µM for 24 h showed a decrease about 35% and 75%, respectively, compared to the control group (P < 0.001) (Fig. 4). In the experimental group treated with fenretinide for 48 h, the expression levels of FOXM1 gene were almost completely suppressed as compared to the control group (P < 0.001) (Fig. 4). Our study is a promising preliminary study to investigate the molecular effect of fenretinide on the FOXM1 gene which appears to be a target for anti-cancer drugs.
As regards CDH5 gene, we found that 1 µM and 5 µM of fenretinide suppressed the expression about 35% and 95% for 24 h (P < 0.001), and 85% and 99% for 48 h (P < 0.001), respectively (Fig. 4). The expression of CDH5 gene which promotes angiogenesis [4] can be induced under hypoxic conditions [28]. Since fenretinide can reduce the expression of the HIF gene under hypoxic conditions [29], it may have reduced the expression of the CDH5 as well. According to the data we obtained, fenretinide significantly suppressed the expression of these pro-angiogenic genes, suggesting promising results against angiogenesis.
In the present study, we also studied some angiogenesis-related miRNA. Fenretinide was applied to the cells at a concentration of 1 µM and 5 µM and sub-experimental groups were formed as the 24 h and 48 h group. However, we didn’t get significant results for miRNA expression other than miR-10b and miR-126 in these groups. miR-10b was demonstrated to be a pro-angiogenic miRNA in breast cancer [30]. It was reported that the increased miR-10b levels were associated with a variety of various outcomes, including increased metastasis and invasive potential in vitro and in vivo [31]. Besides, an increase in miR-10b expression results in increased angiogenesis, cell proliferation and migration. Because of these results, miR-10b is related to bad prognosis, including short relapse-free survival and increased tumor size [31]. Consistent with these results, MiR-10b was documented to be upregulated in endothelial progenitor cells derived from the bone marrow and the tumor–stroma in human xenograft tumor mouse models and syngeneic models [32].
With respect to miR-126, we can say that miR-126 is absolutely related to tumorigenic process and exhibits different expression profiles depending on tumor cell type and micro-environmental conditions. It is important that miR-126 is strictly, specifically and highly expressed in human endothelial cells [33, 34]. Solingen et al. [34] showed that silencing of miR-126 impaired ischemia-induced angiogenesis in mice treated with high dose of antagomir-126 [34]. MiR-126 mediates developmental angiogenesis in vivo and its targeted deletion impairs vascular integrity and causes leaky vessels and partial embryonic lethality in mice [35]. In addition, knockdown of miR-126 in zebrafish was demonstrated to result in loss of vascular integrity during embryonic development [36].
As far as is known, one of the mechanisms of action of miR-126 is the targeting of both phosphoinositol-3 kinase regulatory subunit-2 (PIK3R2) and the Sprouty-related protein, (Spred1), which are repressors of VEGF signaling pathway [35, 36]. As opposed to this angiogenesis mechanism, it was suggested that another targeting of miR-126 is VEGFA which is an angiogenesis and vasculogenesis-promoting growth factor [33]. As autocrine VEGF signaling is also required for vascular homeostasis in endothelial cells [37], future studies are needed to clarify the exact roles of miR-126 expression affecting the mechanisms of angiogenesis.
In spite of these studies, miR-126 was reported to be an anti-angiogenic miRNA in liver cancer [38] and to be down-regulated in a variety of tumors such as gastric cancer [39, 40], colorectal cancer [41, 42], breast cancer [33, 43], prostate cancer [44] and lung cancers [45, 46], but to be up-regulated in the acute myeloid leukemia [47, 48].
Zhu et al. [33] showed that miR-126 was down-regulated and the VEGF/PI3K/AKT signaling pathway was activated in breast cancer. They also showed that transfection of miR-126 mimics into MCF-7 cells decreased VEGF/PI3K/AKT signaling [33]. Similarly, down-regulation of miR-126 expression was found to facilitate angiogenesis and to increase microvessel density (MVD) of gastric cancer [39] and lung cancer tissue [45, 46]. Besides, restoration of miR-126 dramatically reduced MVD and the levels of VEGF, resulting in the inhibition of the growth of lung cancer [45, 46].
Another remarkable matter is that miR-126 is located in the 7th intron of epidermal growth factor-like-domain 7 gene (EGFL7). Sun et al. [49] showed that miR-126 can suppress the proliferation non-small cell lung cancer cells via one of its potential targets, EGFL7 which is involved in cell migration and blood vessel formation [49]. Additionally, in ECV-304 human umbilical vein endothelial cells, miR-126 was shown to down-regulate EGFL7 expression [50].
In our study, we found that miR-10b levels were dramatically suppressed at both doses of fenretinide (P < 0.001). 1 μM of fenretinide in 24 h and 48 h group and 5 μM of fenretinide in 24 h group slightly increased the levels of miR-126 (P < 0.05 and P < 0.01, respectively), but 5 μM of fenretinide in 48 h group increased miR-126 expression approximately twofold (P < 0.001) (Fig. 5). In some studies, all-trans retinoic acid (ATRA) were used and the expression of miR-126 was observed to be upregulated in neuroblastoma cells [51,52,53]. Considering all these publications, we can say that the role of miR-126 in angiogenesis process and cancer is controversial. In our study, the increase in endothelial miR-126 expression may be arised from the treatment of cells with fenretinide, as ATRA does. In addition, antiangiogenic effects of fenretinide are related at least with its suppressive effects on the expression of miR-10b, eNOS, FOXM1, CDH5 genes. Thus, possible anti-angiogenic effects of fenretinide are dominant in endothelial cells. However, further studies that can show the effects of retinoids on angiogenesis process are needed to clarify this pathway.
While the therapeutic effects of fenretinide have been shown in some diseases such as cancer and diabetes, it is not known exactly which molecular mechanisms it affects [54]. If the molecular mechanism of fenretinide is well understood, bioavailability may be increased in pharmacological studies, and consequently this may provide an opportunity to establish a new line of treatment for many pathological issues such as cancer, obesity, diabetes and some ocular disorders.
As a result, our results have shown that fenretinide exhibited anti-angiogenic activity through the suppression of miR-10b and the down-regulation of some angiogenesis-related genes such as eNOS, FOXM1, CDH5, and thus fenretinide effectively suppressed the capillary-like tube formation and cell migration of endothelial cells.
References
Sahin M, Sahin E, Gumuslu S (2009) Cyclooxygenase-2 in cancer and angiogenesis. Angiology 60(2):242–253. https://doi.org/10.1177/0003319708318378
Sahin M, Sahin E, Gumuslu S, Erdogan A, Gultekin M (2010) DNA methylation or histone modification status in metastasis and angiogenesis-related genes: a new hypothesis on usage of DNMT inhibitors and S-adenosylmethionine for genome stability. Cancer Metastasis Rev 29(4):655–676. https://doi.org/10.1007/s10555-010-9253-0
Bussolino F, Mantovani A, Persico G (1997) Molecular mechanisms of blood vessel formation. Trends Biochem Sci 22(7):251–256
Du J, Yang Q, Luo L, Yang D (2017) C1qr and C1qrl redundantly regulate angiogenesis in zebrafish through controlling endothelial Cdh5. Biochem Biophys Res Commun 483(1):482–487. https://doi.org/10.1016/j.bbrc.2016.12.118
Gartel AL (2010) A new target for proteasome inhibitors: FoxM1. Expert Opin Investig Drugs 19(2):235–242. https://doi.org/10.1517/13543780903563364
Park S, Sorenson CM, Sheibani N (2015) PECAM-1 isoforms, eNOS and endoglin axis in regulation of angiogenesis. Clin Sci (Lond) 129(3):217–234. https://doi.org/10.1042/CS20140714
Al Tanoury Z, Piskunov A, Rochette-Egly C (2013) Vitamin A and retinoid signaling: genomic and nongenomic effects. J Lipid Res 54(7):1761–1775. https://doi.org/10.1194/jlr.R030833
Huang P, Chandra V, Rastinejad F (2014) Retinoic acid actions through mammalian nuclear receptors. Chem Rev 114(1):233–254. https://doi.org/10.1021/cr400161b
Sogno I, Vene R, Ferrari N, De Censi A, Imperatori A, Noonan DM, Tosetti F, Albini A (2010) Angioprevention with fenretinide: targeting angiogenesis in prevention and therapeutic strategies. Crit Rev Oncol Hematol 75(1):2–14. https://doi.org/10.1016/j.critrevonc.2009.10.007
Anding AL, Jones JD, Newton MA, Curley RW Jr, Clagett-Dame M (2018) 4-HPR Is an endoplasmic reticulum stress aggravator and sensitizes breast cancer cells resistant to TRAIL/Apo2L. Anticancer Res 38(8):4403–4416. https://doi.org/10.21873/anticanres.12742
Anding AL, Chapman JS, Barnett DW, Curley RW Jr, Clagett-Dame M (2007) The unhydrolyzable fenretinide analogue 4-hydroxybenzylretinone induces the proapoptotic genes GADD153 (CHOP) and Bcl-2-binding component 3 (PUMA) and apoptosis that is caspase-dependent and independent of the retinoic acid receptor. Cancer Res 67(13):6270–6277. https://doi.org/10.1158/0008-5472.CAN-07-0727
Ferrari N, Morini M, Pfeffer U, Minghelli S, Noonan DM, Albini A (2003) Inhibition of Kaposi's sarcoma in vivo by fenretinide. Clin Cancer Res 9(16 Pt 1):6020–6029
Ferrari N, Pfeffer U, Dell'Eva R, Ambrosini C, Noonan DM, Albini A (2005) The transforming growth factor-beta family members bone morphogenetic protein-2 and macrophage inhibitory cytokine-1 as mediators of the antiangiogenic activity of N-(4-hydroxyphenyl)retinamide. Clin Cancer Res 11(12):4610–4619. https://doi.org/10.1158/1078-0432.CCR-04-2210
Samuel W, Kutty RK, Nagineni S, Vijayasarathy C, Chandraratna RA, Wiggert B (2006) N-(4-hydroxyphenyl)retinamide induces apoptosis in human retinal pigment epithelial cells: retinoic acid receptors regulate apoptosis, reactive oxygen species generation, and the expression of heme oxygenase-1 and Gadd153. J Cell Physiol 209(3):854–865. https://doi.org/10.1002/jcp.20774
O'Brien J, Hayder H, Zayed Y, Peng C (2018) Overview of MicroRNA biogenesis, mechanisms of actions, and circulation. Front Endocrinol (Lausanne) 9:402. https://doi.org/10.3389/fendo.2018.00402
Zhuang G, Wu X, Jiang Z, Kasman I, Yao J, Guan Y, Oeh J, Modrusan Z, Bais C, Sampath D, Ferrara N (2012) Tumour-secreted miR-9 promotes endothelial cell migration and angiogenesis by activating the JAK-STAT pathway. EMBO J 31(17):3513–3523. https://doi.org/10.1038/emboj.2012.183
Hu J, Zeng L, Huang J, Wang G, Lu H (2015) miR-126 promotes angiogenesis and attenuates inflammation after contusion spinal cord injury in rats. Brain Res 1608:191–202. https://doi.org/10.1016/j.brainres.2015.02.036
Xu Z, Zhu C, Chen C, Zong Y, Feng H, Liu D, Feng W, Zhao J, Lu A (2018) CCL19 suppresses angiogenesis through promoting miR-206 and inhibiting Met/ERK/Elk-1/HIF-1alpha/VEGF-A pathway in colorectal cancer. Cell Death Dis 9(10):974. https://doi.org/10.1038/s41419-018-1010-2
Liu L, Bi N, Wu L, Ding X, Men Y, Zhou W, Li L, Zhang W, Shi S, Song Y, Wang L (2017) MicroRNA-29c functions as a tumor suppressor by targeting VEGFA in lung adenocarcinoma. Mol Cancer 16(1):50. https://doi.org/10.1186/s12943-017-0620-0
Isanejad A, Alizadeh AM, Amani Shalamzari S, Khodayari H, Khodayari S, Khori V, Khojastehnjad N (2016) MicroRNA-206, let-7a and microRNA-21 pathways involved in the anti-angiogenesis effects of the interval exercise training and hormone therapy in breast cancer. Life Sci 151:30–40. https://doi.org/10.1016/j.lfs.2016.02.090
Umezu T, Imanishi S, Azuma K, Kobayashi C, Yoshizawa S, Ohyashiki K, Ohyashiki JH (2017) Replenishing exosomes from older bone marrow stromal cells with miR-340 inhibits myeloma-related angiogenesis. Blood Adv 1(13):812–823. https://doi.org/10.1182/bloodadvances.2016003251
Chakrabarti M, Khandkar M, Banik NL, Ray SK (2012) Alterations in expression of specific microRNAs by combination of 4-HPR and EGCG inhibited growth of human malignant neuroblastoma cells. Brain Res 1454:1–13. https://doi.org/10.1016/j.brainres.2012.03.017
Herrero Martin D, Boro A, Schafer BW (2013) Cell-based small-molecule compound screen identifies fenretinide as potential therapeutic for translocation-positive rhabdomyosarcoma. PLoS ONE 8(1):e55072. https://doi.org/10.1371/journal.pone.0055072
Folkman J, Shing Y (1992) Angiogenesis. J Biol Chem 267(16):10931–10934
Otrock ZK, Makarem JA, Shamseddine AI (2007) Vascular endothelial growth factor family of ligands and receptors: review. Blood Cells Mol Dis 38(3):258–268. https://doi.org/10.1016/j.bcmd.2006.12.003
Golubkov V, Garcia A, Markland FS (2005) Action of fenretinide (4-HPR) on ovarian cancer and endothelial cells. Anticancer Res 25(1A):249–253
Bassani B, Bartolini D, Pagani A, Principi E, Zollo M, Noonan DM, Albini A, Bruno A (2016) Fenretinide (4-HPR) targets caspase-9, ERK 1/2 and the Wnt3a/beta-catenin pathway in medulloblastoma cells and medulloblastoma cell spheroids. PLoS ONE 11(7):e0154111. https://doi.org/10.1371/journal.pone.0154111
Tang NN, Zhu H, Zhang HJ, Zhang WF, Jin HL, Wang L, Wang P, He GJ, Hao B, Shi RH (2014) HIF-1alpha induces VE-cadherin expression and modulates vasculogenic mimicry in esophageal carcinoma cells. World J Gastroenterol 20(47):17894–17904. https://doi.org/10.3748/wjg.v20.i47.17894
Yasuo M, Mizuno S, Allegood J, Kraskauskas D, Bogaard HJ, Spiegel S, Voelkel NF (2013) Fenretinide causes emphysema, which is prevented by sphingosine 1-phoshate. PLoS ONE 8(1):e53927. https://doi.org/10.1371/journal.pone.0053927
Liu X, Guan Y, Wang L, Niu Y (2017) MicroRNA-10b expression in node-negative breast cancer-correlation with metastasis and angiogenesis. Oncol Lett 14(5):5845–5852. https://doi.org/10.3892/ol.2017.6914
Sheedy P, Medarova Z (2018) The fundamental role of miR-10b in metastatic cancer. Am J Cancer Res 8(9):1674–1688
Plummer PN, Freeman R, Taft RJ, Vider J, Sax M, Umer BA, Gao D, Johns C, Mattick JS, Wilton SD, Ferro V, McMillan NA, Swarbrick A, Mittal V, Mellick AS (2013) MicroRNAs regulate tumor angiogenesis modulated by endothelial progenitor cells. Cancer Res 73(1):341–352. https://doi.org/10.1158/0008-5472.CAN-12-0271
Zhu N, Zhang D, Xie H, Zhou Z, Chen H, Hu T, Bai Y, Shen Y, Yuan W, Jing Q, Qin Y (2011) Endothelial-specific intron-derived miR-126 is down-regulated in human breast cancer and targets both VEGFA and PIK3R2. Mol Cell Biochem 351(1–2):157–164. https://doi.org/10.1007/s11010-011-0723-7
van Solingen C, Seghers L, Bijkerk R, Duijs JM, Roeten MK, van Oeveren-Rietdijk AM, Baelde HJ, Monge M, Vos JB, de Boer HC, Quax PH, Rabelink TJ, van Zonneveld AJ (2009) Antagomir-mediated silencing of endothelial cell specific microRNA-126 impairs ischemia-induced angiogenesis. J Cell Mol Med 13(8A):1577–1585. https://doi.org/10.1111/j.1582-4934.2008.00613.x
Wang S, Aurora AB, Johnson BA, Qi X, McAnally J, Hill JA, Richardson JA, Bassel-Duby R, Olson EN (2008) The endothelial-specific microRNA miR-126 governs vascular integrity and angiogenesis. Dev Cell 15(2):261–271. https://doi.org/10.1016/j.devcel.2008.07.002
Fish JE, Santoro MM, Morton SU, Yu S, Yeh RF, Wythe JD, Ivey KN, Bruneau BG, Stainier DY, Srivastava D (2008) miR-126 regulates angiogenic signaling and vascular integrity. Dev Cell 15(2):272–284. https://doi.org/10.1016/j.devcel.2008.07.008
Lee S, Chen TT, Barber CL, Jordan MC, Murdock J, Desai S, Ferrara N, Nagy A, Roos KP, Iruela-Arispe ML (2007) Autocrine VEGF signaling is required for vascular homeostasis. Cell 130(4):691–703. https://doi.org/10.1016/j.cell.2007.06.054
Jing BQ, Ou Y, Zhao L, Xie Q, Zhang YX (2017) Experimental study on the prevention of liver cancer angiogenesis via miR-126. Eur Rev Med Pharmacol Sci 21(22):5096–5100. https://doi.org/10.26355/eurrev_201711_13825
Chen H, Li L, Wang S, Lei Y, Ge Q, Lv N, Zhou X, Chen C (2014) Reduced miR-126 expression facilitates angiogenesis of gastric cancer through its regulation on VEGF-A. Oncotarget 5(23):11873–11885. https://doi.org/10.18632/oncotarget.2662
Feng R, Chen X, Yu Y, Su L, Yu B, Li J, Cai Q, Yan M, Liu B, Zhu Z (2010) miR-126 functions as a tumour suppressor in human gastric cancer. Cancer Lett 298(1):50–63. https://doi.org/10.1016/j.canlet.2010.06.004
Li XM, Wang AM, Zhang J, Yi H (2011) Down-regulation of miR-126 expression in colorectal cancer and its clinical significance. Med Oncol 28(4):1054–1057. https://doi.org/10.1007/s12032-010-9637-6
Liu Y, Zhou Y, Feng X, An P, Quan X, Wang H, Ye S, Yu C, He Y, Luo H (2014) MicroRNA-126 functions as a tumor suppressor in colorectal cancer cells by targeting CXCR4 via the AKT and ERK1/2 signaling pathways. Int J Oncol 44(1):203–210. https://doi.org/10.3892/ijo.2013.2168
Zhang J, Du YY, Lin YF, Chen YT, Yang L, Wang HJ, Ma D (2008) The cell growth suppressor, mir-126, targets IRS-1. Biochem Biophys Res Commun 377(1):136–140. https://doi.org/10.1016/j.bbrc.2008.09.089
Saito Y, Friedman JM, Chihara Y, Egger G, Chuang JC, Liang G (2009) Epigenetic therapy upregulates the tumor suppressor microRNA-126 and its host gene EGFL7 in human cancer cells. Biochem Biophys Res Commun 379(3):726–731. https://doi.org/10.1016/j.bbrc.2008.12.098
Liu B, Peng XC, Zheng XL, Wang J, Qin YW (2009) MiR-126 restoration down-regulate VEGF and inhibit the growth of lung cancer cell lines in vitro and in vivo. Lung Cancer 66(2):169–175. https://doi.org/10.1016/j.lungcan.2009.01.010
Jusufovic E, Rijavec M, Keser D, Korosec P, Sodja E, Iljazovic E, Radojevic Z, Kosnik M (2012) let-7b and miR-126 are down-regulated in tumor tissue and correlate with microvessel density and survival outcomes in non–small–cell lung cancer. PLoS ONE 7(9):e45577. https://doi.org/10.1371/journal.pone.0045577
Li Z, Chen J (2011) In vitro functional study of miR-126 in leukemia. Methods Mol Biol 676:185–195. https://doi.org/10.1007/978-1-60761-863-8_13
de Leeuw DC, Denkers F, Olthof MC, Rutten AP, Pouwels W, Schuurhuis GJ, Ossenkoppele GJ, Smit L (2014) Attenuation of microRNA-126 expression that drives CD34+38- stem/progenitor cells in acute myeloid leukemia leads to tumor eradication. Cancer Res 74(7):2094–2105. https://doi.org/10.1158/0008-5472.CAN-13-1733
Sun Y, Bai Y, Zhang F, Wang Y, Guo Y, Guo L (2010) miR-126 inhibits non-small cell lung cancer cells proliferation by targeting EGFL7. Biochem Biophys Res Commun 391(3):1483–1489. https://doi.org/10.1016/j.bbrc.2009.12.098
Sun YQ, Zhang F, Bai YF, Guo LL (2010) miR-126 modulates the expression of epidermal growth factor-like domain 7 in human umbilical vein endothelial cells in vitro. Nan Fang Yi Ke Da Xue Xue Bao 30(4):767–770
Das E, Bhattacharyya NP (2014) MicroRNA-432 contributes to dopamine cocktail and retinoic acid induced differentiation of human neuroblastoma cells by targeting NESTIN and RCOR1 genes. FEBS Lett 588(9):1706–1714. https://doi.org/10.1016/j.febslet.2014.03.015
Das S, Foley N, Bryan K, Watters KM, Bray I, Murphy DM, Buckley PG, Stallings RL (2010) MicroRNA mediates DNA demethylation events triggered by retinoic acid during neuroblastoma cell differentiation. Cancer Res 70(20):7874–7881. https://doi.org/10.1158/0008-5472.CAN-10-1534
Foley NH, Bray I, Watters KM, Das S, Bryan K, Bernas T, Prehn JH, Stallings RL (2011) MicroRNAs 10a and 10b are potent inducers of neuroblastoma cell differentiation through targeting of nuclear receptor corepressor 2. Cell Death Differ 18(7):1089–1098. https://doi.org/10.1038/cdd.2010.172
Poliakov E, Samuel W, Duncan T, Gutierrez DB, Mata NL, Redmond TM (2017) Inhibitory effects of fenretinide metabolites N-[4-methoxyphenyl]retinamide (MPR) and 4-oxo-N-(4-hydroxyphenyl)retinamide (3-keto-HPR) on fenretinide molecular targets beta-carotene oxygenase 1, stearoyl-CoA desaturase 1 and dihydroceramide Delta4-desaturase 1. PLoS ONE 12(4):e0176487. https://doi.org/10.1371/journal.pone.0176487
Funding
Funding for this study was provided by grants from Gaziantep University Scientific Research Project Unit (Project Number: TF.YLT.18.43). Also this study was supported by Gaziantep University Health Sciences Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that all authors have no potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yücel, E.I., Sahin, M. Fenretinide reduces angiogenesis by downregulating CDH5, FOXM1 and eNOS genes and suppressing microRNA-10b. Mol Biol Rep 47, 1649–1658 (2020). https://doi.org/10.1007/s11033-020-05252-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-020-05252-6