Abstract
In this article, I present a philosophical account of medical treatment. In support of this account, I offer a suggestive account of medical conditions. The account of medical treatment uses three desiderata to demarcate treatment from non-treatment. Namely, a treatment should: (1) be describable by features that enable it to be standardized and characterized as a discrete intervention, (2) target a specific medical condition, and (3) have the possibility of being effective. The account of medical conditions underlies the second desideratum and attempts to tie medical conditions closely to biological dysfunction, while also including some conditions for which biological dysfunction is absent or its presence uncertain. I offer a simple typology of treatments and show how the accounts are relevant to treatment effectiveness, disease, placebos, contested treatments, and treatment standardization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Which among the following are medical treatments?:Footnote 1
-
swimming with dolphins
-
so-called placebos (such as microcrystalline cellulose pills or saline injections)
-
lysergic acid diethylamide (i.e., LSD) and other psychedelics
-
homeopathy (either as part of a treatment package, or without any awareness of its administration)
-
having morphine administered surreptitiously (and not with advanced consent), or with prior consent and awareness that it will be administered, just not when
-
conversion therapy (i.e., psychotherapeutic methods to change people from being homosexual)
-
acupuncture in which the needles have the appearance of puncturing the skin but actually do not
-
euthanasia
-
using the substance abused to treat substance abuse (such as using opioid agonists to treat opioid use disorder)
-
smoking cigarettes
-
yoga for menstrual pain and discomfort
-
liposuction for obesity
Historically, innumerable exotic, commonplace, unexpected, outlandish, and dangerous substances and procedures have been deployed in sundry attempts to mollify, care for, repair, nourish, fortify, and cure patients [1]. In addition to some of the items on the aforementioned list, there are procedures that currently are — or at one point were considered to be — medical treatments, such as psychotherapy, exorcism, a ritual in ancient Greece involving sleeping in a temple, and diagnosis itself [2]. Additionally, substances as diverse as aspirin and human excrementFootnote 2 and many procedures involving medical devices, such as tourniquets, acupuncture (according to Traditional Chinese Medicine [TCM] principles), and percutaneous coronary intervention, are considered medical treatments. There are also procedures and substances whose effectiveness has not yet been determined or — based on unknown or implausible mechanisms of action — are likely to be ineffective. If the history of medicine is any indication, most of these are likely to be placebos [1]. Yet, are placebos treatments?Footnote 3
Treatment and medical conditions are central to medicine. While it could be argued that there is no correct definition of treatment or medical conditions, or that such definitions do not have any significant implications, the designation of something as a treatment or medical condition can have profound health and social ramifications. “Treatmenthood” and status as a bona fide medical condition can result in something being accorded or denied medical reimbursement, can circumscribe the domain of substances, procedures, and conditions suitable for medical research, and can suggest standards of effectiveness, including for whom and which conditions a putative treatment might be effective. Simply designating something as a treatment could influence attitudes and expectations towards potential effectiveness — which could become a self-fulfilling prophecy, as with some placebos. Whether something like swimming with dolphins (which has been claimed to be effective for patients with mild to moderate depression [3]) even falls under the category of treatment or potential treatment can determine whether resources should be spent on further assessing its effectiveness. The existence of contested or debatable medical conditions such as short stature, ugliness, menopause, and stuttering, and contested or debatable treatments, such as LSD for depression, using the substance abused for the treatment of substance abuse [4], sham acupuncture for anxiety, or typically harmful activities such as smoking cigarettes for “stress” or anxiety, lends gravity to why accounts of treatment and medical conditions might be immediately and clinically useful. Disqualifying such substances and procedures outright from being the types of things that could even potentially ameliorate a medical condition — such as is done for LSD in the United States and other countries — could deprive patients (such as those with severe depression) from what might otherwise be a successful treatment for a refractory condition. Discounting such conditions’ being “medical” could deprive people of access to reimbursed treatments and other social resources, such as the sick role.
Overall, these — and the examples I offered in the opening list (not all of which are necessarily treatments) — are meant to show that an account of treatment that could demarcate treatment from non-treatment could be philosophically important (e.g., by clarifying the relationship between treatments and placebos, and treatment and disease), informative for bioethical debates, and of potential clinical relevance. My intended contribution in this article is to offer accounts of treatment and medical conditions that are useful in these regards and that can fill gaps in little-explored areas of the philosophy of medicine.
My accounts rest on analyses of treatment and medical conditions whose targets are largely for medical and socio-anthropological usage of the terms. Whether they are correct analyses, however, only partly depends on this usage because (with respect to treatment) my account may accord or disclaim treatmenthood to what some consider (or have historically considered) to be (non)treatments. Examples of what I consider to be non-treatments are conversion therapy, homeopathy (for any medical condition) when considered outside of the treatment package in which it is typically administered (i.e., if it were administered surreptitiously), and anything to “treat” drapetomania. Conditions that I think are non-medical are some of the conditions in the Diagnostic and Statistical Manual of Mental Disorders (DSM). In this respect my accounts are not solely descriptive but could be seen as being revisionary and offered in the spirit of philosophical explication [5].
I develop my account of medical treatment by offering a set of desiderata for treatmenthood that is able to demarcate treatment from non-treatment. I also attempt to show how understanding treatmenthood can help distinguish among treatments. Accordingly, I explore various ways in which treatments have been categorized (in the next section), and later I provide a simple typology of treatments (in the penultimate section).Footnote 4 If my account is successful, it will be able to offer a principled understanding of why something should or should not be considered a treatment, and at least one way in which treatments can be classified.
A comprehensive philosophical account of medical treatment does not appear to exist. Multiple factors could explain this lacuna. These include how common treatments are, how readily innumerable examples of treatments can be proffered, how simple and apparently unambiguous it is to identify treatments, how extensively individual treatments can be characterized and explained without need of an underlying theory, and how ostensibly lacking in conceptual problems treatment presents. Yet these factors also underlie why an account of medical treatment could be philosophically significant and practically important. Before I present my account, I next provide an overview of various ways in which treatments have been categorized.
Treatment categorizations
Much of what are considered treatments by modern medicine reflect a basic division of treatments into pharmacological (e.g., drugs and biologics) and nonpharmacological treatments (NPTs; e.g., the expressive arts therapies such as dance, drama, music, and art therapy; physical therapy; acupuncture; yoga; meditation; exercise; medical devices; nutrition therapy and diet; psychotherapy; surgery). This division illustrates how a traditional view of medical treatment as consisting mostly of drugs and surgery is far too constricting of the range of treatments that are and have been used by medicine. Treatments have existed since prehistory [6] and have been characterized in various ways. The earliest reported comparison of treatments may have been that of diets mentioned in the Book of Daniel in the Bible. The many healing systems that have existed underscore not only the diversity of treatments but also how diversely treatments have been conceptualized. Yet throughout much of medical history most treatments have been deemed (in retrospect) as nothing more than placebos [1]. With the advent of randomized controlled trials (RCTs), a mark of treatmenthood could be considered comparison with placebos [7], although many treatments that could not be studied with RCTs were and are still recognized as treatments.
Specific treatments have been characterized in explicit detail from a range of perspectives and methodologies: biochemical, anthropological, psychological, economic, sociological, and, more specifically, from biopsychosocial models, etiological models, hermeneutical approaches (e.g., [8]), and from non-allopathic medicine, such as TCM and complementary and alternative medicine viewpoints. Simple typologies of treatments based on the treatment target can be imagined, such as viewing treatments as those which treat, inter alia, the person (e.g., according to TCM, treating a person having a “heat pattern” with heat-clearing herbs [9]), the disease/condition (riboflavin supplementation to treat cheilosis), symptoms (lip balm to treat cracked lips, a symptom of cheilosis), or risk factors (statins to treat high cholesterol). This can engender distinctions between treatment that is holistic, therapeutic/curative, palliative, and preventive, respectively. However, because many treatments cross these boundaries and because the boundaries between these targets are themselves vague, I do not examine these distinctions any further, with the exception of preventive treatments in a later section.
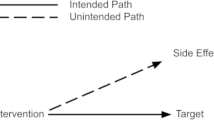
Beyond these approaches, several broader categorizations have been offered. For example, a taxonomy of medical treatments meant to encompass all human therapies has categorized treatments on the basis of three types of therapeutic elements: defining or characteristic, contextual or incidental, and preliminary (such as diagnosis and other factors that trigger self-healing even before when treatment is formally given [10]). In articulating their theory of placebo effects, Miller, Colloca, and Kaptchuk [11] posited healing as being of three types: natural, interpersonal, and technological. Yet another tripartite classification divided treatments into autonomous, specific, and meaning categories [12]. This taxonomy was not developed into an account of treatment but rather offered passim, en route to a theory of placebos.
In summary, various frameworks have been used to categorize treatments, although less attention has been paid to what makes something a treatment in the first place. I next discuss two such approaches.
Accounts of medical treatment based on effectiveness or placebo
Of the scant philosophical work that exists on treatment, treatment has typically been defined or could be understood not intrinsically but instead relative to something else, such as effectiveness or placebos. Each approach, however, has important limitations.
Effectiveness
Effectiveness could be considered as necessary for treatmenthood; i.e., something has to be effective for it to be a treatment.Footnote 5 I reject the necessity of effectiveness for treatmenthood as it is too demanding, vague, and dependent upon an unspecified account of treatment effectiveness. Treatments can have a range of effectiveness, including ineffectiveness. Instead of viewing an ineffective — or probably ineffective — treatment as not being a treatment at all, an alternative is to simply consider such treatments as ineffective or probably ineffective. Although conceptual issues should not be confused with epistemic ones, maintaining that effectiveness is necessary for treatmenthood could render the demarcation of treatment from non-treatment subject to the vicissitudes of establishing effectiveness and an attribution that could only be made retrospectively after an effectiveness determination is made. There is no widely accepted account of effectiveness; indeed, there are few to choose from [13,14,15]. Accordingly, for any given treatment there can be difficulty reaching agreement over a standard of effectiveness.Footnote 6 Many treatments that were considered bona fide treatments throughout history, such as trepanation, bloodletting, or pouring boiling oil on gunshot wounds, are now known to be ineffective or downright harmful, yet have been used for many reasons [16]. While it is possible to conceive of ineffective treatments as not treatments at all, an alternative approach does not tie treatmenthood to effectiveness. This approach better reflects medical history and clinical reality by allowing for the possibility of there being ineffective treatments — just as there can be bad treatments, unethical treatments, or treatments whose effectiveness is unknown.
Placebo
Treatments have also been characterized in relation to placebos, most notably with those based on Grünbaum’s [17] account of placebos. Briefly, such accounts divide treatments into incidental and characteristic features; placebo effects result from the incidental features of treatments in clinical trials [18, 19]. One motivation behind Grünbaumian accounts is being able to identify placebos via a treatment’s incidental features, which can then enable setting up a placebo-controlled trial to evaluate the effectiveness of that treatment. Such accounts suggest that whether something is a treatment can be tested by the use of a placebo. Holman [18, p. 1334], for example, on his way to a more comprehensive definition of placebo, as a first pass writes, “a treatment t* is a placebo in an RCT testing t for D iff it plays the methodological role required to determine whether t is a treatment for D.” Basing an account of treatment on such an account of placebo (were that to be done), however, involves circularity, since the definition of placebo itself involves the notion of treatment. There are other problems with Grünbaumian accounts of placebo. These include indistinguishability of incidental and characteristic features, failure to offer a positive account of placebo effects, and dependence upon (potentially labile and contestable) theories of the specific treatments in question [20].This latter aspect has the effect of turning placebo boundaries into moving targets, similarly making treatments into moving targets.
Admittedly, understanding placebos may be integral to understanding important aspects of treatment; e.g., placebo effects accompany almost all medical encounters, and the ways in which meaning and expectations can interact with the non-psychological features of treatments show why placebo effects are vital to the theory and practice of medicine [10, p. 457; 21, p. 9; 22, p. 1874]. Most accounts of placebos, however, cannot satisfactorily reconcile the role of placebo effects in treatment (clinical practice) with the role of placebos in testing treatments (research) [23, 24]. In summary, placebos are not needed to determine whether something is a treatment, and having incidental and characteristic features is not a necessary attribute of treatments.
Medical treatment desiderata
As mentioned above in the first section, my account of treatment reflects the incredible variety of substances, devices, and procedures that have been and are considered treatments. This is informed by treatments from medical textbooks; treatments used in non-allopathic healing traditions, such as TCM and complementary and alternative medicine; and treatments from medical history. A potential shortcoming of this reckoning, however, is that the attribution of treatmenthood has not always been officially sanctioned by the healthcare community or even made explicit. It could also differ among and between individual patients, clinicians, and cultures. Nonetheless, one salient mark of treatment attribution throughout history has been the idiosyncratic nature of many treatments. My account therefore can capture treatments only used or considered as treatments by a single person. After all, new treatments must arise somehow, and though not all treatments are successful enough to rise to the level of widespread use, there are many treatments that people may swear by that are never studied or even considered by the medical establishment.
Whether something is considered a treatment or medical condition depends on a complex interplay of cultural, personal, social, and political factors, and could change with different societal norms and technologies. The use of methadone as a treatment for heroin addiction or opioid dependency exemplifies this: methadone is viewed by some people as simply a way to manage undesirable addiction behavior, whereas others frame its use within a disease model and therefore consider it a medical treatment [25]. Other examples are any idiosyncratic activity that a person thinks might help them, which might nonetheless be considered by others to not be a treatment.
Therefore, the following (possibly non-exhaustive) list of desiderata is meant to capture necessary features of treatment. Medical treatments:
-
1.
are describable by features that enable them to be standardized and characterized as discrete interventions;
-
2.
target a specific medical condition; and
-
3.
can possibly be effective; i.e., are not solely explainable (in terms of potential effectiveness) by highly implausible mechanisms of action.
Discreteness and standardization
Standardization is how treatments are made discrete and differentiated from other treatments. The simplicity and obviousness of this desideratum should not belie its importance: if treatment types could not be individuated and distinguished from other treatments then identifying a token treatment would be impossible. Standardization can be conceptualized as the package of features describing a treatment. Although this desideratum might seem obvious — after all, if treatments were not defined by features then by what would they be defined? — standardization defined this way (and the inclusion of this desideratum) is meant to reflect the fact that treatments have often been defined not by a unitary set of features but rather as a portmanteau of characteristic and incidental features. In the section above on placebo, I suggested that treatments should not be necessarily viewed according to this Grünbaumian account.
What is sufficient for standardization may involve specifying which elements of a treatment are necessary, which are optional, and what are the bounds for deviation. By looking at standardization this way, treatments with very wide variations can still be (seen as) standardized and validly compared across settings and populations. However, when treatments deviate from what is specified, or are described in ambiguous terms, then treatment comparisons become problematic for research and clinical use. The possibility, especially for complex interventions, of treatments studied in clinical trials being different from treatments administered in clinical practice (despite having the same name and intentions) underscores the importance of standardization and not overlooking contextual factors in the description of a treatment.
How treatments should be described and what should be considered a treatment variation as opposed to a different treatment depend on social and personal factors, including social acceptability, costs, goals, stakes, personal preference, and amenability to research.Footnote 7 When are variations in treatment descriptions acceptable? Walker [26, p. 341], writing in the context of conducting valid RCTs for patient-specific devices, posits that variations are impermissible when they are causally effective; for example, changing pen color in surgery is likely an acceptable variation, whereas changing the surgeon typically is not. However, in terms of standardization as a desideratum for treatmenthood, a type of surgery performed even with a different surgeon could still be considered the same treatment. This is because more than causal efficacy determines what makes a treatment discrete. After all, the causal efficacy of components may be unknown or difficult to assess.
In terms of characterizing a treatment, one proposal I can offer is that treatments should be described at a level of detail sufficient for good predictions of treatment effectiveness in the desired target setting and population.Footnote 8 What constitutes good will differ depending on the social and personal factors just mentioned. Treatments consist of far more than the so-called active ingredient, and which factors (including which contextual factors) are subsumed within the description of a treatment also reflect the aforementioned social and personal factors. Large differences in effectiveness, however, even if consistent across different subpopulations, do not necessarily mean a different treatment is involved. For some drugs, such as morphine, the environment in which it is taken — and even the mindset and awareness of the recipient at the time it is taken — can engender drastically different effects. This can be illustrated by the difference between morphine received via covert administration (morphinec; i.e., without the patient’s awareness of when it is received) and morphine taken in the open (morphineo), with the patient aware of its administration.Footnote 9 Even morphinec has a contextual backdrop: e.g., lying in a hospital bed and being unaware when one is being treated. A common interpretation has been that the difference in effects between the two methods of administration represents placebo effects [27, 28].
Thus, should morphinec and morphineo be viewed as two different treatments, despite the presence of the same pharmacological substance? Or should they be viewed as the same treatment administered or taken under different circumstances, or more generally as a variant of a single treatment? While it might seem that just changing the method of administration should not be sufficient to transform one treatment into another, for research purposes each of these treatments would involve different control groups, and for clinical practice different perceptions and levels of acceptability. Additionally, when certain treatment components, including contextual factors, hold key roles in defining a treatment, they can potentially turn what prima facie might appear to be one treatment into another treatment, despite the same main pharmaceutical constituent being present. For example, some branded pharmaceuticals, such as Sarefem and Prozac, contain the same key ingredient (in this case fluoxetine), but have different branding and indications (Sarefem to treat premenstrual dysphoric disorder, Prozac to treat major depressive disorder, among others). Similarly, Proscar and Propecia both contain finasteride but have different packaging, labelling, dosages, and indications (benign prostatic hyperplasia and androgenic alopecia, respectively). Differences such as branding can be causally effective, as Branthwaite and Cooper’s 1981 study [29] of branded aspirin being more effective than unbranded aspirin — whether placebo or verum — makes clear, as do other examples of the so-called meaning response [12]. Another example is sham acupuncture administered by an empathetic practitioner as part of an attentive, responsive package of care versus acupuncture administered with limited interaction with the patient [30]. Furher still, cocaine at low dosages and when topically applied is used for its anesthetic and vasoconstrictive properties, whereas at higher dosages, when injected or snorted, it induces euphoria.Footnote 10 Low-dosage cocaine might thus be considered one treatment and high-dosage cocaine potentially another, each for different indications.
Different dosages, modes of administration, and contexts of a drug or procedure thus seem like they could entail different treatments. However, all these factors influence what could alternatively be described as discrete treatments whose effects simply vary with context. Different people (or the same person at different times) responding differently to a treatment do not necessarily mean different treatments are involved. Only if the package of features describing a treatment differ from those describing another treatment would there be two different treatments.
Targeting of a specific medical condition
The purpose of this desideratum is to mark off conditions and treatments that are medical from those that are non-medical. Despite the large and varied philosophy of disease literature, and the excellent sociological and philosophical work done in defining the limits of medicalization, little comprehensive attention has been paid to defining medical conditions themselves (with some exceptions, such as Kukla [31], who defines health conditions). Because of the complexity of the issues involved and the limited space I have here, I only provide a preliminary account.
First, some groundwork is needed. Something that did not target a specific medical conditionFootnote 11 could not be a medical treatment on my account. This is to avoid indiscriminately considering anything a treatment simply because it could treat a medical condition, whether known or yet to be discovered. Clinical outcomes are how improvement in medical conditions is assessed. These range from standard measures of effectiveness such as mortality, to patient-reported outcomes such as health-related quality of life, to individual-based metrics such as whether a patient simply feels better after taking a treatment. All outcome measures, whether assessed on a population level (such as in the context of a clinical trial) or on an individual level (such as in clinical practice), are indexed to the condition being targeted and the desired outcome. For example, sulfonylureas are treatments for diabetes but not for gout, and although they are treatments for lowering blood sugar levels, they are not treatments for regenerating pancreatic beta cells. Finally, my focus in this article is the individual — the bearer of a medical condition. A “treatment” that targets the population level is better considered a public health intervention.Footnote 12
What marks off a condition as being medical? The conjecture that medical conditions are whatever are considered, diagnosed, or treated by physicians neglects the many non-physician healthcare practitioners who ostensibly deal with medical conditions. Tying medical conditions to the wider category of healthcare practitioner encounters the same problem of demarcating who counts as one. While suggestive of what is a medical condition, such a definition lies prey to the vacillating sociological contingencies of time, place, and culture. This potentially neglects people in certain roles (e.g., shamans; dentists; podiatrists; physician assistants; art, dance and speech therapists; nutritionists; and chiropractors) who could conceivably be viewed as practicing medicine or at least as administering medical treatments that can have profound effects on medical conditions, and ignores the way most treatments throughout history have achieved their effects (i.e., via the placebo effect, which does not necessarily need a healthcare practitioner to work). Similar issues arise when defining medical treatment as whatever is considered or administered by healthcare practitioners. Indeed, to avoid a circular definition, I tie medical treatmenthood to medical conditions and accordingly define medical conditions independently of medical treatment.Footnote 13
Demarcating what is — or what should be — the domain of medicine is no easy task. Contemporary medicine includes (for better or worse) within its ambit diseases as well as conditions that represent normal variation, such as short stature (for which human growth hormone is considered a medical intervention), or that could be viewed as problems in living or violations of social or individual norms (e.g., some of the conditions listed in the DSM). Medicine also tends to palliation, relief of discomfort related to normal conditions such as menstruation and teething, sleep-wake cycle adjustments (such as to treat jet lag), anesthesia, organ and blood donation, and common dysfunctions of aging like presbyopia [34, pp. 150–151]. That “medicine is, in all essence, about illness” [35, p. 323] carries a ring of truth, though if one holds, as I do, that illness must involve symptoms, then it is not strictly true given that some diseases are asymptomatic. Moreover, many medical conditions, such as blindness and limb paralysis, are not illnesses [36]. Illness typically involves suffering, but not all suffering involves illness or disease.Footnote 14 Not all illnesses even involve disease because illnesses can simply stem from patients’ symptoms in the absence of disease or be associated with contested diseases. Medicine also regularly ministers to risk, whether through public health interventions or what might be considered preventive treatments, such as statins. Yet not all risk states constitute illness [37]. Finally, the aforementioned (footnote 12) autopsy can hardly be said to involve a medical condition that could be treated, yet is squarely part of medicine.
Important to my accounts of treatment and medical conditions is thus the observation that healthcare practitioners intervene on not only disease but also non-disease medical conditions as well as non-medical conditions. There are conditions for which putative medical means can be used, but this does not necessarily make the condition a medical condition. Not all interventions that involve medical means (e.g., cocaine for ennui, barbiturates for euthanasia, steroids for improved sports performance), that are performed by healthcare practitioners (e.g., medically assisted torture, sterilization, some types of cosmetic surgery), or that can significantly improve medical conditions (e.g., poverty reduction and health education programs) are medical treatments. So-called “standard” medical means (like drugs, surgery, and some procedures and devices) can be used for purposes like euthanasia, but this does not make them treatments simply because they would be considered treatments when used for different purposes (like reducing anxiety). By contrast, some interventions, like hot baths for respiratory tract infections or a friend’s support for depression, are not typically considered to be medical yet can still improve symptoms. On my account these are bona fide medical treatments (assuming they meet the three desiderata, such as that the depression is a medical condition) — what might be called “non-medical” medical treatments (i.e., non-medical in the sense of being non-“standard” per the aforementioned list). These are medical treatments that do not involve things people seem to typically associate with medical treatments (see the section “A simple typology of treatments” for an example and further discussion).
With this in mind, it becomes necessary to circumscribe the domain of medicine specifically for medical conditions. I canvas the following categories as possibilities for what should be or might be medical conditions: (1) pathology, (2) pain/discomfort/distress associated with pregnancy and some normal developmental processes, (3) some conditions involving risk for disease, and (4) some types of symptoms. I address each in turn, noting that this list is neither conclusive nor necessarily exhaustive.
Pathology
I consider pathologyFootnote 15 to be a proper subset of medical conditions. Treatment defined or circumscribed on the basis of pathology (or disease) could be seen as elucidating the nature of treatment by seeking to understand the ends of treatment. Stegenga [13], for example, ties integral features of treatment effectiveness to a so-called hybrid conception of disease, holding that an effective treatment must successfully target at least the constitutive causal basis of disease (i.e., its biological basis) or the normative basis of disease (i.e., the harm it causes). “Treatments” that do not successfully target these bases could then be argued to not be treatments because a “treatment” that could not conceptually be effective could be viewed on this account as not being a treatment at all.Footnote 16
Normative conceptions of disease view disease as fundamentally value-laden whereas naturalist conceptions disclaim this value-ladenness. Although conceptual divisions are not as simple as traditionally thought, one useful way to distinguish among conceptions of disease is whether they are dysfunction requiring or not [39]. Boorse’s biostatistical theory (BST) and Wakefield’s harmful dysfunction analysis (HDA) are two of the most well-developed and influential dysfunction-requiring conceptions of disease. The BST posits that diseases are states of statistically subnormal part-functional ability, relative to species, sex, and age [40, 41]. Although there are many conceptions of disease, with little agreement as to the best one [42], there is a strong contingent of contemporary support for at least important aspects of naturalist conceptions of disease, including the notion that disease should be viewed in terms of physiological dysfunction [13, 32, 43,44,45] and that the BST is relevant to clinical practice [32, 45]. In this article, I rely on the BST for my conception of disease (pathology).
Different disease conceptions entail different extensions, and it should not automatically be assumed that naturalist conceptions include more diseases than normative conceptions. Schwartz [46, p. 330], for example, states, “non-DR [dysfunction requiring] definitions are overly inclusive, and this feature leads them to classify stage 1 hypertension and high cholesterol as diseases.” Other authors adhere to naturalist accounts of disease as a way of limiting medicalization and demarcating what can legitimately be claimed of scarce healthcare resources [47]. Although some conceptions of disease overlap in their extensions with what I include under medical conditions, what I consider to be a medical condition, and therefore what can be a treatment, is actually narrower than that implied by some normative conceptions of disease. For example, many (if not all) of the conditions listed in the DSM are considered by many people (lay people, philosophers, and healthcare professionals) to be medical conditions — either brain diseases [48, 49] or autonomous mental disorders (i.e., not necessarily involving brain dysfunction, a possibility entertained by Boorse [50], Graham [51], Jefferson [52], Papineau [53], and Schramme [54]). However, there are also people who challenge the idea that DSM conditions are medical, and on my interpretation of the BST it is likely that only some DSM conditions are diseases while others could be non-pathological medical conditions, conditions involving aspects of diseases not yet recognized by medicine, or not even medical conditions at all. I examine this more below in discussing symptoms.
Pain/discomfort/distress associated with pregnancy and some developmental conditions
As intimated above, yoking treatment solely to a conception of disease assumes that treatments can only target diseases and not other medical conditions. The idea that a treatment can treat non-disease conditions seems to track natural usage of the term. For example, Cosmides and Tooby [55, p. 455], although not necessarily discussing medical conditions, offer a 22-item evolutionary taxonomy of treatable conditions that gives at least some support to the idea that the target of treatment is conceived widely and can involve non-disease conditions.
There are numerous non-disease conditions, such as pregnancy, developmental processes (such as teething, menstruation, and menopause), and possibly others that can also plausibly be seen as medical conditions when associated with pain, discomfort, or distress. The reasons for accepting these as medical conditions and not the pain, discomfort, or distress associated with conditions like hunger, hurt feelings, or aberrant behavior partly stem from the long history of the former conditions as uncontroversially falling under the medical gaze [34]. Moreover, because these are developmental stages, there is not a need to establish thresholds at which the condition turns medical (such as with hunger), or to distinguish them as not reflecting violations of social norms (such as with aberrant behavior).
Risk of disease
Preventive care is a chief concern of medicine. Risk of disease is assessed via various types of epidemiological studies and/or basic research, and is ascertained in clinical practice through the use of increasingly sensitive medical technology that indicates the statistical likelihood of future development of disease. However, there are many risk states for which pathophysiological processes have yet to begin (e.g., risk for subdural hematoma in someone who has yet to suffer from traumatic head injury). Putative preventive treatments (e.g., bike helmets) are thus best thought of as preventive interventions used to thwart the pathophysiological process from occurring at all. They would not be treatments on my account because they would not be targeting a medical condition (since a disease has yet to occur).
Focusing on internal risk states as the types of things that could be medical conditions is an improvement but still encounters the daunting fact that risk is inherent in most of life. It is unclear what distinguishes such risk states that are medical conditions from those that are not. After all, there are multiple types of risk factors for disease, of varying strengths and types of causal relationship. Many non-medical, external states (e.g., coal mining) carry a higher risk of disease than some internal, presumably medical, states (e.g., obesity), making probability of disease on its own a poor distinguishing feature of risk-based medical conditions. The extension of such conditions could be enormous unless criteria are applied to limit them. What these criteria are is not immediately clear. One could stipulate that these could be context-sensitive and dependent on the goals, stakes, and cost-benefit ratios of the situations in which a determination about the status of a putative risk-based condition as being medical needs to be made. That, however, makes the concept of risk-of-disease–based medical conditions potentially capricious and not subject to a stable, objective standard. Even if the seemingly objective standard of probability of disease were used as a desideratum, it is not immediately clear how it would be assessed, where the cutoff would be, or whether certain types of risk (e.g., environmental versus genetic) would count more than others in distinguishing risk states as medical conditions.
Nonetheless, it does seem intuitive to consider drugs such as statins as preventive treatments for stroke and heart attack, especially if used as secondary prevention (i.e., for a person who has already had such an event). However, a person who has had a heart attack presumably already has a disease (heart disease), making their medical condition status not at issue.
Rather than trying to arrive at some a priori way to distinguish between risk states that are medical conditions from those that are not, one could perhaps look towards what modern medicine considers to be non-disease, risk-based medical conditions (such as via what is commonly treated and granted insurance reimbursement) and try to extract from this a principled set of reasons underlying the distinction. For example, some risk states are commonly considered medical conditions (e.g., obesity), either because they are considered diseases themselves or because they carry a high risk for more serious diseases. Schwartz [46] has argued that many common conditions like osteoporosis, hypertension, hypercholesterolemia, and obesity are better seen not as diseases but as risk states. I agree these are likely not diseases for at least some levels of the parameters that currently characterize them as diseases. With their common acceptance in much of contemporary medicine as chronic diseases (for which enormous effort is made to “treat” them), considering them risk-based medical conditions might then not seem unreasonable. However, what makes these and not other risk states medical conditions is still unclear. While some such risk states could be viewed as vulnerabilities related to incipient stages of disease (and therefore possibly medical conditions because of a clear causal nexus and high probability of occurrence), what complicates this picture is when the presence of dysfunction is uncertain, such as in Alzheimer disease [45]. In such cases, uncertainty as to whether dysfunction is present makes the risk of such dysfunction even more uncertain. Nonetheless, some chronic diseases can be characterized as dispositional bodily states or properties [44], and, as Boorse notes [56], some physiological systems could function to prevent future disease. However, the aforementioned line-drawing problem still remains.
An alternative to characterizing states involving risk of disease as medical conditions is simply viewing such states as risk states for which there could be preventive medical interventions. I cannot resolve where the line should lie between these possibilities, so I offer this as a question for future analysis.
Symptoms
The inclusion of this category is meant to reflect medical conditions that are constituted by symptoms even if disease is not confirmed or (possibly not even) present. Symptoms I posit are subjectively experienced indications of pathology, nonmedical responses (like a voluntary cough or a cough in response to dust exposure), or (possibly) non-pathological medical conditions. The latter possibility is motivated by what might be a class of non-pathological medical conditions constituted by symptoms that do not reflect underlying biological dysfunction, yet for prudential or ethical reasons still seem like things that should be in the domain of medicine. Consider regular exposure to loud noise, jet lag, being a refugee, and living above a restaurant. All of these can make people feel very ill and produce symptoms, but do not necessarily involve (identifiable) pathology. Still, for whatever reason (severity, harm, involuntariness, treatment responsiveness, etc.), these symptoms could make sufferers think they have a medical condition, especially if doing so could provide access to the sick role or other needed resources. Such examples, however, should be considered in light of more contentious cases. For example, a breakup after a short relationship could result in a severe depression considered by some to be medical, or by others an unpleasant but non-medical part of life. A critical question thus arises as to what makes some feelings symptoms, given that not every unwanted feeling is a medical condition or indicative of one. Modern psychiatry adopts the route of assuming the symptom complexes (i.e., mental disorders) articulated in the DSM are medical, while in nonpsychiatric medicine there is a strong presumption that, solely or mainly, the application of pathology-related knowledge is required to make this distinction.Footnote 17
However, if medical conditions extend beyond pathology, then it is necessary to articulate clear qualifying and disqualifying features for symptom-based, non-pathological medical conditions. Evaluating the disease status of mental disorders may be a fruitful place to start thinking about this category. This is because of the widely endorsed inclusion of psychiatry in medicine, whereby many conditions, such as those in the DSM, are viewed as medical conditions because they are considered diseases. Yet many scholars (e.g., [57]) question the overreaching of psychiatry into pathologizing normal life, while the “anti-psychiatry” tradition (such as advanced by Szasz [58], though not under that label) and critical psychiatry tradition (such as advanced by Moncrieff [59]) go a step farther by doubting that there are mental diseases at all, viewing many of the conditions in the DSM as violations of social norms and not as medical conditions. Moreover, medical knowledge is limited and its application in practice can result in harm to patients when there is confusion over the relationship between mental disorders and medical conditions [60]. For example, according to many mainstream sources, approximately 50% of symptoms encountered in clinical practice are medically unexplained (reviewed in [61]), where no physical pathology has been identified. Patients with such symptoms continue to suffer (even to the point where some patients “self medicalize” their condition(s) [62]). In many cases, diseases are later found to account for their symptoms. Yet the standard approach in most of (allopathic) medicine is to treat such patients as if they had mental disorders [60]. This, however, can be harmful by resulting in expensive, ineffective, and/or harmful psychological/psychiatric treatment; committing epistemic injustice by not validating patients’ superior perspective on the difference between bodily sensation and psychological distress; stigmatizing patients; and forestalling further investigation that could uncover a potentially deadly condition like heart disease, a rare disease, or one (e.g., systemic lupus erythematosus) strongly associated with many so-called psychological symptoms (e.g., anxiety, depression). Some of these symptoms might also indicate diseases not yet recognized by medicine, such as was the case with myalgic encephalitis/chronic fatigue syndrome [64]. Clinical and ethical considerations therefore seem to support generally recognizing medically unexplained symptoms (MUS) as medical conditions, even if disease might not be present.
If mental disorders are diseases, then my above analysis on pathology applies. On dysfunction-requiring conceptions of disease, there is support for at least some mental disorders being diseases. For example, Boorse [50] thought the BST could apply to mental disorder via the demarcation of core mental functions, an approach also taken by Wakefield’s HDA [65,66,67]. There are problems with this approach, however, such as being able to demarcate precisely what these mental functions are [68,69,70]. Furthermore, psychological dysfunction is not the same as physiological dysfunction, and cognitive, perceptual, affective, and motivational mechanisms could be seen as underlying person-level functions, not part-function as required by the BST. Mental disorders with no neural dysfunction therefore might best be seen as not being pathological in a medical sense, even if there is psychological dysfunction. Additionally, if one views the mind (and therefore mental functions) as inextricably linked with the environment (as some enactivist views do), then the presence of mental dysfunction might intrinsically (and implausibly from a perspective that views diseases as internal states) depend on other people’s behavior.
At the same time, one could argue that the psychiatric conditions that many patients with MUS are diagnosed with (e.g., what DSM-5 calls somatic symptom and related disorders), or some other DSM conditions for that matter, could also be considered non-disease, “mental disorder” medical conditions. However, criteria would then be needed to distinguish such putative medical conditions from the non-medical vicissitudes of life, and it is unclear what these criteria are. Further explicating these issues and resolving the boundaries of this category seem like considerable undertakings in the philosophy of psychiatry and medicine. I cannot attempt these here. Nonetheless, my hope is that my account of medical conditions provides at least a touchstone by which noncontroversial cases and even some controversial cases can be evaluated and considered as being medical or not, and therefore whether a putative treatment satisfying this and the other two desiderata is indeed a medical treatment.
Possibility of effectiveness/no sole posit of highly implausible mechanisms
A treatment that did not even have the biological or physical possibility of being effective would seem to not be a treatment at all. In this sense, putative treatments could be ruled out as treatments ab initio if there is simply no way they could work and be effective, even if they meet the other treatment desiderata. While above I rejected the necessity of effectiveness for treatmenthood, the inconceivability of effectiveness when there are only highly implausible mechanisms that could underlie any effectiveness is different from something being factually ineffective. One reason underlying this distinction is that the mechanisms putatively underlying the former cannot be falsified (e.g., how could one test whether the past lives of past-life regression therapy exist?), whereas the latter can (the miasma thought to cause cholera, though in hindsight incorrect, could nonetheless be investigated and disproven through scientific means). Moreover, different standards of effectiveness could entail the same treatment being effective on one standard but not another [15].
Nonetheless, this desideratum should not be used capriciously to disclaim treatmenthood, since for some putative treatments plausible mechanisms could exist that just have yet to be identified. Moreover, judging a mechanism as being highly implausible is somewhat subjective. More work is needed to identify what qualifies a mechanism as being “highly implausible.”
This desideratum can serve the salutary purpose of drawing attention to the first desideratum since the description of a putative treatment can affect the plausibility of how it could be effective. For example, the mechanismsFootnote 18 by which homeopathy (i.e., the homeopathic substance by itself) is said to work are inconsistent with what is known about the natural world. Using this to undermine homeopathy’s treatmenthood, however, is only applicable to certain descriptions of homeopathy, such as if the homeopathic substance were to be administered to a non-conscious patient. By contrast, homeopathy administered within the context of a caring therapeutic relationship could be effective through placebo effects. Thus, how a putative treatment is characterized, including the context in which it is to be administered, bears on treatmenthood. Since homeopathic substances in clinical practice are invariably administered within the context of a treatment package, if that is how “homeopathy” is characterized, then this desideratum cannot rule homeopathy out as a treatment. Homeopathy could only be ruled out as a treatment by this desideratum if it were characterized in a way such that no other mechanisms than the action of the dissolved substance could be responsible for any therapeutic effects. An example would be if the dissolved substance were to be administered in clinical practice to a non-conscious patient, or, in research settings, surreptitiously in comparison with a control group in which water or some other comparable placebo was also administered surreptitiously (to control for any possible effects of surreptitious administration).
Other desiderata
A desideratum I hold to be uncontroversial and obvious is manipulability; treatments can be manipulated (e.g., such as varying the amount and intensity of exercise, or changing the conditions under which drugs are administered). Related to the requirement for manipulability is not counting absences as treatments. For example, absence of phenylalanine is not a treatment. Absences cannot be manipulated and to allow them could increase the number of treatments, including such oddities as the treatment of not eating too much chocolate. As Fuller [44] notes in relation to diseases, absences can be reframed as capacities. Regarding treatment, absence of phenylalanine can thus be construed as a diet lacking phenylalanine.
Although I hold as necessary for treatmenthood that treatments target medical conditions, this should not belie the ubiquity of people being incidentally treated without their awareness (such as through engagement in various activities in their daily lives, or less commonly via surreptitious administration of drugs). Also, healthcare practitioners can treat incidentally, such as when administering a medicine that treats a medical condition they did not know the patient had. Via placebo effects, a healthcare practitioner could have no intention of treating at all yet still — such as by virtue of the patient’s expectations, beliefs, and conditioned responses to features of the healthcare practitioner’s clinic and/or demeanor — end up treating a patient. Treatment need not even involve a healthcare practitioner (e.g., in self-treatment). The distinction between ex post and ex ante attribution of treatmenthood can help make sense of these observations. In ex ante attribution of treatmenthood, a putative treatment is administered by a healthcare practitioner with either the healthcare practitioner’s or the patient’s awareness (typically both). In ex post attribution of treatmenthood, a putative treatment can be identified on the basis of possible effects it had on a person; the person themselves may have had no awareness they were being treated. This need not entail the treatment was effective; the putative treatment need only satisfy the three desiderata mentioned above to be a bona fide treatment. Any presumed plausibility of only allowing ex ante attribution of treatmenthood could reflect certain institutional arrangements related to the structure of healthcare delivery, and not necessarily intrinsic features of treatment. One could of course stipulate that the idea of ex post attribution of treatmenthood is implausible. The ubiquity of treatment (see the next section), however, suggests otherwise.
There are other candidate desiderata for treatmenthood I reject as I consider them to be too unlikely. One is treatmenthood’s requiring the existence of “plausible” mechanistic evidence or mechanistic reasoning or hypotheses to explain how a treatment works (which is different from treatmenthood requiring the possibility of effectiveness and not the sole posit of highly implausible mechanisms; see the previous section). The attraction of this desideratum may stem from cases of contested treatments, whereby the ability to tell a (good) story as to how the treatment might benefit people affected by a medical condition could be seen as evidence in support of treatmenthood. For example, a nostrum foisted upon an unsuspecting public might attain greater legitimacy in the eyes of potential users when accompanied by a plausible-sounding way in which it could treat one’s condition. However, endorsement of this desideratum is undermined by how capriciously it could be used to accord or disclaim treatmenthood. This is because there are multiple thresholds of what type of plausible mechanistic evidence could be required, with no apparent way to determine invariant superiority.Footnote 19 Moreover, the need for a plausible mechanism conflates conceptual issues with epistemic ones. Differences in availability of evidence, and changing views on what constitutes a plausible mechanism and the evidence needed to support that, would make such a criterion too uncertain and potentially too demanding for treatmenthood. Not requiring this criterion can make it easier for something to be a treatment, but I consider that a virtue as it better reflects medical history and different medical traditions (e.g., TCM, Ayurveda).
Reluctance among some people to accept some of the examples in the introduction as treatments could stem from privileging certain levels (social, psychological, cellular, etc.) that a treatment directly targets or is described on. Another possible desideratum for treatmenthood could thus be the presence or absence of certain level(s) that a putative treatment is described at or works on. Yet many treatments target multiple levels, and all treatments could be described to involve the psychological and social levels (if patients are aware their treatment is being administered by someone else) or the physical level (if the treatment changes biological parameters). Many complex interventions span multiple levels in terms of their descriptions and possible mechanisms, and if the clinical context is included in the description of a treatment, then most treatments, including drugs, could reasonably be described at multiple levels. This is especially true if such contextual factors — as many placebo studies indicate [78, 79] — have clinically relevant effects. Treatmenthood should thus not be ruled out based on the level(s) that a putative treatment is described at or works on.
Incidental treatment and the ubiquity of treatment
One consequence of my account of treatment is that many of the substances or procedures mentioned in the introduction are or could be treatments. Although more detail is needed to describe exactly what is involved in these possible treatments,Footnote 20 their core ingredients as mentioned there might strike some readers as unintuitive, unacceptable, obvious, and/or welcome. These treatment possibilities are not too far from clinical practice, however, especially when supplemented with a fuller description and rationale for what clinical outcomes are desired, and especially when compared with the diverse treatments employed throughout medical history that might strike some people as equally of the sorts of things that are not treatments. The recent uptake of “social prescribing” [80], whereby healthcare practitioners refer patients to community programs to improve their health, and which includes things like befriending, cooking courses, and theater outings, lends testament to the idea that more than the standard medical means of drugs and surgery are valid ways of potentially treating medical conditions.
Some philosophers indeed recognize lifestyle and social interventions as falling within the remit of the medical [81, p. 271]. Sholl, for example, argues that the conflation of pathologization with medicalization entails a problematic distortion of the varieties of medical practice. In explicating the distinction, he ties pathologization to disease and medicalization to treatment, underscoring treatment’s conceptual distinctness from disease [81]. Consequently, he recognizes treatment’s expansive extension, since treatment need not imply pathology, and vice versa. Medicalization can be seen as a neutral term [82] and while it may seem that distinguishing between good and bad forms of medicalization could offer a way for determining what is (i.e., good forms) and is not (i.e., bad forms) a medical condition, the literature on medicalization does not strike at the heart of what it means to be a medical condition in the first place.Footnote 21 My above analysis on the targeting of specific medical conditions thus attempts to fill an important gap in the literature.
The ubiquity of treatments is partly underscored by incidental treatment. This is how people, in retrospect, could be seen as being treated without their awareness. For example, a person whose diet consists of leafy vegetables and citrus fruits could be incidentally treating a folic acid deficiency that causes an anemia of which they are unaware. Even among non-human animals, plants with pharmacological properties are naturally sought out [83]. There are treatments that are (or that contain aspects of) quotidian features of life and are emblematic of lifestyle interventions as treatment, whether involving diet, exercise, brushing one’s teeth, components of psychotherapy and the expressive arts therapies, and innumerable other facets of life. Not conceiving of such features as treatments could be an anthropological oddity, a reflection of a society inured to a certain way of doling out medicine and caring for the sick. Psychotherapy, for example, is commonly considered a medical treatment that comprises multiple components such as positive regard from a therapist, expectations of benefit, talking and being listened to, and empathetic support and encouragement. These are among the common factors of psychotherapy, which have even been shown to contribute more to the treatment effect of psychotherapy than factors specific to or characteristic of individual types of psychotherapy [84]. Conceivably, such components are encountered throughout daily life, with some components sometimes clustering with others, with the same person or different people, in varied locations, and usually without the exchange of money or even awareness that one may be engaging in medical treatment. Why though, in hindsight, are the empathetic glance of a parent, the kind words of a stranger, the insightful analysis of a friend, or the positive expectations of engaging in a social activity any less medical or less of a treatment than trains of similar moments structured in the confines of a 50-minute session delivered by a licensed professional? Alternatively, if these features, or psychotherapy itself, target a DSM mental disorder that is not actually a medical condition, then none would be treatments in such cases.
In holding an important place for incidental treatment and the ubiquity of treatments, my account could be charged with admitting too much and therefore being vacuous. In a word, if everything is potentially a treatment, then it is not clear what are not treatments or how treatments can be clearly and unambiguously identified. However, the desiderata explicated above are meant to prevent this.
A simple typology of treatments
One potential limitation of widening the ambit of what can be considered a treatment is that there is no end or could be no end to the “specificity” of treatments. For example, that riding on a bus while reading a David Sedaris novel, but only on a sunny day, and only after having eaten a pastrami on rye with a Dr. Brown’s Black Cherry Soda, could be a treatment is farcical in direct proportion to the extent to which it is idiosyncratic. Psychotherapy administered using manuals is another example of this type of (putative) treatment in that a highly specific protocol is followed in delivering it. Specificity is not a well-defined construct, but I use it here to refer to a treatment’s complexity (as in complex interventions; see [87]). As mentioned above in discussing discreteness and standardization, multiple factors (besides effectiveness, and including normative factors) determine how a treatment should be characterized. The “pastrami treatment” — or any other putative treatment for that matter — is thus overly specific only to the extent that its desired characterization contains some features or activities that are irrelevantFootnote 22 to that characterization.
In contrast with the specificity of the “pastrami treatment,” certain types of immunotherapies that rely on a patient’s own cells are idiosyncratic in a different sense. The individualized–generic continuum reflects the degree to which a treatment relies on individual, personalized features of a patient. A generic treatment can be described as one that could be “taken off the shelf” and not require any fitting to the patient at hand, whereas an individualized treatment is closely fitted to personal characteristics of a patient, like bespoke patient-specific devices [26].
There are highly individualized treatments (e.g., the immunotherapy) and highly specific putative treatments (e.g., the “pastrami treatment”), as well as combinations of the two. Other possibilities exist, shown in the following 2 × 2 matrix representing a multidimensional continuum of treatment types, which gives representative examples of extreme versions of each type.Footnote 23
Individualized and specific (e.g., a particular art therapy protocol) | Generic and specific (e.g., the “pastrami treatment”; manualized psychotherapy) |
Individualized and non-specific (e.g., T-cell immunotherapy) | Generic and non-specific (e.g., aspirin) |
Some treatments can shift categories, such as the “pastrami treatment” becoming “individualized and specific” if the sandwich could only come from one’s favorite childhood delicatessen. At the same time, some treatments could be said to reside in the borderlands between being generic and being individualized. Consider for example how psychotherapists are responsive to their clients’ individual features [88], yet at the same time could be said to offer generic (putative) treatments that could apply to any person, regardless of their features.
What I have presented of this typology is only a sketch that could benefit from further development. The typology is not mutually exclusive with other classification systems. What may make the typology useful is being able to identify which type a particular treatment is. This could help to better understand the nature of that treatment to make it as specific as it needs to be to accomplish the goals it has. A diminution of specificity could reduce ambiguity and therefore aid in the standardization of treatments by facilitating how they can be distinguished from other treatments.
Conclusion
In this article I have provided intersecting accounts of medical treatment and medical conditions. A salient aspect of my account of medical treatment is the ease with which treatmenthood can be established, subject to three rather undemanding desiderata. One of these is that a treatment should target a medical condition. Although demarcating a condition as being “medical” can have the perlocutionary effect of indicating a degree of importance or seriousness that can represent a call to action, on my account there is no ipso facto implication that a medical condition should be treated. Similarly, something’s being a treatment on my account in no way determines whether it is a good, safe, effective, desirable, socially responsible/ethical, or feasibly administered treatment, or whether it is one that should be investigated through medical research, used clinically, or reimbursed by health insurance. Value judgments are required to make these determinations, the details of which are beyond the scope of this article.
Although the account of treatment I offer here is undoubtedly incomplete and subject to shortcomings, it is meant to encompass all treatments past, present, and future. My account is complementary to Fuller’s [85] account of preventive and curative medical interventions. By not strongly circumscribing the range of possible treatments, my account could quell a therapeutic hegemony and sociopolitical subversion of what should or should not be considered “proper” treatments. Yet, on my account, some of what are commonly thought of as medical treatments — such as psychotherapy and paroxetine hydrochloride — would not be treatments for those conditions they target that are not actually medical conditions. For example, while changing a child’s schooling could be considered a nonmedical approach to addressing the behaviors that could have led to a diagnosis of ADHD, if ADHD is not actually a medical condition (not even one of the non-pathological medical conditions I considered in the above discussion on symptoms), then administering pharmaceuticals to this child would also not constitute medical treatment. This is not to say that anything in my account prevents typically medical means (e.g., drugs) from being used to address nonmedical conditions, including any DSM mental disorders that are not actually medical conditions. Whether such means should be used, though, is a different story, one underwritten by considerations such as desert, responsibility, risk, and anticipated benefit.
Nonetheless, my account of treatment is responsive to individuals’ hopes and diverse conceptions of what could cure and offer succor for the various medical ailments that afflict themselves and others. Although broad conceptions of treatment may risk rampant treatment proliferation, it is not clear what the downside of this is. Not all treatments used by individuals and recognized as treatments need to be studied or used on a population level. Moreover, a great bulwark against bogus and ineffective treatments is a strong theory of treatment effectiveness. To this I mirror the words of Fuller [89, p. 646] and the spirit of Stegenga [90] in suggesting that what might also be needed is an equally strong dose of therapeutic humility.
Change history
09 September 2023
Table format and titles in reference section has been corrected.
Notes
My target in this article is medical treatment, not treatment in general. For simplicity, henceforth I simply mostly refer to “treatment”.
Currently, as fecal microbiota transplantation for recurrent Clostridium difficile infection.
In a work in progress, I answer this affirmatively. The implications of this — for characterizing placebos and placebo effects and establishing treatment effectiveness — are too complex to go into here, which is why I address it in another work. Nonetheless, such work is underscored by the importance that placebos-being-treatments holds for philosophical accounts of placebos. Importantly, for the present work, what have been used as placebos in clinical practice and clinical trials satisfy the “treatmenthood” desiderata I outline in the section on medical treatment desiderata.
None of which should be taken to mean that I think there is a clear-cut individuation of treatments, but rather that certain classifications are useful for certain purposes.
This approach, for example, is taken by Stegenga [13] (see also the section on pathology in the present article). This is different from requiring the possibility of effectiveness (discussed later), or something’s being effective offering presumptive evidence of treatmenthood. Knowing that a treatment is effective could be used as a meta-heuristic in cases of contested treatmenthood; i.e., something’s being effective could offer support for it being a treatment.
Which can especially be the case when safety is subsumed under effectiveness, a situation illustrated by a medical advisory board meeting I once attended where a distinguished oncologist, in full view of representatives of the pharmaceutical company that sponsored the meeting, along with a room full of other oncologists, declared the company’s drug to be poison, despite the median one month extra survival it was shown to provide in clinical studies, though at the expense of intolerable side effects. Granted, this was a view not shared by the pharmaceutical company, who believed their drug to be effective because of the improvement in survival.
Elaborating on these factors or other relevant factors and how they interact to differentiate specific treatments is beyond the scope of this article but may be a fruitful area for future research.
Although it may seem like it, this does not make treatmenthood dependent on treatment effectiveness because a poorly characterized treatment with respect to treatment effectiveness can still be a treatment.
A possibility borne out by a study conducted under the open–hidden paradigm which found the effectiveness of morphineo to be significantly higher than that of morphinec [27].
I do not draw a distinction between illicit and licit drugs with respect to whether they can be treatments (and I thus reject the legality of something as a criterion of treatmenthood). I recognize that some people might not consider use of cocaine for its psychoactive properties to have any legitimate medical purpose, even independent of cocaine’s high risk of adverse events.
I use here the terminology “medical condition” instead of “clinical condition” to avoid confusion with [32] where I list in my chart of clinical conditions what are better thought of as clinical conditions and clinical activities (such as blood donation), and which could imply that clinical conditions are characterized by their being addressed by clinicians, whereas I mean for “medical condition” to have no such necessary implication.
Medical treatment could be considered a proper subset of medical interventions, the latter of which include diagnostic interventions (such as screening programs), public health interventions (such as water fluoridation), and medical procedures/activities (such as autopsy, euthanasia, cosmetic surgery, and interventions to improve sports performance). The feature distinguishing medical treatments from public health interventions appears to be that medical treatments are directed at the individual level whereas public health interventions are directed at the population level. Either can involve changing the social context. For medical treatments, however, a description on the individual level is needed. A public health intervention could accordingly be rewritten as an individual-level medical intervention. This description might vary depending on the person (see the section “Discreteness and standardization”). For example, fluoridation of a city’s water supply is a public health intervention that operationalized as an individual-level intervention could involve for one person drinking the water whereas for another person simply showering with it. Only the former usage would constitute medical treatment for caries.
One could, by contrast, define medical conditions on the basis of what is potentially medically treatable (e.g., as Cooper [33] does with respect to defining disease). The onus then arises for defining treatment and medicine. Cooper [33, p. 278] offers the possibility of medicine being “the science practiced by doctors and other medical personnel,” and recognizes that it can be indeterminate as to what a medical treatment is.
As Stegenga [38, p. 11] wryly notes, “Not all forms of suffering are in the domain of medicine. One need only consider the suffering caused by hunger or climbing high mountains or listening to country music.”
This includes disease, environmental trauma (e.g., heatstroke, altitude sickness), injury, and poisoning.
In personal communication, Stegenga has confirmed this accurately characterizes his view. See also the earlier section on effectiveness.
As Aquino ([63], p. 7) writes “…dealing with a complaint of leg pain requires a medical understanding that can distinguish a normal response to physical exertion from a pathological condition. If the leg pain is pathological, adequate medical knowledge should enable doctors to diagnose and establish the cause, severity and complications of the condition. In cases when leg pain is not pathological, such as when it is caused by muscle fatigue after prolonged physical activity, a clinician offers reassurance and may decide that further medical investigation is not warranted. The clinical process of disease determination then involves a clinician’s use of her medical knowledge to distinguish the normal from the pathological.”
I have argued [15] that a similar problem is also encountered with the Russo–Williamson thesis. More work is needed to identify what the criteria should be that demarcate a mechanism as being “plausible.”
Especially since, for some, I do not mention the treatment target. Also, some I merely describe as nouns, whereas all treatments involve doing something, even if as simple as being administered.
Fuller [85], for example, analyzes the concept of preventive and curative medical interventions using the concept of a medical condition. However, he admits [85, p. 14] that “[a]nalyzing a concept like ‘disease’ or ‘medical condition’ is a formidable (and frequently faced) problem of its own that I will not attempt here.” He instead examines medical interventions via what he views as representative examples (and like me he views medical conditions as the more general category than diseases). Authors in the medicalization literature are also aware of the importance of this question; as Sadler et al. [86, pp. 412–413] write, “whether a human problem is, or is not, metaphysically (‘‘really’’) medical would be a question at the core of a philosophy of medicalization.”
However relevancy is determined, a matter I will not address here, other than to note that while effectiveness is typically how relevancy is determined, establishing effectiveness or its appropriate standard for any given treatment is no straightforward matter [14, 15]. Additionally, some healing traditions even determine relevancy on the basis of religious saliency. For highly specific treatments, relevancy may be a function of certain institutional features involving how the treatment is conceived and administered.
I am aware that “individualized” and “specific” have similar denotations, but for lack of better terms I use them here idiosyncratically.
References
Shapiro, A. K., and E. Shapiro. 1997. The Powerful Placebo: From Ancient Priest to Modern Physician. Baltimore: Johns Hopkins University Press.
Brody, H., and D. B. Waters. 1980. Diagnosis is treatment. The Journal of Family Practice 10 (3): 445–449.
Antonioli, C., and M. A. Reveley. 2005. Randomised controlled trial of animal facilitated therapy with dolphins in the treatment of depression. BMJ 331 (7527): 1231. https://doi.org/10.1136/bmj.331.7527.1231.
Steel, D., and Ş. Tekin. 2021. Can treatment for substance use disorder prescribe the same substance as that used? The case of injectable opioid agonist treatment. Kennedy Institute of Ethics Journal 31: 271–301. https://doi.org/10.1353/ken.2021.0022.
Schwartz, P. H. 2017. Progress in defining disease: improved approaches and increased impact. The Journal of Medicine and Philosophy 42 (4): 485–502. https://doi.org/10.1093/jmp/jhx012.
Evans, D. 2002. Pain, evolution, and the placebo response. Behavioral and Brain Sciences 25 (4): 459–460. https://doi.org/10.1017/S0140525X02260082.
Sullivan, M. D. 1993. Placebo controls and epistemic control in orthodox medicine. The Journal of Medicine and Philosophy 18 (2): 213–231. https://doi.org/10.1093/jmp/18.2.213.
Dalbosco, C. A., F. C. Filho, R. Maraschin, and L. O. Cezar. 2020. Medical discernment and dialogical praxis: treatment as healing oneself. Medicine, Health Care and Philosophy 23 (2): 205–214. https://doi.org/10.1007/s11019-020-09941-8.
Jiang, W.-Y. 2005. Therapeutic wisdom in traditional Chinese medicine: a perspective from modern science. Trends in Pharmacological Sciences 26 (11): 558–563. https://doi.org/10.1016/j.tips.2005.09.006.
Caspi, O., and R. R. Bootzin. 2002. Evaluating how placebos produce change: logical and causal traps and understanding cognitive explanatory mechanisms. Evaluation & the Health Professions 25 (4): 436–464. https://doi.org/10.1177/0163278702238056.
Miller, F. G., L. Colloca, and T. J. Kaptchuk. 2009. The placebo effect: illness and interpersonal healing. Perspectives in Biology and Medicine 52 (4): 518–539. https://doi.org/10.1353/pbm.0.0115.
Moerman, D. E. 2002. Meaning, Medicine, and the “Placebo Effect.” Cambridge University Press.
Stegenga, J. 2015. Effectiveness of medical interventions. Studies in History and Philosophy of Science Part C: Studies in History and Philosophy of Biological and Biomedical Sciences 54: 34–44. https://doi.org/10.1016/j.shpsc.2015.06.005.
Tresker, S. 2022. Treatment effectiveness, generalizability, and the explanatory/pragmatic-trial distinction. Synthese 200: 316. https://doi.org/10.1007/s11229-022-03517-0.
Tresker, S. 2022. Treatment effectiveness and the Russo–Williamson thesis, EBM+, and Bradford Hill’s viewpoints. International Studies in the Philosophy of Science 34 (3): 131–158. https://doi.org/10.1080/02698595.2022.2054396.
Doust, J., and C. Del Mar. 2004. Why do doctors use treatments that do not work? BMJ 328 (7438): 474–475. https://doi.org/10.1136/bmj.328.7438.474.
Grünbaum, A. 1986. The placebo concept in medicine and psychiatry. Psychological Medicine 16 (1): 19–38. https://doi.org/10.1017/S0033291700002506.
Holman, B. 2015. Why most sugar pills are not placebos. Philosophy of Science 82 (5): 1330–1343. https://doi.org/10.1086/683817.
Howick, J. 2017. The relativity of ‘placebos’: defending a modified version of Grünbaum’s definition. Synthese 194 (4): 1363–1396. https://doi.org/10.1007/s11229-015-1001-0.
Friesen, P. 2020. Towards an account of the placebo effect: a critical evaluation alongside current evidence. Biology & Philosophy 35 (1): 11. https://doi.org/10.1007/s10539-019-9733-8.
Kaptchuk, T. J., and F. G. Miller. 2015. Placebo effects in medicine. New England Journal of Medicine 373 (1): 8–9. https://doi.org/10.1056/NEJMp1504023.
Walach, H. 2011. Placebo controls: historical, methodological and general aspects. Philosophical Transactions of the Royal Society B: Biological Sciences 366 (1572): 1870–1878. https://doi.org/10.1098/rstb.2010.0401.
Blease, C. 2018. Consensus in placebo studies: lessons from the philosophy of science. Perspectives in Biology and Medicine 61 (3): 412–429. https://doi.org/10.1353/pbm.2018.0053.
Blease, C. 2018. Psychotherapy and placebos: manifesto for conceptual clarity. Frontiers in Psychiatry 9. https://doi.org/10.3389/fpsyt.2018.00379.
Kreek, M. J. 2000. Methadone-related opioid agonist pharmacotherapy for heroin addiction. Annals of the New York Academy of Science 909: 186–216. https://doi.org/10.1111/j.1749-6632.2000.tb06683.x.
Walker, M. J. 2018. Patient-specific devices and population-level evidence: evaluating therapeutic interventions with inherent variation. Medicine, Health Care and Philosophy 21 (3): 335–345. https://doi.org/10.1007/s11019-017-9807-9.
Colloca, L., L. Lopiano, M. Lanotte, and F. Benedetti. 2004. Overt versus covert treatment for pain, anxiety, and Parkinson’s disease. The Lancet Neurology 3 (11): 679–684. https://doi.org/10.1016/S1474-4422(04)00908-1.
Peiris, N., M. Blasini, T. Wright, and L. Colloca. 2018. The placebo phenomenon: a narrow focus on psychological models. Perspectives in Biology and Medicine 61 (3): 388–400. https://doi.org/10.1353/pbm.2018.0051.
Branthwaite, A., and P. Cooper. 1981. Analgesic effects of branding in treatment of headaches. British Medical Journal (Clinical Research Edition) 282 (6276): 1576–1578. https://doi.org/10.1136/bmj.282.6276.1576.
Kaptchuk, T. J., J. M. Kelley, L. A. Conboy, R. B. Davis, C. E. Kerr, E. E. Jacobson, I. Kirsch, R. N. Schyner, B. H. Nam, L. T. Nguyen, M. Park, A. L. Rivers, C. McManus, E. Kokkotou, D. A. Drossman, P. Goldman, and A. J. Lembo. 2008. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ 336 (7651): 999–1003. https://doi.org/10.1016/j.dza.2010.04.011.
Kukla, Q. 2014. Medicalization, “normal function,” and the definition of health. In: The Routledge Companion to Bioethics, eds. J. D. Arras, E. Fenton, and Q. Kukla. Milton Park: Routledge Handbooks Online.
Tresker, S. 2020. Theoretical and clinical disease and the biostatistical theory. Studies in History and Philosophy of Science Part C: Studies in History and Philosophy of Biological and Biomedical Sciences 82: 101249. https://doi.org/10.1016/j.shpsc.2019.101249.
Cooper, R. 2002. Disease. Studies in History and Philosophy of Science Part C: Studies in History and Philosophy of Biological and Biomedical Sciences 33: 263–282. https://doi.org/10.1016/S0039-3681(02)00018-3.
Boorse, C. 2016. Goals of medicine. In Naturalism in the Philosophy of Health. History, Philosophy and Theory of the Life Sciences, ed. É. Giroux. Cham: Springer. https://doi.org/10.1007/978-3-319-29091-1_9.
Miettinen, O. S., and K. M. Flegel. 2003. Elementary concepts of medicine: V. Disease: one of the main subtypes of illness. Journal of Evaluation in Clinical Practice 9 (3): 321–323. https://doi.org/10.1046/j.1365-2753.2003.00418.x.
Boorse, C. 1997. A rebuttal on health. In What is Disease?, eds. J. M. Humber, and R. F. Almeder. Totowa, NJ: Humana Press. https://doi.org/10.1007/978-1-59259-451-1_1.
Aronowitz, R. A. 2009. The converged experience of risk and disease. The Milbank Quarterly 87: 417–442. https://doi.org/10.1111/j.1468-0009.2009.00563.x.
Stegenga, J. 2021. Medicalization of sexual desire. European Journal of Analytic Philosophy 17 (2): S5–34. https://doi.org/10.31820/ejap.17.3.4.
Schwartz, P. H. 2007. Defining dysfunction: natural selection, design, and drawing a line. Philosophy of Science 74 (3): 364–385. https://doi.org/10.1086/521970.
Boorse, C. 1977. Health as a theoretical concept. Philosophy of Science 44: 542–573. https://doi.org/10.1086/288768.
Boorse, C. 2014. A second rebuttal on health. The Journal of Medicine and Philosophy 39 (6): 683–724. https://doi.org/10.1093/jmp/jhu035.
Boorse, C. 2011. Concepts of health and disease. In: Handbook of the Philosophy of Science: Philosophy of Medicine, ed. F. Gifford, 13–64. Amsterdam: Elsevier.
Cresswell, M. 2008. Szasz and his interlocutors: reconsidering Thomas Szasz’s “Myth of Mental Illness” thesis. Journal for the Theory of Social Behaviour 38: 23–44. https://doi.org/10.1111/j.1468-5914.2008.00359.x.
Fuller, J. 2018. What are chronic diseases? Synthese 195 (7): 3197–3220. https://doi.org/10.1007/s11229-017-1368-1.
Tresker, S. 2020. A typology of clinical conditions. Studies in History and Philosophy of Science Part C: Studies in History and Philosophy of Biological and Biomedical Sciences 83: 101291. https://doi.org/10.1016/j.shpsc.2020.101291.
Schwartz, P. H. 2008. Risk and disease. Perspectives in Biology and Medicine 51 (3): 320–334. https://doi.org/10.1353/pbm.0.0027.
Schramme, T. 2007. The significance of the concept of disease for justice in health care. Theoretical Medicine and Bioethics 28 (2): 121–135. https://doi.org/10.1007/s11017-007-9031-3.
Insel, T. R., and B. N. Cuthbert. 2015. Medicine. Brain disorders? Precisely. Science 348 (6234): 499–500. https://doi.org/10.1126/science.aab2358.
White, P. D., H. Rickards, and A. Z. Zeman. 2012. Time to end the distinction between mental and neurological illnesses. BMJ 344: e3454. https://doi.org/10.1136/bmj.e3454.
Boorse, C. 1976. What a theory of mental health should be. Journal for the Theory of Social Behaviour 6: 61–84. https://doi.org/10.1111/j.1468-5914.1976.tb00359.x.
Graham, G. 2013. Ordering disorder: mental disorder, brain disorder, and therapeutic intervention. In: The Oxford Handbook of Philosophy and Psychiatry. Edited by K. W. M. Fulford, M. Davies, R. G. T. Gipps, G. Graham, J. Z. Sadler, G. Stanghellini and T. Thornton. Oxford University Press. https://doi.org/10.1093/oxfordhb/9780199579563.013.0032.
Jefferson, A. 2020. What does it take to be a brain disorder? Synthese 197: 249–262. https://doi.org/10.1007/s11229-018-1784-x.
Papineau, D. 1994. Mental disorder, illness and biological disfunction. Royal Institute of Philosophy Supplement 37: 73–82. https://doi.org/10.1017/S135824610000998X.
Schramme, T. 2013. On the autonomy of the concept of disease in psychiatry. Frontiers in Psychology 4: 457. https://doi.org/10.3389/fpsyg.2013.00457.
Cosmides, L., and J. Tooby. 1999. Toward an evolutionary taxonomy of treatable conditions. Journal of Abnormal Psychology 108: 453–464. https://doi.org/10.1037/0021-843x.108.3.453.
Boorse, C. 2023. Boundaries of disease: disease and risk. Medical Research Archives 11 (4). https://doi.org/10.18103/mra.v11i4.3599.
Horwitz, A. V., and J. C. Wakefield. 2007. The Loss of Sadness: How Psychiatry Transformed Normal Sorrow into Depressive Disorder. Oxford: Oxford University Press.
Szasz, T. S. 1960. The myth of mental illness. American Psychologist 15(2): 113–118. https://doi.org/10.1037/h0046535.
Moncrieff, J. 2020. It was the brain tumor that done it!”: Szasz and Wittgenstein on the importance of distinguishing disease from behavior and implications for the nature of mental disorder. Philosophy Psychiatry & Psychology 27 (2): 169–181. https://doi.org/10.1353/ppp.2020.0017.
O’Leary, D. 2021. Medicine’s metaphysical morass: how confusion about dualism threatens public health. Synthese 199 (1–2): 1977–2005. https://doi.org/10.1007/s11229-020-02869-9.
O’Leary, D. 2018. Why bioethics should be concerned with medically unexplained symptoms. The American Journal of Bioethics 18 (5): 6–15. https://doi.org/10.1080/15265161.2018.1445312.
Fainzang, S. 2013. The other side of medicalization: self-medicalization and self-medication. Culture Medicine and Psychiatry 37 (3): 488–504. https://doi.org/10.1007/s11013-013-9330-2.
Aquino, Y. S. J. 2020. Is ugliness a pathology? An ethical critique of the therapeuticalization of cosmetic surgery. Bioethics 34 (4): 431–441. https://doi.org/10.1111/bioe.12721.
O’Leary, D. 2019. Ethical classification of ME/CFS in the United Kingdom. Bioethics 33 (6): 716–722. https://doi.org/10.1111/bioe.12559.
Wakefield, J. C. 1992. The concept of mental disorder: on the boundary between biological facts and social values. American Psychologist 47 (3): 373–388. https://doi.org/10.1037//0003-066x.47.3.373.
Wakefield, J. C. 1992. Disorder as harmful dysfunction: a conceptual critique of DSM-III-R’s definition of mental disorder. Psychological Review 99 (2): 232–247. https://doi.org/10.1037/0033-295x.99.2.232.
Wakefield, J. C. 2021. Defining Mental Disorder: Jerome Wakefield and His Critics, eds. L. Faucher, and D. Forest. Cambridge: The MIT Press. https://doi.org/10.7551/mitpress/9949.001.0001.
Schramme, T. 2010. Can we define mental disorder by using the criterion of mental dysfunction? Theoretical Medicine and Bioethics 31 (1): 35–47. https://doi.org/10.1007/s11017-010-9136-y.
Kingma, E. 2013. Naturalist accounts of mental disorder. In: The Oxford Handbook of Philosophy and Psychiatry. Edited by K. W. M. Fulford, M. Davies, R. G. T. Gipps, G. Graham, J. Z. Sadler, G. Stanghellini and T. Thornton. Oxford University Press. https://doi.org/10.1093/oxfordhb/9780199579563.013.0025.
Brülde, B. 2003. The concept of mental disorder. Philosophical Communications Web Series; #29. https://gupea.ub.gu.se/bitstream/handle/2077/19471/gupea_2077_19471_1.pdf?sequence=1&isAllowed=y. Accessed 14 August 2023.
Beauvais, F. 2016. “Memory of water” without water: modeling of Benveniste’s experiments with a personalist interpretation of probability. Axiomathes 26: 329–345. https://doi.org/10.1007/s10516-015-9279-6.
Grimes, D. R. 2012. Proposed mechanisms for homeopathy are physically impossible. Focus on Alternative and Complementary Therapies 17: 149–155. https://doi.org/10.1111/j.2042-7166.2012.01162.x.
Maddox, J., and J. Randi, W. Stewart. 1988. “High-dilution” experiments a delusion. Nature 334: 287–290. https://doi.org/10.1038/334287a0.
Sehon, S., and D. Stanley. 2010. Evidence and simplicity: why we should reject homeopathy. Journal of Evaluation in Clinical Practice 16: 276–281. https://doi.org/10.1111/j.1365-2753.2010.01384.x.
Smith, K. 2012. Against homeopathy–a utilitarian perspective. Bioethics 26: 398–409. https://doi.org/10.1111/j.1467-8519.2010.01876.x.
Smith, K. 2012. Homeopathy is unscientific and unethical. Bioethics 26: 508–512. https://doi.org/10.1111/j.1467-8519.2011.01956.x.
Teixeira, J. 2007. Can water possibly have a memory? A sceptical view. Homeopathy: The Journal of the Faculty of Homeopathy 96: 158–162. https://doi.org/10.1016/j.homp.2007.05.001.
Benedetti, F. 2009. Placebo Effects: Understanding the Mechanisms in Health and Disease. Oxford: Oxford University Press.
Jopling, D. A. 2013. Placebo effects in psychiatry and psychotherapy. In: The Oxford Handbook of Philosophy and Psychiatry. Edited by K. W. M. Fulford, M. Davies, R. G. T. Gipps, G. Graham, J. Z. Sadler, G. Stanghellini and T. Thornton. Oxford University Press. https://doi.org/10.1093/oxfordhb/9780199579563.013.0070.
Bickerdike, L., A. Booth, P. M. Wilson, K. Farley, and K. Wright. 2017. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. British Medical Journal Open 7 (4): e013384. https://doi.org/10.1136/bmjopen-2016-013384.
Sholl, J. 2017. The muddle of medicalization: pathologizing or medicalizing? Theoretical Medicine and Bioethics 38 (4): 265–278. https://doi.org/10.1007/s11017-017-9414-z.
Busfield, J. 2017. The concept of medicalisation reassessed. Sociology of Health & Illness 39 (5): 759–774. https://doi.org/10.1111/1467-9566.12538.
Costa-Neto, E. M. 2012. Zoopharmacognosy, the self-medication behavior of animals. Interfaces Científicas – Saúde e Ambiente 1 (1): 61–72. https://doi.org/10.17564/2316-3798.2012v1n1p61-72.
Wampold, B. E. 2015. How important are the common factors in psychotherapy? An update. World Psychiatry 14 (3): 270–277. https://doi.org/10.1002/wps.20238.
Fuller, J. 2022. Preventive and curative medical interventions. Synthese 200: 61. https://doi.org/10.1007/s11229-022-03579-0.
Sadler, J. Z., F. Jotterand, S. C. Lee, and S. Inrig. 2009. Can medicalization be good? Situating medicalization within bioethics. Theoretical Medicine and Bioethics 30 (6): 411–425. https://doi.org/10.1007/s11017-009-9122-4.
Skivington, K., L. Matthews, and S. A. Simpson et al. 2021. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 374: n2061. https://doi.org/10.1136/bmj.n2061.
Stiles, W. B. 2009. Responsiveness as an obstacle for psychotherapy outcome research: it’s worse than you think. Clinical Psychology: Science and Practice 16: 86–91. https://doi.org/10.1111/j.1468-2850.2009.01148.x.
Fuller, J. 2013. Rationality and the generalization of randomized controlled trial evidence. Journal of Evaluation in Clinical Practice 19 (4): 644–647. https://doi.org/10.1111/jep.12021.
Stegenga, J. 2018. Medical Nihilism. Oxford: Oxford University Press.
Acknowledgements
Many thanks to Christopher Boorse, Andreas De Block, Bert Leuridan, Diane O’Leary, Jonathan Sholl, and Jacob Stegenga, plus two anonymous reviewers for this journal, for helpful comments on earlier drafts of this paper. The author was supported by the Fonds Voor Wetenschappelijk Onderzoek – Vlaanderen (FWO; Research Foundation – Flanders; 1130819N) during part of the writing of this paper and is grateful for their support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tresker, S. An account of medical treatment, with a preliminary account of medical conditions. Theor Med Bioeth 44, 607–633 (2023). https://doi.org/10.1007/s11017-023-09641-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11017-023-09641-3