Abstract
Neuroinflammation is a consequence of overeating and may predispose to the development of cognitive decline and neurological disorders. This study aimed to evaluate the impact of omega-3 supplementation on memory and neuroinflammatory markers in rats fed a high-fat diet. Male Wistar rats were divided into four groups: standard diet (SD); standard diet + omega-3 (SD + O); high fat diet (HFD); and high fat diet + omega-3 (HFD + O). Diet administration was performed for 20 weeks and omega-3 supplementation started at the 16th week. HFD significantly increased body weight, while omega-3 supplementation did not modify the total weight gain. However, animals from the HFD + O group showed a lower level of visceral fat along with an improvement in insulin sensitivity following HFD. Thus, our results demonstrate a beneficial metabolic role of omega-3 following HFD. On the other hand, HFD animals presented an impairment in object recognition memory, which was not recovered by omega-3. In addition, there was an increase in GFAP-positive cells in the cerebral cortex of the HFD group, showing that omega-3 supplementation can be effective to decrease astrogliosis. However, no differences in GFAP number of cells were found in the hippocampus. We also demonstrated a significant increase in gene expression of pro-inflammatory cytokines IL-6 and TNF-α in cerebral cortex of the HFD group, reinforcing the anti-inflammatory role of this family of fatty acids. In summary, omega-3 supplementation was not sufficient to reverse the memory deficit caused by HFD, although it played an important role in reducing the neuroinflammatory profile. Therefore, omega-3 fatty acids may play an important role in the central nervous system, preventing the progression of neuroinflammation in obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obesity has increased over the last decades, making it a major public health problem worldwide. An imbalance between energy intake and energy expenditure leads to the overproduction of body fat, which may cause various metabolic disorders (Hossain et al. 2007; Mello et al. 2006). The association between this excess of body fat and cardiovascular diseases (Aghamohammadzadeh and Heagerty 2012; Kenchaiah et al. 2004; Lotufo 2000), some types of cancers (Demark-Wahnefried et al. 2012) and type II diabetes mellitus is well known (Wannamethee and Shaper 1999). Besides these classical comorbidities, there is paramount evidence of the relationship between obesity and neurological dysfunction, including neuropsychiatric and neurodegenerative diseases (Calsolaro and Edison 2016; Morales et al. 2014).
An important feature of obesity is the chronic low-grade inflammation that occurs in metabolic tissues, especially in adipose tissue. This inflammatory state, named metainflammation, is the main cause of the maladaptative responses to obesity. The increased secretion of pro-inflammatory cytokines by adipose tissue, such as tumor necrosis factor-alpha (TNF-α), interleukin 6 (IL-6) and interleukin-1β (IL-1β), can inhibit insulin signaling (Bulló et al. 2007; Maury and Brichard 2010; Shah et al. 2008). Hence, the pro-inflammatory phenotype is associated with insulin resistance, and together, these features promote a widespread repercussion on the body systems. On the other hand, it has already been demonstrated that a reduction in body weight leads to the increased expression of anti-inflammatory adipokines concomitant with a decrease in insulin resistance and in the levels of pro-inflammatory cytokines (Shah et al. 2008). Thus, strategies to contribute to weight loss are highly beneficial.
Previous studies have shown that, in obesity, inflammation in the hypothalamus may contribute to the inappropriate regulation of energy metabolism (van de Sande-Lee and Velloso 2012). However, this pro-inflammatory activity is not limited to the hypothalamus, being propagated to other brain regions and affecting a variety of brain functions (Gregor and Hotamisligil 2011). In addition, obesity can increase susceptibility to the development of neurodegenerative diseases, and neuroinflammation is a potential causal factor of the dysregulation in the central nervous system (CNS) caused by overeating. It was shown that a high fat diet can lead to the excessive production of IL-6 by activated microglia and also cause the subsequent activation of astrocytes due to the stimulation of pro-inflammatory cytokines (Tapia-González et al. 2011). These neuroinflammatory responses are harmful, since these mechanisms are associated with neuropathological processes and neurodegeneration (Ransohoff et al. 2015). The long-term inflammation could have disastrous consequences in the CNS, such as the loss of synapses, affecting cognition and executive functions (Hein and O'Banion 2009; Kohman and Rhodes 2013). Throughout life, there is a natural decline in cognitive functions; however, some environmental factors, such as obesity, may accelerate this decline (Haan and Wallace 2004). The activation of inflammatory pathways may contribute to an impairment in learning and memory, which may be related to obesity, although the mechanisms by which this occurs are still poorly understood (Hwang et al. 2010; Pistell et al. 2010).
Polyunsaturated fatty acids (PUFAs) from the omega-3 family are well known to suppress neuroinflammation and reduce oxidative stress. These PUFAs have an anti-inflammatory action, reducing the synthesis of arachidonic acid derivatives (Bazan et al. 2012). Furthermore, in the CNS, they influence enzymatic activity, cell signaling, synaptic plasticity, and neurotransmitter release, and modulate cytokines that have neuromodulatory activity (Högyes et al. 2003). It has been suggested that the consumption of unsaturated fatty acids (UFAs) can positively affect spatial learning and memory and also decrease the negative effects of physiological stress on cognitive skills (Nemeth et al. 2015).
Despite the important action of omega-3 PUFAs as anti-inflammatory molecules and their role as neuroprotective compounds, previous studies have not evaluated whether omega-3 supplementation could reverse any outcome of a high-fat diet (HFD). The present study aimed to evaluate the impact of omega-3 on metabolic parameters (weigh gain, visceral adiposity, and insulin resistance), memory and neuroinflammatory markers following diet-induced obesity in rats.
Materials and methods
Animals
Male Wistar rats (n = 40) from the animal facility of the Universidade Federal de Ciências da Saúde de Porto Alegre were used. Animals had free access to standard rat chow and water until the age of 7 months. Rats were housed in plastic cages (2–3 rats per cage) under controlled temperature (22-24 °C) and light (12 h light/12 h dark cycle; lights on at 6:00 a.m.) conditions.
All efforts were made to minimize animal suffering and to reduce the number of animals used in the experiments, which were performed in accordance with the international laws for the care of laboratory animals. All procedures were approved by the Institutional Animal Care and Use Committee (UFCSPA, Brazil, protocol No. 261/14).
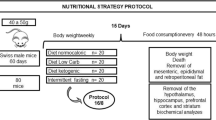
Diet and omega-3 administration
Seven month-old rats were divided into the following experimental groups: standard diet + vehicle (SD, n = 11); standard diet + omega-3 (SD + O, n = 8); high fat diet (HFD, n = 12) + vehicle; and high fat diet + omega-3 (HFD + O, n = 9). SD or HFD was administered for 20 weeks. Omega-3 supplementation was performed from the 16th to the 20th week of diet administration. Omega-3 was administered daily through gavage at a dose of 1 g/kg.
SD and SD + O groups were fed with Nuvilab® CR-1 standard rat chow (NUVITAL®, Curitiba, PR, Brazil) providing a total energy content of 3.4 kcal/g (63% carbohydrates, 26% protein, 11% fat). Animals from HFD and HFD + O groups were fed a high fat diet (Pragsoluções Biociências, Jaú, SP, Brazil) providing a total energy of 4.5 kcal/g (35.7% carbohydrate, 19.2% protein, 45.1% fat). Nutritional information was provided by manufacturers.
Object recognition test
In the last week of the diet administration, animals were submitted to the object recognition test. On the first day, rats were habituated in an acrylic box (40 cm × 40 cm) delimited by four walls with a height of 20 cm. Twenty-four hours after habituation, the training session was conducted. Animals were placed individually in the left rear quadrant of the box containing two different objects (A and B), and were allowed to freely explore them for 5 min. The retention test was performed 24 h after the training session. For the test, rats were individually reintroduced into the box where one of the objects presented during training was randomly replaced by a new object (C). Exploration of an object was defined as directing the nose towards the object at a distance less than 2 cm and/or when the animal touched the object with their nose (Ennaceur and Delacour 1988). The exploration time of the familiar and new objects were counted.
Tissue and blood collection
At the end of experimental time course, animals were decapitated for blood and tissue collection. Trunk blood was collected and, after centrifugation (1500 x g for 10 min at 4 °C), serum was separated and stored at −80 °C for later analysis. The brain was quickly removed and the right and left hemispheres were separated. The right hemisphere was put in a fixative solution for histological analyses. The cerebral cortex was dissected from the left hemisphere and quickly frozen in liquid nitrogen, as previously described in de Moura et al. (2015).
Blood analysis
Serum levels of glucose were analyzed using colorimetric kits (LabTest), according to the manufacturer’s instructions. An enzyme-linked immunosorbent assay (ELISA) commercial kit (Millipore) was used to analyze serum levels of insulin according to the manufacturer’s instructions.
HOMA index
The HOMA (homeostasis model assessment) index was used in order to quantify insulin resistance and beta cell function in the pancreas (Matthews et al. 1985). The index is calculated based on blood levels of glucose (mmol/L) and insulin (mU/L), using the following formula: (glucose blood levels x insulin blood levels) / 22.5 (Nattiv et al. 2007).
Immunohistochemical staining (IHC)
For immunohistochemistry, the left hemisphere of the brain was fixed in a zinc buffer solution (pH 7.4) for 48 h at room temperature. After this period, tissues were dehydrated, embedded in paraffin and sectioned (8 μm thick) using a microtome. Sections were treated with 3% hydrogen peroxide in 10% methanol for 30 min, washed in PBS for 30 min and incubated for 30 min in 3% normal goat serum in PBS containing 0.4% Triton X-100 (PBS-T). Then, sections were incubated for 48 h at 4 °C with a monoclonal anti-GFAP antibody (Millipore), diluted 1:750. Sections were incubated with anti-mouse IgG peroxidase-conjugated secondary antibody (Sigma), diluted 1:500 in PBS-T, for 90 min at room temperature. Immunoreaction was developed using a solution of 0.06% 3,3′-diaminobenzidine tetrahydrochloride (Sigma) and 0.005% hydrogen peroxide in PBS. Sections were counterstained with hematoxylin, dehydrated, and covered with Entellan (Merck) and coverslips. Digital images were acquired using a digital camera coupled to an Olympus BX-41 microscope using a 20× objective lens. The images were analyzed using ImageJ software (http://imagej.nih.gov/ij/). Three randomly selected fields were analyzed in six nonadjacent sections. Five animals per group were analyzed.
Molecular analyses
RNA extraction
RNA was extracted from the samples with Trizol (Invitrogen) which was used according to the manufacturer’s recommendations. The structures of the brain were homogenized in the presence of Trizol (1:5, v/v); aqueous phase was obtained by centrifugation (12,000 x g, 15 min). The RNA was precipitated with isopropanol, for 15 min at room temperature, followed by centrifugation at 12000 x g for 10 min. The pellets were resuspended in 0.1% DEPC-treated water. The concentration of total RNA was determined by measuring the optical density at 260 nm and purity of the RNA was evaluated on the basis of the 280 nm/260 nm ratio and electrophoresis on agarose gel (Langnaese et al. 2008).
cDNA synthesis
Total RNA (1 μg) was used as a template to synthesize cDNA. The RNA was incubated for 5 min at 60 °C with 1 μl oligo (dT) (0.5 μg/μl, Invitrogen), 1 μl 10 mM dNTP and DEPC-water to a final volume of 12 μl, and then for 1 min on ice. The following reagents were then added to a final volume of 19 μl: 4 μl of RT buffer (50 mM Tris-HCl, pH 8.3, 75 mM KCl, 3 mM MgCl2), 2 μl 0.1 M DTT, and 1 μl RNaseOUT (40 U/μl, Invitrogen). After 2 min incubation at 37 °C, 1 μl M-MLV-RT (200 U/μl; Invitrogen) was added and cDNA synthesis was carried out at 50 °C for 1 h. The reaction was inactivated by incubation at 70 °C for 15 min.
Real-time PCR (qPCR)
The expression of TNF-α, IL-6 and IL-10 was assessed. The housekeeping genes beta-actin (ActB) and Cyclophilin A (CypA), which have been shown to be stable in each brain area, were used as controls. Primer sequences are presented in Table 1. Amplification was carried out using 7.5 μL of SYBR Green PCR Master Mix (Applied Biosystems), 0.5 μL of forward and reverse primers (0.33 M each), 100 ng of cDNA and nuclease-free water, in a total volume of 15 μL. Reactions were performed in an optical 96-well plate, using a StepOnePlusTM thermocycler (Applied Biosystems). After an initial denaturation step at 95 °C for 10 min, amplification was performed in 40 cycles of denaturation at 95 °C for 30 s, annealing at 60 °C for 40 s and extension at 72 °C for 40 s. Amplification was followed by a melt curve analysis to confirm PCR product specificity. No signals were detected in the no-template controls. The experimental Ct (cycle threshold) was calculated using the algorithm enhancements provided by the equipment. All samples were run in duplicate and the mean value of each duplicate was used for all further calculations (Cook et al. 2010; Langnaese et al. 2008; Nelissen et al. 2010). The Ct value of each reaction was used to calculate the level of mRNA expression of each specific gene, after normalizing it to the expression of the control housekeeping gene (HKG) genes analyzed in the same reaction plate (Zimmermann-Peruzatto et al. 2016).
Statistical analyses
The data are expressed as mean ± SEM, except for weight gain, which was expressed as median and interquartile range. Data were analyzed by two-way ANOVA with Bonferroni post-hoc. Treatment and diet were used as factors for all ANOVA analyses, except for the object recognition test, in which experimental group and object (familiar and new) were used as factors. GraphPad Prism 5.0 was used for the statistical analyses. The significance level was set at p < 0.05.
Results
Animals fed a HFD gained significantly more weight over time than the animals fed a standard diet (diet effect, F 1,36 = 24.82, p < 0.0001). Omega-3 treatment (HFD + O group) did not revert this parameter and Bonferroni post-hoc showed that weight gain in the HFD + O group was not significantly lower than in the HFD group (p > 0.05). However, when visceral adiposity was evaluated, HFD caused a significant increase in visceral fat compared to standard diet (F 1,36 = 12.49, p = 0.001). Post-hoc analysis showed that omega-3 supplementation is able to prevent visceral adiposity in obese rats (p < 0.05). Glycemia and plasma insulin did not show any differences between groups (p > 0.05). Also, HOMA-IR, which provides an estimation of insulin resistance, did not show a diet effect as analyzed by two-way ANOVA (F 1,36 = 3.178, p > 0.05). However, post-hoc comparison between HFD and HFD + O showed a significant decrease in HOMA-IR after omega-3 supplementation (p < 0.05). This result proves that omega-3 PUFA improves insulin sensitivity in obesity (Table 2).
In order to assess whether HFD-induced obesity can interfere in animal recognition memory, object recognition test was performed. This task evaluates long-term memory through the ability to memorize and recognize both new and already known objects, 24 h after the training session (Caletti et al. 2015; Rossato et al. 2007). When comparing the total exploration time during the test session, there were no differences between groups (p > 0.05, Fig. 1A). However, when comparing the time exploring the familiar or new objects during the test session, a significant effect of object (familiar versus new) was found (F 1,42 = 4.932, p = 0.03). In the SD and SD + O groups, animals spent significantly more time exploring the new object during the test session (p < 0.05), which means that these rats recognized familiar and non-familiar objects. On the other hand, Bonferroni post-hoc showed that animals fed a HFD did not exhibit differences in the exploration time between familiar and new objects (p > 0.05) showing that obesity causes long-term memory impairment. These results also demonstrate that omega-3 did not exert a protective effect on the recognition memory (Fig.1B). We also analyzed the motor activity of the rats and found no differences between groups regarding the duration of locomotion (data not shown).
a. Total time spent exploring both objects during the object recognition test. No significant differences were found among experimental groups. b. Time spent exploring a familiar and a new object during the object recognition test. In SD and SD + O groups, animals spent more time exploring the new object during the retention session. HFD and HFD + O groups did not show differences in the exploration time of familiar and unfamiliar object. Omega-3 did not exert a protective effect on recognition memory. *p < 0.05, familiar versus new object. n = 7–8 for each group. Data are shown as mean ± SEM
GFAP was assessed by immunohistochemistry in order to determine the HFD effect on astrogliosis. GFAP is an astrocyte marker and GFAP labeling is widely used for the detection of tumors of astrocytic lineage (Liedtke et al. 1996), being the most widely used immunohistochemical marker for the identification of astrocytes (Catalani et al. 2002). Astrogliosis is represented by an increased number of GFAP-positive cells, which is found after several types of injury and it also indicates astrocytic activation and neuroinflammation (Kang et al. 2014; Sun et al. 2008; Toklu et al. 2017).
There was an increase in the number of GFAP-positive cells in the cerebral cortex, which is dependent on diet, showing that obesity leads to astrogliosis (F 1,60 = 9.369, p = 0.003) (Fig. 2). Omega-3 treatment decreased the number of GFAP-positive cells (treatment effect, F 1,60 = 8.550, p = 0.004) and Bonferroni post-hoc also showed that the number of positive cells in the HFD + O group was significantly lower than in the HFD group, which indicates that omega-3 may exert a protective role in the cerebral cortex by diminishing the activation state of astrocytes. Interestingly, there was no significant difference between groups in the number of GFAP-positive cell in the hippocampus (p > 0.05, Fig. 3).
GFAP immunoreactivity in the cerebral cortex. The number of GFAP-positive cells was significantly higher in HFD group as shown in the representative photomicrographs of GFAP immunoreactivity in the cerebral cortex (left panel, lower magnification; right panel, higher magnification). Graph shows the number of GFAP-positive cells from two to three random fields analyzed from each of six nonadjacent sections of the cerebral cortex. *p < 0.05 when compared with HFD + O group. n = 5 animals for each group. Data are shown as mean ± SEM
GFAP immunoreactivity in the hippocampus. There was no differences in the number of GFAP-positive cells among groups as shown in the representative photomicrographs of GFAP immunoreactivity in the hippocampus (left panel, lower magnification; right panel, higher magnification). Graph shows the number of GFAP-positive cells from two to three random fields analyzed from each of six nonadjacent sections of the cerebral cortex. n = 5 animals for each group. Data are shown as mean ± SEM
The gene expression of the neuroinflammatory markers TNF-α, IL-6 and IL-10 was also determined in the cerebral cortex. We found a significant increase of the pro-inflammatory cytokines TNF-α (diet effect, F 1,29 = 5.844, p = 0.02; treatment effect, F 1,29 = 10.76, p = 0.002) and IL-6 (treatment effect, F 1,21 = 4.794, p = 0.04) gene expression in the HFD group. Moreover, HFD + O rats exhibited a reduced level of TNF-α and IL-6 compared to HFD rats, demonstrating that omega-3 may control obesity-induced neuroinflammation. The anti-inflammatory cytokine IL-10 did not show differences in gene expression between groups (p > 0.05, Fig. 4).
Discussion
In the present study, we showed that omega-3 supplementation is able to reverse insulin resistance and the increase in visceral adiposity caused by HFD. It is well known that increased visceral fat is a causal factor of metabolic syndrome (Després and Lemieux 2006). The development of visceral adipose tissue also contributes to a heightened secretion of pro-inflammatory mediators, contributing to the systemic state of inflammation found in obesity (Gregor and Hotamisligil 2011). Although we did not find any significant differences in plasma insulin and glycemia, HOMA-IR was significantly higher in the HFD group. Omega-3 supplementation ameliorates insulin sensitivity since the HFD + O group showed a similar HOMA-IR to rats fed a standard diet. Our findings are in agreement with previous studies that demonstrated a reduction in adiposity and an improvement in insulin sensitivity when a high fat diet is associated with omega-3 supplementation (de Sá et al. 2016; Rokling-Andersen et al. 2009; Storlien et al. 1987). In the present study, we showed that HFD induced greater weight gain than SD, independent of omega-3 administration. LeMieux et al. (2015) also reported that omega-3 did not interfere with total body weight in HFD-fed mice. However, they found a reduction in adipocyte size and adipogenesis following omega-3 supplementation (LeMieux et al. 2015). Then, omega-3 exerts an important role in the maintenance of metabolic tissues homeostasis.
In spite of the important metabolic repercussions of omega-3 supplementation, we could not show any improvement in long-term memory related to omega-3 treatment. Our findings are in agreement with previous studies showing memory impairment in experimental models of obesity in rodents. Molteni et al. (2002) reported spatial memory deficits in female rats 2 months after they were fed a high saturated fat and refined sugar diet (Molteni et al. 2002). A similar diet administered for 5 months produced deficits in spatial learning and long-term memory evaluated in the 8-arm radial maze in adult male rats (Ullrich et al. 2010). In our study, 20 weeks of HFD with 45% of energy from fat also promoted memory impairment, as shown by the object recognition task. However, shorter HFD administration is already known to be sufficient to induce cognitive deficits, as demonstrated elsewhere. It was previously shown that four to 5 weeks of a high fat diet also produces spatial memory deficits in young rats (Gergerlioglu et al. 2016; Pathan et al. 2008).
In our study, omega-3 was administered for 4 weeks after 16 weeks of HFD, in order to evaluate whether the effects caused by a HFD could be reversed by omega-3. In this case, the results have shown that omega-3 did not exert a protective effect on animal recognition memory. We can assume that 4 weeks of omega-3 administration was not sufficient to cause an improvement in the recognition memory of these animals following a HFD. It was shown that 12 weeks of administration of docosahexaenoic acid (DHA), a fatty acid from the omega-3 family, promotes an improvement in spatial cognition (Tanabe et al. 2004). Besides, in our study, we used a higher dosage of omega-3 for a shorter period of time. We can speculate that a lower dose of omega-3 over a longer period may have a more positive effect on memory. On the other hand, Sopian et al. (2015) found an improvement in cognitive performance after 3 weeks of fish oil supplementation, with a standard diet enriched with omega-3 PUFAs (Sopian et al. 2015). Another reasonable explanation for our results is that omega-3 is unable to recover the impairment in cognitive function caused by HFD. In Alzheimer’s disease transgenic mice, omega-3 treatment did not promote any beneficial effect on cognition, suggesting that the supplementation of these fatty acids does not protect against Alzheimer’s disease in susceptible individuals (Arendash et al. 2007). However, we cannot exclude their potential in the prevention of cognitive decline. When eicosapentaenoic acid (EPA), also from the omega-3 family, was administered prior to amyloid-β peptide infusion, there was an improvement in the learning ability of rats. Since the deposition of amyloid-β peptide occurs mainly during aging, this finding indicates that omega-3 supplementation may be a strategy to prevent age-related cognitive decline (Hashimoto et al. 2009).
Increasing evidence demonstrates that besides cognitive impairment, HFD can promote insulin resistance, and immune and synaptic changes in different brain areas (Liu et al. 2015; Petrov et al. 2015). Such alterations may promote tissue lesions to which the astrocytes react, elevating GFAP expression. These changes are directly related to neuroinflammation, since astrocytes, in association with microglia, are able to release inflammatory mediators, directly interfering with the nervous system milieu (Theodosis et al. 2008). In our study, we did not address microglia since their recruitment and activation in diet-induced obesity is well demonstrated in the literature (Maldonado-Ruiz et al. 2017). It was also showed that omega-3 inhibits microglial response in neuroinflammatory conditions (Chang et al. 2015; Kurtys et al. 2016), including high-fat diet exposure (Oksman et al. 2006; Cintra et al. 2012; Johnson 2015). Although there have been some studies showing astrogliosis in obesity-induced neuroinflammation, less attention has been paid to these cell responses following a high-fat diet. Thus, in the present study, we focused on GFAP immunostaining to evaluate astrogliosis. In obesity, neuroinflammation is well described in the hypothalamus, which is a primary site where signals coming from the periphery arrive in the CNS (Cavadas et al. 2016; Miller and Spencer 2014). However, there are a few studies focusing on obesity and neuroinflammation in other brain regions. In the present study, we showed an increase in astrocytic activation in the cerebral cortex of the HFD group. However, when evaluating the effect of HFD on GFAP-immunoreactivity in the hippocampus, we did not find any difference between experimental groups. In mice, it was demonstrated that the hippocampal dysfunction caused by high-fat diet is dependent on strain (Xue et al. 2015). Wistar rats show conflicting results, demonstrating a decrease in GFAP immunostaining in the hippocampus following prolonged hypercaloric diet (Gzielo et al. 2016). On the other hand, 4 weeks of a high-fat diet did not change GFAP expression in either the cerebral cortex or the hippocampus (van der Harg et al. 2015). An increase in GFAP immunostaining was shown in transgenic obese rats (Zucker rats) in the cerebral cortex and hippocampus (Tomassoni et al. 2013). Additional studies are necessary to clarify these brain region differences in astrocyte responses to obesity. Thus, despite the conflicting results on the brain areas that exhibit astrocytic activation in response to obesity, certainly this is an important neuroinflammatory response in this condition.
In the present study, we observed that omega-3 exerts a protective effect in the brain by decreasing astrogliosis in the cerebral cortex of the HFD + O group. This finding demonstrates that even for a short period of supplementation, omega-3 is able to exert anti-inflammatory function. In addition to interfering in the inflammation processes, omega-3 can be incorporated into the phospholipids of inflammatory cell membranes, altering inflammatory processes. This change in fatty acid composition allows membranes to maintain its fluidity and to modify the formation of lipid derivatives, being able to influence, in this way, the function of cells involved in the inflammation (Yaqoob and Shaikh 2010). The role of omega-3 PUFAs on the inhibition of nuclear factor κB (NFκB) activation, which is a pro-inflammatory transcription factor, has been reported (Calder 2015). Also, omega-3 can positively modulate an anti-inflammatory gene expression by activating the peroxisome proliferator activated receptor γ (PPARγ) (Heras-Sandoval et al. 2016). In microglial cells, omega-3 treatment decreases the LPS-induced release of TNF-a and IL-6. This effect is mediated through activation of the sirtuin-1 (SIRT1) pathway, which causes NF-kB inhibition due to p65 deacetylation (Inoue et al. 2017). DHA anti-inflammatory effect was also showed in astrocytes followed by saturated fatty acids treatment (Gupta et al. 2012). Thus, these fatty acids have the ability to shift a pro-inflammatory M1 phenotype to M2, which is anti-inflammatory.
The anti-inflammatory effects of omega-3 PUFAs are well known. In obesity, omega-3 prevents macrophage infiltration and decreases inflammatory gene expression in adipose tissue (Todoric et al. 2006). Labrousse et al., found that a 2-month treatment with EPA/DHA prevented the increase in pro-inflammatory cytokine expression in the hippocampus (Labrousse et al. 2012). In the present study, we found an increased mRNA expression of pro-inflammatory cytokines TNF-α and IL-6 in the cerebral cortex after HFD. This pro-inflammatory profile in the brain caused by obesity is already shown in previous studies (Sánchez-Sarasúa et al. 2016; Toyama et al. 2015). Astrocytes and microglia are both important sources of cytokines such as TNF-α and IL-6 during pathological conditions (Baek et al. 2016; Urrutia et al. 2017). In the present study, it was not possible to confirm whether the increased pro-inflammatory cytokine expression is attributed to microglia or astrocytes. However, we believe that astrocytic activation may importantly contribute to this finding, since we also showed a concomitant increase in the number of GFAP-positive cells in the cerebral cortex after HFD. In addition, the neuroinflammatory status has been related to cognitive decline in obesity (Miller and Spencer 2014). In the present study, omega-3 supplementation following the induction of obesity was able to restrain the increase in cytokine expression in the cerebral cortex. Despite this, omega-3 did not improve long-term memory. This result is probably explained by the fact that omega-3 acts by preventing inflammation and consequently, cognitive decline, but it is not able to revert an already established neuronal and/or synaptic damage. This assumption is reinforced by studies focused on aging, since there is a neuroinflammatory profile in this situation.
In conclusion, the supplementation of omega-3 fatty acid for 4 weeks following HFD was able to improve insulin sensitivity, decrease visceral adiposity and diminish the neuroinflammatory profile. These results emphasize the anti-inflammatory role of this family of PUFAs, not only in the periphery, but also in the CNS. However, the lack of a protective effect on the long-term recognition memory after HFD suggests that omega-3 fatty acids are not able to revert already established cognitive impairment. Thus, omega-3 supplementation plays an important role to prevent rather than revert neuronal function impairment.
References
Aghamohammadzadeh R, Heagerty AM (2012) Obesity-related hypertension: epidemiology, pathophysiology, treatments, and the contribution of perivascular adipose tissue. Ann Med 44(Suppl 1):S74–S84. doi:10.3109/07853890.2012.663928
Arendash GW, Jensen MT, Salem N, Hussein N, Cracchiolo J, Dickson A, Leighty R, Potter H (2007) A diet high in omega-3 fatty acids does not improve or protect cognitive performance in Alzheimer's transgenic mice. Neuroscience 149:286–302. doi:10.1016/j.neuroscience.2007.08.018
Baek H, Lim CS, Byun HS, Cho HS, Lee YR, Shin YS, Kim HW, Jeon BH, Kim DW, Hong J, Hur GM, Park JB (2016) The anti-inflammatory role of extranuclear apurinic/apyrimidinic endonuclease 1/redox effector factor-1 in reactive astrocytes. Molecular brain 9:99. doi:10.1186/s13041-016-0280-9
Bazan NG, Molina MF, Gordon WC (2012) Docosahexaenoic acid signalolipidomics in nutrition: significance in aging, neuroinflammation, macular degeneration, alzheimer’s, and other neurodegenerative diseases. Annu Rev Nutr 31:321–351
Bulló M, Casas-Agustench P, Amigó-Correig P, Aranceta J, Salas-Salvadó J (2007) Inflammation, obesity and comorbidities: the role of diet. Public Health Nutr 10:1164–1172. doi:10.1017/S1368980007000663
Calder PC (2015) Marine omega-3 fatty acids and inflammatory processes: effects, mechanisms and clinical relevance. Biochim Biophys Acta 1851:469–484. doi:10.1016/j.bbalip.2014.08.010
Caletti G, Almeida FB, Agnes G, Nin MS, Barros HM, Gomez R (2015) Antidepressant dose of taurine increases mRNA expression of GABAA receptor α2 subunit and BDNF in the hippocampus of diabetic rats. Behav Brain Res 283:11–15. doi:10.1016/j.bbr.2015.01.018
Calsolaro V, Edison P (2016) Neuroinflammation in Alzheimer's disease: current evidence and future directions. Alzheimers Dement 12:719–732. doi:10.1016/j.jalz.2016.02.010
Catalani A, Sabbatini M, Consoli C, Cinque C, Tomassoni D, Azmitia E, Angelucci L, Amenta F (2002) Glial fibrillary acidic protein immunoreactive astrocytes in developing rat hippocampus. Mech Ageing Dev 123:481–490
Cavadas C, Aveleira CA, Souza GF, Velloso LA (2016) The pathophysiology of defective proteostasis in the hypothalamus - from obesity to ageing. Nat Rev Endocrinol 12:723–733. doi:10.1038/nrendo.2016.107
Chang PK, Khatchadourian A, McKinney RA, Maysinger D (2015) Docosahexaenoic acid (DHA): a modulator of microglia activity and dendritic spine morphology. J Neuroinflammation 12:34. doi:10.1186/s12974-015-0244-5
Cintra DE, Ropelle ER, Moraes JC, Pauli JR, Morari J, Souza CT, Grimaldi R, Stahl M, Carvalheira JB, Saad MJ, Velloso LA (2012) Unsaturated fatty acids revert diet-induced hypothalamic inflammation in obesity. PLoS One 7(1):e30571. doi:10.1371/journal.pone.0030571
Cook NL, Kleinig TJ, van den Heuvel C, Vink R (2010) Reference genes for normalising gene expression data in collagenase-induced rat intracerebral haemorrhage. BMC Mol Biol 11:7. doi:10.1186/1471-2199-11-7
de Moura AC, Lazzari VM, Becker RO, Gil MS, Ruthschilling CA, Agnes G, Almeida S, da Veiga AB, Lucion AB, Giovenardi M (2015) Gene expression in the CNS of lactating rats with different patterns of maternal behavior. Neurosci Res 99:8–15. doi:10.1016/j.neures.2015.05.003
de Sá RD, Crisma AR, Cruz MM, Martins AR, Masi LN, do Amaral CL, Curi R, Alonso-Vale MI (2016) Fish oil prevents changes induced by a high-fat diet on metabolism and adipokine secretion in mice subcutaneous and visceral adipocytes. J Physiol 594:6301–6317. doi:10.1113/JP272541
Demark-Wahnefried W, Platz EA, Ligibel JA, Blair CK, Courneya KS, Meyerhardt JA, Ganz PA, Rock CL, Schmitz KH, Wadden T, Philip EJ, Wolfe B, Gapstur SM, Ballard-Barbash R, McTiernan A, Minasian L, Nebeling L, Goodwin PJ (2012) The role of obesity in cancer survival and recurrence. Cancer Epidemiol Biomark Prev 21:1244–1259. doi:10.1158/1055-9965.EPI-12-0485
Després JP, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444:881–887. doi:10.1038/nature05488
Ennaceur A, Delacour J (1988) A new one-trial test for neurobiological studies of memory in rats. 1: behavioral data. Behav Brain Res 31:47–59
Gergerlioglu HS, Oz M, Demir EA, Nurullahoglu-Atalik KE, Yerlikaya FH (2016) Environmental enrichment reverses cognitive impairments provoked by western diet in rats: role of corticosteroid receptors. Life Sci 148:279–285. doi:10.1016/j.lfs.2016.02.011
Gregor MF, Hotamisligil GS (2011) Inflammatory mechanisms in obesity. Annu Rev Immunol 29:415–445. doi:10.1146/annurev-immunol-031210-101322
Gupta S, Knight AG, Keller JN, Bruce-Keller AJ (2012) Saturated long-chain fatty acids activate inflammatory signaling in astrocytes. J Neurochem 120:1060–1071. doi:10.1111/j.1471-4159.2012.07660.x
Gzielo K, Kielbinski M, Ploszaj J, Janeczko K, Gazdzinski SP, Setkowicz Z (2016) Long-term consumption of high-fat diet in rats: effects on microglial and astrocytic morphology and neuronal nitric oxide synthase expression. Cell Mol Neurobiol. doi:10.1007/s10571-016-0417-5
Haan MN, Wallace R (2004) Can dementia be prevented? Brain aging in a population-based context. Annu Rev Public Health 25:1–24. doi:10.1146/annurev.publhealth.25.101802.122951
Hashimoto M, Hossain S, Tanabe Y, Kawashima A, Harada T, Yano T, Mizuguchi K, Shido O (2009) The protective effect of dietary eicosapentaenoic acid against impairment of spatial cognition learning ability in rats infused with amyloid beta(1-40). J Nutr Biochem 20:965–973. doi:10.1016/j.jnutbio.2008.08.009
Hein AM, O'Banion MK (2009) Neuroinflammation and memory: the role of prostaglandins. Mol Neurobiol 40:15–32. doi:10.1007/s12035-009-8066-z
Heras-Sandoval D, Pedraza-Chaverri J, Perez-Rojas JM (2016) Role of docosahexaenoic acid in the modulation of glial cells in Alzheimer's disease. J Neuroinflammation 13:61. doi:10.1186/s12974-016-0525-7
Högyes E, Nyakas C, Kiliaan A, Farkas T, Penke B, Luiten PG (2003) Neuroprotective effect of developmental docosahexaenoic acid supplement against excitotoxic brain damage in infant rats. Neuroscience 119:999–1012
Hossain P, Kawar B, El Nahas M (2007) Obesity and diabetes in the developing world--a growing challenge. N Engl J Med 356:213–215. doi:10.1056/NEJMp068177
Hwang LL, Wang CH, Li TL, Chang SD, Lin LC, Chen CP, Chen CT, Liang KC, Ho IK, Yang WS, Chiou LC (2010) Sex differences in high-fat diet-induced obesity, metabolic alterations and learning, and synaptic plasticity deficits in mice. Obesity (Silver Spring) 18:463–469. doi:10.1038/oby.2009.273
Inoue T, Tanaka M, Masuda S, Ohue-Kitano R, Yamakage H, Muranaka K, Wada H, Kusakabe T, Shimatsu A, Hasegawa K, Satoh-Asahara N (2017) Omega-3 polyunsaturated fatty acids suppress the inflammatory responses of lipopolysaccharide-stimulated mouse microglia by activating SIRT1 pathways. Biochim Biophys Acta 1862:552–560. doi:10.1016/j.bbalip.2017.02.010
Johnson RW (2015) Feeding the beast: can microglia in the senescent brain be regulated by diet? Brain Behav Immun 43:1–8. doi:10.1016/j.bbi.2014.09.022
Kang W, Balordi F, Su N, Chen L, Fishell G, Hebert JM (2014) Astrocyte activation is suppressed in both normal and injured brain by FGF signaling. Proc Natl Acad Sci U S A 111:E2987–E2995. doi:10.1073/pnas.1320401111
Kenchaiah S, Gaziano JM, Vasan RS (2004) Impact of obesity on the risk of heart failure and survival after the onset of heart failure. Med Clin North Am 88:1273–1294. doi:10.1016/j.mcna.2004.04.011
Kohman RA, Rhodes JS (2013) Neurogenesis, inflammation and behavior. Brain Behav Immun 27:22–32. doi:10.1016/j.bbi.2012.09.003
Kurtys E, Eisel UL, Verkuyl JM, Broersen LM, Dierckx RA, de Vries EF (2016) The combination of vitamins and omega-3 fatty acids has an enhanced anti-inflammatory effect on microglia. Neurochem Int 99:206–214. doi:10.1016/j.neuint.2016.07.008
Labrousse VF, Nadjar A, Joffre C, Costes L, Aubert A, Grégoire S, Bretillon L, Layé S (2012) Short-term long chain omega3 diet protects from neuroinflammatory processes and memory impairment in aged mice. PLoS One 7:e36861. doi:10.1371/journal.pone.0036861
Langnaese K, John R, Schweizer H, Ebmeyer U, Keilhoff G (2008) Selection of reference genes for quantitative real-time PCR in a rat asphyxial cardiac arrest model. BMC Mol Biol 9:53. doi:10.1186/1471-2199-9-53
LeMieux MJ, Kalupahana NS, Scoggin S, Moustaid-Moussa N (2015) Eicosapentaenoic acid reduces adipocyte hypertrophy and inflammation in diet-induced obese mice in an adiposity-independent manner. J Nutr 145:411–417. doi:10.3945/jn.114.202952
Liedtke W, Edelmann W, Bieri PL, Chiu FC, Cowan NJ, Kucherlapati R, Raine CS (1996) GFAP is necessary for the integrity of CNS white matter architecture and long-term maintenance of myelination. Neuron 17:607–615
Liu Z, Patil IY, Jiang T, Sancheti H, Walsh JP, Stiles BL, Yin F, Cadenas E (2015) High-fat diet induces hepatic insulin resistance and impairment of synaptic plasticity. PLoS One 10:e0128274. doi:10.1371/journal.pone.0128274
Lotufo PA (2000) Increasing obesity in Brazil: predicting a new peak of cardiovascular mortality. Sao Paulo Med J 118:161–162
Maldonado-Ruiz R, Montalvo-Martínez L, Fuentes-Mera L, Camacho A (2017) Microglia activation due to obesity programs metabolic failure leading to type two diabetes. Nutr Diabetes 7(3):e254. doi:10.1038/nutd.2017.10
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Maury E, Brichard SM (2010) Adipokine dysregulation, adipose tissue inflammation and metabolic syndrome. Mol Cell Endocrinol 314:1–16. doi:10.1016/j.mce.2009.07.031
Mello MM, Studdert DM, Brennan TA (2006) Obesity--the new frontier of public health law. N Engl J Med 354:2601–2610. doi:10.1056/NEJMhpr060227
Miller AA, Spencer SJ (2014) Obesity and neuroinflammation: a pathway to cognitive impairment. Brain Behav Immun 42:10–21. doi:10.1016/j.bbi.2014.04.001
Molteni R, Barnard RJ, Ying Z, Roberts CK, Gómez-Pinilla F (2002) A high-fat, refined sugar diet reduces hippocampal brain-derived neurotrophic factor, neuronal plasticity, and learning. Neuroscience 112:803–814
Morales I, Guzmán-Martínez L, Cerda-Troncoso C, Farías GA, Maccioni RB (2014) Neuroinflammation in the pathogenesis of Alzheimer's disease. A rational framework for the search of novel therapeutic approaches. Front Cell Neurosci 8:112. doi:10.3389/fncel.2014.00112
Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP, Medicine ACoS (2007) American College of Sports Medicine position stand. The female athlete triad. Med Sci Sports Exerc 39:1867–1882. doi:10.1249/mss.0b013e318149f111
Nelissen K, Smeets K, Mulder M, Hendriks JJ, Ameloot M (2010) Selection of reference genes for gene expression studies in rat oligodendrocytes using quantitative real time PCR. J Neurosci Methods 187:78–83. doi:10.1016/j.jneumeth.2009.12.018
Nemeth M, Millesi E, Wagner KH, Wallner B (2015) Sex-specific effects of diets high in unsaturated fatty acids on spatial learning and memory in guinea pigs. PLoS One 10:e0140485. doi:10.1371/journal.pone.0140485
Oksman M, Iivonen H, Hogyes E, Amtul Z, Penke B, Leenders I, Broersen L, Lütjohann D, Hartmann T, Tanila H (2006) Impact of different saturated fatty acid, polyunsaturated fatty acid and cholesterol containing diets on beta-amyloid accumulation in APP/PS1 transgenic mice. Neurobiol Dis 23(3):563–572. doi:10.1016/j.nbd.2006.04.013
Pathan AR, Gaikwad AB, Viswanad B, Ramarao P (2008) Rosiglitazone attenuates the cognitive deficits induced by high fat diet feeding in rats. Eur J Pharmacol 589:176–179. doi:10.1016/j.ejphar.2008.06.016
Petrov D, Pedrós I, Artiach G, Sureda FX, Barroso E, Pallàs M, Casadesús G, Beas-Zarate C, Carro E, Ferrer I, Vazquez-Carrera M, Folch J, Camins A (2015) High-fat diet-induced deregulation of hippocampal insulin signaling and mitochondrial homeostasis deficiences contribute to Alzheimer disease pathology in rodents. Biochim Biophys Acta 1852:1687–1699. doi:10.1016/j.bbadis.2015.05.004
Pistell PJ, Morrison CD, Gupta S, Knight AG, Keller JN, Ingram DK, Bruce-Keller AJ (2010) Cognitive impairment following high fat diet consumption is associated with brain inflammation. J Neuroimmunol 219:25–32. doi:10.1016/j.jneuroim.2009.11.010
Ransohoff RM, Schafer D, Vincent A, Blachère NE, Bar-Or A (2015) Neuroinflammation: ways in which the immune system affects the brain. Neurotherapeutics 12:896–909. doi:10.1007/s13311-015-0385-3
Rokling-Andersen MH, Rustan AC, Wensaas AJ, Kaalhus O, Wergedahl H, Røst TH, Jensen J, Graff BA, Caesar R, Drevon CA (2009) Marine n-3 fatty acids promote size reduction of visceral adipose depots, without altering body weight and composition, in male Wistar rats fed a high-fat diet. Br J Nutr 102:995–1006. doi:10.1017/S0007114509353210
Rossato JI, Bevilaqua LR, Myskiw JC, Medina JH, Izquierdo I, Cammarota M (2007) On the role of hippocampal protein synthesis in the consolidation and reconsolidation of object recognition memory. Learn Mem 14:36–46. doi:10.1101/lm.422607
Sánchez-Sarasúa S, Moustafa S, García-Avilés Á, López-Climent MF, Gómez-Cadenas A, Olucha-Bordonau FE, Sánchez-Pérez AM (2016) The effect of abscisic acid chronic treatment on neuroinflammatory markers and memory in a rat model of high-fat diet induced neuroinflammation. Nutr Metab (Lond) 13:73. doi:10.1186/s12986-016-0137-3
Shah A, Mehta N, Reilly MP (2008) Adipose inflammation, insulin resistance, and cardiovascular disease. JPEN J Parenter Enteral Nutr 32:638–644. doi:10.1177/0148607108325251
Sopian NF, Ajat M, Shafie NI, Noor MH, Ebrahimi M, Rajion MA, Meng GY, Ahmad H (2015) Does short-term dietary omega-3 fatty acid supplementation influence brain hippocampus gene expression of zinc transporter-3? Int J Mol Sci 16:15800–15810. doi:10.3390/ijms160715800
Storlien LH, Kraegen EW, Chisholm DJ, Ford GL, Bruce DG, Pascoe WS (1987) Fish oil prevents insulin resistance induced by high-fat feeding in rats. Science 237:885–888
Sun J, Zheng JH, Zhao M, Lee S, Goldstein H (2008) Increased in vivo activation of microglia and astrocytes in the brains of mice transgenic for an infectious R5 human immunodeficiency virus type 1 provirus and for CD4-specific expression of human cyclin T1 in response to stimulation by lipopolysaccharides. J Virol 82:5562–5572. doi:10.1128/jvi.02618-07
Tanabe Y, Hashimoto M, Sugioka K, Maruyama M, Fujii Y, Hagiwara R, Hara T, Hossain SM, Shido O (2004) Improvement of spatial cognition with dietary docosahexaenoic acid is associated with an increase in Fos expression in rat CA1 hippocampus. Clin Exp Pharmacol Physiol 31:700–703. doi:10.1111/j.1440-1681.2004.04068.x
Tapia-González S, García-Segura LM, Tena-Sempere M, Frago LM, Castellano JM, Fuente-Martín E, García-Cáceres C, Argente J, Chowen JA (2011) Activation of microglia in specific hypothalamic nuclei and the cerebellum of adult rats exposed to neonatal overnutrition. J Neuroendocrinol 23:365–370. doi:10.1111/j.1365-2826.2011.02113.x
Theodosis DT, Poulain DA, Oliet SH (2008) Activity-dependent structural and functional plasticity of astrocyte-neuron interactions. Physiol Rev 88:983–1008. doi:10.1152/physrev.00036.2007
Todoric J, Löffler M, Huber J, Bilban M, Reimers M, Kadl A, Zeyda M, Waldhäusl W, Stulnig TM (2006) Adipose tissue inflammation induced by high-fat diet in obese diabetic mice is prevented by n-3 polyunsaturated fatty acids. Diabetologia 49:2109–2119. doi:10.1007/s00125-006-0300-x
Toklu HZ, Yang Z, Oktay S, Sakarya Y, Kirichenko N, Matheny MK, Muller-Delp J, Strang K, Scarpace PJ, Wang KKW, Tumer N (2017) Overpressure blast injury-induced oxidative stress and neuroinflammation response in rat frontal cortex and cerebellum. Behav Brain Res. doi:10.1016/j.bbr.2017.04.025
Tomassoni D, Nwankwo IE, Gabrielli MG, Bhatt S, Muhammad AB, Lokhandwala MF, Tayebati SK, Amenta F (2013) Astrogliosis in the brain of obese Zucker rat: a model of metabolic syndrome. Neurosci Lett 543:136–141. doi:10.1016/j.neulet.2013.03.025
Toyama K, Koibuchi N, Hasegawa Y, Uekawa K, Yasuda O, Sueta D, Nakagawa T, Ma M, Kusaka H, Lin B, Ogawa H, Ichijo H, Kim-Mitsuyama S (2015) ASK1 is involved in cognitive impairment caused by long-term high-fat diet feeding in mice. Sci Rep 5:10844. doi:10.1038/srep10844
Ullrich C, Pirchl M, Humpel C (2010) Hypercholesterolemia in rats impairs the cholinergic system and leads to memory deficits. Mol Cell Neurosci 45:408–417. doi:10.1016/j.mcn.2010.08.001
Urrutia PJ, Hirsch EC, Gonzalez-Billault C, Nunez MT (2017) Hepcidin attenuates amyloid beta-induced inflammatory and pro-oxidant responses in astrocytes and microglia. J Neurochem. doi:10.1111/jnc.14005
van de Sande-Lee S, Velloso LA (2012) Hypothalamic dysfunction in obesity. Arq Bras Endocrinol Metabol 56:341–350
van der Harg JM, Eggels L, Ruigrok SR, Hoozemans JJ, la Fleur SE, Scheper W (2015) Neuroinflammation is not a prerequisite for diabetes-induced tau phosphorylation. Front Neurosci 9:432. doi:10.3389/fnins.2015.00432
Wannamethee SG, Shaper AG (1999) Weight change and duration of overweight and obesity in the incidence of type 2 diabetes. Diabetes Care 22:1266–1272
Xue Y, Li J, Yan L, Lu L, Liao FF (2015) Genetic variability to diet-induced hippocampal dysfunction in BXD recombinant inbred (RI) mouse strains. Behav Brain Res 292:83–94. doi:10.1016/j.bbr.2015.06.023
Yaqoob P, Shaikh SR (2010) The nutritional and clinical significance of lipid rafts. Curr Opin Clin Nutr Metab Care 13:156–166. doi:10.1097/MCO.0b013e328335725b
Zimmermann-Peruzatto JM, Lazzari VM, Agnes G, Becker RO, de Moura AC, Guedes RP, Lucion AB, Almeida S, Giovenardi M (2016) The impact of oxytocin gene knockout on sexual behavior and gene expression related to neuroendocrine Systems in the Brain of female mice. Cell Mol Neurobiol. doi:10.1007/s10571-016-0419-3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Funding
This study was supported by CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico).
Rights and permissions
About this article
Cite this article
de Andrade, A.M., Fernandes, M.C., de Fraga, L.S. et al. Omega-3 fatty acids revert high-fat diet-induced neuroinflammation but not recognition memory impairment in rats. Metab Brain Dis 32, 1871–1881 (2017). https://doi.org/10.1007/s11011-017-0080-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-017-0080-7