Abstract
D-galactose (GAL) has been used as an animal model for brain aging and antiaging studies. GAL stimulates oxidative stress in several tissues including brain. Carnosine (CAR; β-alanil-L-histidine) and taurine (TAU; 2-aminoethanesulfonic acid) exhibit antioxidant properties. CAR and TAU have anti-aging and neuroprotective effects. We investigated the effect of CAR and TAU supplementations on oxidative stress and brain damage in GAL-treated rats. Rats received GAL (300 mg/kg; s.c.; 5 days per week) alone or together with CAR (250 mg/kg/daily; i.p.; 5 days per week) or TAU (2.5 % w/w; in rat chow) for 2 months. Brain malondialdehyde (MDA), protein carbonyl (PC) and glutathione (GSH) levels and superoxide dismutase (SOD), glutathione peroxidase (GSH-Px), glutathione transferase (GST) and acetylcholinesterase (AChE) activities were determined. Expressions of B cell lymphoma-2 (Bcl-2), Bax and caspase-3 were also evaluated in the brains by immunohistochemistry. GAL treatment increased brain MDA and PC levels and AChE activities. It decreased significantly brain GSH levels, SOD and GSH-Px but not GST activities. GAL treatment caused histopathological changes and increased apoptosis. CAR and TAU significantly reduced brain AChE activities, MDA and PC levels and elevated GSH levels in GAL-treated rats. CAR, but not TAU, significantly increased low activities of SOD and GSH-Px. Both CAR and TAU diminished apoptosis and ameliorated histopathological findings in the brain of GAL-treated rats. Our results indicate that CAR and TAU may be effective to prevent the development of oxidative stress, apoptosis and histopathological deterioration in the brain of GAL-treated rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
D-galactose (GAL)-induced aging model in rodents is produced by consecutive GAL injections for 6–8 weeks. This model exhibits accelerated aging in tissues such as brain, liver and others (Anand et al. 2012; Hsia et al. 2012; Tsai and Yin 2012). It has been demonstrated that increased formation of reactive oxygen species (ROS) and lipid/protein oxidations play an important role in GAL-induced accelerated aging model (Anand et al. 2012; Hsia et al. 2012; Lan et al. 2012; Tsai and Yin 2012; Prakash and Kumar 2013; Wu et al. 2014; Xian et al. 2014; Haider et al. 2015), as well as in natural aging (Harman 2001; Parıldar-Karpuzoğlu et al. 2008; Aydın et al. 2010).
Carnosine (CAR; β-alanyl-L-histidine) has membrane protecting activity and metal chelating ability. CAR is also a potent scavenger of ROS and aldehydes. It inhibits lipid peroxidation and protein oxidation In addition, CAR can scavenge reactive carbonyl species and reduce the formation of AGEs (Hipkiss 2009; Boldyrev et al. 2013). CAR has been used to prevent oxidative stress-induced pathologies such as ischemia-reperfusion, liver injury, atherosclerosis and diabetic complications (Hipkiss 2009; Boldyrev et al. 2013; Uysal et al. 2015). Some investigators have also proposed that CAR has anti-aging and neuroprotective actions (Hipkiss 2009; Boldyrev et al. 2013; Fayaz et al. 2015). We also reported that CAR treatment diminished oxidative stress in serum and tissues of naturally aged rats (Aydın et al. 2010).
Taurine (TAU; 2-aminoethanesulfonic acid) is the major intracellular free β-amino acid. TAU is synthesized from cysteine and methionine and ingested with certain foodstuffs. It decreases tissue lipid peroxidation by scavenging or quenching oxygen-derived free radicals or binding free metal ions such as Fe2+ or Cu+ via its sulfonic acid group (Schaffer et al. 2003). In addition, TAU was also reported to have antiapoptotic properties (Menzie et al. 2013). TAU was found to be a protective agent against oxidative stress-induced pathologies such as atherosclerosis, diabetic complications, hepatic and gastrointestinal damage (Das et al. 2012; Miyazaki and Matsuzaki 2014). TAU has also antiaging and neuroprotective properties as an antioxidant (El Idrissi et al. 2013; Menzie et al. 2013). We (Parıldar-Karpuzoğlu et al. 2008) and others (Yıldırım et al. 2007) have reported that TAU treatment decreased oxidative stress in tissues of naturally aged rats.
GAL-induced aging model has been frequently used for brain aging and antiaging pharmacology studies. We recently reported that blueberry treatment diminished oxidative stress and apoptosis together with amelioration of histopathological findings in brains of GAL-induced aged rats (Çoban et al. 2015). In our study, we wanted to investigate the efficiency of CAR and TAU in the brain tissue of rats exposed to same aging model. Therefore, brain malondialdehyde (MDA), protein carbonyl (PC) and glutathione (GSH) levels and Cu, Zn superoxide dismutase (SOD), glutathione peroxidase (GSH-Px) and glutathione transferase (GST) as well as acetylcholinesterase (AChE) activities were determined. In addition, expressions of apoptosis-related proteins, proapoptotic Bax, antiapoptotic B cell lymphoma-2 (Bcl-2) as well as caspase-3 were evaluated in the brain of GAL-treated rats by immunohistochemical analysis.
Materials and methods
Chemicals
GAL, CAR, TAU and other chemicals were of the highest purity and were obtained from Sigma-Aldrich (St Louis, Missouri, USA).
Animals and experimental design
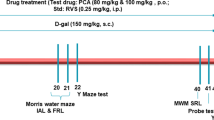
Male Wistar rats (200–220 g) were used for experiments. Animals were obtained from Yeditepe University Animal Center. Rats were caged at 22 °C, with 12-hr light–dark cycle. They had free access to food and water ad libitum. The experimental procedure used in this study met the guidelines of the Animals Ethics Reviews Committee of Yeditepe University. Rats were divided into six groups (n = 8 each); a) Group 1 was used as the control. b) Group 2 was injected with CAR (250 mg/kg/daily; i.p.; 5 days per week) intraperitoneally. c) Group 3 was fed with TAU (2.5 % w/w) containing commercial rat chow. d) Group 4 was treated with GAL (300 mg/kg; 5 days per week) subcutaneously. e) Group 5 was injected with GAL and CAR as mentioned above. f) Group 6 was injected with GAL and fed with TAU as mentioned above. All animals were dosed for the entire 2 months. Group 1 and group 4 are mutual groups in this study and in our previous study (Çoban et al. 2015) which were conducted at the same time.
Blood and tissue samples
All rats were sacrificed by taking blood via cardiac puncture under sodium thiopental anesthesia (50 mg/kg, i.p.) after 2 months. Whole brains except cerebellum were quickly removed and washed in 0.9 % NaCl. Brain samples were frozen at −80 °C for later uses. Brain tissues were homogenized in ice-cold 0.15 M KCl (10 %; w/v) and postmitochondrial fractionswere obtained for SOD, GSH-Px, GST and AChE activities. Therefore, brain homogenates were centrifuged at 600×g for 10 min at 4 °C to remove crude fractions. Then, supernatants were centrifuged at 10,000×g for 20 min.
Determination of brain MDA and PC levels
Lipid peroxidation was assessed by measuring the levels of MDA by thiobarbituric acid (TBA) test (Ohkawa et al. 1979). The reaction mixture containing 0.2 ml of tissue homogenate, 0.2 ml of 8.1 % sodium dodecyl sulfate, 1.5 ml of 20 % (v/v) acetic acid solution (adjusted to pH:3.5 with NaOH), 1.5 ml of 0.8 % TBA and 0.6 ml of distilled water were placed in a water bath at 95 °C for 1 h. After cooling, 1.0 ml distilled water and 5.0 ml of butanol:pyridine mixture (15:1; v/v) were added. After centrifugation at 3000 rpm for 10 min, absorbances were read at 532 nm spectrophotometrically. The breakdown product of 1,1,3,3-tetraethoxypropane was used as a standard.
The oxidative protein damage was measured by the quantification of carbonyl groups based on spectrophotometric detection of the reaction between 2,4-dinitrophenylhydrazine (DNPH) and PC to form protein hydrazones (Reznick and Packer 1994). Brain tissues (150–200 mg) were homogenized in 3 ml of 50 mM phophate buffer pH 7.4 containing 1 mM EDTA and a cocktail of protease inhibitors. 1 ml of homogenates were incubated in glass test tubes with 4.0 ml of 10 mM DNPH dissolved in 2.5 M HCl, allowed to stand for 1 h in the dark and stirred every 15 min. Then, 5 ml of 20 % (w/v) trichloracetic acid was added to the reaction mixture. Tubes were left in ice bucket for 10 min and centrifuged for 5 min to collect the protein precipitates. The precipitates were washed 3 times with 4 ml of ethanol-ethylacetate (1:1; v/v) mixture to remove the free DNPH and other concomitants. The final precipitates were dissolved in 2.0 ml of 6 M guanidine hydrochloride solution and left 10 min at 37 °C. The absorbance was measured at 360 nm. PC was determined using a molar extinction coefficient (22,000 M−1cm−1) and expressed as nmoles of carbonyls/mg protein.
Determination of GSH levels
GSH levels in brain homogenates were measured by using 5,5′-dithiobis-(2-nitrobenzoate) (DTNB) at 412 nm spectrophotometrically (Beutler et al. 1963). In brief, 1 ml of homogenate (10 %; w/v) and 1 ml of 0.15 M KCl were mixed and deproteinized by addition of 3 ml of metaphosphoric acid solution (30 g NaCl, 1.67 g metaphosphoric acid, and 0.2 g EDTA in 100 ml distilled water). Tubes were centrifugated at 3000 rpm for 20 min, 0.5 ml of supernatant was added to 2 ml of 0.3 M Na2HPO4.2H2O and 0.5 ml DTNB (0.4 mg/ml in 1 % sodium citrate) solution. Absorbances at 412 nm were measured immediately after mixing. GSH levels were calculated using extinction coefficient (13,600 M−1cm−1).
Determination of SOD activity
SOD activity was assayed by its ability to increase the riboflavin-sensitized photooxidation of o-dianisidine (Mylorie et al. 1986). 2.7 ml of 50 mM potassium phosphate buffer (pH:7.8) containing 0.1 mM EDTA, 0.05 ml distilled water, 0.1 ml of 0.39 mM riboflavin dissolved in 10 mM potassium phosphate buffer (pH:7.5), 0.1 ml of 6 mM o-dianisidine.2HCl and 0.05 ml of postmitochondrial fraction were mixed and illuminated with 20 W fluorescence lambs at 37 °C for 8 min. Absorbance readings were taken before and after 8 min of illumination at 460 nm. SOD activity was calculated according to the difference in absorbances. A standard curve was prepared by using bovine SOD and results were expressed as U/mg protein.
Determination of GSH-Px activity
GSH-Px activities were measured using cumene hydroperoxide as substrate (Lawrence and Burk 1976). The assay mixture contained 50 mM potassium phoshate buffer (pH:7.0), 1 mM EDTA, 1 mM sodium azide, 0.2 mM NADPH, 1 mM GSH, 0.5 IU/ml glutathione reductase, 1.2 mM cumene hydroperoxide and 0.1 ml of diluted postmitochondrial fraction in a total volume of 1 ml. Reaction was followed spectrophotometrically (340 nm) at 37 °C after the addition of cumene hydroperoxide. Results were calculated using extinction coefficient of NADPH (6.22 × 103 M−1cm−1) and expressed as nmol/min/mg protein.
Determination of GST activity
GST activity was measured using 1-chloro-2,4-dinitrobenzene (CDNB) as substrate (Habig and Jacoby 1981). The assay mixture contained 100 mM potassium phoshate buffer (pH:7.0), 1 mM CDNB, 1 mM GSH and 0.2 ml of diluted postmitochondrial fraction in a total volume of 3 ml. Reaction was started with the addition of CDNB and followed spectophotometrically (340 nm) at 25 °C. Results were calculated using the extinction coefficient (9600 M−1cm−1) of the product formed by the conjugation of GSH and CDNB. Values were expressed as nmol/min/mg protein.
Determination of AChE activity
AchE activity is a marker of loss of cholinergic neurons in the brain. The AChE activity was assessed by Ellman method (1961). Briefly, 0.1 ml of post mitochondrial fraction was added to 2.65 ml of 100 mM potassium phosphate buffer (pH:7.4). The reaction was started with the addition of 0.1 ml of 24 mM acetylcholine iodide as substrate and change in absorbance (412 nm) was noted every 30 s for 150 s at 25 °C. Results were calculated using the molar extinction coefficient of chromophore (13,600 M−1cm−1) and expressed as nmol of substrate hydrolyzed/min/mg protein.
Determination of protein levels
Protein levels were determined using bicinchoninic acid (Smith et al. 1985). Briefly, 0.01 ml of diluted postmitochondrial fraction was added to 0.2 ml bicinchoninic acid solution containing 0.08 % CuSO4, incubated for 30 min at 37 °C and absorbance was read at 562 nm.
Immunohistochemical analysis for Bax, Bcl-2 and caspase 3 in the brain
After routine tissue processing 3 μm thick 3 sections from each paraffin block for the immunohistochemistry were deparaffinized in xylene and dehydrated in graded ethyl alcohol. Following deparaffinization, the slides for Bax, Bcl-2 and Caspase 3 were boiled for 20 min in 10 mM citrate buffer (pH:6.0), followed by cooling at room temperature for 20 min, and then rinsed with distilled water. The slides were immersed for 30 min in 0.3 % hydrogen peroxide (H2O2) in methanol for endogenous peroxide inactivation followed by three washes in phosphate buffer saline (PBS, pH:7.4) at room temperature. Subsequently, non-specific binding was blocked by PBS containing 1 % goat serum and 1 % bovine serum albumin which was applied for 30 min. Next, for each slide Bax (dilution 1:100, Santa Cruz, Europe), Bcl-2 (MS-123-R7, ready to use kit, Rat monoclonal antibody, Thermo, Neomarkers, Fremont, USA), Caspase 3 (dilution 1:10, Rabbit anti-active polyclonal antibody, Chemicon, Europe) were applied for 1 h at room temperature. After washing in PBS, peroxidase activity was localized with chromogen 3,3′-diaminobenzidine (DAB; DAKO Liquid DAB-Substrate-chromogen K-3466, CA, USA) and 0.03 % H2O2. Sections were counter-stained with haematoxylen, cleaned and mounted. Negative control studies were performed concurrently in the absence of the primary antibody. Positive control studies were also performed simultaneously in human breast carcinoma sections for Bax and Bcl-2, human tonsil section for Caspase-3 as stated in data sheets. Brown staining in the cytoplasm of neuronal cells was considered as “positive” and no staining as “negative” for Bcl-2, Bax and caspase antibodies. Positive staining for all antibodies was graded as: 3+ for positive stained total neuronal cell number>50 %, 2+ for 25–49 %, 1+ for 10–24 % and 0 for <9 % positive staining.
Light microscopic examination
The brain tissues were fixed in 10 % formalin, for 24 h. After routine automated tissue processing (Thermo Scientific Excelsior Tissue Processor), the tissues containing cortical areas of parietotemporal and frontal lobes were embedded in paraffin. Four micrometer-thick sections obtained from each paraffin block were stained with haematoxylen and eosin (H&E) for histopathological evaluation under digital light microscope Olympus BX51. During light microscopic examination; vacuolar changes, edema and inflammation (detecting lymphocytes considered as inflammation) status of brain tissues were evaluated and graded into 4 categories as follows: none, mild, moderate and severe.
Statistical analysis
The results were expressed as mean ± SD. One-way analysis of variance (ANOVA) followed by Tukey’s post-hoc test was used for equal variances. Kruskal-Wallis test was performed for unequal variances. In all cases, a difference was considered significant when p < 0.05.
Results
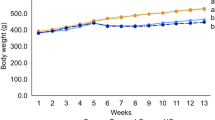
During the experimental process, there were no inflammation in injection sites of rats and significant differences in general appearance. There were no significant differences in food intake, water intake, final body weight and brain weight among the groups (data not shown).
GAL caused significant increases in brain MDA and PC levels. CAR and TAU treatments were observed to decrease MDA and PC levels (Fig. 1). GAL treatment resulted in significant decreases in GSH levels, and SOD and GSH-Px activities in the brain. However, brain GST activity remained unchanged. CAR treatment was observed to increase GSH levels and SOD and GSH-Px activities. However, GST activity remained unchanged. TAU treatment increased GSH levels but it did not alter SOD, GSH-Px and GST activities in GAL-treated rats (Table 1). GAL caused significant increases in brain AChE activity. CAR and TAU treatments were observed to decrease increased activity of AChE in GAL-treated rats (Fig. 2).
The effects of carnosine (CAR) and taurine (TAU) treatments on brain malondialdehyde (MDA) and protein carbonyl (PC) levels in D-galactose (GAL)-treated rats (Mean ± SD; n = 8 each). a p < 0.05 GAL vs control; b p < 0.05 GAL vs CAR group; c p < 0.05 GAL vs TAU; d p < 0.05 GAL vs GAL+CAR; e p < 0.05 GAL vs GAL+TAU
Immunohistochemical results were shown in Table 2. Bax expression increased in GAL-treated group when compared to control groups and GAL+CAR and GAL+TAU treated groups. However, Bcl-2 expression was slightly decreased in GAL-treated group when compared to control groups, GAL+CAR and GAL+TAU-treated groups (Fig. 3). Caspase-3 expressions also increased in GAL-treated group when compared to control groups and GAL+CAR and GAL+TAU treated groups (Fig. 4).
The effects of carnosine (CAR) and taurine (TAU) treatments on Bax and Bcl-2 expressions in the brain of galactose (GAL)-treated rats in immunohistochemical analysis (×400). Brown staining represents the Bax positive neuronal and glial cells. Bax expression was increased in GAL- treated rats (2+) when compared to control (0), GAL+CAR and GAL+TAU (+1) groups. Bcl-2 expression was slightly decreased in GAL-treated group when compared to control, GAL+CAR and GAL+ TAU groups. Groups: a Control; b GAL; c GAL+CAR; d GAL+TAU
The effects of carnosine (CAR) and taurine (TAU) treatments on caspase-3 expression in the brain of galactose (GAL)-treated rats in immunohistochemical analysis in D-galactose (GAL)-treated rats (×400). Brown staining represents the caspase-3 positive neuronal and glial cells. Caspase-3 expression was increased in GAL-treated rats (2+) when compared to control (0), GAL+CAR and GAL+TAU (+1) groups. Groups: a Control; b GAL; c GAL+CAR; d GAL+TAU
In the GAL-treated rats, histopathological examination of the brain revealed marked vacuolar changes, slight edema and mild inflammatory infiltration in cortical areas when compared to control group. These findings may be seen in brain ischemia or neurodegenerative processes. In both GAL+CAR- and GAL+TAU-treated groups, the histopathological examination of brain revealed slight to moderate decrease in vacuolar changes; moderate decrease in edema and marked decrease in inflammation, when compared to only GAL-treated rat brains (Fig. 5).
Discussion
GAL treatment (100–500 mg/kg body weight; s.c.) for 2 months to rodents is suitable to produce age-related disease model. Increased lipid peroxide and PC levels (Anand et al. 2012; Hsia et al. 2012; Prakash and Kumar 2013; Wu et al. 2014; Xian et al. 2014; Haider et al. 2015) and AGEs formation (Tsai and Yin 2012), histopathological changes (Anand et al. 2012; Wu et al. 2014) and progressive deterioration in learning and memory capacity (Lan et al. 2012; Prakash and Kumar 2013; Xian et al. 2014; Haider et al. 2015) were detected in GAL-treated rodents. In our study, rats were given GAL for 2 months. Brain MDA and PC levels increased, however, GSH levels and SOD and GSH-Px activities were found to decrease following GAL treatment. Lower levels of GSH, the substrate of GSH-Px, may cause the diminished GSH-Px activity. In addition, accumulation of H2O2 leads to decreased SOD activity. These findings clearly show that GAL treatment causes a significant oxidative stress in the brain as indicated by increased MDA and PC levels and diminished activity of antioxidant enzymes.
We recently reported that CAR and TAU supplementation decreased prooxidant status together with histopathological amelioration in the liver of GAL-treated rats (Kalaz et al. 2014). However, there is no study about the effect of TAU treatment in brain of GAL-treated rodents, but there is one study with CAR (Han et al. 2014). CAR and TAU are found in high concentrations especially in the brain. Their brain levels were shown to increase by CAR or TAU supplementations because exogenous CAR and TAU are able to cross the blood–brain barrier when administered therapeutically (Jin et al. 2005; Menzie et al. 2013). Therefore, it has been suggested that CAR (Hipkiss 2009; Boldyrev et al. 2013; Fayaz et al. 2015) and TAU (El Idrissi et al. 2013; Menzie et al. 2013) can be used to protect the brain against acute neuronal injury and chronic degeneration processes. Recently, Han et al. (2014) have investigated the effect of CAR treatment on GAL-induced oxidative stress and learning dysfunction in BALB/c mice. GAL (approximately 300 mg/kg/day; s.c) was injected to mice for 8 weeks. From the beginning of the fifth week, CAR (40 mg/kg, orally) were administered until the end of studies. Authors have detected that CAR treatment decreased high levels of MDA in serum, liver and brain. This treatment increased low levels of GSH and oxygen radical antioxidant capacity in brain and liver. CAR treatment also causes significant decreases in brain AGEs levels. However, this treatment did not improve impaired spatial memory and learning induced by D-GAL in mice (Han et al. 2014).
In the current study, GAL-injected rats were simultaneously treated with CAR or TAU for 8 weeks. The doses for CAR or TAU were effective concentrations and they were chosen according to our previous studies (Parıldar-Karpuzoğlu et al. 2008; Aydın et al. 2010; Kalaz et al. 2014). CAR treatment was observed to decrease brain MDA and PC levels and increase GSH levels in GAL-treated rats. These findings are in accordance with Han et al. (2014). As it is known, increased oxidative stress leads to copper release from the SOD molecule and results in enzyme molecule’s fragmentation. Transition metals such as iron and copper react with H2O2 to produce hydroxyl radicals through Fenton-like reactions. In the current study, CAR treatment is found to increase brain SOD activity in GAL-treated rats, which supports the fact that CAR is a good scavenger of superoxide and hydroxyl radicals sparing SOD molecule. Therefore, CAR is suggested to protect SOD from oxidative damage through the actions of copper chelating and radical scavenging. Indeed, it has been reported that in vivo CAR treatment protected brain SOD under oxidative stress conditions such as hypobaric hypoxia and accelerated aging (Stvolinskii et al. 2003).
In this study, we found that TAU treatment reduced MDA and PC levels and increased brain GSH levels without affecting changes in antioxidant enzyme activities in GAL-treated rats. Several mechanisms may play a role in TAU-mediated reduction in oxidative stress. TAU was reported to protect cells by scavenging oxygen free radicals, binding free metal ions such as Fe2+ by its sulfonic acid group. Since cysteine is a precursor of TAU and GSH, TAU supplementation may cause enhancement in GSH levels by directing cysteine into the GSH synthesis pathway. Therefore, increments in GSH levels after TAU treatment may play an additional role in decreasing oxidative stress.
On the other hand, chronic administration of GAL showed marked increase of the activity of AChE enzyme, one of the specific cholinergic markers (Haider et al. 2015; Ruan et al. 2014). Increases in AChE activity caused by GAL treatment may lead to a reduction of cholinergic neurotransmission due to a decrease in acetylcholine levels in synaptic cleft (Zhang et al. 2011; Ruan et al. 2014). Thus, modulation of cholinergic neurotransmission may be one of the mechanisms involved in the impairment of cognitive functions of GAL-treated rodents (Zhang et al. 2011). In our study, CAR and TAU treatments were observed to decrease high AChE activity in brain of GAL-treated rats. Decrease in AchE activity may improve cholinergic neurotransmission by restorating acetylcholine levels in synaptic cleft. Although there is no study investigating the effect of CAR treatment on AChE activity in the literature, some authors have also reported that TAU treatment resulted in decreases in AChE activity and an improvement in learning and memory in acute ethanol toxicity (Rosemberg et al. 2010).
Mitochondrial apoptotic pathway plays an important role in brain aging in GAL-treated rodents (Tsai and Yin 2012; Wu et al. 2014; Prakash and Kumar 2013; Lan et al. 2012). In our study, increased proapoptotic Bax and decreased antiapoptotic Bcl-2 protein expressions together with increased caspase-3 protein expressions were detected in GAL-treated rats by immunohistochemical procedures. CAR and TAU treatments, on the other hand, decreased caspase-3 and Bax expressions and increased Bcl-2 expressions in GAL-treated rats. These results indicate that CAR and TAU treatments exert antiapoptotic effect in the brain of GAL-treated rats. CAR and TAU also ameliorated GAL-induced histopathological changes in the brain.
Our results indicate that CAR and TAU may be effective to prevent the development of oxidative stress, apoptosis and histopathological deterioration in the brain of GAL-treated rats.
References
Anand KV, Jaabir MSM, Thomas PA, Geraldine P (2012) Protective role of chrysin against oxidative stress in D-galactose-induced aging in an experimental rat model. Geriatr Gerontol Int 12:741–750
Aydın AF, Küçükgergin C, Özdemirler-Erata G, Koçak-Toker N, Uysal M (2010) The effect of carnosine treatment on prooxidant-antioxidant balance in liver, heart and brain tissues of male aged rats. Biogerontology 11:103–109
Beutler E, Duron O, Kelly BM (1963) Improved method for the determination of blood glutathione. J Lab Clin Med 61:882–888
Boldyrev AA, Aldini G, Derave W (2013) Physiology and pathophysiology of carnosine. Physiol Rev 93:1803–1845
Çoban J, Doğan-Ekici I, Aydın AF, Kalaz EB, Doğru-Abbasoğlu S, Uysal M (2015) Blueberry treatment decreased D-galactose-induced oxidative stress and brain damage in rats. Metab Brain Dis 30:793–802
Das J, Roy A, Sil PC (2012) Mechanism of the protective action of taurine in toxin and drug induced organ pathophysiology and diabetic complications: a review. Food Funct 3:1251–1264
El Idrissi A, Shen CH, L’Amoreaux WJ (2013) Neuroprotective role of taurine during aging. Amino Acids 45:735–750
Ellman GL, Courtney KD, Andres V Jr, Feather-Stone RM (1961) A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem Pharmacol 7:88–95
Fayaz SM, Majid A, Rajanikant GK (2015) Carnosine-induced neuroprotection. In: Preedy VR (ed) Imidazole dipeptides. Chemistry, analysis, function and effects. The Royal Society of Chemistry, Cambridge, pp 412–431
Habig WH, Jacoby WB (1981) Assays for differentation of glutathione s-transferases. Methods Enzymol 77:398–405
Haider S, Liaquat L, Shahzad S, Sadir S, Madiha S, Batool Z, Tabassum S, Saleem S, Naqvi F, Perveen T (2015) A high dose of short term exogenous d-galactose administration in young male rats produces symptoms simulating the natural aging process. Life Sci 124:110–119
Han CH, Lin YS, Lee TL, Liang HJ, Hou WC (2014) Asn-Trp dipeptides improve the oxidative stress and learning dysfunctions in D-galactose-induced BALB/c mice. Food Funct 5:2228–2236
Harman D (2001) Aging: overwiev. Ann N Y Acad Sci 928:1–21
Hipkiss AR (2009) Carnosine and its possible roles in nutrition and health. Adv Food Nutr Res 57:87–154
Hsia CH, Wang CH, Kuo YW, Ho YJ, Chen HL (2012) Fructo-oligosaccharide systemically diminished D-galactose-induced oxidative molecule damages in BALB/cJ mice. Br J Nutr 107:1787–1792
Jin CL, Yang LX, Wu XH, Li Q, Ding MP, Fan YY, Zhang WP, Luo JH, Chen Z (2005) Effects of carnosine on amygdaloid-kindled seizures in Sprague–Dawley rats. Neuroscience 135:939–947
Kalaz EB, Çoban J, Aydın AF, Doğan-Ekici I, Doğru-Abbasoğlu S, Öztezcan S, Uysal M (2014) Carnosine and taurine treatments decreased oxidative stress and tissue damage induced by D-galactose in rat liver. J Physiol Biochem 70:15–25
Lan Z, Liu J, Chen L, Fu Q, Luo J, Qu R, Kong L, Ma S (2012) Danggui-Shaoyao-San ameliorates cognition deficits and attenuates oxidative stress-related neuronal apoptosis in d-galactose-induced senescent mice. J Ethnopharmacol 141:386–395
Lawrence RA, Burk RF (1976) Glutathione peroxidase activity in selenium-deficient rat liver. Biochem Biophys Res Commun 71:952–958
Menzie J, Prentice H, Wu JY (2013) Neuroprotective mechanisms of taurine against ischemic stroke. Brain Sci 3:877–907
Miyazaki T, Matsuzaki Y (2014) Taurine and liver diseases: a focus on the heterogeneous protective properties of taurine. Amino Acids 46:101–110
Mylorie AA, Collins H, Umbles C, Kyle J (1986) Erythrocyte superoxide dismutase activity and other parameters of copper status in rats ingesting lead acetate. Toxicol Appl Pharmacol 82:512–520
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxidation in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Parıldar-Karpuzoğlu H, Mehmetçik G, Özdemirler-Erata G, Doğru-Abbasoğlu S, Koçak-Toker N, Uysal M (2008) The effect of taurine treatment on prooxidant-antioxidant balance in livers and brains of old rats. Pharmacol Rep 60:673–678
Prakash A, Kumar A (2013) Pioglitazone alleviates the mitochondrial apoptotic pathway and mito-oxidative damage in the d-galactose-induced mouse model. Clin Exp Pharmacol Physiol 40:644–651
Reznick AZ, Packer L (1994) Oxidative damage to proteins: spectrophotometric method for carbonyl assay. Methods Enzymol 233:357–363
Rosemberg DB, da Rocha RF, Rico EP, Zanotto-Filho A, Dias RD, Bogo MR (2010) Taurine prevents enhancement of acetylcholinesterase activity induced by acute ethanol exposure and decreases the level of markers of oxidative stress in zebra fish brain. Neuroscience 171:683–692
Ruan Q, Hu X, Ao H, Ma H, Gao Z, Liu F, Kong D, Bao Z, Yu Z (2014) The neurovascular protective effects of huperzine A on D-galactose-induced inflammatory damage in the rat hippocampus. Gerontology 60:424–439
Schaffer S, Azuma J, Takahashi K, Mozaffari M (2003) Why is taurine cytoprotective? Adv Exp Med Biol 526:307–321
Smith PK, Krohn RI, Hermanson GT, Mallia AK, Gartner FH, Provenzano MD, Fujimoto EK, Goeke NM, Olson BJ, Klenk DC (1985) Measurement of protein using bicinchoninic acid. Anal Biochem 150:76–85
Stvolinskii SL, Fedorova TN, Yuneva MO, Boldyrev AA (2003) Protective effect of carnosine on Cu, Zn-superoxide dismutase during impaired oxidative metabolism in the brain in vivo. Bull Exp Biol Med 135:130–132
Tsai SJ, Yin MC (2012) Anti-oxidative, anti-glycative and anti-apoptotic effects of oleanolic acid in brain of mice treated by D-galactose. Eur J Pharmacol 689:81–88
Uysal M, Doğru-Abbasoğlu S, Koçak-Toker N (2015) Carnosine protection against liver injury. In: Preedy VR (ed) Imidazole dipeptides. Chemistry, analysis, function and effects. The Royal Society of Chemistry, Cambridge, pp 510–527
Wu W, Wang X, Xiang Q, Meng X, Peng Y, Du N, Liu Z, Sun Q, Wang C, Liu X (2014) Astaxanthin alleviates brain aging in rats by attenuating oxidative stress and increasing BDNF levels. Food Funct 5:158–166
Xian YF, Su ZR, Chen JN, Lai XP, Mao QQ, Cheng CH, Ip SP, Lin ZX (2014) Isorhynchophylline improves learning and memory impairments induced by D-galactose in mice. Neurochem Int 76:42–49
Yıldırım Z, Kılıç N, Özer Ç, Babul A, Take G, Erdoğan D (2007) Effects of taurine in cellular responses to oxidative stress in young and middle-aged rat liver. Ann N Y Acad Sci 1100:553–561
Zhang WW, Sun QX, Liu YH, Gao W, Li YH, Lu K, Wang Z (2011) Chronic administration of Liu Wei Dihuang protects rat’s brain against D-galactose-induced impairment of cholinergic system. Acta Physiol Sin 63:245–255
Acknowledgment
The present work was supported by Research Fund of Istanbul University (Project No: 5786).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aydın, A.F., Çoban, J., Doğan-Ekici, I. et al. Carnosine and taurine treatments diminished brain oxidative stress and apoptosis in D-galactose aging model. Metab Brain Dis 31, 337–345 (2016). https://doi.org/10.1007/s11011-015-9755-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-015-9755-0